Good Mid-Term Clinical Outcomes and Low Arthroplasty Conversion Rates After Hip Arthroscopy with Labral Debridement Without Refixation or Reconstruction
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
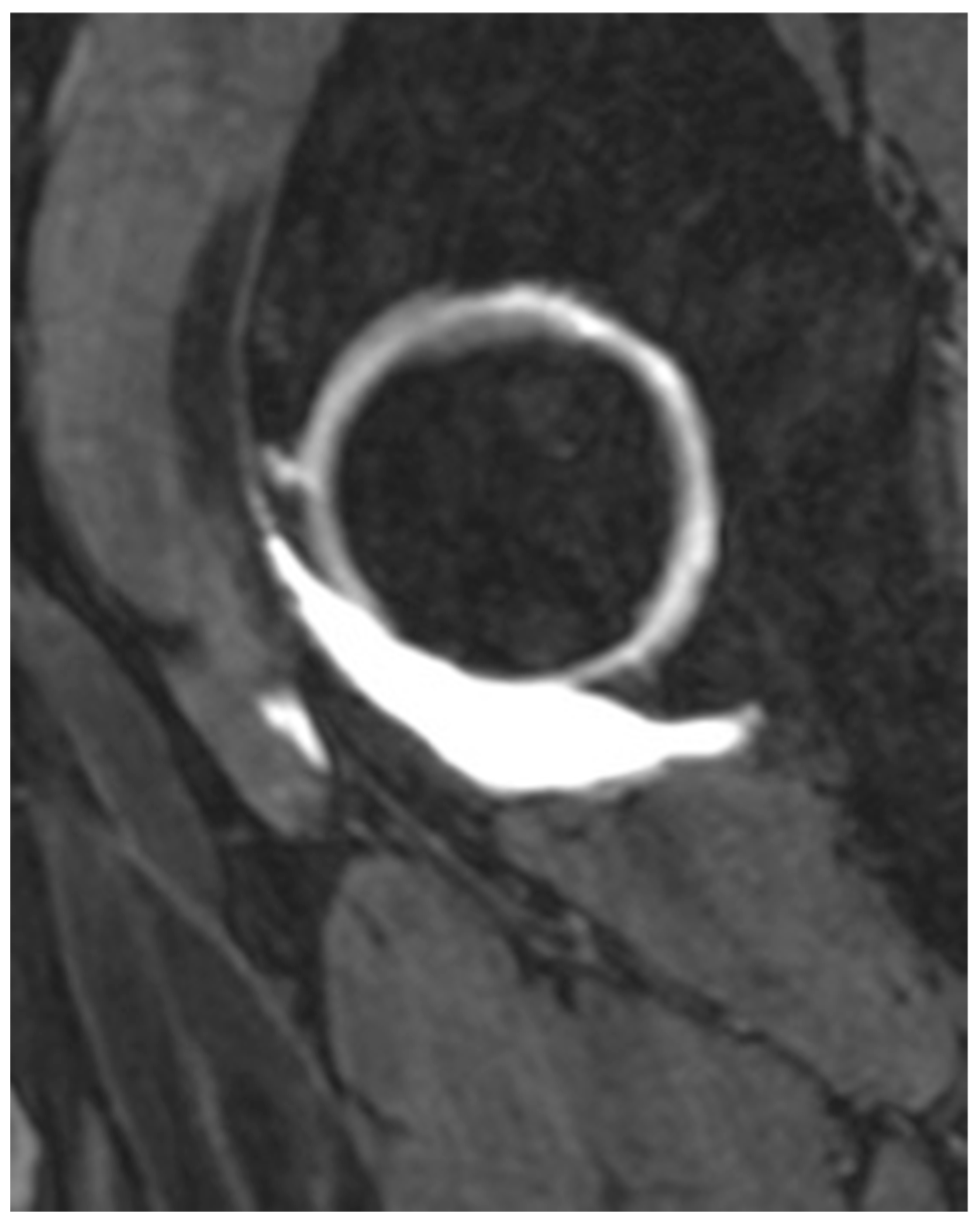
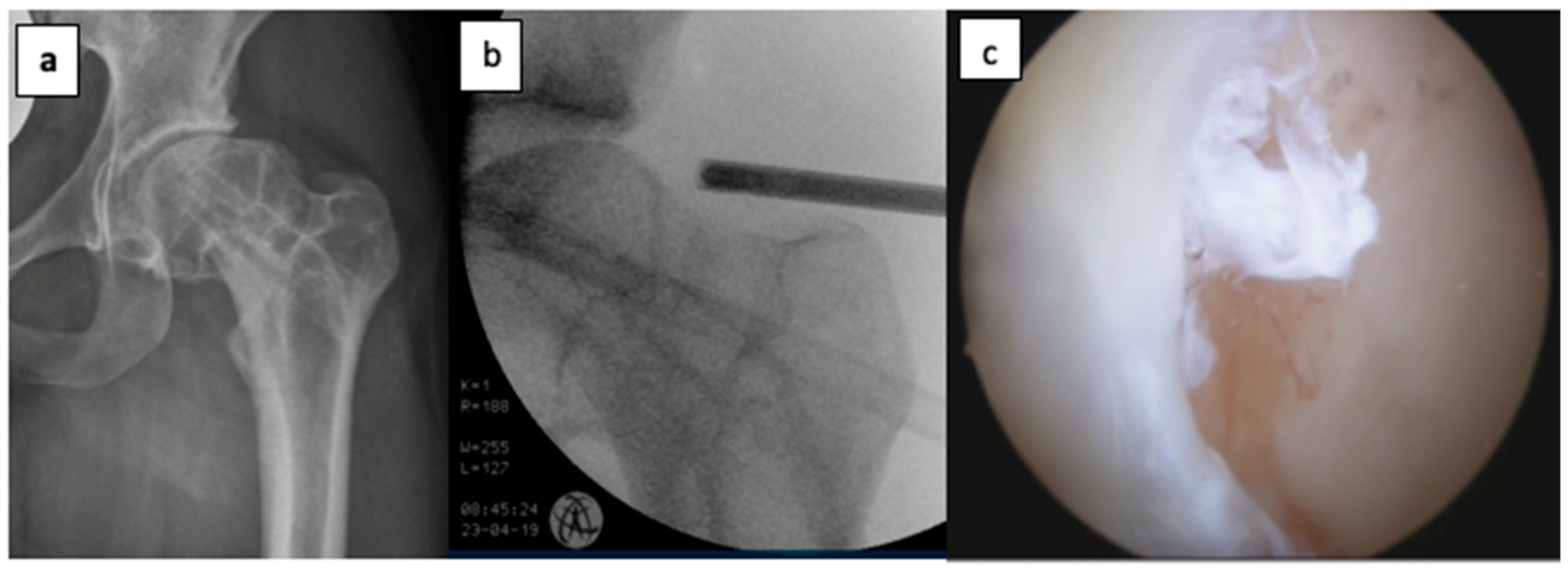
2.2. Indications
2.3. Follow-Up and Outcomes
2.4. Statistics
3. Results
3.1. Demographic Data
3.2. Conversion to THA
3.3. Postoperative Outcomes
3.4. Impact of Loss to Follow-Up and Sensitivity Analysis
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| FAI | Femuroacetabular impingement |
| HOOS | Hip Osteoarthritis Outcome Score |
| THA | Total hip arthroplasty |
| OA | Osteoarthritis |
| SHD | Surgical hip dislocation |
| MRI | Magnetic resonance imaging |
| SD | Standard deviation |
| IQR | Interquartile range |
References
- Nho, S.J.; Magennis, E.M.; Singh, C.K.; Kelly, B.T. Outcomes after the arthroscopic treatment of femoroacetabular impingement in a mixed group of high-level athletes. Am. J. Sports Med. 2011, 39, 14S–19S. [Google Scholar] [CrossRef] [PubMed]
- Menge, T.J.; Briggs, K.K.; Dornan, G.J.; McNamara, S.C.; Philippon, M.J. Survivorship and Outcomes 10 Years Following Hip Arthroscopy for Femoroacetabular Impingement: Labral Debridement Compared with Labral Repair. J. Bone Jt. Surg. Am. 2017, 99, 997–1004. [Google Scholar] [CrossRef]
- Ganz, R.; Gill, T.J.; Gautier, E.; Ganz, K.; Krügel, N.; Berlemann, U. Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J. Bone Jt. Surg. Br. 2001, 83, 1119–1124. [Google Scholar] [CrossRef]
- McCarthy, J.C.; Noble, P.C.; Schuck, M.R.; Wright, J.; Lee, J. The Otto E. Aufranc Award: The role of labral lesions to development of early degenerative hip disease. Clin. Orthop. 2001, 393, 25–37. [Google Scholar] [CrossRef] [PubMed]
- Domb, B.G.; Hartigan, D.E.; Perets, I. Decision Making for Labral Treatment in the Hip: Repair Versus Débridement Versus Reconstruction. J. Am. Acad. Orthop. Surg. 2017, 25, e53–e62. [Google Scholar] [CrossRef]
- Lynch, T.S.; Minkara, A.; Aoki, S.; Bedi, A.; Bharam, S.; Clohisy, J.; Harris, J.; Larson, C.; Nepple, J.; Nho, S.; et al. Best Practice Guidelines for Hip Arthroscopy in Femoroacetabular Impingement: Results of a Delphi Process. J. Am. Acad. Orthop. Surg. 2020, 28, 81–89. [Google Scholar] [CrossRef] [PubMed]
- Mehta, N.; Chamberlin, P.; Marx, R.G.; Hidaka, C.; Ge, Y.; Nawabi, D.H.; Lyman, S. Defining the Learning Curve for Hip Arthroscopy: A Threshold Analysis of the Volume-Outcomes Relationship. Am. J. Sports Med. 2018, 46, 1284–1293. [Google Scholar] [CrossRef]
- Hoppe, D.J.; de Sa, D.; Simunovic, N.; Bhandari, M.; Safran, M.R.; Larson, C.M.; Ayeni, O.R. The learning curve for hip arthroscopy: A systematic review. Arthroscopy 2014, 30, 389–397. [Google Scholar] [CrossRef]
- Domb, B.G.; Kyin, C.; Rosinsky, P.J.; Shapira, J.; Yelton, M.J.; Meghpara, M.B.; Lall, A.C.; Maldonado, D.R. Circumferential Labral Reconstruction for Irreparable Labral Tears in the Primary Setting: Minimum 2-Year Outcomes With a Nested Matched-Pair Labral Repair Control Group. Arthrosc. J. Arthrosc. Relat. Surg. 2020, 36, 2583–2597. [Google Scholar] [CrossRef]
- Lall, A.C.; Annin, S.; Chen, J.W.; Diulus, S.; Ankem, H.K.; Rosinsky, P.J.; Shapira, J.; Meghpara, M.B.; Maldonado, D.R.; Hartigan, D.; et al. Consensus-based classification system for intra-operative management of labral tears during hip arthroscopy—Aggregate recommendations from high-volume hip preservation surgeons. J. Hip Preserv. Surg. 2020, 7, 644–654. [Google Scholar] [CrossRef]
- Kelly, B.T.; Weiland, D.E.; Schenker, M.L.; Philippon, M.J. Arthroscopic Labral Repair in the Hip: Surgical Technique and Review of the Literature. Arthrosc. J. Arthrosc. Relat. Surg. 2005, 21, 1496–1504. [Google Scholar] [CrossRef] [PubMed]
- Sawyer, G.A.; Briggs, K.K.; Dornan, G.J.; Ommen, N.D.; Philippon, M.J. Clinical Outcomes After Arthroscopic Hip Labral Repair Using Looped Versus Pierced Suture Techniques. Am. J. Sports Med. 2015, 43, 1683–1688. [Google Scholar] [CrossRef] [PubMed]
- Harris, J.D. Hip labral repair: Options and outcomes. Curr. Rev. Musculoskelet. Med. 2016, 9, 361–367. [Google Scholar] [CrossRef]
- Byrd, J.W. Hip arthroscopy utilizing the supine position. Arthroscopy 1994, 10, 275–280. [Google Scholar] [CrossRef] [PubMed]
- Blasimann, A.; Dauphinee, S.; Staal, J. Translational, cross-cultural adaption, and psychometric pro- perties of the german version of the hip disability and osteoarthritis outcome score. J. Orthop. Sports Phys. Ther. 2014, 44, 989. [Google Scholar] [CrossRef]
- Paliobeis, C.P.; Villar, R.N. The prevalence of dysplasia in femoroacetabular impingement. Hip Int. 2011, 21, 141–145. [Google Scholar] [CrossRef]
- Spencer, A.D.; Newby, N.L.; Nosrat, C.; Wong, S.E.; Zhang, A.L.; Hagen, M.S. Evaluation of Outcomes Following Arthroscopic Treatment of Femoroacetabular Impingement Syndrome Across Different Surgeons, Surgical Techniques, and Postoperative Protocols: A Multi-institutional Study. Orthop. J. Sports Med. 2025, 13, 3766. [Google Scholar] [CrossRef]
- Norman, G.R.; Sloan, J.A.; Wyrwich, K.W. Interpretation of changes in health-related quality of life: The remarkable universality of half a standard deviation. Med. Care 2003, 41, 582–592. [Google Scholar] [CrossRef]
- Gupta, A.; Redmond, J.M.; Stake, C.E.; Dunne, K.F.; Domb, B.G. Does Primary Hip Arthroscopy Result in Improved Clinical Outcomes?: 2-Year Clinical Follow-up on a Mixed Group of 738 Consecutive Primary Hip Arthroscopies Performed at a High-Volume Referral Center. Am. J. Sports Med. 2016, 44, 74–82. [Google Scholar] [CrossRef]
- Harris, J.D.; McCormick, F.M.; Abrams, G.D.; Gupta, A.K.; Ellis, T.J.; Bach, B.R.; Bush-Joseph, C.A.; Nho, S.J. Complications and Reoperations During and After Hip Arthroscopy: A Systematic Review of 92 Studies and More Than 6000 Patients. Arthrosc. J. Arthrosc. Relat. Surg. 2013, 29, 589–595. [Google Scholar] [CrossRef]
- Riff, A.J.; Kunze, K.N.; Movassaghi, K.; Hijji, F.; Beck, E.C.; Harris, J.D.; Nho, S.J. Systematic Review of Hip Arthroscopy for Femoroacetabular Impingement: The Importance of Labral Repair and Capsular Closure. Arthrosc. J. Arthrosc. Relat. Surg. 2019, 35, 646–656.e3. [Google Scholar] [CrossRef] [PubMed]
- Philippon, M.J.; Christensen, J.C.; Wahoff, M.S. Rehabilitation after Arthroscopic Repair of Intra-Articular Disorders of the Hip in a Professional Football Athlete. J. Sport Rehabil. 2009, 18, 118–134. [Google Scholar] [CrossRef] [PubMed]
- Philippon, M.J.; Faucet, S.C.; Briggs, K.K. Arthroscopic Hip Labral Repair. Arthrosc. Tech. 2013, 2, e73–e76. [Google Scholar] [CrossRef]
- Byrd, J.W.T.; Jones, K.S. Hip arthroscopy in the presence of dysplasia. Arthroscopy 2003, 19, 1055–1060. [Google Scholar] [CrossRef]
- Murata, Y.; Fukase, N.; Dornan, G.; Martin, M.; Soares, R.; Pierpoint, L.; Philippon, M.J. Arthroscopic Treatment of Femoroacetabular Impingement in Patients With and Without Borderline Developmental Dysplasia of the Hip: A Systematic Review and Meta-analysis. Orthop. J. Sports Med. 2021, 9, 15973. [Google Scholar] [CrossRef] [PubMed]
- Ayeni, O.R.; Adamich, J.; Farrokhyar, F.; Simunovic, N.; Crouch, S.; Philippon, M.J.; Bhandari, M. Surgical management of labral tears during femoroacetabular impingement surgery: A systematic review. Knee Surg. Sports Traumatol. Arthrosc. 2014, 22, 756–762. [Google Scholar] [CrossRef]
- Ibrahim, M.M.; Poitras, S.; Bunting, A.C.; Sandoval, E.; Beaulé, P.E. Does acetabular coverage influence the clinical outcome of arthroscopically treated cam-type femoroacetabular impingement (FAI)? Bone Jt. J. 2018, 100-B, 831–838. [Google Scholar] [CrossRef]
- Nguyen, T.Q.; Friedman, J.M.; Flores, S.E.; Zhang, A.L. Fast Starters and Slow Starters After Hip Arthroscopy for Femoroacetabular Impingement: Correlation of Early Postoperative Pain and 2-Year Outcomes. Am. J. Sports Med. 2020, 48, 2903–2909. [Google Scholar] [CrossRef]
- Kucharik, M.P.; Abraham, P.F.; Nazal, M.R.; Varady, N.H.; Eberlin, C.T.; Meek, W.M.; Martin, S.D. Arthroscopic Acetabular Labral Repair Versus Labral Debridement: Long-term Survivorship and Functional Outcomes. Orthop. J. Sports Med. 2022, 10, 12. [Google Scholar] [CrossRef]
- Palmer, A.J.R.; Gupta, V.A.; Fernquest, S.; Rombach, I.; Dutton, S.J.; Mansour, R.; Wood, S.; Khanduja, V.; Pollard, T.C.B.; McCaskie, A.W.; et al. Arthroscopic hip surgery compared with physiotherapy and activity modification for the treatment of symptomatic femoroacetabular impingement: Multicentre randomised controlled trial. BMJ 2019, 364, l185. [Google Scholar] [CrossRef]
- Henry, L.E.; Leon, B.; Ventimiglia, D.J.; McCurdy, M.A.; Dabic, S.; Leong, N.L.; Packer, J.D.; Henn, R.F., 3rd; Meredith, S.J. Higher preoperative patient expectations predict better patient-reported psychosocial health outcomes after hip arthroscopy. J. Orthop. 2025, 64, 23–28. [Google Scholar] [CrossRef] [PubMed]
- Filbay, S.R.; Kemp, J.L.; Ackerman, I.N.; Crossley, K.M. Quality of life impairments after hip arthroscopy in people with hip chondropathy. J. Hip Preserv. Surg. 2016, 3, 154–164. [Google Scholar] [CrossRef] [PubMed]
| Indications | n (77) |
|---|---|
| Isolated labral tears | 24 (28.57%) |
| Combined labral tears and cam/pincer impingement | 49 (63.64%) |
| Posttraumatic | 3 (3.9%) |
| Chondromatosis (excluded due to primary desease) | 1 (1.3%) |
| Preoperative Score | Postoperative Score | p Value | |
|---|---|---|---|
| HOOS symptoms | 13 [3] | 14 [8] | p = 0.11 |
| HOOS pain | 25 [3] | 29.5 [10] | p < 0.001 |
| HOOS daily activity | 48 [9] | 56 [21] | p < 0.001 |
| HOOS sport | 10 [3] | 11 [6] | p = 0.006 |
| HOOS quality of life | 9 [3] | 11.5 [7] | p = 0.014 |
| HOOS total (%) | 67.6 [10.7] | 76.0 [35.6] | p < 0.001 |
| Predictor | Coefficient | 95% CI | p-Value | Interpretation |
|---|---|---|---|---|
| Age | −0.43 | [−1.19, 0.33] | 0.259 | No significant effect |
| Gender | +8.72 | [−9.96, 27.40] | 0.352 | No significant difference (trend: higher scores in females) |
| Alpha angle | +0.19 | [−1.01, 1.38] | 0.756 | No significant effect |
| Dysplasia | −5.79 | [−28.49, 16.92] | 0.610 | No significant effect |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gahleitner, M.; Hofer, D.; Hochgatterer, R.; Gotterbarm, T.; Klasan, A. Good Mid-Term Clinical Outcomes and Low Arthroplasty Conversion Rates After Hip Arthroscopy with Labral Debridement Without Refixation or Reconstruction. J. Clin. Med. 2025, 14, 3236. https://doi.org/10.3390/jcm14093236
Gahleitner M, Hofer D, Hochgatterer R, Gotterbarm T, Klasan A. Good Mid-Term Clinical Outcomes and Low Arthroplasty Conversion Rates After Hip Arthroscopy with Labral Debridement Without Refixation or Reconstruction. Journal of Clinical Medicine. 2025; 14(9):3236. https://doi.org/10.3390/jcm14093236
Chicago/Turabian StyleGahleitner, Manuel, Daniel Hofer, Rainer Hochgatterer, Tobias Gotterbarm, and Antonio Klasan. 2025. "Good Mid-Term Clinical Outcomes and Low Arthroplasty Conversion Rates After Hip Arthroscopy with Labral Debridement Without Refixation or Reconstruction" Journal of Clinical Medicine 14, no. 9: 3236. https://doi.org/10.3390/jcm14093236
APA StyleGahleitner, M., Hofer, D., Hochgatterer, R., Gotterbarm, T., & Klasan, A. (2025). Good Mid-Term Clinical Outcomes and Low Arthroplasty Conversion Rates After Hip Arthroscopy with Labral Debridement Without Refixation or Reconstruction. Journal of Clinical Medicine, 14(9), 3236. https://doi.org/10.3390/jcm14093236







