Health Priorities and Participation in Peer-Led Active Rehabilitation Camps Among Persons with Spinal Cord Injury: A Prospective Cohort Study
Abstract
1. Introduction
2. Materials and Methods
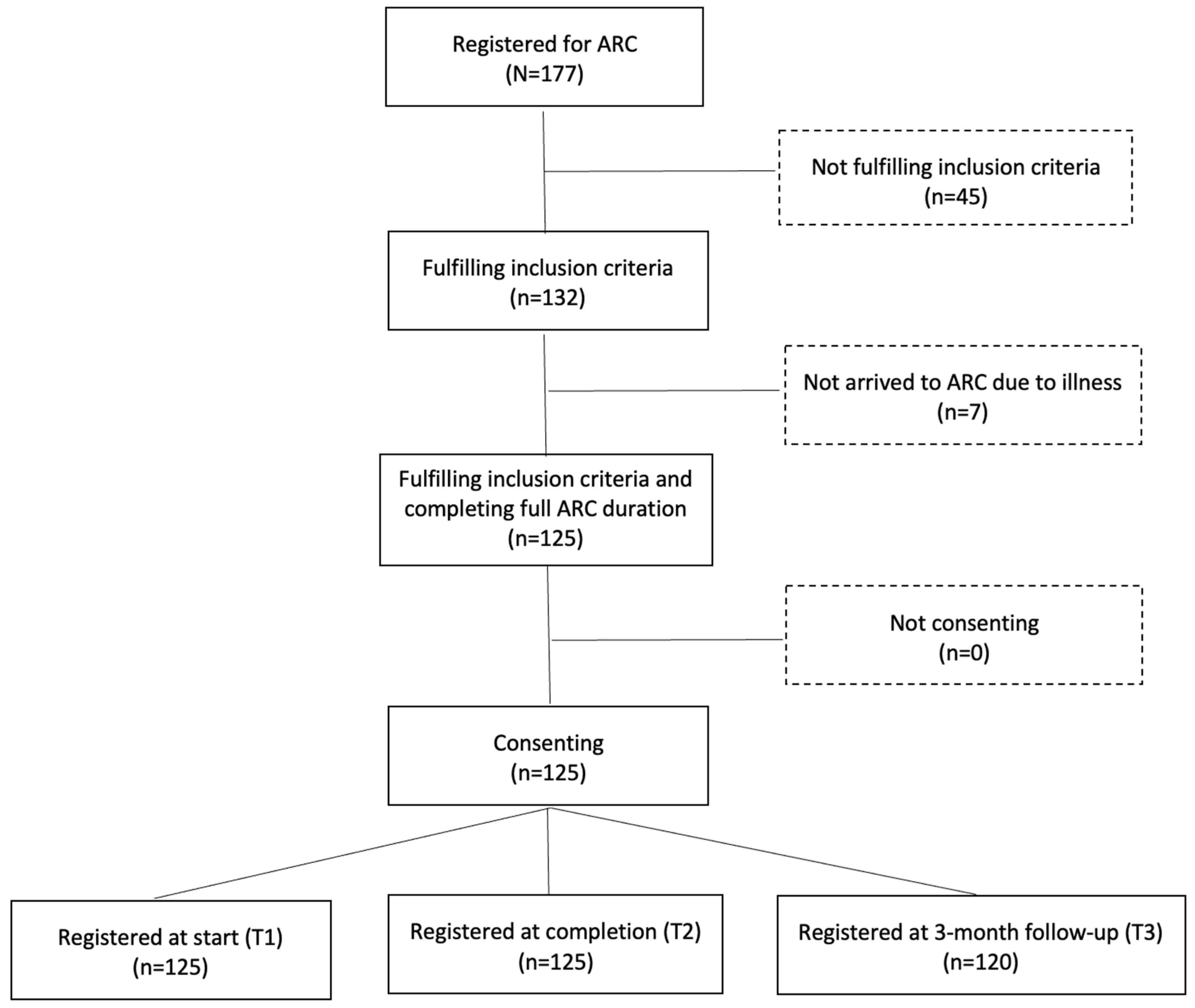
2.1. Design
2.2. Setting and Participants
2.3. Procedures
2.4. Outcomes
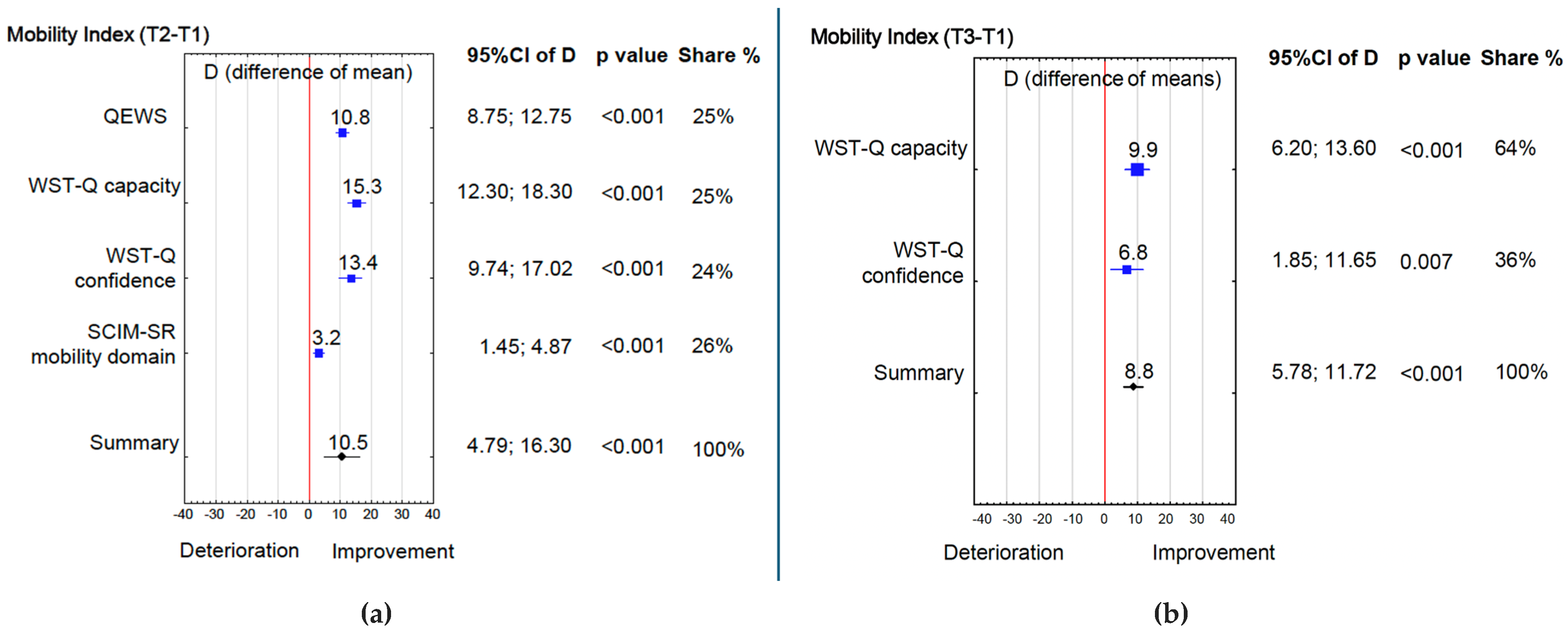
- Mobility function (walking & wheeling) was matched with four Inter-PEER outcome measures:
- ➢
- The Queensland Evaluation of Wheelchair Skills (QEWS), an SCI-specific measure that assesses the abilities of: (1) negotiating an indoor circuit; (2) ascending and descending a ramp; (3) maintaining balance on the back wheels; (4) ascending and descending a gutter; and (5) distance covered during a six-minute push test [14]. Each task is scored 0–5 (total: 0–25). QEWS is simple to administer, reliable, valid and sufficiently sensitive for detecting changes during ARC and a 10-week period of inpatient rehabilitation [11,14]. The internal consistency of the QEWS was satisfactory in this study cohort (α = 0.84–0.86).
- ➢
- The Wheelchair Skills Test Questionnaire (WST-Q, v4.3) for manually operated wheelchairs was used to subjectively assess capacity and confidence in 24 wheelchair skills, with capacity and confidence scores converted to a 0–100 scale [15]. The WST-Q has demonstrated strong content, construct, and concurrent validity for individuals with SCI [15]. A success rate for individual skills ≥ 20% was considered clinically significant [15]. The internal consistency for the WST-Q capacity in this study cohort was satisfactory for particular study terms (α = 0.95–0.96) and for the WST-Q confidence (α = 0.95–0.96).
- ➢
- The mobility indoors/outdoors domain of the Spinal Cord Independence Measure Self-report (SCIM-SR) [16]. The SCIM-SR evaluates the level of independence in individuals with SCI based on 17 items divided into three domains: (1) self-care (eating, grooming, bathing, dressing), (2) respiration and sphincter management, and (3) mobility (in room/toilet and indoors/outdoors). Domain scores range between 0 and 40 with higher scores indicating a higher functional level. Each item is weighted according to the subjective value of the activity, the difficulty level of performing the task, and the time required. The internal consistency for the SCIM-SR domains in this study cohort was satisfactory (α = 0.78–0.80).
- ➢
- The corresponding item of the Moorong Self-efficacy scale (MSES), i.e., Get out of my house (Item 5) [17]. The MSES is a 16-item scale rating confidence in the ability to control behaviour and outcomes on a 7-point Likert scale (1 = very uncertain, 7 = very certain) with higher scores indicating high self-efficacy [18]. It was developed specifically for people with SCI, and comprises three domains: (1) personal function, (2) social function, and (3) general self-efficacy [18]. The MSES has shown strong evidence of construct validity, stability and internal consistency [17]. The internal consistency for the MSES in this study cohort was satisfactory for particular study terms (α = 0.88–0.91).
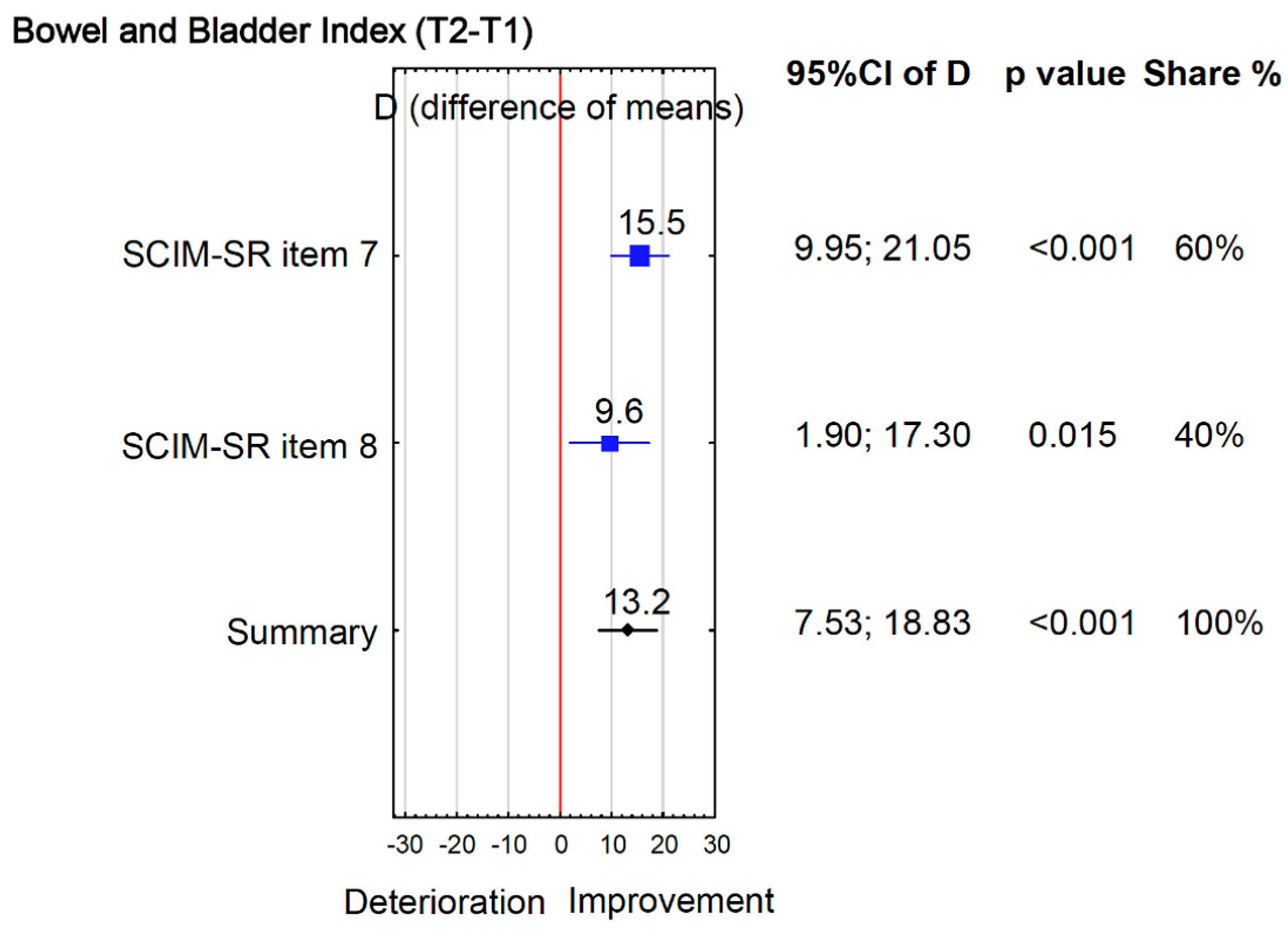
- Bowel and bladder functions were matched with two subjective measures:
- ➢
- The corresponding items of the SCIM-SR, i.e., Bladder management (Item 6), Bowel management (Item 7), Using the toilet (Item 8), Transfer from the wheelchair to the toilet/tub (Item 11) [16].
- ➢
- The corresponding item 2 of the MSES, i.e., I can avoid having bowel accidents.
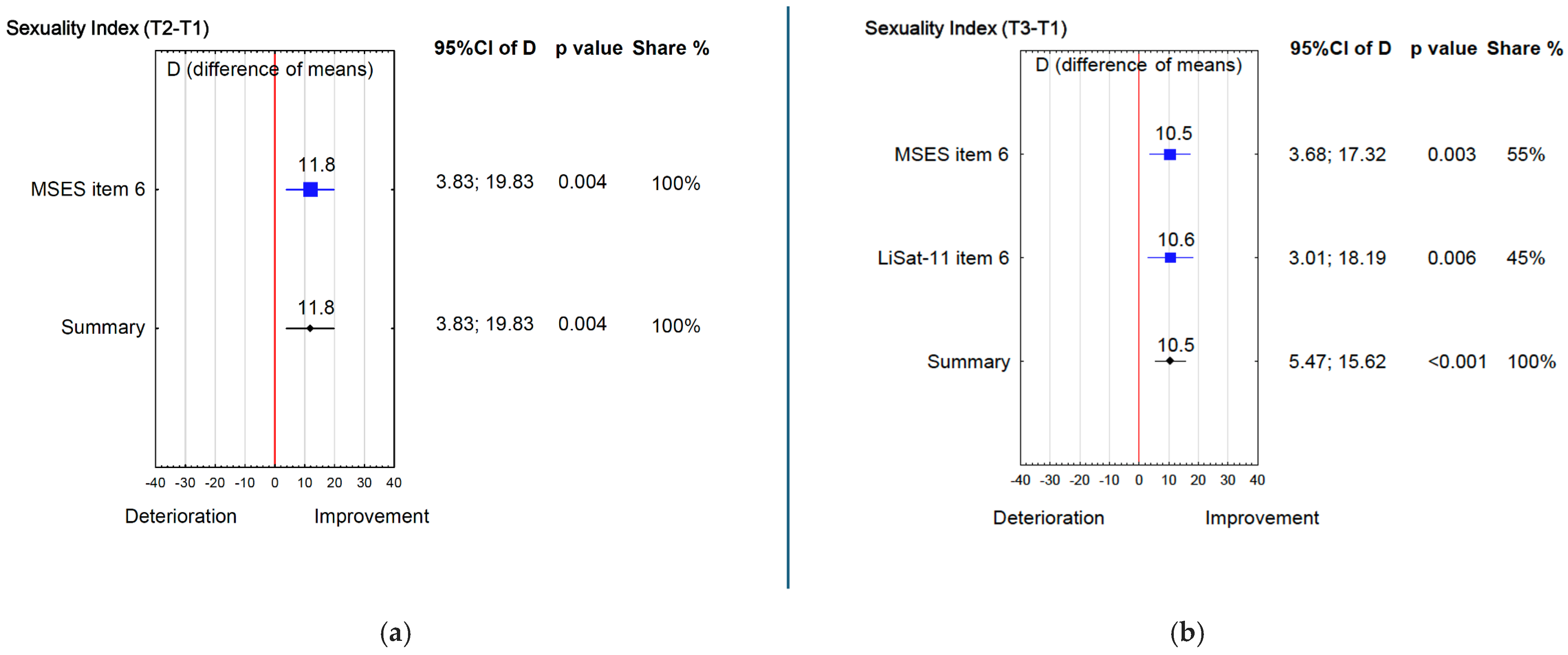
- Sexual function was matched with two Inter-PEER outcome measures:
- ➢
- The corresponding item of the Life Satisfaction Questionnaire (LiSat-11), i.e., satisfaction with sexual life (Item 5) [18]. The LiSat-11 consists of 11 items covering global life satisfaction (one item) and domain-specific satisfaction across ten areas. Each item is rated on a 6-point scale from 1 (very dissatisfied) to 6 (very satisfied), with higher scores indicating greater life satisfaction. The LiSat-11 is valid for the general population [18] and has demonstrated satisfactory internal consistency in individuals with SCI [19]. In this study cohort, the internal consistency of the LiSat-11 was satisfactory (α = 0.85–0.86).
- ➢
- The corresponding item 6 of the MSES, i.e., I can have a satisfying sexual relationship.
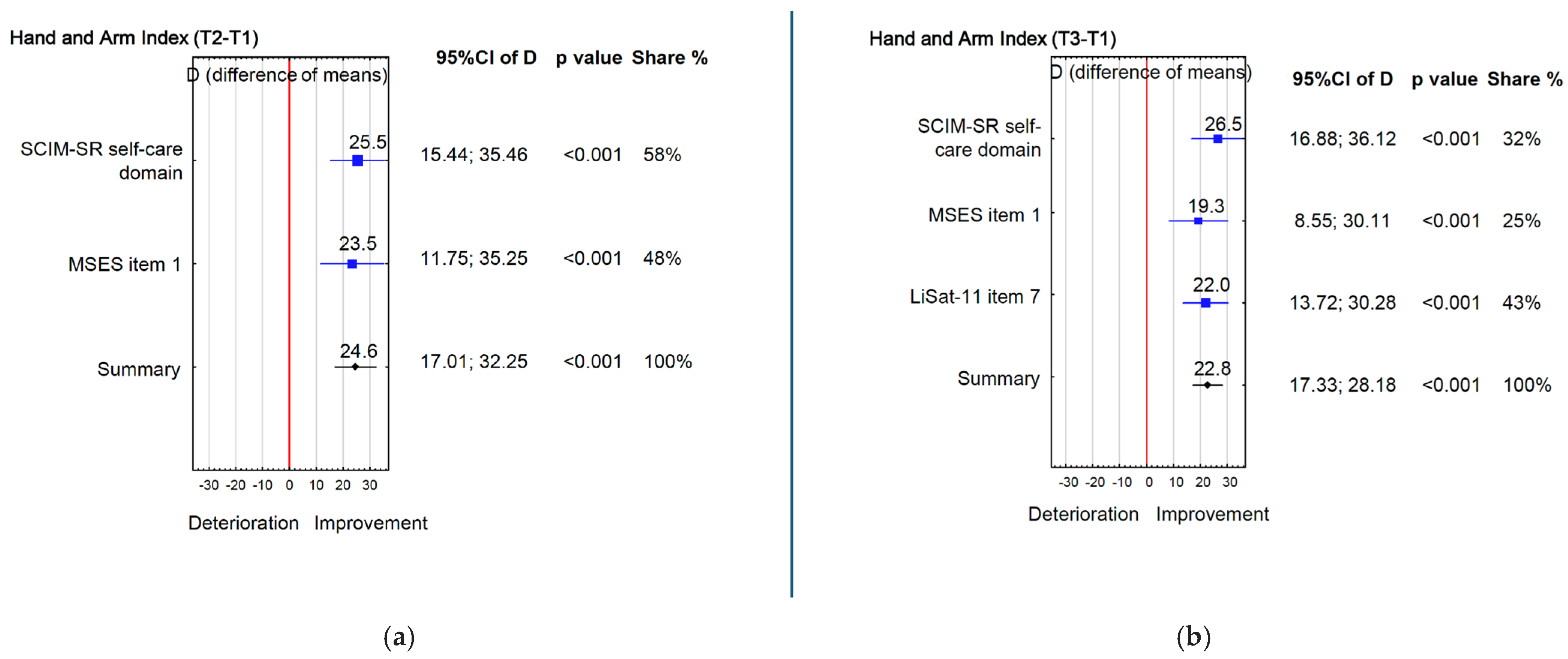
- Management of the tetraplegic upper limb aims to maximize hand function to enable performance of daily tasks as independently as possible [20]. Based on that, hand and arm function in individuals with tetraplegia was matched with three Inter-PEER outcome measures:
2.5. Statistical Analysis
3. Results
4. Discussion
Study Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Feigin, V.L.; Nichols, E.; Alam, T.; Bannick, M.S.; Beghi, E.; Blake, N.; Culpepper, W.J.; Dorsey, E.R.; Elbaz, A.; Ellenbogen, R.G.; et al. Global, Regional, and National Burden of Neurological Disorders, 1990–2016: A Systematic Analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019, 18, 459–480. [Google Scholar] [CrossRef] [PubMed]
- Simpson, L.A.; Eng, J.J.; Hsieh, J.T.C.; Wolfe And The Spinal Cord Injury; Re, D.L. The Health and Life Priorities of Individuals with Spinal Cord Injury: A Systematic Review. J. Neurotrauma 2012, 29, 1548–1555. [Google Scholar] [CrossRef] [PubMed]
- Huh, S.; Ko, H.-Y. Recovery Target Priorities of People with Spinal Cord Injuries in Korea Compared with Other Countries: A Survey. Spinal Cord 2020, 58, 998–1003. [Google Scholar] [CrossRef]
- Lo, C.; Tran, Y.; Anderson, K.; Craig, A.; Middleton, J. Functional Priorities in Persons with Spinal Cord Injury: Using Discrete Choice Experiments to Determine Preferences. J. Neurotrauma 2016, 33, 1958–1968. [Google Scholar] [CrossRef]
- Tasiemski, T.; Priebe, M.M.; Wilski, M. Life Satisfaction and Life Values in People with Spinal Cord Injury Living in Three Asian Countries: A Multicultural Study. J. Spinal Cord Med. 2013, 36, 118–126. [Google Scholar] [CrossRef] [PubMed]
- Tasiemski, T.; Kujawa, J.; Tederko, P.; Rubinelli, S.; Middleton, J.W.; Craig, A.; Post, M.W. Comparison of Life Satisfaction in Persons with Spinal Cord Injury Living in 22 Countries with Different Economic Status. Arch. Phys. Med. Rehabil. 2021, 103, 1285–1293. [Google Scholar] [CrossRef]
- Roels, E.H.; Aertgeerts, B.; Ramaekers, D.; Peers, K. Hospital- and Community-Based Interventions Enhancing (Re)Employment for People with Spinal Cord Injury: A Systematic Review. Spinal Cord 2016, 54, 2–7. [Google Scholar] [CrossRef]
- Divanoglou, A.; Tasiemski, T.; Augutis, M.; Trok, K. Active Rehabilitation—A Community Peer-Based Approach for Persons with Spinal Cord Injury: International Utilisation of Key Elements. Spinal Cord 2017, 55, 545–552. [Google Scholar] [CrossRef]
- Tederko, P.; Jagodzinski, R.; Krasuski, M.; Tarnacka, B. People with Spinal Cord Injury in Poland. Am. J. Phys. Med. Rehabil. 2017, 96, S102–S105. [Google Scholar] [CrossRef]
- Divanoglou, A.; Tasiemski, T.; Jörgensen, S. INTERnational Project for the Evaluation of “activE Rehabilitation” (Inter-PEER)—A Protocol for a Prospective Cohort Study of Community Peer-Based Training Programmes for People with Spinal Cord Injury. BMC Neurol. 2020, 20, 14. [Google Scholar] [CrossRef]
- Divanoglou, A.; Trok, K.; Jörgensen, S.; Hultling, C.; Sekakela, K.; Tasiemski, T. Active Rehabilitation for Persons with Spinal Cord Injury in Botswana–Effects of a Community Peer-Based Programme. Spinal Cord 2019, 57, 897–905. [Google Scholar] [CrossRef]
- Tasiemski, T.; Urbański, P.K.; Jörgensen, S.; Feder, D.; Trok, K.; Divanoglou, A. Effects of Wheelchair Skills Training during Peer-Led Active Rehabilitation Camps for People with Spinal Cord Injury in Poland: A Cohort Study. Spinal Cord 2024, 62, 651–657. [Google Scholar] [CrossRef]
- Divanoglou, A.; Berndtsson, E.; Tasiemski, T.; Fellinghauer, C.S.; Jörgensen, S. Effects of Community Peer-Led Programmes for People with Spinal Cord Injury in Sweden–the INTERnational Project for the Evaluation of Active Rehabilitation (INTER-PEER). Spinal Cord 2025, 63, 567–578. [Google Scholar] [CrossRef]
- Gollan, E.J.; Harvey, L.A.; Simmons, J.; Adams, R.; McPhail, S.M. Development, Reliability and Validity of the Queensland Evaluation of Wheelchair Skills (QEWS). Spinal Cord 2015, 53, 743–749. [Google Scholar] [CrossRef] [PubMed]
- Kirby, R.L.; Worobey, L.A.; Cowan, R.; Pedersen, J.P.; Heinemann, A.W.; Dyson-Hudson, T.A.; Shea, M.; Smith, C.; Rushton, P.W.; Boninger, M.L. Wheelchair Skills Capacity and Performance of Manual Wheelchair Users With Spinal Cord Injury. Arch. Phys. Med. Rehabil. 2016, 97, 1761–1769. [Google Scholar] [CrossRef]
- Fekete, C.; Eriks-Hoogland, I.; Baumberger, M.; Catz, A.; Itzkovich, M.; Lüthi, H.; Post, M.W.M.; Von Elm, E.; Wyss, A.; Brinkhof, M.W.G. Development and Validation of a Self-Report Version of the Spinal Cord Independence Measure (SCIM III). Spinal Cord 2013, 51, 40–47. [Google Scholar] [CrossRef]
- Middleton, J.W.; Tran, Y.; Lo, C.; Craig, A. Reexamining the Validity and Dimensionality of the Moorong Self-Efficacy Scale: Improving Its Clinical Utility. Arch. Phys. Med. Rehabil. 2016, 97, 2130–2136. [Google Scholar] [CrossRef] [PubMed]
- Fugl-Meyer, A.R.; Bränholm, I.-B.; Fugl-Meyer, K.S. Happiness and Domain-Specific Life Satisfaction in Adult Northern Swedes. Clin. Rehabil. 1991, 5, 25–33. [Google Scholar] [CrossRef]
- Post, M.W.; Van Leeuwen, C.M.; Van Koppenhagen, C.F.; De Groot, S. Validity of the Life Satisfaction Questions, the Life Satisfaction Questionnaire, and the Satisfaction with Life Scale in Persons with Spinal Cord Injury. Arch. Phys. Med. Rehabil. 2012, 93, 1832–1837. [Google Scholar] [CrossRef]
- Anderson, K.D. Targeting Recovery: Priorities of the Spinal Cord-Injured Population. J. Neurotrauma 2004, 21, 1371–1383. [Google Scholar] [CrossRef]
- Fekete, C.; Post, M.W.; Bickenbach, J.; Middleton, J.; Prodinger, B.; Selb, M.; Stucki, G. A Structured Approach to Capture the Lived Experience of Spinal Cord Injury: Data Model and Questionnaire of the International Spinal Cord Injury Community Survey. Am. J. Phys. Med. Rehabil. 2017, 96, S5–S16. [Google Scholar] [CrossRef] [PubMed]
- Scivoletto, G.; Tamburella, F.; Laurenza, L.; Molinari, M. The Spinal Cord Independence Measure: How Much Change Is Clinically Significant for Spinal Cord Injury Subjects. Disabil. Rehabil. 2013, 35, 1808–1813. [Google Scholar] [CrossRef]
- Urbański, P.K.; Kim, Y.; Conners, R.T.; Nadolska, A.; Tasiemski, T. Life Satisfaction in Persons with Spinal Cord Injury across the Seasons. Spinal Cord 2021, 59, 193–200. [Google Scholar] [CrossRef]
- Giurleo, C.; McIntyre, A.; Kras-Dupuis, A.; Wolfe, D.L. Addressing the Elephant in the Room: Integrating Sexual Health Practice in Spinal Cord Injury Rehabilitation. Disabil. Rehabil. 2022, 44, 3245–3252. [Google Scholar] [CrossRef]
- James, M.H.; Porter, J.E.; Kattel, S.; Prokopiv, V.; Hopwood, P. Peer Educators in the Facilitation of Sexuality and Respectful Relationship Education for People with an Intellectual Disability: A Scoping Review and Narrative Synthesis. Sex. Disabil. 2022, 40, 487–502. [Google Scholar] [CrossRef]
- Tasiemski, T.; Wilski, M.; Urbański, P. One World Project’s Wheelchair Skills Training Camp in Morocco-Effects of a Community Peer-Based Programme. Disabil. Rehabil. Assist. Technol. 2023, 18, 736–742. [Google Scholar] [CrossRef] [PubMed]
- Ferretti, E.C.; Curi, H.T.; Andrade, L.F.; Cooper, R.A.; Soárez, P.C.D. Conceptual Mapping Proposed to Comprehend the Effect of Wheelchair Mobility on Social Participation and Quality of Life: A Systematic Review*. Disabil. Rehabil. Assist. Technol. 2024, 19, 814–830. [Google Scholar] [CrossRef] [PubMed]
- Savic, G.; Frankel, H.L.; Jamous, M.A.; Soni, B.M.; Charlifue, S. Long-Term Bladder and Bowel Management after Spinal Cord Injury: A 20-Year Longitudinal Study. Spinal Cord 2018, 56, 575–581. [Google Scholar] [CrossRef]
- Wirth, B.; van Hedel, H.J.A.; Kometer, B.; Dietz, V.; Curt, A. Changes in Activity After a Complete Spinal Cord Injury as Measured by the Spinal Cord Independence Measure II (SCIM II). Neurorehabil. Neural Repair 2008, 22, 145–153. [Google Scholar] [CrossRef]
- Bandura, A. Self-Efficacy: Toward a Unifying Theory of Behavioral Change. Psychol. Rev. 1977, 84, 191. [Google Scholar] [CrossRef]
| Demographic and Injury Characteristics | Participants with SCI (N = 125) |
|---|---|
| Sex (n, %) | |
| Male | 83 (66.4) |
| Female | 42 (33.6) |
| Age for those with TSCI (mean years ± SD) | 42.2 ± 14.2 |
| Age for those with NTSCI (mean years ± SD) | 32.3 ± 15.8 |
| Marital status (n, %) | |
| Single | 59 (47.2) |
| Married | 50 (40.0) |
| Cohabiting or in a partnership | 7 (5.6) |
| Separated or divorced | 7 (5.6) |
| Widowed | 2 (1.6) |
| Education (n, %) | |
| Primary | 27 (20.8) |
| Vocational | 35 (28.0) |
| Secondary | 33 (26.4) |
| Post-secondary | 4 (3.2) |
| Bachelor | 9 (7.2) |
| Post-graduate | 18 (14.4) |
| Employment status (n, %) | |
| Employed | 15 (12.0) |
| Not employed | 38 (30.4) |
| Student | 10 (8.0) |
| Retired due to health condition | 51 (40.8) |
| Retired due to age | 11 (8.8) |
| Level o SCI (n, %) | |
| Paraplegia | 79 (63.2) |
| Tetraplegia | 46 (36.8) |
| Completeness of SCI (n, %) | |
| Complete | 54 (43.2) |
| Incomplete | 71 (56.8) |
| Cause of traumatic SCI (n, %) | 93 (74.4) |
| Sport | 12 (9.6) |
| Recreation | 13 (10.4) |
| Work related | 10 (8.0) |
| Traffic accident | 28 (22.4) |
| Fall < 1 m | 4 (3.2) |
| Fall > 1 m | 26 (20.8) |
| Cause of non-traumatic SCI (n, %) | 32 (25.6) |
| Spina bifida | 21 (16.8) |
| Degenerative changes | 2 (1.6) |
| Tumour benign | 6 (4.8) |
| Tumour malignant | 1 (0.8) |
| Vascular disorders | 1 (0.8) |
| Infection | 1 (0.8) |
| Time since injury for those with TSCI (mean years ± SD) | 5.7 ± 7.2 |
| Time since disease for those with NTSCI (mean years ± SD) | 14.8 ± 10.2 |
| Attendance in Active Rehabilitation Camps (n, %) | |
| First comers | 81 (64.8) |
| Recurrent comers | 44 (35.2) |
| T2 − T1 | T3 − T1 | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Health Priorities Following SCI | n | Range | T1 | T2 | T3 | p Value | Effect Size | p Value | Effect Size |
| Mobility (walking & wheeling) 1 | |||||||||
| QEWS (total score) | 96 | 1–25 | 11.8 ± 7.2 | 14.4 ± 7.4 | N/A | ≤0.001 | 2.3 | N/A | N/A |
| WST-Q capacity (total score) | 96 | 1–100 | 48.8 ± 25.3 | 64.1 ± 25.5 | 58.7 ± 28.2 | ≤0.001 | 2.2 | ≤0.001 | 1.2 |
| WST-Q confidence (total score) | 96 | 1–100 | 57.0 ± 27.9 | 70.4 ± 25.1 | 63.6 ± 28.1 | ≤0.001 | 1.6 | 0.001 | 0.7 |
| SCIM-SR mobility indoors/outdoors (domain score) | 96 | 0–30 | 6.1 ± 2.5 | 7.1 ± 2.0 | 6.7 ± 2.4 | 0.001 | 0.7 | 0.144 | N/A |
| MSES item 5. Get out of my house | 96 | 1–7 | 4.9 ± 2.0 | 5.3 ± 1.8 | 4.9 ± 1.9 | 0.147 | N/A | 0.781 | N/A |
| Bowel and bladder function 1 | |||||||||
| SCIM-SR item 6. Bladder | 116 | 0–15 | 4.6 ± 4.1 | 5.3 ± 4.2 | 5.0 ± 4.3 | 0.111 | N/A | 0.428 | N/A |
| SCIM-SR item 7. Bowel | 116 | 0–10 | 6.6 ± 4.7 | 8.2 ± 4.1 | 7.4 ± 4.4 | 0.001 | 0.7 | 0.228 | N/A |
| SCIM-SR item 8. Toilet use | 116 | 0–5 | 2.6 ± 1.9 | 3.1 ± 1.8 | 2.7 ± 1.8 | 0.015 | 0.5 | 0.751 | N/A |
| MSES item 2. Avoid bowel accidents | 116 | 1–7 | 4.6 ± 1.8 | 4.9 ± 1.7 | 4.7 ± 1.8 | 0.188 | N/A | 0.427 | N/A |
| Sexual function 1 | |||||||||
| MSES item 6. Satisfying sexual relation | 99 | 1–7 | 3.6 ± 1.9 | 4.3 ± 1.8 | 4.2 ± 1.8 | 0.004 | 0.6 | 0.004 | 0.5 |
| LiSat-11 item 6. Sexual life | 99 | 1–6 | 2.5 ± 1.7 | N/A | 3.1 ± 1.7 | N/A | N/A | 0.010 | 0.6 |
| Arm and hand function 2 | |||||||||
| SCIM-SR self-care (domain score) | 44 | 0–20 | 9.7 ± 5.8 | 14.8 ± 5.5 | 15.0 ± 5.1 | ≤0.001 | 0.9 | ≤0.001 | 0.9 |
| MSES item 1. Maintain personal hygiene | 44 | 1–7 | 4.7 ± 2.1 | 6.1 ± 1.3 | 5.9 ± 1.5 | 0.001 | 0.6 | 0.003 | 0.6 |
| LiSat-11 item 7. Manage self-care | 44 | 1–6 | 3.1 ± 1.5 | N/A | 4.4 ± 1.2 | N/A | N/A | ≤0.001 | 0.9 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Tasiemski, T.; Urbański, P.K.; Feder, D.; Lewandowska, M.; Divanoglou, A. Health Priorities and Participation in Peer-Led Active Rehabilitation Camps Among Persons with Spinal Cord Injury: A Prospective Cohort Study. J. Clin. Med. 2026, 15, 176. https://doi.org/10.3390/jcm15010176
Tasiemski T, Urbański PK, Feder D, Lewandowska M, Divanoglou A. Health Priorities and Participation in Peer-Led Active Rehabilitation Camps Among Persons with Spinal Cord Injury: A Prospective Cohort Study. Journal of Clinical Medicine. 2026; 15(1):176. https://doi.org/10.3390/jcm15010176
Chicago/Turabian StyleTasiemski, Tomasz, Piotr Kazimierz Urbański, Dawid Feder, Magdalena Lewandowska, and Anestis Divanoglou. 2026. "Health Priorities and Participation in Peer-Led Active Rehabilitation Camps Among Persons with Spinal Cord Injury: A Prospective Cohort Study" Journal of Clinical Medicine 15, no. 1: 176. https://doi.org/10.3390/jcm15010176
APA StyleTasiemski, T., Urbański, P. K., Feder, D., Lewandowska, M., & Divanoglou, A. (2026). Health Priorities and Participation in Peer-Led Active Rehabilitation Camps Among Persons with Spinal Cord Injury: A Prospective Cohort Study. Journal of Clinical Medicine, 15(1), 176. https://doi.org/10.3390/jcm15010176





