Good Mid-Term Clinical Outcomes and Low Arthroplasty Conversion Rates After Hip Arthroscopy with Labral Debridement Without Refixation or Reconstruction
Abstract
:1. Introduction
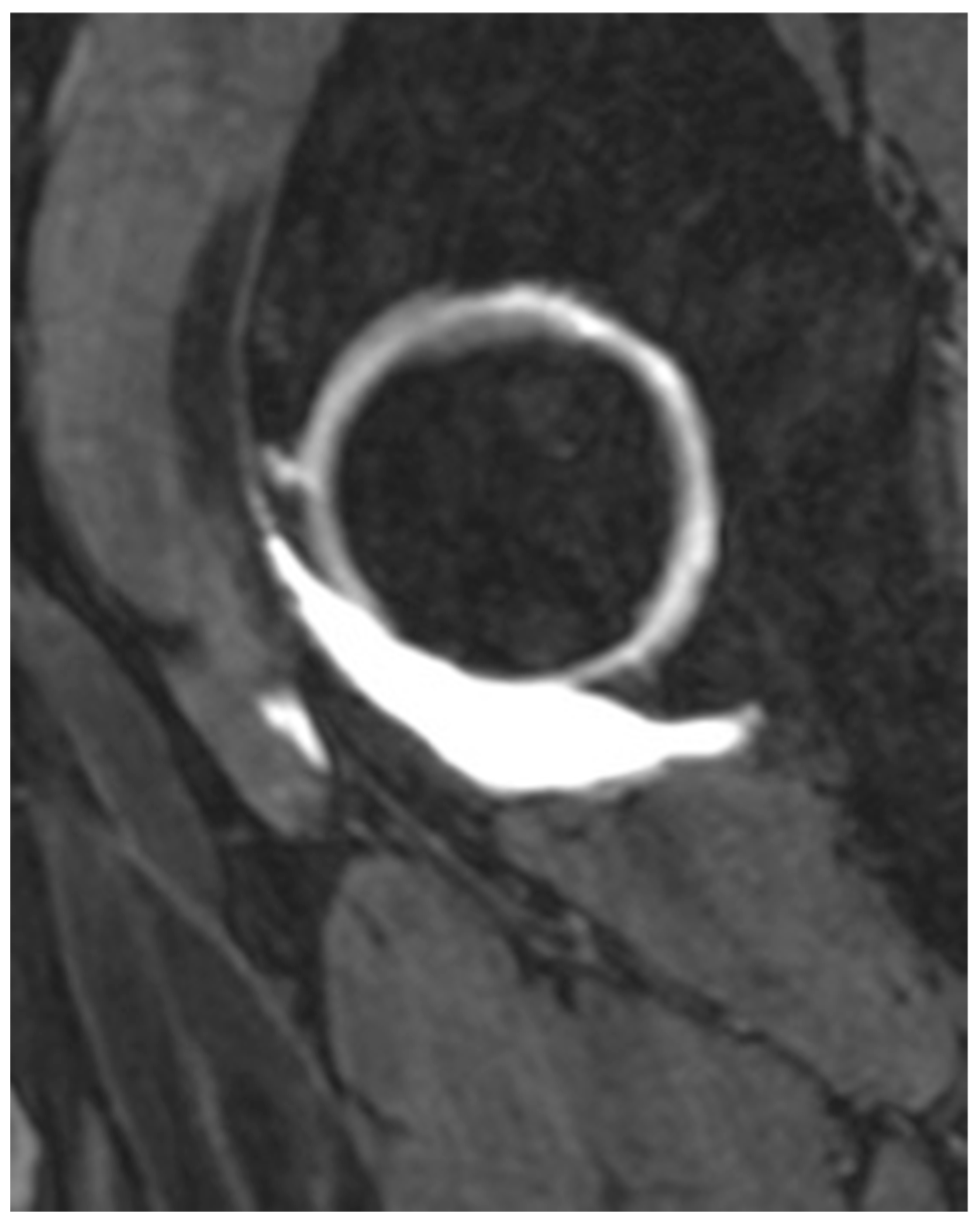
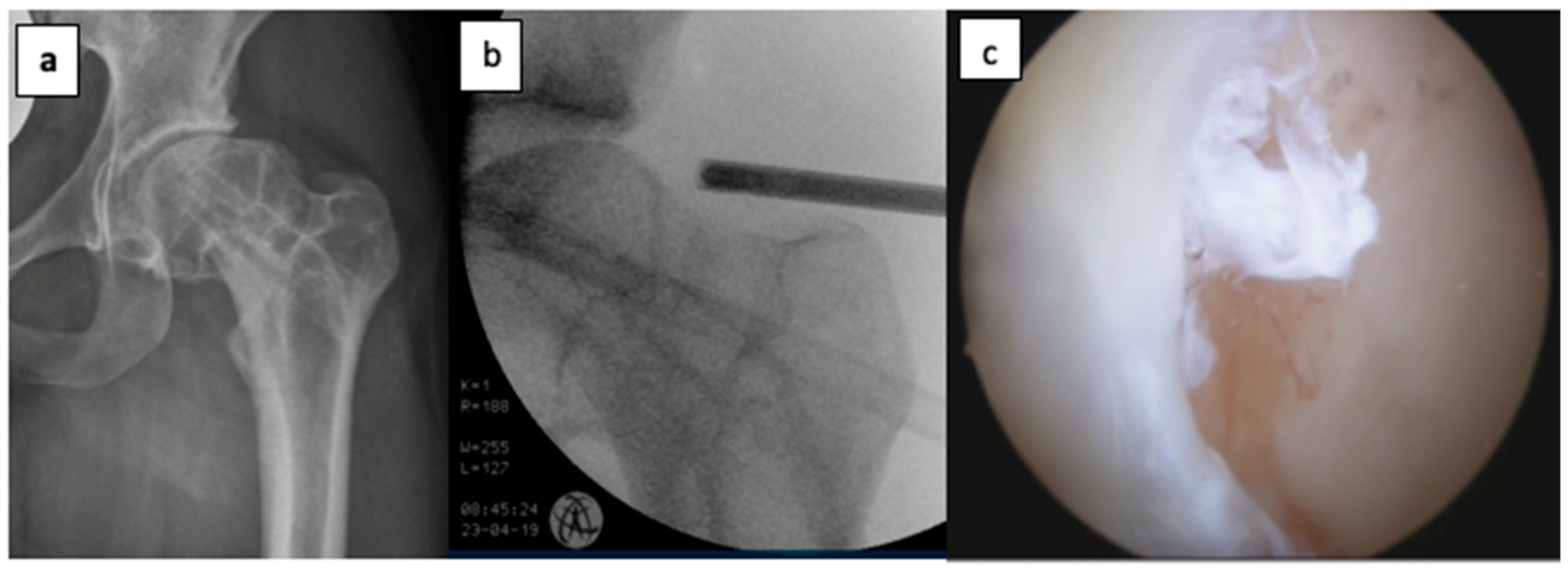
2. Materials and Methods
2.1. Patients
2.2. Indications
2.3. Follow-Up and Outcomes
2.4. Statistics
3. Results
3.1. Demographic Data
3.2. Conversion to THA
3.3. Postoperative Outcomes
3.4. Impact of Loss to Follow-Up and Sensitivity Analysis
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| FAI | Femuroacetabular impingement |
| HOOS | Hip Osteoarthritis Outcome Score |
| THA | Total hip arthroplasty |
| OA | Osteoarthritis |
| SHD | Surgical hip dislocation |
| MRI | Magnetic resonance imaging |
| SD | Standard deviation |
| IQR | Interquartile range |
References
- Nho, S.J.; Magennis, E.M.; Singh, C.K.; Kelly, B.T. Outcomes after the arthroscopic treatment of femoroacetabular impingement in a mixed group of high-level athletes. Am. J. Sports Med. 2011, 39, 14S–19S. [Google Scholar] [CrossRef] [PubMed]
- Menge, T.J.; Briggs, K.K.; Dornan, G.J.; McNamara, S.C.; Philippon, M.J. Survivorship and Outcomes 10 Years Following Hip Arthroscopy for Femoroacetabular Impingement: Labral Debridement Compared with Labral Repair. J. Bone Jt. Surg. Am. 2017, 99, 997–1004. [Google Scholar] [CrossRef]
- Ganz, R.; Gill, T.J.; Gautier, E.; Ganz, K.; Krügel, N.; Berlemann, U. Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J. Bone Jt. Surg. Br. 2001, 83, 1119–1124. [Google Scholar] [CrossRef]
- McCarthy, J.C.; Noble, P.C.; Schuck, M.R.; Wright, J.; Lee, J. The Otto E. Aufranc Award: The role of labral lesions to development of early degenerative hip disease. Clin. Orthop. 2001, 393, 25–37. [Google Scholar] [CrossRef] [PubMed]
- Domb, B.G.; Hartigan, D.E.; Perets, I. Decision Making for Labral Treatment in the Hip: Repair Versus Débridement Versus Reconstruction. J. Am. Acad. Orthop. Surg. 2017, 25, e53–e62. [Google Scholar] [CrossRef]
- Lynch, T.S.; Minkara, A.; Aoki, S.; Bedi, A.; Bharam, S.; Clohisy, J.; Harris, J.; Larson, C.; Nepple, J.; Nho, S.; et al. Best Practice Guidelines for Hip Arthroscopy in Femoroacetabular Impingement: Results of a Delphi Process. J. Am. Acad. Orthop. Surg. 2020, 28, 81–89. [Google Scholar] [CrossRef] [PubMed]
- Mehta, N.; Chamberlin, P.; Marx, R.G.; Hidaka, C.; Ge, Y.; Nawabi, D.H.; Lyman, S. Defining the Learning Curve for Hip Arthroscopy: A Threshold Analysis of the Volume-Outcomes Relationship. Am. J. Sports Med. 2018, 46, 1284–1293. [Google Scholar] [CrossRef]
- Hoppe, D.J.; de Sa, D.; Simunovic, N.; Bhandari, M.; Safran, M.R.; Larson, C.M.; Ayeni, O.R. The learning curve for hip arthroscopy: A systematic review. Arthroscopy 2014, 30, 389–397. [Google Scholar] [CrossRef]
- Domb, B.G.; Kyin, C.; Rosinsky, P.J.; Shapira, J.; Yelton, M.J.; Meghpara, M.B.; Lall, A.C.; Maldonado, D.R. Circumferential Labral Reconstruction for Irreparable Labral Tears in the Primary Setting: Minimum 2-Year Outcomes With a Nested Matched-Pair Labral Repair Control Group. Arthrosc. J. Arthrosc. Relat. Surg. 2020, 36, 2583–2597. [Google Scholar] [CrossRef]
- Lall, A.C.; Annin, S.; Chen, J.W.; Diulus, S.; Ankem, H.K.; Rosinsky, P.J.; Shapira, J.; Meghpara, M.B.; Maldonado, D.R.; Hartigan, D.; et al. Consensus-based classification system for intra-operative management of labral tears during hip arthroscopy—Aggregate recommendations from high-volume hip preservation surgeons. J. Hip Preserv. Surg. 2020, 7, 644–654. [Google Scholar] [CrossRef]
- Kelly, B.T.; Weiland, D.E.; Schenker, M.L.; Philippon, M.J. Arthroscopic Labral Repair in the Hip: Surgical Technique and Review of the Literature. Arthrosc. J. Arthrosc. Relat. Surg. 2005, 21, 1496–1504. [Google Scholar] [CrossRef] [PubMed]
- Sawyer, G.A.; Briggs, K.K.; Dornan, G.J.; Ommen, N.D.; Philippon, M.J. Clinical Outcomes After Arthroscopic Hip Labral Repair Using Looped Versus Pierced Suture Techniques. Am. J. Sports Med. 2015, 43, 1683–1688. [Google Scholar] [CrossRef] [PubMed]
- Harris, J.D. Hip labral repair: Options and outcomes. Curr. Rev. Musculoskelet. Med. 2016, 9, 361–367. [Google Scholar] [CrossRef]
- Byrd, J.W. Hip arthroscopy utilizing the supine position. Arthroscopy 1994, 10, 275–280. [Google Scholar] [CrossRef] [PubMed]
- Blasimann, A.; Dauphinee, S.; Staal, J. Translational, cross-cultural adaption, and psychometric pro- perties of the german version of the hip disability and osteoarthritis outcome score. J. Orthop. Sports Phys. Ther. 2014, 44, 989. [Google Scholar] [CrossRef]
- Paliobeis, C.P.; Villar, R.N. The prevalence of dysplasia in femoroacetabular impingement. Hip Int. 2011, 21, 141–145. [Google Scholar] [CrossRef]
- Spencer, A.D.; Newby, N.L.; Nosrat, C.; Wong, S.E.; Zhang, A.L.; Hagen, M.S. Evaluation of Outcomes Following Arthroscopic Treatment of Femoroacetabular Impingement Syndrome Across Different Surgeons, Surgical Techniques, and Postoperative Protocols: A Multi-institutional Study. Orthop. J. Sports Med. 2025, 13, 3766. [Google Scholar] [CrossRef]
- Norman, G.R.; Sloan, J.A.; Wyrwich, K.W. Interpretation of changes in health-related quality of life: The remarkable universality of half a standard deviation. Med. Care 2003, 41, 582–592. [Google Scholar] [CrossRef]
- Gupta, A.; Redmond, J.M.; Stake, C.E.; Dunne, K.F.; Domb, B.G. Does Primary Hip Arthroscopy Result in Improved Clinical Outcomes?: 2-Year Clinical Follow-up on a Mixed Group of 738 Consecutive Primary Hip Arthroscopies Performed at a High-Volume Referral Center. Am. J. Sports Med. 2016, 44, 74–82. [Google Scholar] [CrossRef]
- Harris, J.D.; McCormick, F.M.; Abrams, G.D.; Gupta, A.K.; Ellis, T.J.; Bach, B.R.; Bush-Joseph, C.A.; Nho, S.J. Complications and Reoperations During and After Hip Arthroscopy: A Systematic Review of 92 Studies and More Than 6000 Patients. Arthrosc. J. Arthrosc. Relat. Surg. 2013, 29, 589–595. [Google Scholar] [CrossRef]
- Riff, A.J.; Kunze, K.N.; Movassaghi, K.; Hijji, F.; Beck, E.C.; Harris, J.D.; Nho, S.J. Systematic Review of Hip Arthroscopy for Femoroacetabular Impingement: The Importance of Labral Repair and Capsular Closure. Arthrosc. J. Arthrosc. Relat. Surg. 2019, 35, 646–656.e3. [Google Scholar] [CrossRef] [PubMed]
- Philippon, M.J.; Christensen, J.C.; Wahoff, M.S. Rehabilitation after Arthroscopic Repair of Intra-Articular Disorders of the Hip in a Professional Football Athlete. J. Sport Rehabil. 2009, 18, 118–134. [Google Scholar] [CrossRef] [PubMed]
- Philippon, M.J.; Faucet, S.C.; Briggs, K.K. Arthroscopic Hip Labral Repair. Arthrosc. Tech. 2013, 2, e73–e76. [Google Scholar] [CrossRef]
- Byrd, J.W.T.; Jones, K.S. Hip arthroscopy in the presence of dysplasia. Arthroscopy 2003, 19, 1055–1060. [Google Scholar] [CrossRef]
- Murata, Y.; Fukase, N.; Dornan, G.; Martin, M.; Soares, R.; Pierpoint, L.; Philippon, M.J. Arthroscopic Treatment of Femoroacetabular Impingement in Patients With and Without Borderline Developmental Dysplasia of the Hip: A Systematic Review and Meta-analysis. Orthop. J. Sports Med. 2021, 9, 15973. [Google Scholar] [CrossRef] [PubMed]
- Ayeni, O.R.; Adamich, J.; Farrokhyar, F.; Simunovic, N.; Crouch, S.; Philippon, M.J.; Bhandari, M. Surgical management of labral tears during femoroacetabular impingement surgery: A systematic review. Knee Surg. Sports Traumatol. Arthrosc. 2014, 22, 756–762. [Google Scholar] [CrossRef]
- Ibrahim, M.M.; Poitras, S.; Bunting, A.C.; Sandoval, E.; Beaulé, P.E. Does acetabular coverage influence the clinical outcome of arthroscopically treated cam-type femoroacetabular impingement (FAI)? Bone Jt. J. 2018, 100-B, 831–838. [Google Scholar] [CrossRef]
- Nguyen, T.Q.; Friedman, J.M.; Flores, S.E.; Zhang, A.L. Fast Starters and Slow Starters After Hip Arthroscopy for Femoroacetabular Impingement: Correlation of Early Postoperative Pain and 2-Year Outcomes. Am. J. Sports Med. 2020, 48, 2903–2909. [Google Scholar] [CrossRef]
- Kucharik, M.P.; Abraham, P.F.; Nazal, M.R.; Varady, N.H.; Eberlin, C.T.; Meek, W.M.; Martin, S.D. Arthroscopic Acetabular Labral Repair Versus Labral Debridement: Long-term Survivorship and Functional Outcomes. Orthop. J. Sports Med. 2022, 10, 12. [Google Scholar] [CrossRef]
- Palmer, A.J.R.; Gupta, V.A.; Fernquest, S.; Rombach, I.; Dutton, S.J.; Mansour, R.; Wood, S.; Khanduja, V.; Pollard, T.C.B.; McCaskie, A.W.; et al. Arthroscopic hip surgery compared with physiotherapy and activity modification for the treatment of symptomatic femoroacetabular impingement: Multicentre randomised controlled trial. BMJ 2019, 364, l185. [Google Scholar] [CrossRef]
- Henry, L.E.; Leon, B.; Ventimiglia, D.J.; McCurdy, M.A.; Dabic, S.; Leong, N.L.; Packer, J.D.; Henn, R.F., 3rd; Meredith, S.J. Higher preoperative patient expectations predict better patient-reported psychosocial health outcomes after hip arthroscopy. J. Orthop. 2025, 64, 23–28. [Google Scholar] [CrossRef] [PubMed]
- Filbay, S.R.; Kemp, J.L.; Ackerman, I.N.; Crossley, K.M. Quality of life impairments after hip arthroscopy in people with hip chondropathy. J. Hip Preserv. Surg. 2016, 3, 154–164. [Google Scholar] [CrossRef] [PubMed]
| Indications | n (77) |
|---|---|
| Isolated labral tears | 24 (28.57%) |
| Combined labral tears and cam/pincer impingement | 49 (63.64%) |
| Posttraumatic | 3 (3.9%) |
| Chondromatosis (excluded due to primary desease) | 1 (1.3%) |
| Preoperative Score | Postoperative Score | p Value | |
|---|---|---|---|
| HOOS symptoms | 13 [3] | 14 [8] | p = 0.11 |
| HOOS pain | 25 [3] | 29.5 [10] | p < 0.001 |
| HOOS daily activity | 48 [9] | 56 [21] | p < 0.001 |
| HOOS sport | 10 [3] | 11 [6] | p = 0.006 |
| HOOS quality of life | 9 [3] | 11.5 [7] | p = 0.014 |
| HOOS total (%) | 67.6 [10.7] | 76.0 [35.6] | p < 0.001 |
| Predictor | Coefficient | 95% CI | p-Value | Interpretation |
|---|---|---|---|---|
| Age | −0.43 | [−1.19, 0.33] | 0.259 | No significant effect |
| Gender | +8.72 | [−9.96, 27.40] | 0.352 | No significant difference (trend: higher scores in females) |
| Alpha angle | +0.19 | [−1.01, 1.38] | 0.756 | No significant effect |
| Dysplasia | −5.79 | [−28.49, 16.92] | 0.610 | No significant effect |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gahleitner, M.; Hofer, D.; Hochgatterer, R.; Gotterbarm, T.; Klasan, A. Good Mid-Term Clinical Outcomes and Low Arthroplasty Conversion Rates After Hip Arthroscopy with Labral Debridement Without Refixation or Reconstruction. J. Clin. Med. 2025, 14, 3236. https://doi.org/10.3390/jcm14093236
Gahleitner M, Hofer D, Hochgatterer R, Gotterbarm T, Klasan A. Good Mid-Term Clinical Outcomes and Low Arthroplasty Conversion Rates After Hip Arthroscopy with Labral Debridement Without Refixation or Reconstruction. Journal of Clinical Medicine. 2025; 14(9):3236. https://doi.org/10.3390/jcm14093236
Chicago/Turabian StyleGahleitner, Manuel, Daniel Hofer, Rainer Hochgatterer, Tobias Gotterbarm, and Antonio Klasan. 2025. "Good Mid-Term Clinical Outcomes and Low Arthroplasty Conversion Rates After Hip Arthroscopy with Labral Debridement Without Refixation or Reconstruction" Journal of Clinical Medicine 14, no. 9: 3236. https://doi.org/10.3390/jcm14093236
APA StyleGahleitner, M., Hofer, D., Hochgatterer, R., Gotterbarm, T., & Klasan, A. (2025). Good Mid-Term Clinical Outcomes and Low Arthroplasty Conversion Rates After Hip Arthroscopy with Labral Debridement Without Refixation or Reconstruction. Journal of Clinical Medicine, 14(9), 3236. https://doi.org/10.3390/jcm14093236







