Irritable Bowel Syndrome in Inflammatory Bowel Disease: An Evidence-Based Practical Review
Abstract
1. Introduction
2. Challenging Transitional Perspectives
3. Obstacles to Understanding IBS in IBD
3.1. Distinguishing Active IBD from IBS in IBD
3.1.1. Fecal Calprotectin
3.1.2. Cross-Sectional Imaging
3.1.3. Endoscopic Assessment
3.1.4. Histological Assessment
3.1.5. Patient-Reported Outcome Measures (PROMs)
3.2. Determining the Prevalence of IBS in IBD
4. The Etiology of IBS in IBD
4.1. Altered Motility and Visceral Hypersensitivity
4.2. Epithelial Barrier Disruption and Mucosal Immune Dysfunction
4.3. Dysbiosis
4.4. Gut–Central Nervous System Neural Processing
5. General Approaches to Managing IBS in IBD
6. Management of Key Gastrointestinal Symptoms
6.1. Abdominal Pain
6.1.1. Non-Pharmacological Management of Abdominal Pain
Brain–Gut Behavioral Therapy
Low-FODMAP Diet
Physical Exercise
6.1.2. Pharmacological Management of Abdominal Pain
Opioids
Brain–Gut Neuromodulators
Antispasmodics
6.2. Constipation
6.2.1. Non-Pharmacological Management of Constipation
Diet
Physical Exercise
Pelvic Floor Biofeedback Therapy
6.2.2. Pharmacological Management of Constipation
6.3. Diarrhea
6.3.1. Non-Pharmacological Management of Diarrhea
6.3.2. Pharmacological Management of Diarrhea
6.4. Fecal Incontinence
6.4.1. Non-Pharmacological Management of Fecal Incontinence
6.4.2. Pharmacological Management of Fecal Incontinence
6.5. Abdominal Bloating
6.5.1. Non-Pharmacological Management of Abdominal Bloating
Diet
Brain–Gut Behavioral Therapy
Biofeedback Therapy
6.5.2. Pharmacological Management of Abdominal Bloating
7. Future Directions
7.1. Advancing Diagnostic Precision
7.2. Mechanistic and Longitudinal Research
7.3. Targeted Therapeutic Trials
7.4. Holistic Outcome Assessment
7.5. The Patient-Physician Relationship
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CAI | Clinical activity index |
| CD | Crohn’s disease |
| CDAI | Clinical disease activity index |
| CRP | C-reactive protein |
| DGBI | Disorder of Gut–Brain Interaction |
| FODMAP | Fermentable oligosaccharides, disaccharides, monosaccharides and polyols |
| FDA | Food and Drug Administration |
| FI | Fecal incontinence |
| HBI | Harvey–Bradshaw Index |
| IBD | Inflammatory bowel disease |
| IBDQ | Inflammatory bowel disease questionnaire |
| IBS | Irritable bowel syndrome |
| IBS-C | Irritable bowel syndrome—constipation predominant |
| IBS-D | Irritable bowel syndrome—diarrhea predominant |
| IBS-SSS | Irritable bowel syndrome—severity scoring system |
| IPAA | Ileal pouch–anal anastomosis |
| MCT | Multi-convergent therapy |
| PROM | Patient-reported outcome measure |
| QoL | Quality of life |
| RCT | Randomized controlled trial |
| SCCAI | Simple clinical colitis activity index |
| SIBDQ | Short inflammatory bowel disease questionnaire |
| SIBO | Small intestinal bacterial overgrowth |
| SSRI | Selective serotonin reuptake inhibitor |
| TCA | Tricyclic antidepressant |
| UC | Ulcerative colitis |
References
- Sperber, A.D.; Bangdiwala, S.I.; Drossman, D.A.; Ghoshal, U.C.; Simren, M.; Tack, J.; Whitehead, W.E.; Dumitrascu, D.L.; Fang, X.; Fukudo, S.; et al. Worldwide Prevalence and Burden of Functional Gastrointestinal Disorders, Results of Rome Foundation Global Study. Gastroenterology 2021, 160, 99–114.e3. [Google Scholar] [CrossRef]
- Jaafari, H.; Houghton, L.A.; West, R.M.; Agrawal, A.; Aziz, I.; Black, C.J.; Corsetti, M.; Shuweihdi, F.; Eugenicos, M.; Paine, P.A.; et al. The national prevalence of disorders of gut brain interaction in the United Kingdom in comparison to their worldwide prevalence: Results from the Rome foundation global epidemiology study. Neurogastroenterol. Motil. 2023, 35, e14574. [Google Scholar] [CrossRef] [PubMed]
- Mearin, F.; Lacy, B.E.; Chang, L.; Chey, W.D.; Lembo, A.J.; Simren, M.; Spiller, R. Bowel Disorders. Gastroenterology 2016, 150, 1393–1407. [Google Scholar]
- Sartor, R.B. Mechanisms of disease: Pathogenesis of Crohn’s disease and ulcerative colitis. Nat. Clin. Pract. Gastroenterol. Hepatol. 2006, 3, 390–407. [Google Scholar] [CrossRef]
- Ng, S.C.; Shi, H.Y.; Hamidi, N.; Underwood, F.E.; Tang, W.; Benchimol, E.I.; Panaccione, R.; Ghosh, S.; Wu, J.C.Y.; Chan, F.K.L.; et al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: A systematic review of population-based studies. Lancet 2017, 390, 2769–2778. [Google Scholar] [CrossRef]
- Hracs, L.; Windsor, J.W.; Gorospe, J.; Cummings, M.; Coward, S.; Buie, M.J.; Quan, J.; Goddard, Q.; Caplan, L.; Markovinović, A.; et al. Global evolution of inflammatory bowel disease across epidemiologic stages. Nature 2025, 642, 458–466. [Google Scholar] [CrossRef] [PubMed]
- Wellens, J.; Sabino, J.; Vanuytsel, T.; Tack, J.; Vermeire, S. Recent advances in clinical practice: Mastering the challenge-managing IBS symptoms in IBD. Gut 2025, 74, 312–321. [Google Scholar] [CrossRef]
- Aziz, I.; Simrén, M. The overlap between irritable bowel syndrome and organic gastrointestinal diseases. Lancet Gastroenterol. Hepatol. 2021, 6, 139–148. [Google Scholar] [CrossRef] [PubMed]
- Aliu, A.; Bosch, D.; Keszthelyi, D.; Ardabili, A.R.; Colombel, J.F.; Sawyer, R.; Törnblom, H.; Hart, A.; Jonkers, D.M.A.E.; Pierik, M.J.; et al. Review article: A practical approach to persistent gastrointestinal symptoms in inflammatory bowel disease in remission. Aliment. Pharmacol. Ther. 2024, 59, 1470–1488. [Google Scholar] [CrossRef]
- Grover, M.; Herfarth, H.; Drossman, D.A. The functional-organic dichotomy: Postinfectious irritable bowel syndrome and inflammatory bowel disease-irritable bowel syndrome. Clin. Gastroenterol. Hepatol. 2009, 7, 48–53. [Google Scholar] [CrossRef]
- Isgar, B.; Harman, M.; Kaye, M.D.; Whorwell, P.J. Symptoms of irritable bowel syndrome in ulcerative colitis in remission. Gut 1983, 24, 190–192. [Google Scholar] [CrossRef]
- Reghefaoui, M.; Peresuodei, T.S.; Palacios, M.S.S.; Gill, A.; Orji, C.; Reghefaoui, T.; Mostafa, J. The Role of Serological Markers in the Prediction of Disease Course and Response to Therapy in Inflammatory Bowel Disease. Cureus 2023, 15, e48442. [Google Scholar] [CrossRef]
- Moran, G.W.; Gordon, M.; Sinopolou, V.; Radford, S.J.; Darie, A.M.; Vuyyuru, S.K.; Alrubaiy, L.; Arebi, N.; Blackwell, J.; Butler, T.D.; et al. British Society of Gastroenterology guidelines on inflammatory bowel disease in adults: 2025. Gut 2025, 74, s1–s101. [Google Scholar] [CrossRef]
- Pathirana, W.G.W.; Chubb, S.P.; Gillett, M.J.; Vasikaran, S.D. Faecal Calprotectin. Clin. Biochem. Rev. 2018, 39, 77–90. [Google Scholar] [PubMed]
- Lamb, C.A.; Kennedy, N.A.; Raine, T.; Hendy, P.A.; Smith, P.J.; Limdi, J.K.; Hayee, B.; Lomer, M.C.E.; Parkes, G.C.; Selinger, C.; et al. British Society of Gastroenterology consensus guidelines on the management of inflammatory bowel disease in adults. Gut 2019, 68, s1–s106. [Google Scholar] [CrossRef] [PubMed]
- Rokkas, T.; Portincasa, P.; Koutroubakis, I.E. Fecal calprotectin in assessing inflammatory bowel disease endoscopic activity: A diagnostic accuracy meta-analysis. J. Gastrointestin. Liver Dis. 2018, 27, 299–306. [Google Scholar] [CrossRef]
- Ananthakrishnan, A.N.; Adler, J.; Chachu, K.A.; Nguyen, N.H.; Siddique, S.M.; Weiss, J.M.; Sultan, S.; Velayos, F.S.; Cohen, B.L.; Singh, S. AGA Clinical Practice Guideline on the Role of Biomarkers for the Management of Crohn’s Disease. Gastroenterology 2023, 165, 1367–1399. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Ananthakrishnan, A.N.; Nguyen, N.H.; Cohen, B.L.; Velayos, F.S.; Weiss, J.M.; Sultan, S.; Siddique, S.M.; Adler, J.; Chachu, K.A. AGA Clinical Practice Guideline on the Role of Biomarkers for the Management of Ulcerative Colitis. Gastroenterology 2023, 164, 344–372. [Google Scholar] [CrossRef]
- Kopylov, U.; Yung, D.E.; Engel, T.; Avni, T.; Battat, R.; Ben-Horin, S.; Plevris, J.N.; Eliakim, R.; Koulaouzidis, A. Fecal calprotectin for the prediction of small-bowel Crohn’s disease by capsule endoscopy: A systematic review and meta-analysis. Eur. J. Gastroenterol. Hepatol. 2016, 28, 1137–1144. [Google Scholar] [CrossRef]
- Sipponen, T.; Haapamäki, J.; Savilahti, E.; Alfthan, H.; Hämäläinen, E.; Rautiainen, H.; Koskenpato, J.; Nuutinen, H.; Färkkilä, M. Fecal calprotectin and S100A12 have low utility in prediction of small bowel Crohn’s disease detected by wireless capsule endoscopy. Scand. J. Gastroenterol. 2012, 47, 778–784. [Google Scholar] [CrossRef]
- Rimola, J.; Torres, J.; Kumar, S.; Taylor, S.A.; Kucharzik, T. Recent advances in clinical practice: Advances in cross-sectional imaging in inflammatory bowel disease. Gut 2022, 71, 2587–2597. [Google Scholar] [CrossRef] [PubMed]
- Shaban, N.; Hoad, C.L.; Naim, I.; Alshammari, M.; Radford, S.J.; Clarke, C.; Marciani, L.; Moran, G. Imaging in inflammatory bowel disease: Current and future perspectives. Frontline Gastroenterol. 2022, 13, e28–e34. [Google Scholar] [CrossRef] [PubMed]
- Menys, A.; Taylor, S.A.; Emmanuel, A.; Ahmed, A.; Plumb, A.A.; Odille, F.; Alam, A.; Halligan, S.; Atkinson, D. Global small bowel motility: Assessment with dynamic MR imaging. Radiology 2013, 269, 443–450. [Google Scholar] [CrossRef]
- Menys, A.; Puylaert, C.; Nolthenius, C.E.T.; Plumb, A.A.; Makanyanga, J.; Tielbeek, J.A.; Pendse, D.; Brosens, L.A.; Rodriguez-Justo, M.; Atkinson, D.; et al. Quantified Terminal Ileal Motility during MR Enterography as a Biomarker of Crohn Disease Activity: Prospective Multi-Institution Study. Radiology 2018, 289, 428–435. [Google Scholar] [CrossRef]
- Plumb, A.A.; Moran, G.; Chowdhury, K.; Ahmed, N.; Philpott, S.; Ahmad, T.; Bloom, S.; Hart, A.; Jacobs, I.; Menys, A.; et al. Small Bowel Motility Quantified by Cine MRI to Predict Longer-Term Response in Patients with Crohn’s Disease Commencing Biological Therapy: The Motility Study. Inflamm. Bowel Dis. 2025, 31, 2438–2450. [Google Scholar] [CrossRef]
- Radford, S.J.; Taylor, S.; Moran, G. Ultrasound use to assess Crohn’s disease in the UK: A survey of British Society of Gastroenterology Inflammatory Bowel Disease Group members. Frontline Gastroenterol. 2022, 13, 471–476. [Google Scholar] [CrossRef]
- Innocenti, T.; Rocco, C.; Scarallo, L.; Lionetti, P.; Galli, A.; Dragoni, G. Systematic Review of Available Intestinal Ultrasound Scores for Inflammatory Bowel Disease and Update on Validation Studies. Inflamm. Bowel Dis. 2025, 31, 3194–3212. [Google Scholar] [CrossRef]
- Allocca, M.; Dell’Avalle, C.; Furfaro, F.; Zilli, A.; D’Amico, F.; Peyrin-Biroulet, L.; Fiorino, G.; Danese, S. Early Intestinal Ultrasound Predicts Long-Term Endoscopic Response to Biologics in Ulcerative Colitis. J. Crohn’s Colitis 2023, 17, 1579–1586. [Google Scholar] [CrossRef]
- Ripollés, T.; Paredes, J.M.; Martínez-Pérez, M.J.; Rimola, J.; Jauregui-Amezaga, A.; Bouzas, R.; Martin, G.; Moreno-Osset, E. Ultrasonographic Changes at 12 Weeks of Anti-TNF Drugs Predict 1-year Sonographic Response and Clinical Outcome in Crohn’s Disease: A Multicenter Study. Inflamm. Bowel Dis. 2016, 22, 2465–2473. [Google Scholar] [CrossRef]
- St-Pierre, J.; Delisle, M.; Kheirkhahrahimabadi, H.; Goodsall, T.M.; Bryant, R.V.; Christensen, B.; Vaughan, R.; Al-Ani, A.; Ingram, R.J.M.; Heatherington, J.; et al. Bedside Intestinal Ultrasound Performed in an Inflammatory Bowel Disease Urgent Assessment Clinic Improves Clinical Decision-Making and Resource Utilization. Crohns Colitis 360 2023, 5, otad050. [Google Scholar] [CrossRef]
- Schroeder, K.W.; Tremaine, W.J.; Ilstrup, D.M. Coated oral 5-aminosalicylic acid therapy for mildly to moderately active ulcerative colitis. A randomized study. N. Engl. J. Med. 1987, 317, 1625–1629. [Google Scholar] [CrossRef]
- Peyrin-Biroulet, L.; Sandborn, W.; Sands, B.E.; Reinisch, W.; Bemelman, W.; Bryant, R.V.; D’Haens, G.; Dotan, I.; Dubinsky, M.; Feagan, B.; et al. Selecting Therapeutic Targets in Inflammatory Bowel Disease (STRIDE): Determining Therapeutic Goals for Treat-to-Target. Off. J. Am. Coll. Gastroenterol.|ACG 2015, 110, 1324–1338. [Google Scholar] [CrossRef]
- Vuitton, L.; Peyrin-Biroulet, L.; Colombel, J.F.; Pariente, B.; Pineton de Chambrun, G.; Walsh, A.J.; Panes, J.; Travis, S.P.L.; Mary, J.Y.; Marteau, P. Defining endoscopic response and remission in ulcerative colitis clinical trials: An international consensus. Aliment. Pharmacol. Ther. 2017, 45, 801–813. [Google Scholar] [CrossRef]
- Mary, J.Y.; Modigliani, R. Development and validation of an endoscopic index of the severity for Crohn’s disease: A prospective multicentre study. Groupe d’Etudes Thérapeutiques des Affections Inflammatoires du Tube Digestif (GETAID). Gut 1989, 30, 983–989. [Google Scholar] [CrossRef]
- Daperno, M.; D’Haens, G.; Van Assche, G.; Baert, F.; Bulois, P.; Maunoury, V.; Sostegni, R.; Rocca, R.; Pera, A.; Gevers, A.; et al. Development and validation of a new, simplified endoscopic activity score for Crohn’s disease: The SES-CD. Gastrointest. Endosc. 2004, 60, 505–512. [Google Scholar] [CrossRef]
- Bryant, R.V.; Winer, S.; Spl, T.; Riddell, R.H. Systematic review: Histological remission in inflammatory bowel disease. Is ‘complete’ remission the new treatment paradigm? An IOIBD initiative. J. Crohn’s Colitis 2014, 8, 1582–1597. [Google Scholar] [CrossRef] [PubMed]
- de Jong, M.J.; Huibregtse, R.; Masclee, A.A.M.; Jonkers, D.; Pierik, M.J. Patient-Reported Outcome Measures for Use in Clinical Trials and Clinical Practice in Inflammatory Bowel Diseases: A Systematic Review. Clin. Gastroenterol. Hepatol. 2018, 16, 648–663.e3. [Google Scholar] [CrossRef] [PubMed]
- Gracie, D.J.; Williams, C.J.; Sood, R.; Mumtaz, S.; Bholah, M.H.; Hamlin, P.J.; Ford, A.C. Poor Correlation Between Clinical Disease Activity and Mucosal Inflammation, and the Role of Psychological Comorbidity, in Inflammatory Bowel Disease. Am. J. Gastroenterol. 2016, 111, 541–551. [Google Scholar] [CrossRef]
- Marrie, R.A.; Graff, L.A.; Fisk, J.D.; Patten, S.B.; Bernstein, C.N. The Relationship Between Symptoms of Depression and Anxiety and Disease Activity in IBD Over Time. Inflamm. Bowel Dis. 2021, 27, 1285–1293. [Google Scholar] [CrossRef]
- Gebeyehu, G.G.; Taylor, F.; Dobson, L.; Cummings, J.R.F.; Bloom, S.; Kennedy, N.A.; Christiansen, P.; Bodger, K. Validation of the IBD-Control Questionnaire across different sociodemographic and clinical subgroups: Secondary analysis of a nationwide electronic survey. J. Crohn’s Colitis 2024, 18, 275–285. [Google Scholar] [CrossRef] [PubMed]
- Fairbrass, K.M.; Costantino, S.J.; Gracie, D.J.; Ford, A.C. Prevalence of irritable bowel syndrome-type symptoms in patients with inflammatory bowel disease in remission: A systematic review and meta-analysis. Lancet Gastroenterol. Hepatol. 2020, 5, 1053–1062. [Google Scholar] [CrossRef]
- Vivinus-Nébot, M.; Frin-Mathy, G.; Bzioueche, H.; Dainese, R.; Bernard, G.; Anty, R.; Filippi, J.; Saint-Paul, M.C.; Tulic, M.K.; Verhasselt, V.; et al. Functional bowel symptoms in quiescent inflammatory bowel diseases: Role of epithelial barrier disruption and low-grade inflammation. Gut 2014, 63, 744–752. [Google Scholar] [CrossRef]
- Katinios, G.; Casado-Bedmar, M.; Walter, S.A.; Vicario, M.; González-Castro, A.M.; Bednarska, O.; Söderholm, J.D.; Hjortswang, H.; Keita, A.V. Increased Colonic Epithelial Permeability and Mucosal Eosinophilia in Ulcerative Colitis in Remission Compared with Irritable Bowel Syndrome and Health. Inflamm. Bowel Dis. 2020, 26, 974–984. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, M.; Pu, A.; Jencks, K.; Bishu, S.; Higgins, P.; Chey, W.D.; Rao, K.; Lee, A. Predictors of irritable bowel syndrome-like symptoms in quiescent inflammatory bowel disease. Neurogastroenterol. Motil. 2024, 36, e14809. [Google Scholar] [CrossRef] [PubMed]
- Butt, M.F.; Corsetti, M. Editorial: Rebuilding Rome-Revising Diagnostic Criteria for Irritable Bowel Syndrome. Aliment. Pharmacol. Ther. 2025, 61, 392–393. [Google Scholar] [CrossRef]
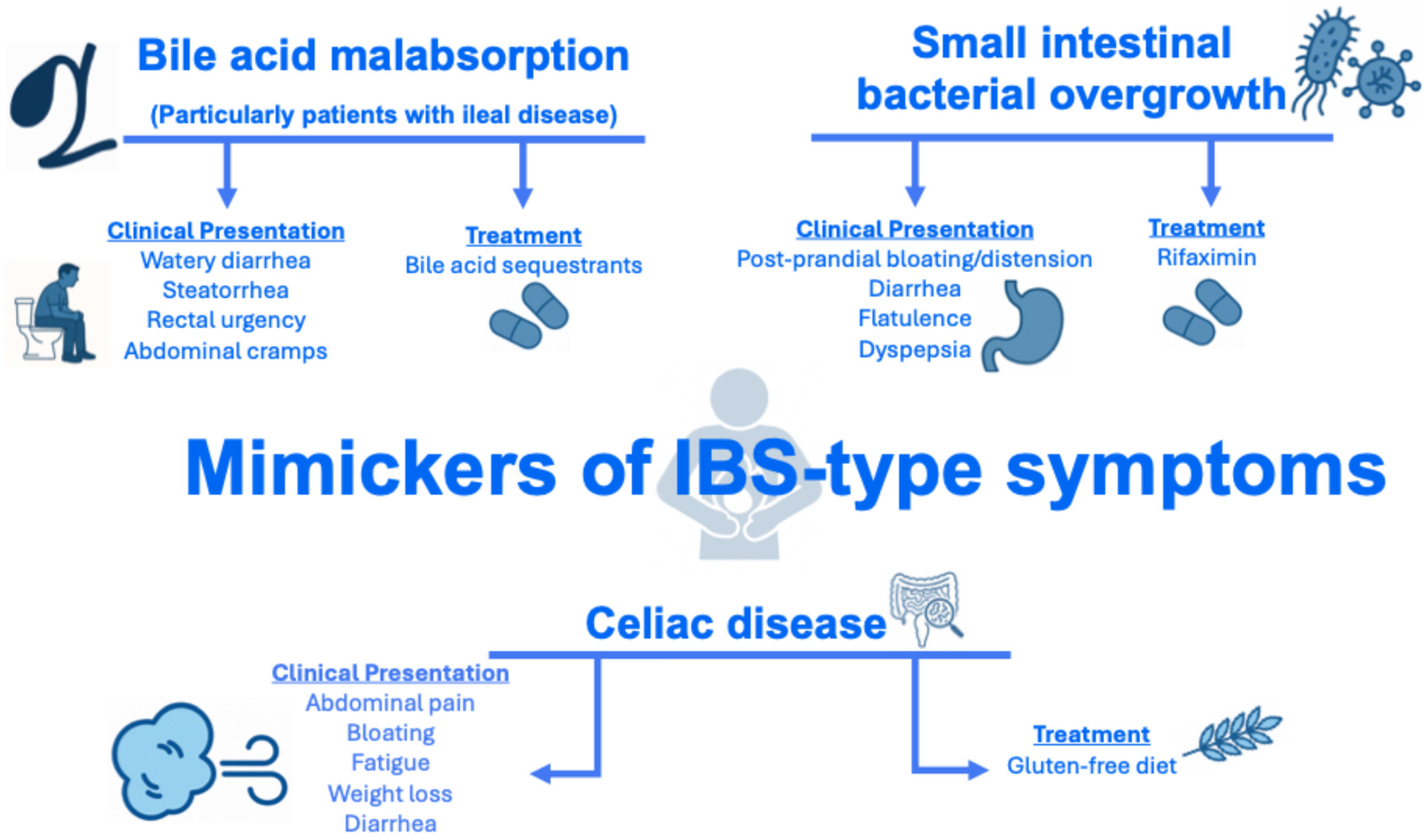
- Shah, A.; Morrison, M.; Burger, D.; Martin, N.; Rich, J.; Jones, M.; Koloski, N.; Walker, M.M.; Talley, N.J.; Holtmann, G.J. Systematic review with meta-analysis: The prevalence of small intestinal bacterial overgrowth in inflammatory bowel disease. Aliment. Pharmacol. Ther. 2019, 49, 624–635. [Google Scholar] [CrossRef]
- Vítek, L. Bile acid malabsorption in inflammatory bowel disease. Inflamm. Bowel Dis. 2015, 21, 476–483. [Google Scholar] [CrossRef]
- Drossman, D.A. Functional Gastrointestinal Disorders: History, Pathophysiology, Clinical Features and Rome IV. Gastroenterology 2016, 150, 1262–1279.e2. [Google Scholar] [CrossRef] [PubMed]
- Reddy, S.N.; Bazzocchi, G.; Chan, S.; Akashi, K.; Villanueva-Meyer, J.; Yanni, G.; Mena, I.; Snape, W.J., Jr. Colonic motility and transit in health and ulcerative colitis. Gastroenterology 1991, 101, 1289–1297. [Google Scholar] [CrossRef]
- Rao, S.S.; Read, N.W.; Stobart, J.A.; Haynes, W.G.; Benjamin, S.; Holdsworth, C.D. Anorectal contractility under basal conditions and during rectal infusion of saline in ulcerative colitis. Gut 1988, 29, 769–777. [Google Scholar] [CrossRef]
- Rao, S.S.; Read, N.W.; Davison, P.A.; Bannister, J.J.; Holdsworth, C.D. Anorectal sensitivity and responses to rectal distention in patients with ulcerative colitis. Gastroenterology 1987, 93, 1270–1275. [Google Scholar] [CrossRef]
- Pittayanon, R.; Lau, J.T.; Yuan, Y.; Leontiadis, G.I.; Tse, F.; Surette, M.; Moayyedi, P. Gut Microbiota in Patients with Irritable Bowel Syndrome—A Systematic Review. Gastroenterology 2019, 157, 97–108. [Google Scholar] [CrossRef]
- Iliev, I.D.; Ananthakrishnan, A.N.; Guo, C.-J. Microbiota in inflammatory bowel disease: Mechanisms of disease and therapeutic opportunities. Nat. Rev. Microbiol. 2025, 23, 509–524. [Google Scholar] [CrossRef]
- Vila, A.V.; Imhann, F.; Collij, V.; Jankipersadsing, S.A.; Gurry, T.; Mujagic, Z.; Kurilshikov, A.; Bonder, M.J.; Jiang, X.; Tigchelaar, E.F.; et al. Gut microbiota composition and functional changes in inflammatory bowel disease and irritable bowel syndrome. Sci. Transl. Med. 2018, 10, eaap8914. [Google Scholar] [CrossRef]
- Mayer, E.A.; Ryu, H.J.; Bhatt, R.R. The neurobiology of irritable bowel syndrome. Mol. Psychiatry 2023, 28, 1451–1465. [Google Scholar] [CrossRef]
- De Giorgio, R.; Guerrini, S.; Barbara, G.; Stanghellini, V.; De Ponti, F.; Corinaldesi, R.; Moses, P.L.; Sharkey, K.A.; Mawe, G.M. Inflammatory neuropathies of the enteric nervous system. Gastroenterology 2004, 126, 1872–1883. [Google Scholar] [CrossRef]
- Le Berre, C.; Naveilhan, P.; Rolli-Derkinderen, M. Enteric glia at center stage of inflammatory bowel disease. Neurosci. Lett. 2023, 809, 137315. [Google Scholar] [CrossRef]
- Morales-Soto, W.; Gulbransen, B.D. Enteric Glia: A New Player in Abdominal Pain. Cell Mol. Gastroenterol. Hepatol. 2019, 7, 433–445. [Google Scholar] [CrossRef]
- Schneider, K.M.; Blank, N.; Alvarez, Y.; Thum, K.; Lundgren, P.; Litichevskiy, L.; Sleeman, M.; Bahnsen, K.; Kim, J.; Kardo, S.; et al. The enteric nervous system relays psychological stress to intestinal inflammation. Cell 2023, 186, 2823–2838.e20. [Google Scholar] [CrossRef] [PubMed]
- Spiegel, B.M.; Farid, M.; Esrailian, E.; Talley, J.; Chang, L. Is irritable bowel syndrome a diagnosis of exclusion?: A survey of primary care providers, gastroenterologists, and IBS experts. Am. J. Gastroenterol. 2010, 105, 848–858. [Google Scholar] [CrossRef] [PubMed]
- Lau, M.S.Y.; Ford, A.C. Do Lay People Accept a Positive Diagnosis of Irritable Bowel Syndrome? Gastroenterology 2015, 149, 252–253. [Google Scholar] [CrossRef]
- Daly, M.; Zarate-Lopez, N. Functional gastrointestinal disorders: History taking skills in practice. Clin. Med. 2021, 21, e480–e486. [Google Scholar] [CrossRef]
- Butt, M.F. Approaches to building rapport with patients. Clin. Med. 2021, 21, e662–e663. [Google Scholar] [CrossRef]
- Ahmad, Z.; Barakat, R.; Ghous, M.A.; Butt, M.F. Patient voice at scale: Artificial intelligence-assisted qualitative analysis of patient-clinician rapport in public social media. Panminerva Med. 2025. [Google Scholar] [CrossRef]
- Berrill, J.W.; Sadlier, M.; Hood, K.; Green, J.T. Mindfulness-based therapy for inflammatory bowel disease patients with functional abdominal symptoms or high perceived stress levels. J. Crohns Colitis 2014, 8, 945–955. [Google Scholar] [CrossRef] [PubMed]
- Hoekman, D.R.; Vlieger, A.M.; Stokkers, P.C.; Mahhmod, N.; Rietdijk, S.; de Boer, N.K.; de Meij, T.G.; Frankenhuis, C.; D’Haens, G.R.; Benninga, M.A. Hypnotherapy for Irritable Bowel Syndrome-Type Symptoms in Patients with Quiescent Inflammatory Bowel Disease: A Randomized, Controlled Trial. J. Crohn’s Colitis 2020, 15, 1106–1113. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, N.; Ankersen, D.V.; Felding, M.; Wachmann, H.; Végh, Z.; Molzen, L.; Burisch, J.; Andersen, J.R.; Munkholm, P. Low-FODMAP diet reduces irritable bowel symptoms in patients with inflammatory bowel disease. World J. Gastroenterol. 2017, 23, 3356–3366. [Google Scholar] [CrossRef]
- Cox, S.R.; Prince, A.C.; Myers, C.E.; Irving, P.M.; Lindsay, J.O.; Lomer, M.C.; Whelan, K. Fermentable Carbohydrates [FODMAPs] Exacerbate Functional Gastrointestinal Symptoms in Patients with Inflammatory Bowel Disease: A Randomised, Double-blind, Placebo-controlled, Cross-over, Re-challenge Trial. J. Crohns Colitis 2017, 11, 1420–1429. [Google Scholar] [CrossRef]
- Bodini, G.; Zanella, C.; Crespi, M.; Lo Pumo, S.; Demarzo, M.G.; Savarino, E.; Savarino, V.; Giannini, E.G. A randomized, 6-wk trial of a low FODMAP diet in patients with inflammatory bowel disease. Nutrition 2019, 67–68, 110542. [Google Scholar] [CrossRef] [PubMed]
- Cox, S.R.; Lindsay, J.O.; Fromentin, S.; Stagg, A.J.; McCarthy, N.E.; Galleron, N.; Ibraim, S.B.; Roume, H.; Levenez, F.; Pons, N.; et al. Effects of Low FODMAP Diet on Symptoms, Fecal Microbiome, and Markers of Inflammation in Patients with Quiescent Inflammatory Bowel Disease in a Randomized Trial. Gastroenterology 2020, 158, 176–188.e7. [Google Scholar] [CrossRef]
- Lee, J.; Park, S.B.; Kim, H.W.; Lee, H.S.; Jee, S.R.; Lee, J.H.; Kim, T.O. Clinical Efficacy of Probiotic Therapy on Bowel-Related Symptoms in Patients with Ulcerative Colitis during Endoscopic Remission: An Observational Study. Gastroenterol. Res. Pract. 2022, 2022, 9872230. [Google Scholar] [CrossRef]
- Tomita, T.; Fukui, H.; Okugawa, T.; Nakanishi, T.; Mieno, M.; Nakai, K.; Eda, H.; Kitayama, Y.; Oshima, T.; Shinzaki, S.; et al. Effect of Bifidobacterium bifidum G9-1 on the Intestinal Environment and Diarrhea-Predominant Irritable Bowel Syndrome (IBS-D)-like Symptoms in Patients with Quiescent Crohn’s Disease: A Prospective Pilot Study. J. Clin. Med. 2023, 12, 3368. [Google Scholar] [CrossRef]
- Tomita, T.; Fukui, H.; Morishita, D.; Mori, S.; Oshima, T.; Shinzaki, S.; Miwa, H. Efficacy of Serotonin Type 3 Receptor Antagonist Ramosetron on Diarrhea-Predominant Irritable Bowel Syndrome (IBS-D)-Like Symptoms in Patients with Quiescent Inflammatory Bowel Disease: A Randomized, Double-Blind, Placebo-Controlled Trial. J. Clin. Med. 2022, 11, 6882. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, Y.; Kanazawa, M.; Fukudo, S.; Drossman, D.A. Biopsychosocial model of irritable bowel syndrome. J. Neurogastroenterol. Motil. 2011, 17, 131–139. [Google Scholar] [CrossRef]
- Barberio, B.; Zamani, M.; Black, C.J.; Savarino, E.V.; Ford, A.C. Prevalence of symptoms of anxiety and depression in patients with inflammatory bowel disease: A systematic review and meta-analysis. Lancet Gastroenterol. Hepatol. 2021, 6, 359–370. [Google Scholar] [CrossRef]
- Engelmann-Kewitz, M.; Khwaja, I.; Takahashi, K.; Parkes, M.; Norton, C.; Hart, A.; Bulmer, D.; Aziz, Q. Factors associated with chronic abdominal pain in patients with inflammatory bowel disease in remission: A pilot cross-sectional study. Neurogastroenterol. Motil. 2024, 36, e14881. [Google Scholar] [CrossRef]
- Janssen, L.M.; Ardabili, A.R.; Romberg-Camps, M.J.L.; Winkens, B.; van den Broek, R.J.; Hulst, J.; Verwijs, H.J.A.; Keszthelyi, D.; Jonkers, D.M.A.E.; van Bodegraven, A.A.; et al. Abdominal pain in patients with inflammatory bowel disease in remission: A prospective study on contributing factors. Aliment. Pharmacol. Ther. 2023, 58, 1041–1051. [Google Scholar] [CrossRef]
- Wileman, V.; Chilcot, J.; Norton, C.; Hart, A.; Miller, L.; Stagg, I.; Seaton, N.; Pollok, R.; Aziz, Q.; Moss-Morris, R. Modifiable Psychological Factors are Associated with Clusters of Pain, Fatigue, Fecal Incontinence, and Irritable Bowel Syndrome-Type Symptoms in Inflammatory Bowel Disease: A Latent Profile Analysis. J. Crohn’s Colitis 2025, 19, jjae183. [Google Scholar] [CrossRef] [PubMed]
- Keefer, L.; Ballou, S.K.; Drossman, D.A.; Ringstrom, G.; Elsenbruch, S.; Ljótsson, B. A Rome Working Team Report on Brain-Gut Behavior Therapies for Disorders of Gut-Brain Interaction. Gastroenterology 2022, 162, 300–315. [Google Scholar] [CrossRef]
- Black, C.J.; Thakur, E.R.; Houghton, L.A.; Quigley, E.M.M.; Moayyedi, P.; Ford, A.C. Efficacy of psychological therapies for irritable bowel syndrome: Systematic review and network meta-analysis. Gut 2020, 69, 1441–1451. [Google Scholar] [CrossRef] [PubMed]
- Goodoory, V.C.; Khasawneh, M.; Thakur, E.R.; Everitt, H.A.; Gudleski, G.D.; Lackner, J.M.; Moss-Morris, R.; Simren, M.; Vasant, D.H.; Moayyedi, P.; et al. Effect of Brain-Gut Behavioral Treatments on Abdominal Pain in Irritable Bowel Syndrome: Systematic Review and Network Meta-Analysis. Gastroenterology 2024, 167, 934–943.e5. [Google Scholar] [CrossRef]
- Vasant, D.H.; Paine, P.A.; Black, C.J.; Houghton, L.A.; Everitt, H.A.; Corsetti, M.; Agrawal, A.; Aziz, I.; Farmer, A.D.; Eugenicos, M.P.; et al. British Society of Gastroenterology guidelines on the management of irritable bowel syndrome. Gut 2021, 70, 1214. [Google Scholar] [CrossRef]
- Butt, M.F.; Bush, D.; Aliyu, A.; Darie, A.; Mohanan, A.; Sibelli, A.; Card, T.; Corsetti, M. O24 Interim analysis of outcomes for a digital prescription mobile application for adults with irritable bowel syndrome: A prospective interventional study. Gut 2025, 74, A17. [Google Scholar]
- Ford, A.C.; Wright-Hughes, A.; Alderson, S.L.; Ow, P.L.; Ridd, M.J.; Foy, R.; Bianco, G.; Bishop, F.L.; Chaddock, M.; Cook, H.; et al. Amitriptyline at Low-Dose and Titrated for Irritable Bowel Syndrome as Second-Line Treatment in primary care (ATLANTIS): A randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 2023, 402, 1773–1785. [Google Scholar] [CrossRef] [PubMed]
- Iskandar, H.N.; Cassell, B.; Kanuri, N.; Gyawali, C.P.; Gutierrez, A.; Dassopoulos, T.; Ciorba, M.A.; Sayuk, G.S. Tricyclic antidepressants for management of residual symptoms in inflammatory bowel disease. J. Clin. Gastroenterol. 2014, 48, 423–429. [Google Scholar] [CrossRef] [PubMed]
- Drossman, D.A.; Tack, J.; Ford, A.C.; Szigethy, E.; Törnblom, H.; Van Oudenhove, L. Neuromodulators for Functional Gastrointestinal Disorders (Disorders of Gut-Brain Interaction): A Rome Foundation Working Team Report. Gastroenterology 2018, 154, 1140–1171.e1. [Google Scholar] [CrossRef]
- Coates, M.D.; Johri, A.; Gorrepati, V.S.; Maheshwari, P.; Dalessio, S.; Walter, V.; Stuart, A.; Koltun, W.; Bernasko, N.; Tinsley, A.; et al. Abdominal pain in quiescent inflammatory bowel disease. Int. J. Colorectal Dis. 2021, 36, 93–102. [Google Scholar] [CrossRef]
- Hart, A.; Miller, L.; Hamborg, T.; Stagg, I.; McGuinness, S.; Wileman, V.; Tzorovili, E.; Mihaylova, B.; Roukas, C.; Aziz, Q.; et al. DOP59 What is the relationship between fatigue, pain and urgency in people with inflammatory bowel disease? Results of the IBD-BOOST survey in 8486 participants. J. Crohn’s Colitis 2023, 17, i130–i132. [Google Scholar] [CrossRef]
- Dilmaghani, S.; Dunleavy, K.; Fehlmann, T.; Raffals, L.; Chedid, V. P1175 Abdominal Pain is Associated with Poor Quality of Life in Quiescent Inflammatory Bowel Disease: A Cross-sectional Study of the SPARC Inflammatory Bowel Disease Cohort. J. Crohn’s Colitis 2024, 18, i2082–i2084. [Google Scholar] [CrossRef]
- van Gils, T.; Törnblom, H.; Hreinsson, J.P.; Jonefjäll, B.; Strid, H.; Simrén, M. Factors Associated with Abdominal Pain in Patients With Active and Quiescent Ulcerative Colitis: A Multicohort Study. Aliment. Pharmacol. Ther. 2025, 61, 268–277. [Google Scholar] [CrossRef]
- Sinopoulou, V.; Gordon, M.; Akobeng, A.K.; Gasparetto, M.; Sammaan, M.; Vasiliou, J.; Dovey, T.M. Interventions for the management of abdominal pain in Crohn’s disease and inflammatory bowel disease. Cochrane Database Syst. Rev. 2021, 11, Cd013531. [Google Scholar]
- Sinopoulou, V.; Gordon, M.; Dovey, T.M.; Akobeng, A.K. Interventions for the management of abdominal pain in ulcerative colitis. Cochrane Database Syst. Rev. 2021, 7, Cd013589. [Google Scholar]
- Norton, C.; Czuber-Dochan, W.; Artom, M.; Sweeney, L.; Hart, A. Systematic review: Interventions for abdominal pain management in inflammatory bowel disease. Aliment. Pharmacol. Ther. 2017, 46, 115–125. [Google Scholar] [CrossRef]
- Norton, C.; Syred, J.; Kerry, S.; Artom, M.; Sweeney, L.; Hart, A.; Czuber-Dochan, W.; Taylor, S.J.C.; Mihaylova, B.; Roukas, C.; et al. Supported online self-management versus care as usual for symptoms of fatigue, pain and urgency/incontinence in adults with inflammatory bowel disease (IBD-BOOST): Study protocol for a randomised controlled trial. Trials 2021, 22, 516. [Google Scholar] [CrossRef] [PubMed]
- Norton, C.; Moss-Morris, R.; Hart, A.; Cléirigh-Büttner, F.; Hamborg, T.; Stagg, I.; Aziz, Q.; Czuber-Dochan, W.; Dibley, L.; Mihaylova, B.; et al. O28 IBD-BOOST, a digital cognitive behavioural self-management programme for fatigue, and/or pain, and/or faecal incontinence in IBD: Randomised controlled trial. Gut 2024, 73, A16. [Google Scholar]
- Cuffe, M.S.; Staudacher, H.M.; Aziz, I.; Adame, E.C.; Krieger-Grubel, C.; Madrid, A.M.; Ohlsson, B.; Black, C.J.; Ford, A.C. Efficacy of dietary interventions in irritable bowel syndrome: A systematic review and network meta-analysis. Lancet Gastroenterol. Hepatol. 2025, 10, 520–536. [Google Scholar] [CrossRef] [PubMed]
- Ville, A.; McRae, R.; Nomchong, J.; Reidlinger, D.P.; Davidson, A.R.; Staudacher, H.M.; Albarqouni, L. Effects of a Low FODMAP Diet in Inflammatory Bowel Disease and Patient Experiences: A Mixed Methods Systematic Literature Review and Meta-Analysis. J. Hum. Nutr. Diet. 2025, 38, e70106. [Google Scholar] [CrossRef]
- Zhan, Y.L.; Zhan, Y.A.; Dai, S.X. Is a low FODMAP diet beneficial for patients with inflammatory bowel disease? A meta-analysis and systematic review. Clin. Nutr. 2018, 37, 123–129. [Google Scholar] [CrossRef] [PubMed]
- Peng, Z.; Yi, J.; Liu, X. A Low-FODMAP Diet Provides Benefits for Functional Gastrointestinal Symptoms but Not for Improving Stool Consistency and Mucosal Inflammation in IBD: A Systematic Review and Meta-Analysis. Nutrients 2022, 14, 2072. [Google Scholar] [CrossRef]
- Więcek, M.; Panufnik, P.; Kaniewska, M.; Lewandowski, K.; Rydzewska, G. Low-FODMAP Diet for the Management of Irritable Bowel Syndrome in Remission of IBD. Nutrients 2022, 14, 4562. [Google Scholar] [CrossRef]
- Yelencich, E.; Truong, E.; Widaman, A.M.; Pignotti, G.; Yang, L.; Jeon, Y.; Weber, A.T.; Shah, R.; Smith, J.; Sauk, J.S.; et al. Avoidant Restrictive Food Intake Disorder Prevalent Among Patients with Inflammatory Bowel Disease. Clin. Gastroenterol. Hepatol. 2022, 20, 1282–1289.e1. [Google Scholar] [CrossRef] [PubMed]
- Bamidele, J.O.; Brownlow, G.M.; Flack, R.M.; Buckle, R.L.; Shaw, C.C.; Shiha, M.G.; Aziz, I. The Mediterranean Diet for Irritable Bowel Syndrome. Ann. Intern. Med. 2025, 178, 1709–1717. [Google Scholar] [CrossRef]
- Nunan, D.; Cai, T.; Gardener, A.D.; Ordóñez-Mena, J.M.; Roberts, N.W.; Thomas, E.T.; Mahtani, K.R. Physical activity for treatment of irritable bowel syndrome. Cochrane Database Syst. Rev. 2022, 6, Cd011497. [Google Scholar] [CrossRef]
- Colombel, J.F.; Shin, A.; Gibson, P.R. AGA Clinical Practice Update on Functional Gastrointestinal Symptoms in Patients with Inflammatory Bowel Disease: Expert Review. Clin. Gastroenterol. Hepatol. 2019, 17, 380–390.e1. [Google Scholar] [CrossRef]
- Busse, J.W.; Wang, L.; Kamaleldin, M.; Craigie, S.; Riva, J.J.; Montoya, L.; Mulla, S.M.; Lopes, L.C.; Vogel, N.; Chen, E.; et al. Opioids for Chronic Noncancer Pain: A Systematic Review and Meta-analysis. Jama 2018, 320, 2448–2460. [Google Scholar] [CrossRef]
- Coates, M.D.; Seth, N.; Clarke, K.; Abdul-Baki, H.; Mahoney, N.; Walter, V.; Regueiro, M.D.; Ramos-Rivers, C.; Koutroubakis, I.E.; Bielefeldt, K.; et al. Opioid Analgesics Do Not Improve Abdominal Pain or Quality of Life in Crohn’s Disease. Dig. Dis. Sci. 2020, 65, 2379–2387. [Google Scholar] [CrossRef]
- Butt, M.F.; Goodoory, V.C.; Ng, C.E.; Black, C.J.; Ford, A.C.; Corsetti, M.; Paine, P. Prevalence of Opioid Use and Associated Healthcare Outcomes in Rome IV Irritable Bowel Syndrome in the United Kingdom. Aliment. Pharmacol. Ther. 2025. [Google Scholar] [CrossRef]
- Butt, M.F.; Cefalo, F.; Sbarigia, C.; Dhali, A.; Corsetti, M. Impact of Opioid and Cannabis Use on Low-Dose Amitriptyline Efficacy in Cyclical Vomiting Syndrome: A Real-World Study in the United Kingdom. Neurogastroenterol. Motil. 2025, 37, e70007. [Google Scholar] [CrossRef] [PubMed]
- Butt, M.F.; Isherwood, G.; Lewis-Lawson, T.; Sbarigia, C.; Lambiase, C.; Aburumman, R.N.M.; Dhali, A.; Bush, D.; Card, T.; Corsetti, M. Clinical Characteristics and Outcomes of Patients with Rome IV Functional Dyspepsia Who Consume Opioids: A Real-World Study. Neurogastroenterol. Motil. 2025, 37, e15019. [Google Scholar] [CrossRef]
- Farmer, A.D.; Gallagher, J.; Bruckner-Holt, C.; Aziz, Q. Narcotic bowel syndrome. Lancet Gastroenterol. Hepatol. 2017, 2, 361–368. [Google Scholar] [CrossRef] [PubMed]
- Khasawneh, M.; Mokhtare, M.; Moayyedi, P.; Black, C.J.; Ford, A.C. Efficacy of gut-brain neuromodulators in irritable bowel syndrome: An updated systematic review and meta-analysis. Lancet Gastroenterol. Hepatol. 2025, 10, 537–549. [Google Scholar] [CrossRef]
- Hanna-Jairala, I.; Drossman, D.A. Central Neuromodulators in Irritable Bowel Syndrome: Why, How, and When. Am. J. Gastroenterol. 2024, 119, 1272–1284. [Google Scholar] [CrossRef] [PubMed]
- Khalif, I.L.; Quigley, E.M.; Makarchuk, P.A.; Golovenko, O.V.; Podmarenkova, L.F.; Dzhanayev, Y.A. Interactions between symptoms and motor and visceral sensory responses of irritable bowel syndrome patients to spasmolytics (antispasmodics). J. Gastrointestin. Liver Dis. 2009, 18, 17–22. [Google Scholar]
- Ruepert, L.; Quartero, A.O.; de Wit, N.J.; van der Heijden, G.J.; Rubin, G.; Muris, J.W. Bulking agents, antispasmodics and antidepressants for the treatment of irritable bowel syndrome. Cochrane Database Syst. Rev. 2011, 2011, Cd003460. [Google Scholar] [CrossRef]
- Black, C.J.; Yuan, Y.; Selinger, C.P.; Camilleri, M.; Quigley, E.M.M.; Moayyedi, P.; Ford, A.C. Efficacy of soluble fibre, antispasmodic drugs, and gut-brain neuromodulators in irritable bowel syndrome: A systematic review and network meta-analysis. Lancet Gastroenterol. Hepatol. 2020, 5, 117–131. [Google Scholar] [CrossRef]
- Miller, C.; Emmanuel, A.; Zarate-Lopez, N.; Taylor, S.; Bloom, S. Constipation in ulcerative colitis: Pathophysiology and practical management. Frontline Gastroenterol. 2021, 12, 493–499. [Google Scholar] [CrossRef] [PubMed]
- James, S.L.; van Langenberg, D.R.; Taylor, K.M.; Gibson, P.R. Characterization of ulcerative colitis-associated constipation syndrome (proximal constipation). JGH Open 2018, 2, 217–222. [Google Scholar] [CrossRef]
- Al Snih, G.M.; Bailey, K.R.; Oblizajek, N.R.; Bharucha, A.E. Symptoms of Constipation: Relationship Between Questionnaires and Diaries and Impact on Quality of Life. Clin Gastroenterol. Hepatol. 2025. [Google Scholar] [CrossRef] [PubMed]
- Bassotti, G.; Bologna, S.; Antonelli, E. Constipation in Ulcerative Colitis: An Underestimated Problem. J. Clin. Med. 2025, 14, 5428. [Google Scholar] [CrossRef]
- Dimidi, E.; van der Schoot, A.; Barrett, K.; Farmer, A.D.; Lomer, M.C.; Scott, S.M.; Whelan, K. British Dietetic Association Guidelines for the Dietary Management of Chronic Constipation in Adults. J. Hum. Nutr. Diet. 2025, 38, e70133. [Google Scholar] [CrossRef]
- Gearry, R.B.; Irving, P.M.; Barrett, J.S.; Nathan, D.M.; Shepherd, S.J.; Gibson, P.R. Reduction of dietary poorly absorbed short-chain carbohydrates (FODMAPs) improves abdominal symptoms in patients with inflammatory bowel disease-a pilot study. J. Crohns Colitis 2009, 3, 8–14. [Google Scholar] [CrossRef]
- Yurtdaş, G.; Acar-Tek, N.; Akbulut, G.; Cemali, Ö.; Arslan, N.; Beyaz Coşkun, A.; Zengin, F.H. Risk Factors for Constipation in Adults: A Cross-Sectional Study. J. Am. Coll. Nutr. 2020, 39, 713–719. [Google Scholar] [CrossRef]
- Kim, Y.J.; Lee, S.G.; Lee, J.S.; Choi, Y.J.; Son, C.G. Comparative characteristics of fatigue in irritable bowel syndrome and inflammatory bowel disease: A systematic review and meta-analysis. J. Psychosom. Res. 2024, 177, 111589. [Google Scholar] [CrossRef]
- Chochinov, S.; Dolovich, C.; Ly, G.; Oketola, A.; Narvey, S.; Raman, M.; Webber, S.; Bernstein, C.N. A Population-Based Assessment of Physical Activity and Exercise in Persons with IBD. J. Clin. Gastroenterol. 2025. [Google Scholar] [CrossRef]
- Radford, S.J.; Janiszewski, H.; Moran, G.W. Physical activity and fatigue in adults with inflammatory bowel disease (IBD): A systematic review. Gastrointest. Nurs. 2019, 17, 16–21. [Google Scholar] [CrossRef]
- Bharucha, A.E.; Lacy, B.E. Mechanisms, Evaluation, and Management of Chronic Constipation. Gastroenterology 2020, 158, 1232–1249.e3. [Google Scholar] [CrossRef]
- Wald, A.; Bharucha, A.E.; Limketkai, B.; Malcolm, A.; Remes-Troche, J.M.; Whitehead, W.E.; Zutshi, M. ACG Clinical Guidelines: Management of Benign Anorectal Disorders. Am. J. Gastroenterol. 2021, 116, 1987–2008. [Google Scholar] [CrossRef]
- Rao, S.S.; Bharucha, A.E.; Chiarioni, G.; Felt-Bersma, R.; Knowles, C.; Malcolm, A.; Wald, A. Functional Anorectal Disorders. Gastroenterology 2016, 150, 1430–1442.e4. [Google Scholar] [CrossRef]
- Ratuapli, S.K.; Bharucha, A.E.; Noelting, J.; Harvey, D.M.; Zinsmeister, A.R. Phenotypic identification and classification of functional defecatory disorders using high-resolution anorectal manometry. Gastroenterology 2013, 144, 314–322.e2. [Google Scholar] [CrossRef]
- Rezaie, A.; Gu, P.; Kaplan, G.G.; Pimentel, M.; Al-Darmaki, A.K. Dyssynergic Defecation in Inflammatory Bowel Disease: A Systematic Review and Meta-Analysis. Inflamm. Bowel Dis. 2018, 24, 1065–1073. [Google Scholar] [CrossRef] [PubMed]
- Bharucha, A.E.; Rao, S.S. An update on anorectal disorders for gastroenterologists. Gastroenterology 2014, 146, 37–45.e2. [Google Scholar] [CrossRef] [PubMed]
- Chang, L.; Chey, W.D.; Imdad, A.; Almario, C.V.; Bharucha, A.E.; Diem, S.; Greer, K.B.; Hanson, B.; Harris, L.A.; Ko, C.; et al. American Gastroenterological Association-American College of Gastroenterology Clinical Practice Guideline: Pharmacological Management of Chronic Idiopathic Constipation. Gastroenterology 2023, 164, 1086–1106. [Google Scholar] [CrossRef]
- Serra, J.; Pohl, D.; Azpiroz, F.; Chiarioni, G.; Ducrotté, P.; Gourcerol, G.; Hungin, A.P.S.; Layer, P.; Mendive, J.M.; Pfeifer, J.; et al. European society of neurogastroenterology and motility guidelines on functional constipation in adults. Neurogastroenterol. Motil. 2020, 32, e13762. [Google Scholar] [CrossRef] [PubMed]
- Lacy, B.E. Review article: An analysis of safety profiles of treatments for diarrhoea-predominant irritable bowel syndrome. Aliment. Pharmacol. Ther. 2018, 48, 817–830. [Google Scholar] [CrossRef]
- Ayton, D.; Hoque, S. P0185 Prevalence of IBS-like symptoms in Ulcerative Colitis patients in clinical remission. J. Crohn’s Colitis 2025, 19, i588-i. [Google Scholar] [CrossRef]
- Samaha, C.; Dueker, J.; Johnston, E.; Schwartz, M.; Binion, D.; Duerr, R.; Ghaffari, A. S1310 Prevalence of Persistent Gastrointestinal Symptoms in IBD Patients with Endoscopically Quiescent Disease. Off. J. Am. Coll. Gastroenterol.|ACG 2024, 119, S937–S938. [Google Scholar] [CrossRef]
- Boland, K.; Bedrani, L.; Turpin, W.; Kabakchiev, B.; Stempak, J.; Borowski, K.; Nguyen, G.; Steinhart, A.H.; Smith, M.I.; Croitoru, K.; et al. Persistent Diarrhea in Patients with Crohn’s Disease After Mucosal Healing Is Associated with Lower Diversity of the Intestinal Microbiome and Increased Dysbiosis. Clin. Gastroenterol. Hepatol. 2021, 19, 296–304.e3. [Google Scholar] [CrossRef]
- Bassotti, G.; de Roberto, G.; Chistolini, F.; Sietchiping-Nzepa, F.; Morelli, O.; Morelli, A. Twenty-four-hour manometric study of colonic propulsive activity in patients with diarrhea due to inflammatory (ulcerative colitis) and non-inflammatory (irritable bowel syndrome) conditions. Int. J. Color. Dis. 2004, 19, 493–497. [Google Scholar] [CrossRef]
- Savarino, E.; Zingone, F.; Barberio, B.; Marasco, G.; Akyuz, F.; Akpinar, H.; Barboi, O.; Bodini, G.; Bor, S.; Chiarioni, G.; et al. Functional bowel disorders with diarrhoea: Clinical guidelines of the United European Gastroenterology and European Society for Neurogastroenterology and Motility. United Eur. Gastroenterol. J. 2022, 10, 556–584. [Google Scholar] [CrossRef] [PubMed]
- Cangemi, D.J.; Lacy, B.E. Management of irritable bowel syndrome with diarrhea: A review of nonpharmacological and pharmacological interventions. Therap. Adv. Gastroenterol. 2019, 12, 1756284819878950. [Google Scholar] [CrossRef]
- Lembo, A.; Sultan, S.; Chang, L.; Heidelbaugh, J.J.; Smalley, W.; Verne, G.N. AGA Clinical Practice Guideline on the Pharmacological Management of Irritable Bowel Syndrome with Diarrhea. Gastroenterology 2022, 163, 137–151. [Google Scholar] [CrossRef]
- Ford, A.C.; Harris, L.A.; Lacy, B.E.; Quigley, E.M.M.; Moayyedi, P. Systematic review with meta-analysis: The efficacy of prebiotics, probiotics, synbiotics and antibiotics in irritable bowel syndrome. Aliment. Pharmacol. Ther. 2018, 48, 1044–1060. [Google Scholar] [CrossRef]
- Lacy, B.E.; Pimentel, M.; Brenner, D.M.; Chey, W.D.; Keefer, L.A.; Long, M.D.; Moshiree, B. ACG Clinical Guideline: Management of Irritable Bowel Syndrome. Am. J. Gastroenterol. 2021, 116, 17–44. [Google Scholar] [CrossRef] [PubMed]
- Mayer, E.A.; Bradesi, S. Alosetron and irritable bowel syndrome. Expert. Opin. Pharmacother. 2003, 4, 2089–2098. [Google Scholar] [CrossRef] [PubMed]
- Gunn, D.; Topan, R.; Barnard, L.; Fried, R.; Holloway, I.; Brindle, R.; Corsetti, M.; Scott, M.; Farmer, A.; Kapur, K.; et al. Randomised, placebo-controlled trial and meta-analysis show benefit of ondansetron for irritable bowel syndrome with diarrhoea: The TRITON trial. Aliment. Pharmacol. Ther. 2023, 57, 1258–1271. [Google Scholar] [CrossRef] [PubMed]
- Sbarigia, C.; Lambiase, C.; Butt, M.F.; Aliyu, A.I.; Spiller, R.; Corsetti, M. Clinical Characteristics and Outcomes of Rome IV Diarrhea-Predominant Irritable Bowel Syndrome and Functional Diarrhea Prescribed with Ondansetron: A Real-World Study. Neurogastroenterol. Motil. 2025, 37, e70193. [Google Scholar] [CrossRef]
- Wright-Hughes, A.; Ow, P.L.; Alderson, S.L.; Ridd, M.J.; Foy, R.; Bishop, F.L.; Chaddock, M.; Fernandez, C.; Guthrie, E.A.; Muir, D.P.; et al. Predictors of response to low-dose amitriptyline for irritable bowel syndrome and efficacy and tolerability according to subtype: Post hoc analyses from the ATLANTIS trial. Gut 2025, 74, 728–739. [Google Scholar] [CrossRef]
- Decraecker, L.; De Looze, D.; Hirsch, D.P.; De Schepper, H.; Arts, J.; Caenepeel, P.; Bredenoord, A.J.; Kolkman, J.; Bellens, K.; Van Beek, K.; et al. Treatment of non-constipated irritable bowel syndrome with the histamine 1 receptor antagonist ebastine: A randomised, double-blind, placebo-controlled trial. Gut 2024, 73, 459–469. [Google Scholar] [CrossRef]
- Weerts, Z.Z.R.M.; Masclee, A.A.M.; Witteman, B.J.M.; Clemens, C.H.M.; Winkens, B.; Brouwers, J.R.B.J.; Frijlink, H.W.; Muris, J.W.M.; De Wit, N.J.; Essers, B.A.B.; et al. Efficacy and Safety of Peppermint Oil in a Randomized, Double-Blind Trial of Patients with Irritable Bowel Syndrome. Gastroenterology 2020, 158, 123–136. [Google Scholar] [CrossRef]
- Khunsriraksakul, C.; Ziegler, O.; Liu, D.; Kulaylat, A.S.; Coates, M.D. The Impact of Antispasmodic Use on Abdominal Pain and Opioid Use in Inflammatory Bowel Disease: A Population-Based Study. Aliment. Pharmacol. Ther. 2025, 61, 1944–1956. [Google Scholar] [CrossRef]
- Bharucha, A.E. Management of fecal incontinence. Gastroenterol. Hepatol. 2008, 4, 807–817. [Google Scholar]
- Kamal, N.; Motwani, K.; Wellington, J.; Wong, U.; Cross, R.K. Fecal Incontinence in Inflammatory Bowel Disease. Crohns Colitis 360 2021, 3, otab013. [Google Scholar] [CrossRef]
- Mack, I.; Hahn, H.; Gödel, C.; Enck, P.; Bharucha, A.E. Global Prevalence of Fecal Incontinence in Community-Dwelling Adults: A Systematic Review and Meta-analysis. Clin Gastroenterol. Hepatol. 2024, 22, 712–731.e8. [Google Scholar] [CrossRef] [PubMed]
- Bharucha, A.E.; Seide, B.M.; Zinsmeister, A.R.; Melton, L.J., 3rd. Relation of bowel habits to fecal incontinence in women. Am. J. Gastroenterol. 2008, 103, 1470–1475. [Google Scholar] [CrossRef]
- Butt, M.F.; Rao, S.S.C.; Whitehead, W.E.; Twist, S.; Lowry, A.C.; Wu, J.M.; Bailey, K.R.; Bharucha, A.E. Development and Validation of a Bowel Diary for Fecal Incontinence: Comparison with a Questionnaire. Neurogastroenterol. Motil. 2025, 37, e70080. [Google Scholar] [CrossRef]
- Butt, M.F.; Rao, S.S.C.; Meyer, I.; Chey, W.D.; Whitehead, W.E.; Richter, H.E.; Menees, S.B.; Busby-Whitehead, J.; Lamichhane, R.; Chen, J.; et al. Cluster Analysis of Fecal Incontinence Symptoms: Associations with Anorectal Physiology and Quality of Life. Clin. Gastroenterol. Hepatol. 2025. [Google Scholar] [CrossRef]
- Cleveland, N.K.; Rai, V.; El Jurdi, K.; Rao, S.S.; Giurcanu, M.C.; Rubin, D.T. Ulcerative Colitis Patients Have Reduced Rectal Compliance Compared with Non-Inflammatory Bowel Disease Controls. Gastroenterology 2022, 162, 331–333.e1. [Google Scholar] [CrossRef]
- Papathanasopoulos, A.A.; Katsanos, K.H.; Tatsioni, A.; Christodoulou, D.K.; Tsianos, E.V. Increased fatigability of external anal sphincter in inflammatory bowel disease: Significance in fecal urgency and incontinence. J. Crohns Colitis 2010, 4, 553–560. [Google Scholar] [CrossRef]
- Assmann, S.L.; Keszthelyi, D.; Kleijnen, J.; Anastasiou, F.; Bradshaw, E.; Brannigan, A.E.; Carrington, E.V.; Chiarioni, G.; Ebben, L.D.A.; Gladman, M.A.; et al. Guideline for the diagnosis and treatment of Faecal Incontinence-A UEG/ESCP/ESNM/ESPCG collaboration. United Eur. Gastroenterol. J. 2022, 10, 251–286. [Google Scholar] [CrossRef]
- Bharucha, A.E.; Knowles, C.H.; Malcolm, A. An Evidence-Based Practical Review on Common Benign Anorectal Disorders: Hemorrhoids, Anal Fissure, Dyssynergic Defecation, and Fecal Incontinence. Gastroenterology 2025. [Google Scholar] [CrossRef]
- Bharucha, A.E.; Zinsmeister, A.R.; Schleck, C.D.; Melton, L.J., 3rd. Bowel disturbances are the most important risk factors for late onset fecal incontinence: A population-based case-control study in women. Gastroenterology 2010, 139, 1559–1566. [Google Scholar] [CrossRef]
- Blackett, J.W.; Bharucha, A.E. Fecal Incontinence in Adults: New Therapies. Off. J. Am. Coll. Gastroenterol.|ACG 2025, 120, 2027–2041. [Google Scholar] [CrossRef]
- Moshiree, B.; Drossman, D.; Shaukat, A. AGA Clinical Practice Update on Evaluation and Management of Belching, Abdominal Bloating, and Distention: Expert Review. Gastroenterology 2023, 165, 791–800.e3. [Google Scholar] [CrossRef]
- Chey, W.D.; Hashash, J.G.; Manning, L.; Chang, L. AGA Clinical Practice Update on the Role of Diet in Irritable Bowel Syndrome: Expert Review. Gastroenterology 2022, 162, 1737–1745.e5. [Google Scholar] [CrossRef]
- Goyal, O.; Nohria, S.; Batta, S.; Dhaliwal, A.; Goyal, P.; Sood, A. Low fermentable oligosaccharides, disaccharides, monosaccharides, and polyols diet versus traditional dietary advice for functional dyspepsia: A randomized controlled trial. J. Gastroenterol. Hepatol. 2022, 37, 301–309. [Google Scholar] [CrossRef]
- Böhn, L.; Störsrud, S.; Liljebo, T.; Collin, L.; Lindfors, P.; Törnblom, H.; Simrén, M. Diet low in FODMAPs reduces symptoms of irritable bowel syndrome as well as traditional dietary advice: A randomized controlled trial. Gastroenterology 2015, 149, 1399–1407.e2. [Google Scholar] [CrossRef] [PubMed]
- Gaylord, S.A.; Palsson, O.S.; Garland, E.L.; Faurot, K.R.; Coble, R.S.; Mann, J.D.; Frey, W.; Leniek, K.; Whitehead, W.E. Mindfulness training reduces the severity of irritable bowel syndrome in women: Results of a randomized controlled trial. Am. J. Gastroenterol. 2011, 106, 1678–1688. [Google Scholar] [CrossRef]
- Damianos, J.A.; Tomar, S.K.; Azpiroz, F.; Barba, E. Abdominophrenic Dyssynergia: A Narrative Review. Am. J. Gastroenterol. 2023, 118, 41–45. [Google Scholar] [CrossRef]
- Barba, E.; Livovsky, D.M.; Accarino, A.; Azpiroz, F. Thoracoabdominal Wall Motion-Guided Biofeedback Treatment of Abdominal Distention: A Randomized Placebo-Controlled Trial. Gastroenterology 2024, 167, 538–546.e1. [Google Scholar] [CrossRef] [PubMed]
- Iovino, P.; Neri, M.C.; D’Alba, L.; Santonicola, A.; Chiarioni, G. Pelvic floor biofeedback is an effective treatment for severe bloating in disorders of gut-brain interaction with outlet dysfunction. Neurogastroenterol. Motil. 2022, 34, e14264. [Google Scholar] [CrossRef] [PubMed]
- Sharara, A.I.; Aoun, E.; Abdul-Baki, H.; Mounzer, R.; Sidani, S.; Elhajj, I. A randomized double-blind placebo-controlled trial of rifaximin in patients with abdominal bloating and flatulence. Am. J. Gastroenterol. 2006, 101, 326–333. [Google Scholar] [CrossRef] [PubMed]
- Poynard, T.; Naveau, S.; Mory, B.; Chaput, J.C. Meta-analysis of smooth muscle relaxants in the treatment of irritable bowel syndrome. Aliment. Pharmacol. Ther. 1994, 8, 499–510. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Vázquez, M.A.; Vázquez-Elizondo, G.; González-González, J.A.; Gutiérrez-Udave, R.; Maldonado-Garza, H.J.; Bosques-Padilla, F.J. Effect of antispasmodic agents, alone or in combination, in the treatment of Irritable Bowel Syndrome: Systematic review and meta-analysis. Rev. Gastroenterol. Mex. 2012, 77, 82–90. [Google Scholar] [CrossRef]
- Ke, M.; Tack, J.; Quigley, E.M.; Zou, D.; Choi, S.C.; Leelakusolvong, S.; Liu, A.; Kim, J. Effect of Prucalopride in the Treatment of Chronic Constipation in Asian and Non-Asian Women: A Pooled Analysis of 4 Randomized, Placebo-controlled Studies. J. Neurogastroenterol. Motil. 2014, 20, 458–468. [Google Scholar] [CrossRef]
- Lacy, B.E.; Schey, R.; Shiff, S.J.; Lavins, B.J.; Fox, S.M.; Jia, X.D.; Blakesley, R.E.; Hao, X.; Cronin, J.A.; Currie, M.G.; et al. Linaclotide in Chronic Idiopathic Constipation Patients with Moderate to Severe Abdominal Bloating: A Randomized, Controlled Trial. PLoS ONE 2015, 10, e0134349. [Google Scholar] [CrossRef]
- Lembo, A.J.; Schneier, H.A.; Shiff, S.J.; Kurtz, C.B.; MacDougall, J.E.; Jia, X.D.; Shao, J.Z.; Lavins, B.J.; Currie, M.G.; Fitch, D.A.; et al. Two randomized trials of linaclotide for chronic constipation. N. Engl. J. Med. 2011, 365, 527–536. [Google Scholar] [CrossRef]
- Chey, W.D.; Lembo, A.J.; Lavins, B.J.; Shiff, S.J.; Kurtz, C.B.; Currie, M.G.; MacDougall, J.E.; Jia, X.D.; Shao, J.Z.; Fitch, D.A.; et al. Linaclotide for irritable bowel syndrome with constipation: A 26-week, randomized, double-blind, placebo-controlled trial to evaluate efficacy and safety. Am. J. Gastroenterol. 2012, 107, 1702–1712. [Google Scholar] [CrossRef]
- Tack, J.; Broekaert, D.; Fischler, B.; Van Oudenhove, L.; Gevers, A.M.; Janssens, J. A controlled crossover study of the selective serotonin reuptake inhibitor citalopram in irritable bowel syndrome. Gut 2006, 55, 1095–1103. [Google Scholar] [CrossRef] [PubMed]
- Dellschaft, N.; Hoad, C.; Marciani, L.; Gowland, P.; Spiller, R. Small bowel water content assessed by MRI in health and disease: A collation of single-centre studies. Aliment. Pharmacol. Ther. 2022, 55, 327–338. [Google Scholar] [CrossRef]
- Menys, A.; Hoad, C.; Spiller, R.; Scott, S.M.; Atkinson, D.; Marciani, L.; Taylor, S.A. Spatio-temporal motility MRI analysis of the stomach and colon. Neurogastroenterol. Motil. 2019, 31, e13557. [Google Scholar] [CrossRef]
- Scott, R.A.; Williams, H.G.; Hoad, C.L.; Alyami, A.; Ortori, C.A.; Grove, J.I.; Marciani, L.; Moran, G.W.; Spiller, R.C.; Menys, A.; et al. MR Measures of Small Bowel Wall T2 Are Associated with Increased Permeability. J. Magn. Reson. Imaging 2021, 53, 1422–1431. [Google Scholar] [CrossRef] [PubMed]
- Butt, M.F.; Scotto, D.; Gilmartin, C.G.S.; Dhali, A.; Gonem, S.; Singhal, S.; Monaghan, T.M.; Frain, J.; Corsetti, M. A Medical Student Curriculum on Functional Medical Disorders. Clin. Teach. 2025, 22, e70117. [Google Scholar] [CrossRef]
- Butt, M.F.; Visaggi, P.; Singh, R.; Vork, L. Lack of awareness of neurogastroenterology and motility within medical education: Time to fill the gap. Neurogastroenterol. Motil. 2023, 35, e14666. [Google Scholar] [CrossRef] [PubMed]
- Butt, M.F. Simulated patients uncovered. Clin. Teach. 2018, 15, 81–82. [Google Scholar] [CrossRef] [PubMed]





| First Author, Year, Reference | Study Design, IBD Population (Crohn’s Disease [CD] vs. Ulcerative Colitis [UC]), Number of Patients | Intervention Studied | Definition of Inflammatory Bowel Disease (IBD) Remission | Definition of Irritable Bowel Syndrome (IBS) | Any Other Disorder of Gut–Brain Interaction (DGBI) Considered in the Study? | Main Findings |
|---|---|---|---|---|---|---|
| Berrill et al., 2014 [65] | Non-blinded RCT of 66 IBD patients | MCT (multi-convergent therapy)—a form of psychotherapy | SCCAI < 3 in UC (modified to exclude ‘general wellbeing’); HBI < 5 in CD; CRP < 10 mg/L | Rome III | No |
|
| Pedersen et al., 2017 [67] | Open-label randomized controlled trial (RCT) of 89 patients with IBD | Low-FODMAP diet | Absence of recent relapse, steroid use or therapy adjustment; simple clinical colitis activity index (SCCAI) ≤ 2 and fecal calprotectin < 100 μg/g in UC; Harvey–Bradshaw Index (HBI) < 5 and fecal calprotectin < 200 μg/g in CD; c-reactive protein (CRP) ≤ 10 mg/L | Rome III | No |
|
| Cox et al., 2017 [68] | Double-blind, placebo-controlled, cross-over RCT of 32 IBD patients | Low-FODMAP diet | Fecal calprotectin < 250 μg/g; CRP < 10 mg/L | Rome III | Functional bloating and functional diarrhea (Rome III) |
|
| Bodini et al., 2019 [69] | RCT of 55 IBD patients | Low-FODMAP diet | Mayo score < 6 in UC; HBI < 8 in CD | Rome IV | No |
|
| Cox et al., 2020 [70] | Single-blind RCT of 52 IBD patients | Low-FODMAP diet | Physician global assessment; stable medications with no recent IBD flares; Fecal calprotectin < 250 μg/g; CRP < 10 mg/L | Rome III | Functional bloating and functional diarrhea (Rome III) |
|
| Hoekman et al., 2020 [66] | Open-label RCT of 80 IBD patients | Hypnotherapy | Physician’s global assessment and fecal calprotectin ≤ 100 µg/g, or ≤200 µg/g without inflammation at endoscopy | Rome III | No |
|
| Lee et al., 2022 [71] | Observational study of 43 patients with UC | Biotop capsule® (Lactobacillus acidophilus, Clostridium butyricum TO-A, Bacillus mesentericus TO-A and Streptococcus faecalis T-110) | Mayo endoscopic score ≤ 1 | Rome IV | No |
|
| Tomita et al., 2022 [73] | Double-blind, placebo-controlled RCT of 70 IBD patients | Ramosetron | CAI ≤ 4 in UC; CDAI ≤ 150 in CD CRP ≤ 0.3 mg/dL | Rome III—Japanese version | No |
|
| Tomita et al., 2023 [72] | Prospective pilot study of 12 patients with CD | Bifidobacterium bifidum G9-1 (BBG9-1) | Endoscopy; CD activity index (CDAI) ≤ 150; CRP ≤ 0.3 mg/dL | Rome III—Japanese version | No |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Butt, M.F.; Reghefaoui, M.H.; Benedict, A.S.; Reghefaoui, M.; Al-Jabir, H.; Shaikh, A.; Vojtekova, K.; Moran, G.W.; Corsetti, M.; Aziz, Q. Irritable Bowel Syndrome in Inflammatory Bowel Disease: An Evidence-Based Practical Review. J. Clin. Med. 2026, 15, 116. https://doi.org/10.3390/jcm15010116
Butt MF, Reghefaoui MH, Benedict AS, Reghefaoui M, Al-Jabir H, Shaikh A, Vojtekova K, Moran GW, Corsetti M, Aziz Q. Irritable Bowel Syndrome in Inflammatory Bowel Disease: An Evidence-Based Practical Review. Journal of Clinical Medicine. 2026; 15(1):116. https://doi.org/10.3390/jcm15010116
Chicago/Turabian StyleButt, Mohsin F., Mustafa H. Reghefaoui, Aaron Shailesh Benedict, Maiss Reghefaoui, Hussain Al-Jabir, Aneeqa Shaikh, Katarina Vojtekova, Gordon W. Moran, Maura Corsetti, and Qasim Aziz. 2026. "Irritable Bowel Syndrome in Inflammatory Bowel Disease: An Evidence-Based Practical Review" Journal of Clinical Medicine 15, no. 1: 116. https://doi.org/10.3390/jcm15010116
APA StyleButt, M. F., Reghefaoui, M. H., Benedict, A. S., Reghefaoui, M., Al-Jabir, H., Shaikh, A., Vojtekova, K., Moran, G. W., Corsetti, M., & Aziz, Q. (2026). Irritable Bowel Syndrome in Inflammatory Bowel Disease: An Evidence-Based Practical Review. Journal of Clinical Medicine, 15(1), 116. https://doi.org/10.3390/jcm15010116






