A Modeling Study for Hip Fracture Rates in Romania
Abstract
1. Introduction
2. Materials and Methods
2.1. Modeling and Data Sources
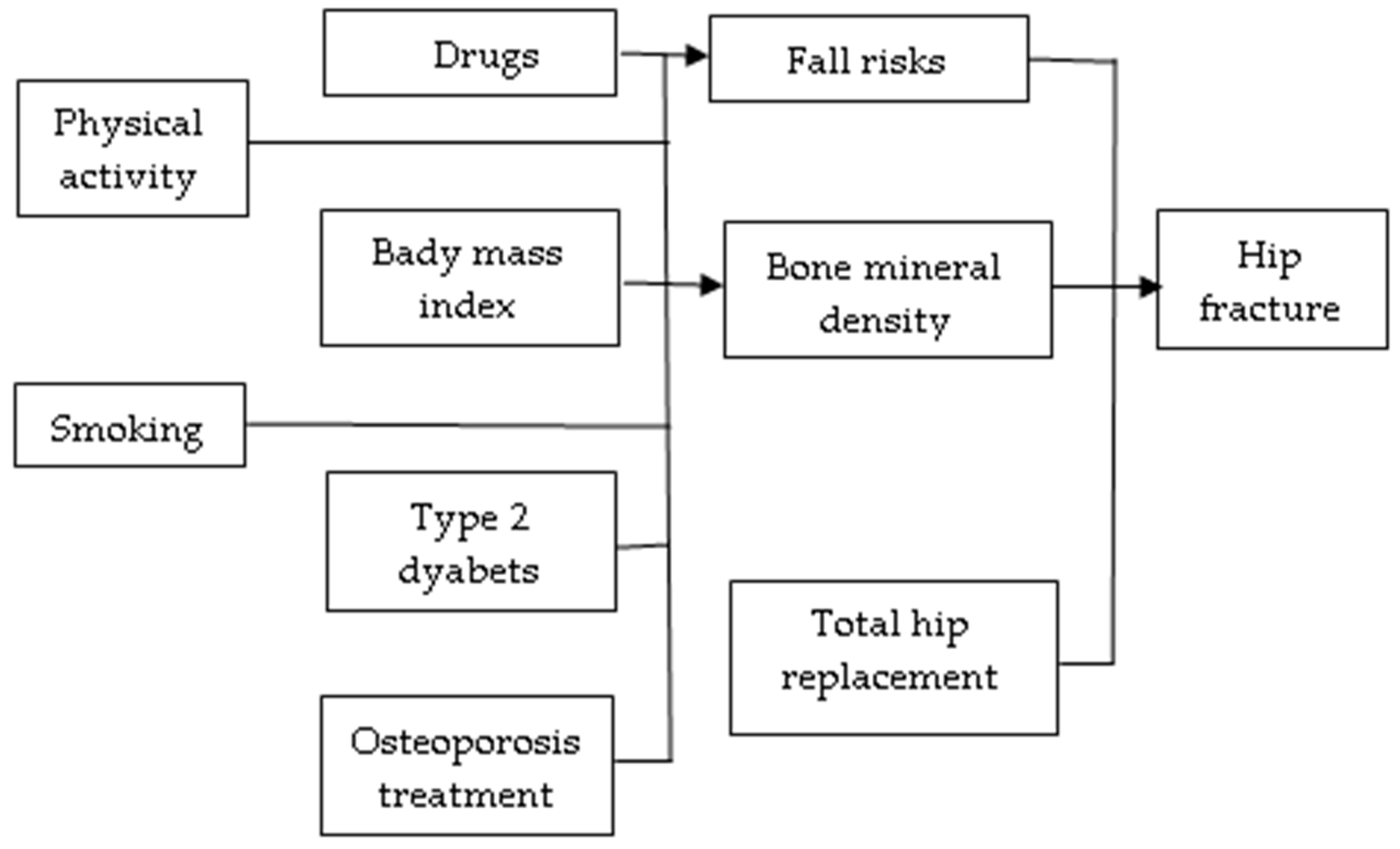
2.2. Selection of Variables
- There is evidence of a causal association with hip fracture (independent (multiple adjusted) RR < 1 or RR > 1), using relative risk estimates for the variable’s association with hip fracture, based on the published scientific literature;
- There are acceptable estimates available to indicate prevalence by sex, in Romania, in 2008 and 2018.
2.3. Expected and Observed Numbers of Hip Fractures
- (a)
- Antiosteoporotic treatments applied to patients diagnosed with osteoporosis (NXmed);
- (b)
- The prevalence of risk factors and preventive measures were calculated based on the variation in the number of hip fractures (NXi) corresponding to the temporal evolution of each factor (Ri), out of a total of n, denoted by NXrisk.
2.4. Component of the Built Model Based on Antiosteoporotic Treatment
2.5. Component of the Built Model Based on Risk Factors
2.6. Data Analysis
3. Results
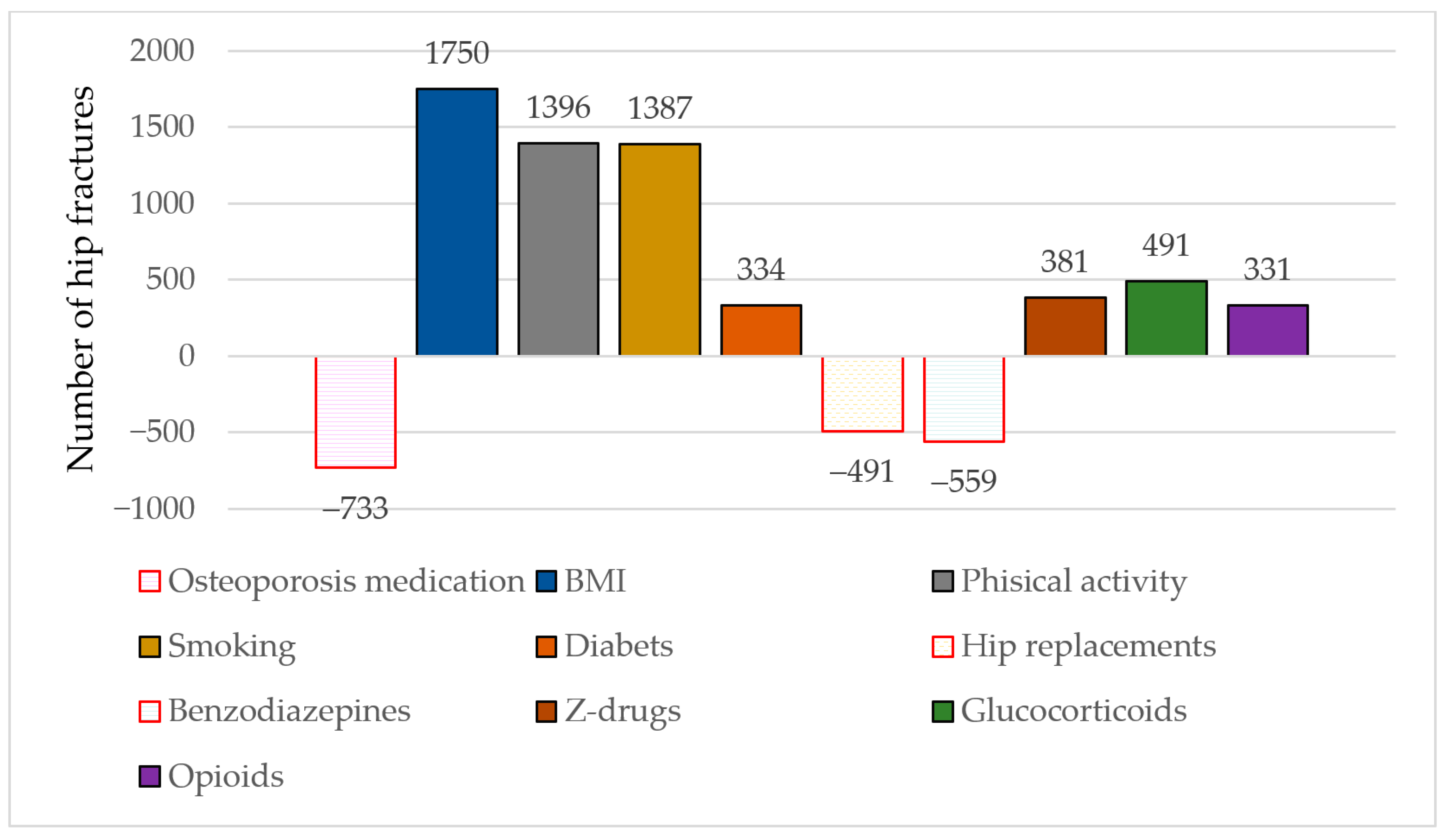
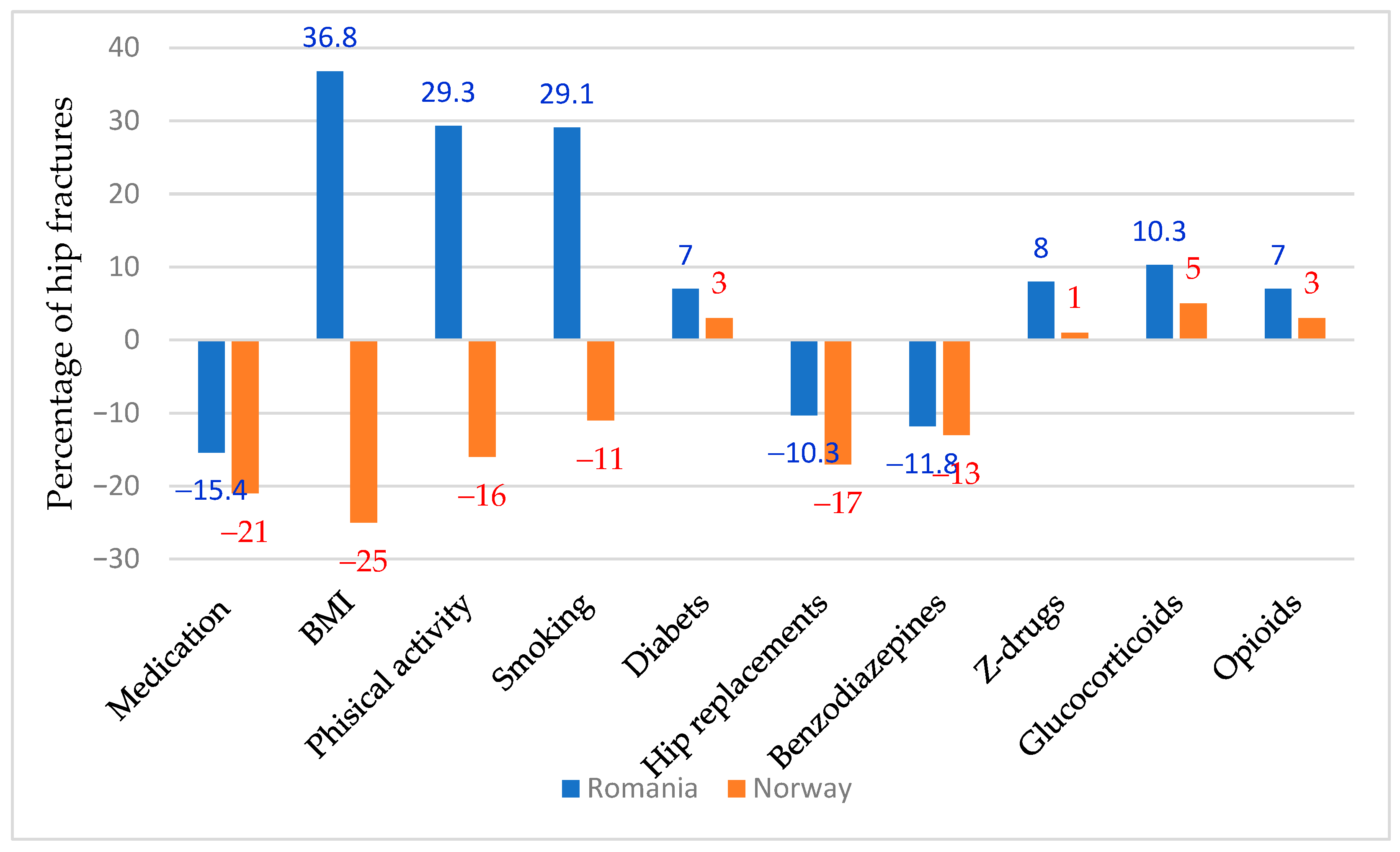
3.1. The Number of Expected Fractures and the Number of Explained Fractures
3.2. Changes in Treatment
3.3. Changes in Risk Factors
3.4. Changes in Drugs with Side Effects
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Treatments | RR (95% CI) |
|---|---|
| Alendronate, high compliance | 0.47 (0.27; 0.81) |
| Alendronate, medium compliance | 0.25 (0.2; 0.3) |
| Zoledronic acid | 0.59 (0.42; 0.83) |
| Denosumab | 0.60 (0.37; 0.97) |
| Risk/preventive factors | RR (95% CI) |
| Body mass index ≥ 25 kg/m2 | Women 50–59: 0.52 (0.40; 0.68) 60–69: 0.66 (0.55; 0.78) 70+: 0.63 (0.57; 0.70) Men 50–59: 0.49 (0.35; 0.68) 60–69: 0.76 (0.62; 0.93) 70+: 0.68 (0.59; 0.77) |
| Physical activity (>1 h/week) | 0.87 (0.8; 0.96) |
| Smoking | Women: 1.30 (1.16; 1.45) Men: 1.47 (1.28; 1.66) |
| Type 2 diabetes | 1.27 (1.16; 1.39) |
| Total hip replacements | 0.50 (0.48; 0.52) |
| Drugs with side effects | |
| Benzodiazepines | 1.52 (1.37; 1.68) |
| Z-drugs | 1.90 (1.68; 2.13) |
| Glucocorticoids | 1.37 (1.28; 1.47) |
| Opioids | 1.54 (1.34; 1.77) |
References
- Al-Khatib, Y.; Dasari, K. Hip Fracture Post-operative Mortality and Polypharmacy: A New Risk Predictor? Cureus 2023, 15, e47089. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.A.; Slart, R.H.J.A.; Ali, D.S.; Bock, O.; Carey, J.J.; Camacho, P.; Engelke, K.; Erba, P.A.; Harvey, N.C.; Lems, W.F.; et al. Osteoporotic Fractures: Diagnosis, Evaluation, and Significance From the International Working Group on DXA Best Practices. Mayo Clin. Proc. 2024, 99, 1127–1141. [Google Scholar] [CrossRef]
- Li, L.; Bennett-Brown, K.; Morgan, C.; Dattani, R. Hip fractures. Br. J. Hosp. Med. 2020, 81, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Buzkova, P.; Cauley, J.A.; Fink, H.A.; Robbins, J.A.; Mukamal, K.J.; Barzilay, J.I. Age-Related Factors Associated With The Risk of Hip Fracture. Endocr. Pract. 2023, 29, 478–483. [Google Scholar] [CrossRef]
- Borgström, F.; Karlsson, L.; Ortsäter, G.; Norton, N.; Halbout, P.; Cooper, C.; Lorentzon, M.; McCloskey, E.V.; Harvey, N.C.; Javaid, M.K.; et al. Fragility fractures in Europe: Burden, management and opportunities. Arch. Osteoporos. 2020, 15, 59. [Google Scholar] [CrossRef] [PubMed]
- Haleem, S.; Choudri, M.J.; Kainth, G.S.; Parker, M.J. Mortality following hip fracture: Trends and geographical variations over the last SIXTY years. Injury 2023, 54, 620–629. [Google Scholar] [CrossRef]
- van Riet-Nales, D.A.; Sundberg, K.; de Boer, A.; Hirschlérova, B. Developing patient-centric medicines for older people: Reflections from the draft EMA paper on the pharmaceutical development of medicines for use in the older population. Br. J. Clin. Pharmacol. 2020, 86, 2008–2013. [Google Scholar] [CrossRef]
- Hjelholt, T.J.; Johnsen, S.P.; Brynningsen, P.K.; Andersen, G.; Pedersen, A.B. Impact of Stroke History on the Risk of Recurrent Hip Fracture or Major Osteoporotic Fractures among Patients with Incident Hip Fracture: A Nationwide Cohort Study. J. Bone Miner. Res. 2023, 38, 278–287. [Google Scholar] [CrossRef]
- Abatzis-Papadopoulos, M.; Tigkiropoulos, K.; Nikas, S.; Papoutsis, I.; Kostopoulou, O.; Stavridis, K.; Karamanos, D.; Lazaridis, I.; Saratzis, N. The effectiveness and safety of direct oral anticoagulants compared to conventional pharmacologic thromboprophylaxis in hip fracture patients: A systematic review and meta-analysis of randomized controlled trials. Orthop. Traumatol. Surg. Res. 2023, 109, 103364. [Google Scholar] [CrossRef]
- Taylor, N.F.; Rimayanti, M.U.; Peiris, C.L.; Snowdon, D.A.; Harding, K.E.; Semciw, A.I.; O’Halloran, P.D.; Wintle, E.; Williams, S.; Shields, N. Hip fracture has profound psychosocial impacts: A systematic review of qualitative studies. Age Ageing. 2024, 53, afae194. [Google Scholar] [CrossRef]
- Kjeldgaard, H.K.; Holvik, K.; Abrahamsen, B.; Tell, G.S.; Meyer, H.E.; O’Flaherty, M. Explaining declining hip fracture rates in Norway: A population-based modelling study. Lancet Reg. Health Eur. 2023, 30, 100643. [Google Scholar] [CrossRef] [PubMed]
- Ford, E.S.; Ajani, U.A.; Croft, J.B.; Critchley, J.A.; Labarthe, D.R.; Kottke, T.E.; Giles, W.H.; Capewell, S. Explaining the decrease in U.S. deaths from coronary disease, 1980–2000. N. Engl. J. Med. 2007, 356, 2388–2398. [Google Scholar] [CrossRef] [PubMed]
- Hotchkiss, J.W.; Davies, C.A.; Dundas, R.; Hawkins, N.; Jhund, P.S.; Scholes, S.; Bajekal, M.; Flaherty, M.O.; Critchley, J.; Leyland, A.H.; et al. Explaining trends in Scottish coronary heart disease mortality between 2000 and 2010 using IMPACTSEC model: Retrospective analysis using routine data. BMJ 2014, 348, g1088. [Google Scholar] [CrossRef] [PubMed]
- Bajekal, M.; Scholes, S.; Love, H.; Hawkins, N.; O’flaherty, M.; Raine, R.; Capewell, S. Analysing Recent Socioeconomic Trends in Coronary Heart Disease Mortality in England, 2000–2007: A Population Modelling Study. PLoS Med. 2012, 9, e1001237. [Google Scholar] [CrossRef]
- Bandosz, P.; O’Flaherty, M.; Drygas, W.; Rutkowski, M.; Koziarek, J.; Wyrzykowski, B.; Bennett, K.; Zdrojewski, T.; Capewell, S. Decline in mortality from coronary heart disease in Poland after socioeconomic transformation: Modelling study. BMJ 2012, 344, d8136. [Google Scholar] [CrossRef]
- Mikolajczyk, T.; Moldovan, L.; Chalupczak, A.; Moldovan, F. Computer Aided Learning Process. Procedia Eng. 2017, 181, 1028–1035. [Google Scholar] [CrossRef]
- Mikolajczyk, T.; Moldovan, F.; Ciobanu, I.; Chalupczak, A.; Georgiana Marin, A. Brain Research Using Computer Test. Procedia Technol. 2016, 22, 1113–1120. [Google Scholar] [CrossRef]
- Moldovan, F. New Approaches and Trends in Health Care. Procedia Manuf. 2018, 22, 947–951. [Google Scholar] [CrossRef]
- Ciobanu, I.; Stanculescu Badea, D.I.; Iliescu, A.; Magdalena Popescu, A.; Seiciu, P.S.; Mikolajczyk, T.; Moldovan, F.; Berteanu, M. The Usability Pilot Study of a Mechatronic System for Gait Rehabilitation. Procedia Manuf. 2018, 22, 864–871. [Google Scholar] [CrossRef]
- Moldovan, F. Recent trends in bioprinting. Procedia Manuf. 2019, 32, 95–101. [Google Scholar] [CrossRef]
- Institutul National de Statistica (National Institute of Statistics). Serii Istorice de Date. Populatia Romaniei 1860–2020 (Historical Data Series. Population of Romania 1860–2020). Available online: https://insse.ro/cms/files/publicatii/Populatia-Romaniei/populatia-romaniei-1860-2020-serii-istorice-de-date.pdf (accessed on 26 March 2025).
- Grigorie, D.; Sucaliuc, A.; Ciutan, M.; Vladescu, C. Incidence and time trend of hip fractures in Romania: A nationwide study from 2008 TO 2018. Acta Endocrinol. 2019, 15, 505–512. [Google Scholar] [CrossRef] [PubMed]
- Dobre, R.; Niculescu, D.A.; Cirstoiu, C.; Popescu, G.; Poiana, C. Osteoporotic Hip Fracture Incidence Rates in the Main Urban Area of Romania. Acta Endocrinol. 2021, 17, 60–67. [Google Scholar] [CrossRef]
- Sacu, C.; Ciutan, M. Analiza episoadelor de spitalizare determinate de osteoporoză în România în perioada 2008-2020 (Analysis of hospitalization episodes due to osteoporosis in Romania in the period 2008–2020). Health Manag. 2021, 4, 18–24. [Google Scholar]
- Moldovan, L.; Gligor, A.; Grif, H.S.; Moldovan, F. Dynamic Numerical Simulation of the 6-PGK Parallel Robot Manipulator. Proc. Rom. Acad. Ser. A 2019, 20, 67–75. [Google Scholar]
- Kanis, J.A.; Johnell, O.; Oden, A.; Jonsson, B.; De Laet, C.; Dawson, A. Risk of hip fracture according to the World Health Organization criteria for osteopenia and osteoporosis. Bone 2000, 27, 585–590. [Google Scholar] [CrossRef]
- NCD Risk Factor Collaboration (NCD-RisC). Heterogeneous contributions of change in population distribution of body mass index to change in obesity and underweight. Elife 2021, 10, e60060. [Google Scholar] [CrossRef] [PubMed]
- Flegal, K.M. Body-mass index and all-cause mortality. Lancet 2017, 389, 2284–2285. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.H.; Yi, S.W.; Yi, J.J.; Kim, Y.M.; Won, Y.J. Association Between Body Mass Index and the Risk of Hip Fracture by Sex and Age: A Prospective Cohort Study. J. Bone Miner. Res. 2018, 33, 1603–1611. [Google Scholar] [CrossRef]
- Xiang, B.Y.; Huang, W.; Zhou, G.Q.; Hu, N.; Chen, H.; Chen, C. Body mass index and the risk of low bone mass-related fractures in women compared with men: A PRISMA-compliant meta-analysis of prospective cohort studies. Medicine 2017, 96, e5290. [Google Scholar] [CrossRef]
- World Obesity. Global Obesity Observatory. Available online: https://data.worldobesity.org/country/romania-178/#data_prevalence (accessed on 26 March 2025).
- Ministerul Sănătății (Ministry of Health). Raportul Național al Stării de Sănătate a Populației (National Report on the HEALTH STATus of the Population). Available online: https://insp.gov.ro/2021/12/29/raportul-national-al-starii-de-sanatate-a-populatiei-2020/ (accessed on 26 March 2025).
- Global Adult Tobacco Study (GATS). FACT SHEET ROMANIA 2018. Available online: https://cdn.who.int/media/docs/default-source/ncds/ncd-surveillance/data-reporting/romania/gats-romania-2018-factsheet.pdf?sfvrsn=2206beb4_1 (accessed on 26 March 2025).
- Global Adult Tobacco Study (GATS) FISA DE COMPARATIE ROMANIA 2011 si 2018 (COMPARISON SHEET ROMANIA 2011 and 2018). Available online: https://insp.gov.ro/download/cnepss/proiecte_si_parteneriate/gats/Informatii-generale-GATS-Romania.pdf (accessed on 26 March 2025).
- The National Endoprosthesis Registry. Available online: https://www.rne.ro/rne/informatii/ (accessed on 26 March 2025).
- Miron, A.A.; Petric, P.S.; Teodorescu, A.; Ifteni, P.; Chele, G.; Szalontay, A.S. Benzodiazepines and Mood Stabilizers in Schizophrenia Patients Treated with Oral versus Long-Acting Injectable Antipsychotics-An Observational Study. Brain Sci. 2023, 13, 173. [Google Scholar] [CrossRef]
- Vasiliu, O. Current evidence and future perspectives in the exploration of sleep-related eating disorder-a systematic literature review. Front. Psychiatry 2024, 15, 1393337. [Google Scholar] [CrossRef]
- Mazilu, D.; Boltasiu Tataru, L.A.; Mardale, D.A.; Bija, M.S.; Ismail, S.; Zanfir, V.; Negoi, F.; Balanescu, A.R. Eosinophilic Fasciitis: Current and Remaining Challenges. Int. J. Mol. Sci. 2023, 24, 1982. [Google Scholar] [CrossRef] [PubMed]
- Sandru, F.; Carsote, M.; Dumitrascu, M.C.; Albu, S.E.; Valea, A. Glucocorticoids and Trabecular Bone Score. J. Med. Life 2020, 13, 449–453. [Google Scholar] [CrossRef] [PubMed]
- Rajnoveanu, R.M.; Harangus, A.; Todea, D.A.; Man, M.A.; Budin, C.E.; Rajnoveanu, A.G. Opioids in Treatment of Refractory Dyspnea in Chronic Obstructive Pulmonary Disease: Yes, No or Maybe. J. Pers. Med. 2024, 14, 318. [Google Scholar] [CrossRef]
- Cismaru, C.A.; Cismaru, G.L.; Nabavi, S.F.; Ghanei, M.; Burz, C.C.; Nabavi, S.M.; Berindan Neagoe, I. Multiple potential targets of opioids in the treatment of acute respiratory distress syndrome from COVID-19. J. Cell Mol. Med. 2021, 25, 591–595. [Google Scholar] [CrossRef]
- Moldovan, F.; Moldovan, L.; Bataga, T. A Comprehensive Research on the Prevalence and Evolution Trend of Orthopedic Surgeries in Romania. Healthcare 2023, 11, 1866. [Google Scholar] [CrossRef] [PubMed]
- Willers, C.; Norton, N.; Harvey, N.C.; Jacobson, T.; Johansson, H.; Lorentzon, M.; McCloskey, E.V.; Borgstrom, F.; Kanis, J.A. SCOPE review panel of the IOF. Osteoporosis in Europe: A compendium of country-specific reports. Arch. Osteoporos. 2022, 17, 23. [Google Scholar] [CrossRef]
- Moldovan, F.; Moldovan, L.; Bataga, T. The Environmental Sustainability Assessment of an Orthopedics Emergency Hospital Supported by a New Innovative Framework. Sustainability 2023, 15, 13402. [Google Scholar] [CrossRef]
- Li, N.; Hiligsmann, M.; Boonen, A.; van Oostwaard, M.M.; de Bot, R.T.A.L.; Wyers, C.E.; Bours, S.P.G.; van den Bergh, J.P. The impact of fracture liaison services on subsequent fractures and mortality: A systematic literature review and meta-analysis. Osteoporos. Int. 2021, 32, 1517–1530. [Google Scholar] [CrossRef]
- Shen, J.; Leslie, W.D.; Nielson, C.M.; Majumdar, S.R.; Morin, S.N.; Orwoll, E.S. Associations of Body Mass Index With Incident Fractures and Hip Structural Parameters in a Large Canadian Cohort. J. Clin. Endocrinol. Metab. 2016, 101, 476–484. [Google Scholar] [CrossRef]
- Mikkila, S.; Johansson, J.; Nordstrom, A.; Nordstrom, P.; Emaus, N.; Handegard, B.H.; Morseth, B.; Welde, B. A 15-year follow-up study of hip bone mineral density and associations with leisure time physical activity. The Tromsø Study 2001–2016. PLoS ONE 2022, 17, e0262228. [Google Scholar] [CrossRef] [PubMed]
- Yuan, S.; Michaelsson, K.; Wan, Z.; Larsson, S.C. Associations of Smoking and Alcohol and Coffee Intake with Fracture and Bone Mineral Density: A Mendelian Randomization Study. Calcif. Tissue Int. 2019, 105, 582–588. [Google Scholar] [CrossRef]
- Sheu, A.; Greenfield, J.R.; White, C.P.; Center, J.R. Assessment and treatment of osteoporosis and fractures in type 2 diabetes. Trends Endocrinol. Metab. 2022, 33, 333–344. [Google Scholar] [CrossRef]
- da Silva, A.V.; Meneghetti, S.M.P.; Meneghetti, M.R. Benzodiazepines: Drugs with Chemical Skeletons Suitable for the Preparation of Metallacycles with Potential Pharmacological Activity. Molecules. 2021, 26, 2796. [Google Scholar] [CrossRef] [PubMed]
- Muehlan, C.; Roch, C.; Vaillant, C.; Dingemanse, J. The orexin story and orexin receptor antagonists for the treatment of insomnia. J. Sleep. Res. 2023, 32, e13902. [Google Scholar] [CrossRef]
- Dautzenberg, L.; Beglinger, S.; Tsokani, S.; Zevgiti, S.; Raijmann, R.C.M.A.; Rodondi, N.; Scholten, R.J.P.M.; Rutjes, A.W.S.; Di Nisio, M.; Emmelot-Vonk, M.; et al. Interventions for preventing falls and fall-related fractures in community-dwelling older adults: A systematic review and network meta-analysis. J. Am. Geriatr. Soc. 2021, 69, 2973–2984. [Google Scholar] [CrossRef] [PubMed]
- GBD 2020 Alcohol Collaborators. Population-level risks of alcohol consumption by amount, geography, age, sex, and year: A systematic analysis for the Global Burden of Disease Study 2020. Lancet 2022, 400, 185–235, Erratum in Lancet 2022, 400, 358. [Google Scholar] [CrossRef]
- Chiodini, I.; Gennari, L. Falls, fractures and vitamin D: A never-ending story? Nat. Rev. Rheumatol. 2019, 15, 6–8. [Google Scholar] [CrossRef]
- Miller, P.D. Underdiagnosis and Undertreatment of Osteoporosis: The Battle to Be Won. J. Clin. Endocrinol. Metab. 2016, 101, 852–859. [Google Scholar] [CrossRef]
- Kirilova, E.; Johansson, H.; Kirilov, N.; Vladeva, S.; Petranova, T.; Kolarov, Z.; Liu, E.; Lorentzon, M.; Vandenput, L.; Harvey, N.C.; et al. Epidemiology of hip fractures in Bulgaria: Development of a country-specific FRAX model. Arch. Osteoporos. 2020, 15, 28. [Google Scholar] [CrossRef]
| Gender | Population in 2008 [Thousands of Inhabitants] | Observed Number of Hip Fractures in 2008 (NO(2008)) | Fracture Rate in 2008 per 10,000 Inhabitants (r(2008)) | Population in 2018 [Thousands of Inhabitants] | Observed Number of Hip Fractures in 2018 (NO(2018)) | Fracture Rate in 2018 per 10,000 Inhabitants (r(2018)) | Expected Number of Fractures in 2018 (NE) | No. of Fractures Requiring Explanation (NXestimated) |
|---|---|---|---|---|---|---|---|---|
| Women | 11,541.5 | 7513 | 6.5 | 11,371 | 11,512 | 10.12 | 7391 95% CI: [7219; 7563] | 4121 95% CI: [3949; 4293] |
| Men | 11,000.5 | 4266 | 3.87 | 11,838 | 5220 | 4.4 | 4581 95% CI: [4442; 4720] | 639 95% CI: [500; 778] |
| Total | 22,542 | 11,779 | 5.22 | 22,209 | 16,732 | 7.53 | 11,972 | 4760 |
| Gender | RR of Hip Fracture per 10,000 People with Osteoporosis a | Fracture Rate in 2008 per 10,000 Inhabitants | Fracture Rate in 2018 per 10,000 Inhabitants | Osteoporosis Hip Fracture Rate per 10,000, in 2008 b | Osteoporosis Hip Fracture Rate per 10,000, in 2018 b | No. of Patients in 2008 | No. of Patients in 2018 | Relative Risk Reduction c | Number of Fractures Explained (+Generated/−Prevented) | % Explained of Total Hip Fractures |
|---|---|---|---|---|---|---|---|---|---|---|
| Best Estimate (Range) | Best Estimate (Range) | |||||||||
| Women | 6.4 | 6.5 | 10.12 | 41.60 | 64.77 | 6586 | 2443 | - | −614 (−722/−521) | −12.9 (−15.1/−10.8) |
| Men | 4.8 | 3.87 | 4.4 | 18.57 | 21.12 | 2092 | 777 | −119 (−139/−101) | −2.5 (−2.8/−2.1) | |
| Total | 8678 | 3220 | 0.53 | −733 (−861/−622) | −15.4 (−17.9/−12.9) |
| Population Risk Factor | Absolute Level of Risk Factor | Change in Risk Factor | Relative Risk | Number of Fractures Explained (+Generated/ −Prevented) | % Explained of Total Hip Fractures | ||
|---|---|---|---|---|---|---|---|
| 2008 | 2018 | Absolute Change | Relative Change (%) | Best Estimate (Range) | Best Estimate (Range) | ||
| BMI > 25 | |||||||
| Women | 55.2 | 61.1 | 5.9 | 10.7 | 0.66 | 1028 (872/1209) | 21.6 (18.1/25.4) |
| Men | 61.9 | 75.1 | 13.2 | 21.3 | 0.76 | 722 (614/848) | 15.2 (12.8/17.6) |
| Total | 58.4 | 67.7 | 9.3 | 15.9 | – | 1750 (1486/2057) | 36.8 (30.9/39.8) |
| Physical activity (%) | |||||||
| Women | 58.1 | 77.0 | 18.9 | 32.5 | 0.87 | 964 (821/1134) | 20.3 (17.2/23.8) |
| Men | 54.3 | 68.2 | 13.9 | 25.6 | 0.87 | 432 (368/508) | 9.1 (7.7/10.7) |
| Total | 57.1 | 73.1 | 16.0 | 28.0 | – | 1396 (1189/1642) | 29.4 (24.9/34.5) |
| Prevalence of smoking (%) | |||||||
| Women | 16.8 | 21.7 | 4.9 | 29.2 | 1.3 | 427 (401/501) | 9.0 (7.6/10.5) |
| Men | 26.8 | 40.4 | 13.6 | 50.8 | 1.47 | 960 (815/1128) | 20.1 (17.1/23.6) |
| Total | 19.6 | 29.1 | 9.5 | 48.5 | – | 1387 (1216/1629) | 29.1 (24.7/34.1) |
| Prevalence of diabetes (%) | |||||||
| Women | 4.2 | 6.1 | 1.9 | 45.2 | 1.27 | 162 (134/189) | 3.4 (2.8/3.9) |
| Men | 6.5 | 9.8 | 3.3 | 50.8 | 1.27 | 172 (144/201) | 3.6 (2.9/4.2) |
| Total | 5.2 | 7.8 | 2.6 | 50.0 | – | 334 (278/390) | 7.0 (5.7/8.1) |
| Total hip replacements (%) | |||||||
| Women | 5.1 | 6.9 | 1.8 | 35.3 | 0.5 | −316 (−371/−268) | −6.6 (−7.4/−5.6) |
| Men | 3.7 | 5.3 | 1.6 | 43.2 | 0.5 | −175 (−204/−147) | −3.6 (−4.2/−2.9) |
| Total | 4.5 | 6.2 | 1.7 | 37.8 | – | −491 (−575/−415) | −10.2 (−11.6/−8.5) |
| Total | – | – | – | – | – | 4376 | 92.0 |
| Population Risk Factor | Absolute Level of Risk Factor | Change in Risk Factor | Relative Risk | Number of Fractures Explained (+Generated/−Prevented) | % Explained of Total Hip Fractures | ||
|---|---|---|---|---|---|---|---|
| 2008 | 2018 | Absolute Change | Relative Change (%) | Best Estimate (Range) | Best Estimate (Range) | ||
| Benzodiazepines | |||||||
| Women | 13.1 | 6.8 | −6.3 | −48.1 | 1.52 | −437 (−553/−369) | −9.2 (−10.8/−7.7) |
| Men | 6.4 | 3.7 | −2.7 | −42.2 | 1.52 | −122 (−142/−102) | −2.6 (−3.1/−2.2) |
| Total | 10.7 | 5.7 | −5.0 | −46.7 | – | −559 (−695/−471) | −11.8 (−13.9/−9.9) |
| Z-drugs | |||||||
| Women | 21.5 | 18.0 | −3.5 | −16.3 | 1.19 | 295 (249/347) | 6.2 (5.3/7.2) |
| Men | 10.5 | 9.1 | −1.4 | −13.3 | 1.19 | 86 (72/99) | 1.8 (1.5/2.1) |
| Total | 16.9 | 14.3 | −2.6 | −15.4 | – | 381 (321/446) | 8.0 (6.8/9.3) |
| Glucocorticoids | |||||||
| Women | 2.9 | 4.7 | 1.8 | 62.1 | 1.37 | 316 (268/369) | 6.6 (5.6/7.7) |
| Men | 2.1 | 3.7 | 1.6 | 76.2 | 1.37 | 175 (148/173) | 3.7 (3.1/4.3) |
| Total | 2.6 | 4.3 | 1.7 | 65.3 | – | 491 (416/542) | 10.3 (8.7/12.0) |
| Opioids | |||||||
| Women | 16.4 | 17.2 | 0.8 | 4.9 | 1.54 | 177 (149/208) | 3.7 (3.1/4.3) |
| Men | 13.9 | 15.0 | 1.1 | 7.9 | 1.54 | 154 (129/181) | 3.2 (2.7/3.7) |
| Total | 15.7 | 16.4 | 0.7 | 4.5 | – | 331 (278/389) | 7.0 (5.8/8.0) |
| Total | 644 | 13.5 | |||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moldovan, F.; Moldovan, L. A Modeling Study for Hip Fracture Rates in Romania. J. Clin. Med. 2025, 14, 3162. https://doi.org/10.3390/jcm14093162
Moldovan F, Moldovan L. A Modeling Study for Hip Fracture Rates in Romania. Journal of Clinical Medicine. 2025; 14(9):3162. https://doi.org/10.3390/jcm14093162
Chicago/Turabian StyleMoldovan, Flaviu, and Liviu Moldovan. 2025. "A Modeling Study for Hip Fracture Rates in Romania" Journal of Clinical Medicine 14, no. 9: 3162. https://doi.org/10.3390/jcm14093162
APA StyleMoldovan, F., & Moldovan, L. (2025). A Modeling Study for Hip Fracture Rates in Romania. Journal of Clinical Medicine, 14(9), 3162. https://doi.org/10.3390/jcm14093162







