Directly Visualized Carpal Tunnel Release via a Proximal Mini-Transverse Incision: Surgical Technique and Clinical Outcomes
Abstract
:1. Introduction
2. Materials and Methods
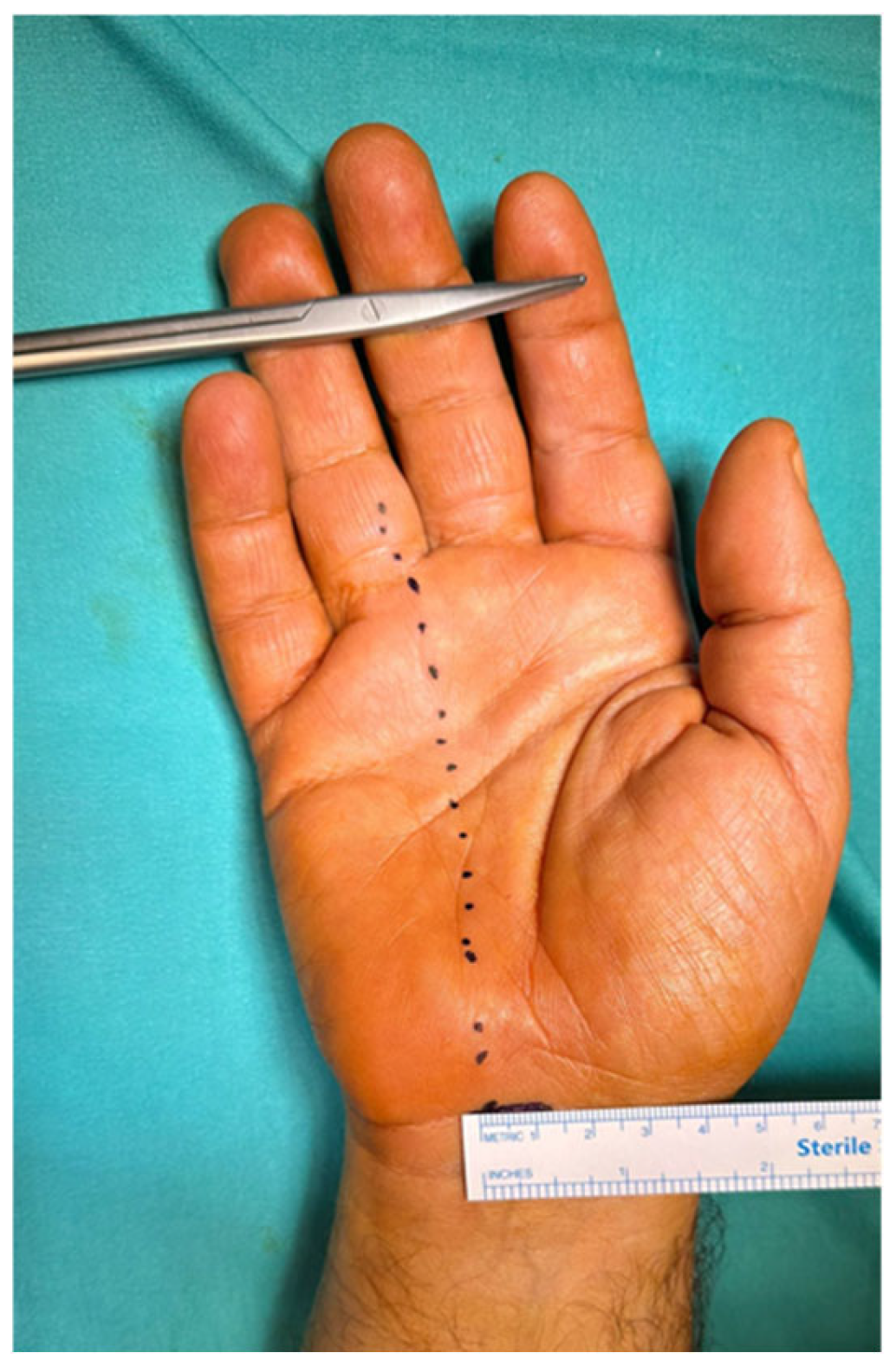
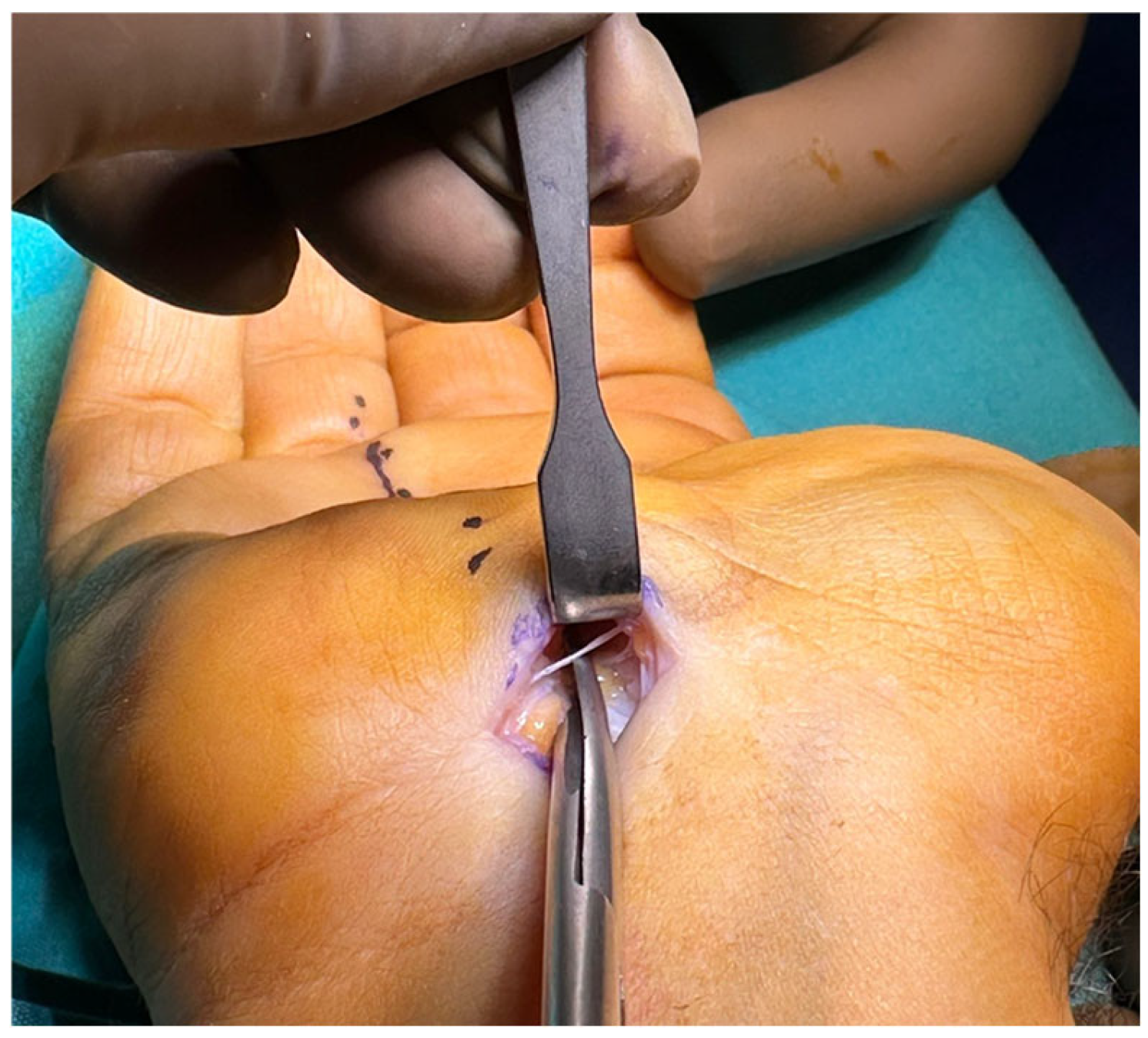
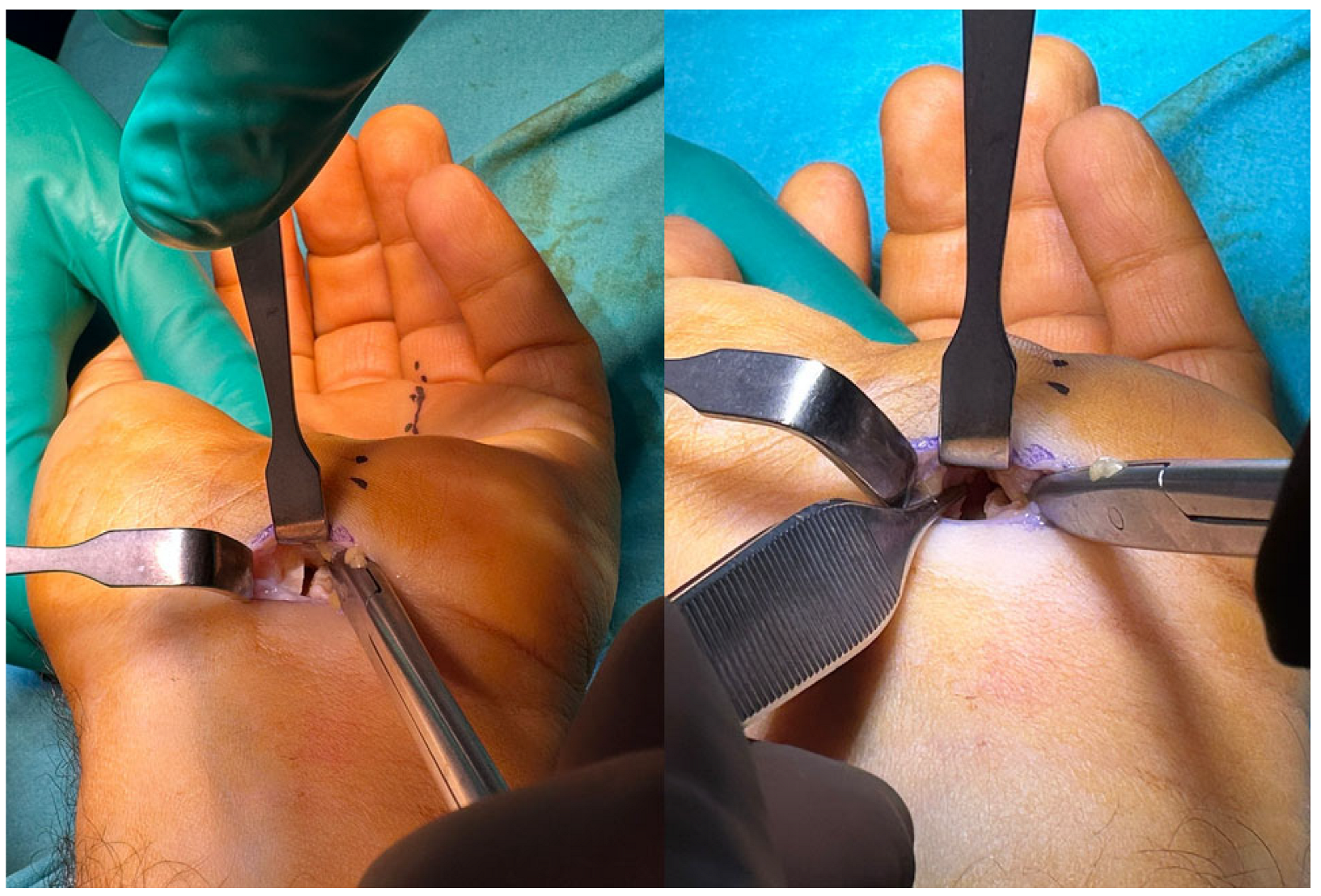
2.1. Surgical Technique
2.2. Postoperative Care
2.3. Outcome Measures
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CTS | Carpal tunnel syndrome |
| EMG | Electromyography |
| AAEM | American Association of Electrodiagnostic Medicine |
| Quick-DASH | Quick Disabilities of the Arm, Shoulder, and Hand Questionnaire |
| BCTSQ | Boston Carpal Tunnel Syndrome Questionnaire |
| VAS | Visual analog scale |
| SSS | Symptom Severity Scale |
| FSS | Functional Status Scale |
| ASSH | American Society for Surgery of the Hand |
References
- Karamanos, E.; Jillian, B.-Q.; Person, D. Endoscopic Carpal Tunnel Release. Orthop. Clin. N. Am. 2020, 51, 361–368. [Google Scholar] [CrossRef] [PubMed]
- Osiak, K.; Elnazir, P.; Walocha, J.A.; Pasternak, A. Carpal Tunnel Syndrome: State-of-the-Art Review. Folia Morphol. 2022, 81, 851–862. [Google Scholar] [CrossRef]
- Yunoki, M.; Kanda, T.; Suzuki, K.; Uneda, A.; Hirashita, K.; Yoshino, K. Importance of Recognizing Carpal Tunnel Syndrome for Neurosurgeons: A Review. Neurol. Med. Chir. 2017, 57, 172–183. [Google Scholar] [CrossRef] [PubMed]
- Orhurhu, V.; Orman, S.; Peck, J.; Urits, I.; Orhurhu, M.S.; Jones, M.R.; Manchikanti, L.; Kaye, A.D.; Odonkor, C.; Hirji, S.; et al. Carpal Tunnel Release Surgery—A Systematic Review of Open and Endoscopic Approaches. Anesth. Pain Med. 2020, 10, e112291. [Google Scholar] [CrossRef]
- Kim, P.-T.; Lee, H.-J.; Kim, T.-G.; Jeon, I.-H. Current Approaches for Carpal Tunnel Syndrome. Clin. Orthop. Surg. 2014, 6, 253. [Google Scholar] [CrossRef]
- Zamborsky, R.; Kokavec, M.; Simko, L.; Bohac, M. Carpal Tunnel Syndrome: Symptoms, Causes and Treatment Options. Literature Reviev. Ortop. Traumatol. Rehabil. 2017, 19, 1–8. [Google Scholar] [CrossRef]
- Avci, S.; Sayli, U. Carpal Tunnel Release Using a Short Palmar Incision and a New Knife. J. Hand Surg. 2000, 25, 357–360. [Google Scholar] [CrossRef]
- Chou, R.C.; Robinson, D.M.; Homer, S. Ultrasound-guided Percutaneous Carpal Tunnel Release: A Systematic Review. PM&R 2023, 15, 363–379. [Google Scholar] [CrossRef]
- Rajeswaran, G.; Healy, J.; Lee, J. Percutaneous Release Procedures: Trigger Finger and Carpal Tunnel. Semin. Musculoskelet. Radiol. 2016, 20, 432–440. [Google Scholar] [CrossRef]
- Stecco, C.; Macchi, V.; Lancerotto, L.; Tiengo, C.; Porzionato, A.; De Caro, R. Comparison of Transverse Carpal Ligament and Flexor Retinaculum Terminology for the Wrist. J. Hand Surg. 2010, 35, 746–753. [Google Scholar] [CrossRef]
- Boya, H.; Özcan, Ö.; Öztekïn, H.H. Long-term Complications of Open Carpal Tunnel Release. Muscle Nerve 2008, 38, 1443–1446. [Google Scholar] [CrossRef] [PubMed]
- Michelotti, B.; Romanowsky, D.; Hauck, R.M. Prospective, Randomized Evaluation of Endoscopic Versus Open Carpal Tunnel Release in Bilateral Carpal Tunnel Syndrome: An Interim Analysis. Ann. Plast. Surg. 2014, 73, S157–S160. [Google Scholar] [CrossRef] [PubMed]
- Hajibarati, B.; Molaei, H.; Hasanzadeh, A.; Ahmadzade, A.; Mirshahi, M.; Abdorrazzaghi, H. Carpal Tunnel Syndrome: Open or Endoscopic Release Surgery Method? Arch. Bone Jt. Surg. 2022, 10, 677. [Google Scholar] [CrossRef] [PubMed]
- Liawrungrueang, W.; Wongsiri, S.; Sarasombath, P. Endoscopic Carpal Surgery in Carpal Tunnel Syndrome: A Systematic Review. SAGE Open Med. 2023, 11, 20503121231177111. [Google Scholar] [CrossRef]
- Concannon, M.J.; Brownfield, M.L.; Puckett, C.L. The Incidence of Recurrence after Endoscopic Carpal Tunnel Release. Plast. Reconstr. Surg. 2000, 105, 1662–1665. [Google Scholar] [CrossRef]
- Gaba, S.; Bhogesha, S.; Singh, O. Limited Incision Carpal Tunnel Release. IJOO 2017, 51, 192–198. [Google Scholar] [CrossRef]
- Lee, Y.-S.; Youn, H.; Shin, S.-H.; Chung, Y.-G. Minimally Invasive Carpal Tunnel Release Using a Hook Knife through a Small Transverse Carpal Incision: Technique and Outcome. Clin. Orthop. Surg. 2023, 15, 318. [Google Scholar] [CrossRef]
- Abouzahr, M.K.; Patsis, M.C.; Chiu, D.T.W. Carpal Tunnel Release Using Limited Direct Vision. Plast. Reconstr. Surg. 1995, 95, 534. [Google Scholar] [CrossRef]
- Chapman, C.B.; Ristic, S.; Rosenwasser, M.P. Complete Median Nerve Transection as a Complication of Carpal Tunnel Release with a Carpal Tunnel Tome. Am. J. Orthop. 2001, 30, 652–653. [Google Scholar]
- Padua, L.; Lo Monaco, M.; Padua, R.; Gregori, B.; Tonali, P. Neurophysiological Classification of Carpal Tunnel Syndrome: Assessment of 600 Symptomatic Hands. Ital. J. Neuro. Sci. 1997, 18, 145–150. [Google Scholar] [CrossRef]
- Cansü, E.; Heydar, A.M.; Alakbarov, A.; Ünal, M.B. Neglected Lunate Dislocation Presenting as Carpal Tunnel Syndrome. Case Rep. Plast. Surg. Hand Surg. 2015, 2, 22–24. [Google Scholar] [CrossRef]
- Chammas, M. Carpal Tunnel Syndrome—Le syndrome du canal carpien. Chir. Main 2014, 33, 75–94. [Google Scholar] [CrossRef] [PubMed]
- Koldas Dogan, S.; Ay, S.; Evcik, D.; Baser, O. Adaptation of Turkish Version of the Questionnaire Quick Disability of the Arm, Shoulder, and Hand (Quick DASH) in Patients with Carpal Tunnel Syndrome. Clin. Rheumatol. 2011, 30, 185–191. [Google Scholar] [CrossRef] [PubMed]
- Khoshnevis, J.; Layegh, H.; Yavari, N.; Eslami, G.; Afsharfard, A.; Reza Kalantar-Motamedi, S.M.; Zarrintan, S. Comparing Open Conventional Carpal Tunnel Release with Mini-Incision Technique in the Treatment of Carpal Tunnel Syndrome: A Non-Randomized Clinical Trial. Ann. Med. Surg. 2020, 55, 119–123. [Google Scholar] [CrossRef]
- Murthy, P.G.; Goljan, P.; Mendez, G.; Jacoby, S.M.; Shin, E.K.; Osterman, A.L. Mini-Open versus Extended Open Release for Severe Carpal Tunnel Syndrome. Hand 2015, 10, 34–39. [Google Scholar] [CrossRef]
- Mardanpour, K.; Rahbar, M.; Mardanpour, S. Functional Outcomes of 300 Carpal Tunnel Release: 1.5 Cm Longitudinal Mini-Incision. Asian J. Neurosurg. 2019, 14, 693–697. [Google Scholar] [CrossRef]
- Muhammed Fazil, V.V.; Surendran, S.; Karuppal, R.; Gopinathan, P.; Marthya, A. Mini-Open Transverse Flexor Crease Incision versus Limited Longitudinal Palmar Incision Carpal Tunnel Release: A Short Term Outcome Study. J. Orthop. 2022, 29, 15–21. [Google Scholar] [CrossRef]
- Jugovac, I.; Burgić, N.; Mićović, V.; Radolović-Prenc, L.; Uravić, M.; Golubović, V.; Stancić, M.F. Carpal Tunnel Release by Limited Palmar Incision vs Traditional Open Technique: Randomized Controlled Trial. Croat. Med. J. 2002, 43, 33–36. [Google Scholar]
- Bal, E. Comparison between Two Mini Incision Techniques Utilized in Carpal Tunnel Release. Acta Orthop. Traumatol. Turc. 2008, 42, 234–237. [Google Scholar] [CrossRef]
- DaSilva, M.F.; Moore, D.C.; Weiss, A.-P.C.; Akelman, E.; Sikirica, M. Anatomy of the Palmar Cutaneous Branch of the Median Nerve: Clinical Significance. J. Hand Surg. 1996, 21, 639–643. [Google Scholar] [CrossRef]
- Nathan, P.A.; Meadows, K.D.; Keniston, R.C. Rehabilitation of Carpal Tunnel Surgery Patients Using a Short Surgical Incision and an Early Program of Physical Therapy. J. Hand Surg. 1993, 18, 1044–1050. [Google Scholar] [CrossRef]
- Keramettin, A.; Cengiz, C.; Nilgun, C.; Ayhan, B. Microsurgical Open Mini Uniskin Incision Technique in the Surgical Treatment of Carpal Tunnel Syndrome. Neurol. India 2006, 54, 64. [Google Scholar] [CrossRef] [PubMed]
- Korkmaz, M.; Ekici, M.A.; Cepoglu, M.C.; Oztürk, H. Mini Transverse versus Longitudinal Incision in Carpal Tunnel Syndrome. J. Coll. Physicians Surg. Pak. 2013, 23, 645–648. [Google Scholar] [PubMed]
- Ma, T.; Wang, D.; Hu, Y.; Zhao, X.; Wang, W.; Song, L. Mini-Transverse Incision Using a Novel Bush-Hook versus Conventional Open Incision for Treatment of Carpal Tunnel Syndrome: A Prospective Study. J. Orthop. Surg. Res. 2021, 16, 462. [Google Scholar] [CrossRef]
- Wang, D.; Ma, T.; Hu, Y.; Zhao, X.; Song, L. Effectiveness and Safety of Surgical Treatment of Carpal Tunnel Syndrome via a Mini-Transverse Incision and a Bush Hook versus a Mid-Palmar Small Longitudinal Incision. J. Orthop. Surg. Res. 2022, 17, 75. [Google Scholar] [CrossRef]
- Cellocco, P.; Rossi, C.; Bizzarri, F.; Patrizio, L.; Costanzo, G. Mini-Open Blind Procedure Versus Limited Open Technique for Carpal Tunnel Release: A 30-Month Follow-Up Study. J. Hand Surg. 2005, 30, 493–499. [Google Scholar] [CrossRef]
- Castillo, T.N.; Yao, J. Prospective Randomized Comparison of Single-Incision and Two-Incision Carpal Tunnel Release Outcomes. Hand 2014, 9, 36–42. [Google Scholar] [CrossRef]


| Grade | Criteria |
|---|---|
| Mild Carpal Tunnel Syndrome | Only sensory peak latency and falling sensory amplitude |
| Moderate Carpal Tunnel Syndrome | Abnormal median sensory interaction with addition of motor distal latency prolongation |
| Severe Carpal Tunnel Syndrome | Median motor and sensory distal latency prolongation in addition to sensory and motor amplitude decrease |
| Very Severe Carpal Tunnel Syndrome | No median sonsory or motor response |
| Variable | Value |
|---|---|
| Sex | |
| Female | 48 |
| Male | 27 |
| Age | 52 ± 7.3 (38–62) years |
| Side | |
| Bilateral | 21 |
| Right | 36 |
| Left | 18 |
| Hand dominance | |
| Dominant | 49 |
| Non-dominant | 26 |
| Follow-up period | 28 ± 4.8 (14–52) months |
| EMG grade (AAEM grading system) | |
| Grade 1 (mild) | - |
| Grade 2 (moderate) | 39 |
| Grade 3 (severe) | 57 |
| Grade 4 (very severe) | - |
| Preoperative | Postoperative | |||||
|---|---|---|---|---|---|---|
| 3 Months | p-Value | Final Follow-Up | p-Value * | |||
| VAS score | 5.2 ± 1.4 | 1.4 ± 1.1 | >0.001 | 0.7 ± 0.7 | 0.0019 | |
| Quick-DASH Score | 27.46 ± 7 | 10.2 ± 3.8 | >0.001 | 7.4 ± 24.6 | 0.65 | |
| BCTSQ | SSS | 3.6 ± 1.2 | 1.75 ± 0.6 | >0.001 | 1.2 ± 0.7 | 0.14 |
| FSS | 3.8 ± 0.9 | 2 ± 1 | 0.001 | 1.2 ± 0.6 | 0.13 | |
| Grip strength (in kg) | 24.2 ± 8.9 | 25.6 ± 6.5 | >0.001 | 28.2 ± 2.6 | >0.001 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Heydar, A.M.; Kürklü, M. Directly Visualized Carpal Tunnel Release via a Proximal Mini-Transverse Incision: Surgical Technique and Clinical Outcomes. J. Clin. Med. 2025, 14, 3234. https://doi.org/10.3390/jcm14093234
Heydar AM, Kürklü M. Directly Visualized Carpal Tunnel Release via a Proximal Mini-Transverse Incision: Surgical Technique and Clinical Outcomes. Journal of Clinical Medicine. 2025; 14(9):3234. https://doi.org/10.3390/jcm14093234
Chicago/Turabian StyleHeydar, Ahmed Majid, and Mustafa Kürklü. 2025. "Directly Visualized Carpal Tunnel Release via a Proximal Mini-Transverse Incision: Surgical Technique and Clinical Outcomes" Journal of Clinical Medicine 14, no. 9: 3234. https://doi.org/10.3390/jcm14093234
APA StyleHeydar, A. M., & Kürklü, M. (2025). Directly Visualized Carpal Tunnel Release via a Proximal Mini-Transverse Incision: Surgical Technique and Clinical Outcomes. Journal of Clinical Medicine, 14(9), 3234. https://doi.org/10.3390/jcm14093234







