A Comparison of Two Fascial Plane Blocks for Abdominal Analgesia in Laparoscopic Cholecystectomy Surgery (M-TAPA vs. External Oblique Intercostal Plane Block): A Prospective Randomized Study
Abstract
1. Introduction
2. Materials and Methods
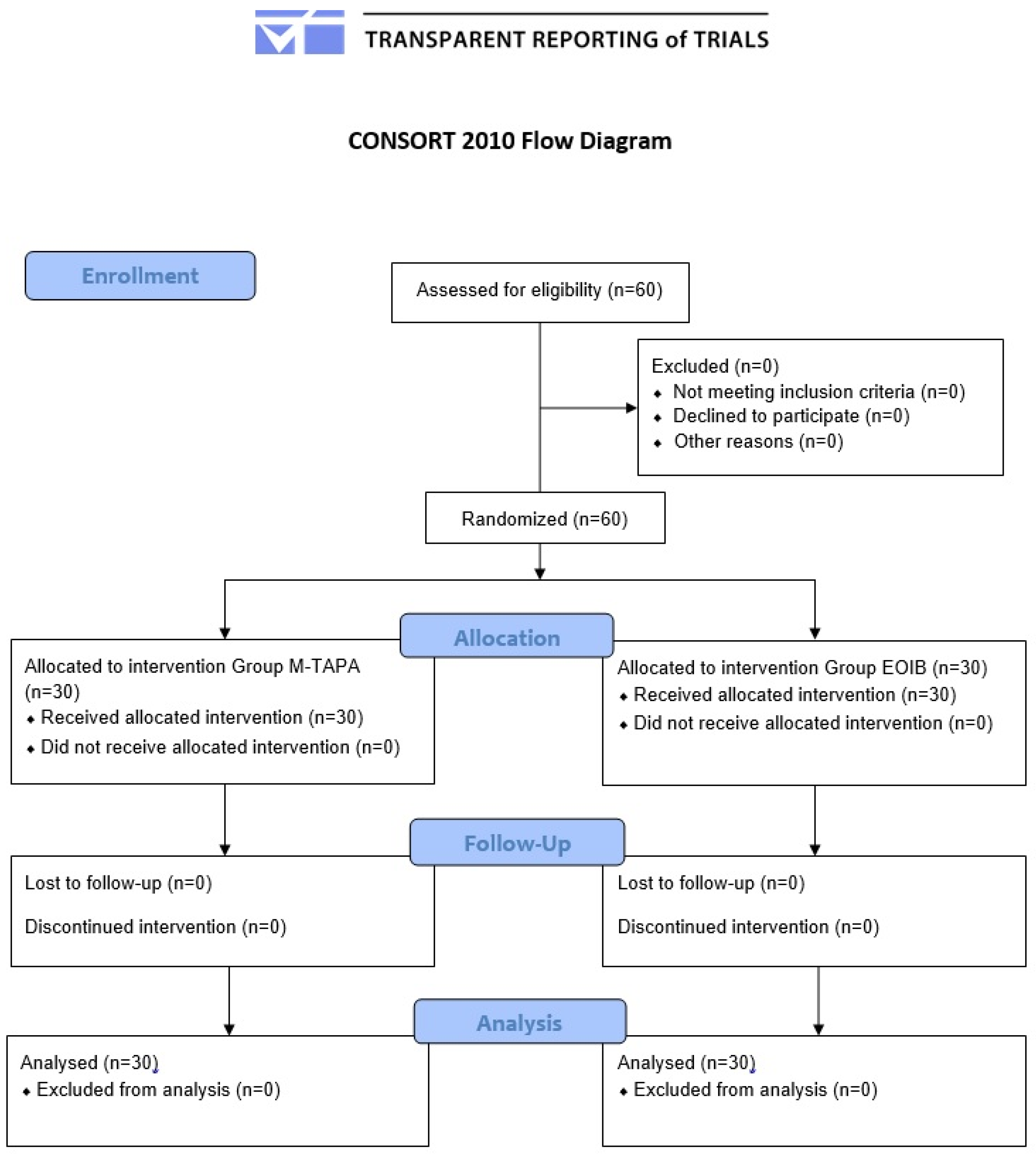
2.1. Study Design and Patient Population
2.2. Grouping, Randomization, and Blinding
2.3. Anesthesia Management and Surgical Technique
2.4. Interfascial Plane Block Procedures
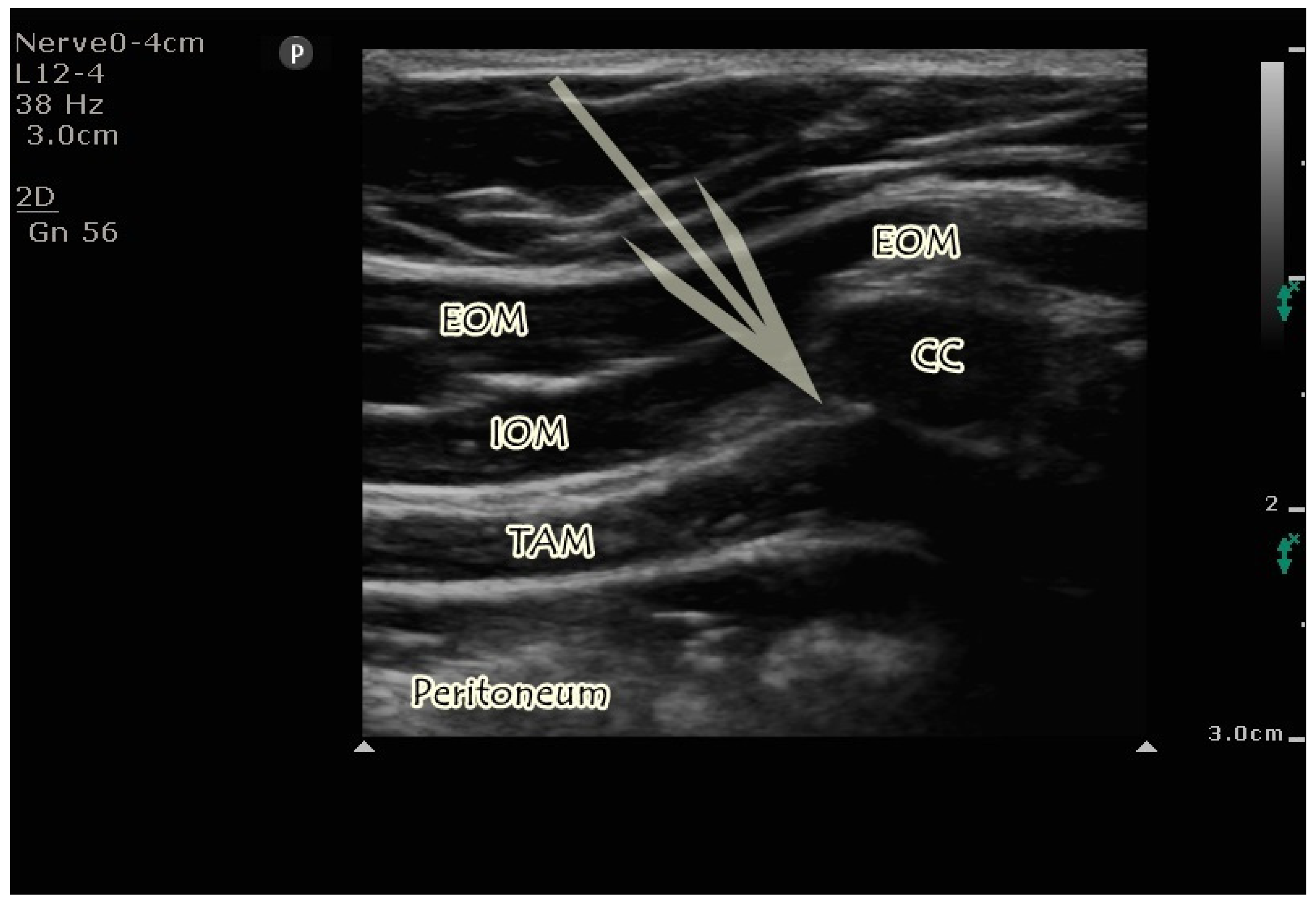
2.4.1. US-Guided M-TAPA Block
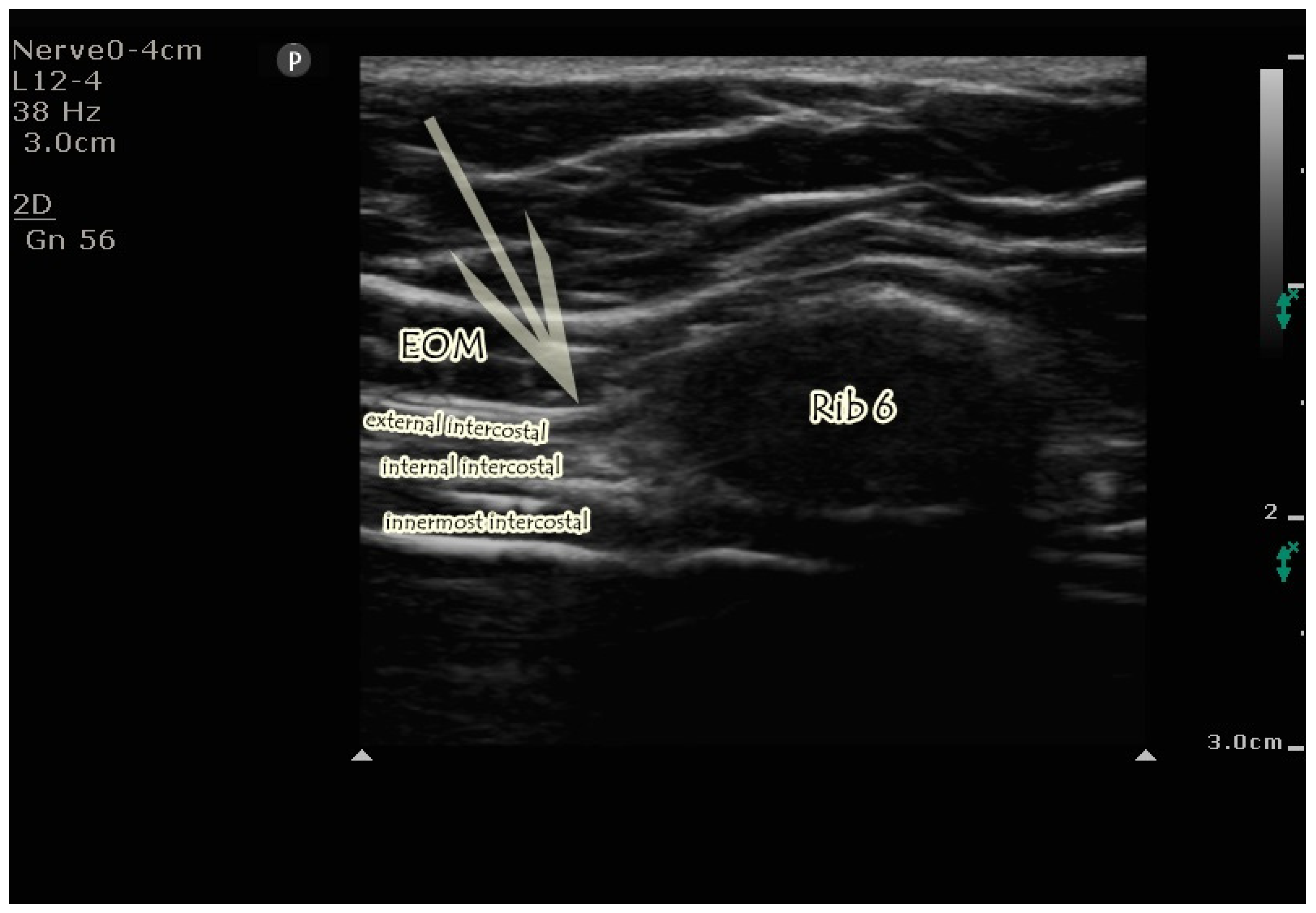
2.4.2. US-Guided EOIB
2.5. Postoperative Analgesia Management and Outcomes
2.6. Sample Size
2.7. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kapoor, T.; Wrenn, S.M.; Callas, P.W.; Abu-Jaish, W. Cost Analysis and Supply Utilization of Laparoscopic Cholecystectomy. Minim. Invasive Surg. 2018, 2018, 7838103. [Google Scholar] [CrossRef] [PubMed]
- Mitra, S.; Khandelwal, P.; Roberts, K.; Kumar, S.; Vadivelu, N. Pain relief in laparoscopic cholecystectomy--a review of the current options. Pain Pract. 2012, 12, 485–496. [Google Scholar] [CrossRef] [PubMed]
- Wills, V.L.; Hunt, D.R. Pain after laparoscopic cholecystectomy. Br. J. Surg. 2000, 87, 273–284. [Google Scholar] [CrossRef] [PubMed]
- Blichfeldt-Eckhardt, M.R.; Ording, H.; Andersen, C.; Licht, P.B.; Toft, P. Early visceral pain predicts chronic pain after laparoscopic cholecystectomy. Pain 2014, 155, 2400–2407. [Google Scholar] [CrossRef]
- Zewdu, D.; Tantu, T.; Eanga, S.; Tilahun, T. Analgesic efficacy of erector spinae plane block versus transversus abdominis plane block for laparoscopic cholecystectomy: A systematic review and meta-analysis of randomized controlled trial. Front. Med. 2024, 11, 1399253. [Google Scholar] [CrossRef]
- Bourgeois, C.; Oyaert, L.; Van de Velde, M.; Pogatzki-Zahn, E.; Freys, S.M.; Sauter, A.R.; Joshi, G.P.; Dewinter, G.; PROSPECT working Group of the European Society of Regional Anaesthesia and Pain Therapy (ESRA). Pain management after laparoscopic cholecystectomy: A systematic review and procedure-specific postoperative pain management (PROSPECT) recommendations. Eur. J. Anaesthesiol. 2024, 41, 841–855. [Google Scholar] [CrossRef] [PubMed]
- Tulgar, S.; Selvi, O.; Thomas, D.T.; Deveci, U.; Özer, Z. Modified thoracoabdominal nerves block through perichondrial approach (M-TAPA) provides effective analgesia in abdominal surgery and is a choice for opioid sparing anesthesia. J. Clin. Anesth. 2019, 55, 109. [Google Scholar] [CrossRef]
- Elsharkawy, H.; Kolli, S.; Soliman, L.M.; Seif, J.; Drake, R.L.; Mariano, E.R.; El-Boghdadly, K. The External Oblique Intercostal Block: Anatomic Evaluation and Case Series. Pain Med. 2021, 22, 2436–2442. [Google Scholar] [CrossRef] [PubMed]
- Tulgar, S.; Ahiskalioglu, A.; Selvi, O.; Thomas, D.T.; Ozer, Z. Similarities between external oblique fascial plane block and blockage of thoracoabdominal nerves through perichondral approach (TAPA). J. Clin. Anesth. 2019, 57, 91–92. [Google Scholar] [CrossRef]
- Ohgoshi, Y.; Kawagoe, I.; Ando, A.; Ikegami, M.; Hanai, S.; Ichimura, K. Novel external oblique muscle plane block for blockade of the lateral abdominal wall: A pilot study on volunteers. Can. J. Anaesth. 2022, 69, 1203–1210. [Google Scholar] [CrossRef]
- Tulgar, S. Comments on blockade of thoracoabdominal nerves through the perichondrial approach. Can. J. Anaesth. 2024, 71, 921–922. [Google Scholar] [CrossRef]
- Alver, S.; Ciftci, B.; Güngör, H.; Gölboyu, B.E.; Ozdenkaya, Y.; Alici, H.A.; Tulgar, S. Efficacy of modified thoracoabdominal nerve block through perichondrial approach following laparoscopic inguinal hernia repair surgery: A randomized controlled trial. Braz. J. Anesthesiol. 2023, 73, 595–602. [Google Scholar] [CrossRef]
- Hamilton, D.L.; Manickam, B.P.; Wilson, M.A.J.; Abdel Meguid, E. External oblique fascial plane block. Reg. Anesth. Pain Med. 2019, 44, 528–529. [Google Scholar] [CrossRef]
- Korkusuz, M.; Basaran, B.; Et, T.; Bilge, A.; Yarimoglu, R.; Yildirim, H. Bilateral external oblique intercostal plane block (EOIPB) in patients undergoing laparoscopic cholecystectomy: A randomized controlled trial. Saudi Med. J. 2023, 44, 1037–1046. [Google Scholar] [CrossRef]
- Avci, O.; Gundogdu, O.; Balci, F.; Tekcan, M.N. Effects of Modified Thoracoabdominal Nerve Block Through Perichondrial Approach on Postoperative Pain and Analgaesic Consumption in Patients Undergoing Laparoscopic Cholecystectomy. J. Coll. Physicians Surg. Pak. 2024, 34, 5–10. [Google Scholar] [CrossRef] [PubMed]
- Güngör, H.; Ciftci, B.; Alver, S.; Gölboyu, B.E.; Ozdenkaya, Y.; Tulgar, S. Modified thoracoabdominal nerve block through perichondrial approach (M-TAPA) vs local infiltration for pain management after laparoscopic cholecystectomy surgery: A randomized study. J. Anesth. 2023, 37, 254–260. [Google Scholar] [CrossRef]
- Bilge, A.; Başaran, B.; Et, T.; Korkusuz, M.; Yarımoğlu, R.; Toprak, H.; Kumru, N. Ultrasound-guided bilateral modified-thoracoabdominal nerve block through a perichondrial approach (M-TAPA) in patients undergoing laparoscopic cholecystectomy: A randomized double-blind controlled trial. BMC Anesthesiol. 2022, 22, 329. [Google Scholar] [CrossRef]
- Doymus, O.; Ahiskalioglu, A.; Kaciroglu, A.; Bedir, Z.; Tayar, S.; Yeni, M.; Karadeniz, E. External Oblique Intercostal Plane Block Versus Port-Site Infiltration for Laparoscopic Sleeve Gastrectomy: A Randomized Controlled Study. Obes. Surg. 2024, 34, 1826–1833. [Google Scholar] [CrossRef]
- Turunc, E.; Dost, B.; Sarikaya Ozel, E.; Kaya, C.; Ustun, Y.B.; Bilgin, S.; Ozbalci, G.S.; Koksal, E. Bilateral Ultrasound-Guided External Oblique Intercostal Block Vs. Modified Thoracoabdominal Nerve Block Through Perichondrial Approach for Postoperative Analgesia in Patients Undergoing Laparoscopic Sleeve Gastrectomy Surgery: A Randomized Controlled Study. Obes Surg. 2024, 34, 3726–3734. [Google Scholar] [CrossRef]
- Chin, K.J.; McDonnell, J.G.; Carvalho, B.; Sharkey, A.; Pawa, A.; Gadsden, J. Essentials of Our Current Understanding: Abdominal Wall Blocks. Reg. Anesth. Pain 2017, 42, 133–183. [Google Scholar] [CrossRef]
- Ohgoshi, Y.; Anetai, H.; Hanai, S.; Ichimura, K.; Kawagoe, I. The key to success in blocking lateral cutaneous branches with re-modified thoracoabdominal nerves block through perichondrial approach: A newly discovered space between the endothoracic fascia, diaphragm, and costodiaphragmatic recess. J. Anesth. 2024, 38, 642–649. [Google Scholar] [CrossRef]
- Aikawa, K.; Yokota, I.; Maeda, Y.; Morimoto, Y. Evaluation of sensory loss obtained by modified-thoracoabdominal nerves block through perichondrial approach in patients undergoing gynecological laparoscopic surgery: A prospective observational study. Reg. Anesth. Pain Med. 2022, 47, 134–135. [Google Scholar] [CrossRef]
- Zinboonyahgoon, N.; Luksanapruksa, P.; Piyaselakul, S.; Pangthipampai, P.; Lohasammakul, S.; Luansritisakul, C.; Mali-Ong, S.; Sateantantikul, N.; Chueaboonchai, T.; Vlassakov, K. The ultrasound-guided proximal intercostal block: Anatomical study and clinical correlation to analgesia for breast surgery. BMC Anesthesiol. 2019, 19, 94. [Google Scholar] [CrossRef]
- Tanaka, N.; Suzuka, T.; Kadoya, Y.; Okamoto, N.; Sato, M.; Kawanishi, H.; Azuma, C.; Nishi, M.; Kawaguchi, M. Efficacy of modified thoracoabdominal nerves block through perichondrial approach in open gynecological surgery: A prospective observational pilot study and a cadaveric evaluation. BMC Anesthesiol. 2022, 22, 107. [Google Scholar] [CrossRef]
- Çiftçi, B.; Güngör, H.; Alver, S.; Akın, A.N.; Özdenkaya, Y.; Tulgar, S. Clinical Experience for Modified Thoracoabdominal Nerve Block Through Perichondrial Approach (M-TAPA) in Five Patients. Dermatomal Evaluation and Application of Different Volumes: A Case Series and Review of Literature. Turk. J. Anaesthesiol. Reanim. 2023, 51, 354–357. [Google Scholar] [CrossRef]
- Ciftci, B.; Alici, H.A.; Ansen, G.; Sakul, B.U.; Tulgar, S. Cadaveric investigation of the spread of the thoracoabdominal nerve block using the perichondral and modified perichondral approaches. Korean J. Anesthesiol. 2022, 75, 357–359. [Google Scholar] [CrossRef]
- de Oliveira, E.J.S.G.; De Lima, R.C.; Sakata, R.K.; Freire, T.T.; de Almeida Lima, E.L.; de Oliveira, C.M.B.; Moura, E.C.R.; da Cunha Leal, P. Modified Thoracoabdominal Nerve Block Through the Perichondral Approach (M-TAPA) in Laparoscopic Sleeve Gastroplasty: A Case Series. Obes. Surg. 2022, 32, 197–201. [Google Scholar] [CrossRef] [PubMed]
- Aikawa, K.; Tanaka, N.; Morimoto, Y. Modified thoracoabdominal nerves block through perichondrial approach (M-TAPA) provides a sufficient postoperative analgesia for laparoscopic sleeve gastrectomy. J. Clin. Anesth. 2020, 59, 44–45. [Google Scholar] [CrossRef] [PubMed]
- Gurbuz, H.; Ekinci, M.; Kaciroglu, A. Modified thoracoabdominal nerves block through perichondrial approach (M-TAPA) for nephrectomy in children. Paediatr. Anaesth. 2024, 34, 1162–1164. [Google Scholar] [CrossRef] [PubMed]
- Matsuura, H.; Terada, Y.; Rokkaku, Y.; Tamagawa, H.; Taniguchi, E.; Saito, Y.; Tsujimura, N.; Tanaka, N.; Kawaguchi, M. Analgesic efficacy of modified thoracoabdominal nerves block through the perichondrial approach in laparoscopic cholecystectomy: A retrospective study with propensity analysis. Asian J. Endosc. Surg. 2023, 16, 648–652. [Google Scholar] [CrossRef] [PubMed]
- Castillo-Dávila, L.F.; Torres-Anaya, C.J.; Vazquez-Apodaca, R.; Borboa-Olivares, H.; Espino-Y-Sosa, S.; Torres-Torres, J. Modified thoracoabdominal nerve block via perichondral approach: An alternative for perioperative pain management in laparoscopic cholecystectomy in a middle-income country. BMC Anesthesiol. 2024, 24, 304. [Google Scholar] [CrossRef]
- Mehmet Selim, Ç.; Halide, S.; Erkan Cem, Ç.; Onur, K.; Sedat, H.; Senem, U. Efficacy of Unilateral External Oblique Intercostal Fascial Plane Block Versus Subcostal TAP Block in Laparoscopic Cholecystectomy: Randomized, Prospective Study. Surg. Innov. 2024, 31, 381–388. [Google Scholar] [CrossRef]
- Erskine, R.N.; White, L. A review of the external oblique intercostal plane block—A novel approach to analgesia for upper abdominal surgery. J. Clin. Anesth. 2022, 82, 110953. [Google Scholar] [CrossRef] [PubMed]
- White, L.; Ji, A. External oblique intercostal plane block for upper abdominal surgery: Use in obese patients. Br. J. Anaesth. 2022, 128, e295–e297. [Google Scholar] [CrossRef] [PubMed]
- Kavakli, A.S.; Sahin, T.; Koc, U.; Karaveli, A. Ultrasound-Guided External Oblique Intercostal Plane Block for Postoperative Analgesia in Laparoscopic Sleeve Gastrectomy: A Prospective, Randomized, Controlled, Patient and Observer-Blinded Study. Obes. Surg. 2024, 34, 1505–1512. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Fusco, P.; Pascarella, G.; Stecco, C.; Blanco, R.; Forero, M.; Pawa, A.; Tulgar, S.; Strumia, A.; Remore, L.M.; De Cassai, A.; et al. Factors to consider for fascial plane blocks’ success in acute and chronic pain management. Minerva Anestesiol. 2024, 90, 87–97. [Google Scholar] [CrossRef]
- Maximos, S.; Vaillancourt-Jean, É.; Mouksassi, S.; De Cassai, A.; Ayoub, S.; Ruel, M.; Desroches, J.; Hétu, P.O.; Moore, A.; Williams, S. Peak plasma concentration of total and free bupivacaine after erector spinae plane and pectointercostal fascial plane blocks. Can. J. Anaesth. 2022, 69, 1151–1159. [Google Scholar] [CrossRef]
| Group EOIB (n = 30) | Group M-TAPA (n = 30) | p | |
|---|---|---|---|
| Age | 44 (37–48) | 46 (37–52) | * 0.684 |
| Gender (M/F) | 13/17 | 16/14 | † 1 |
| ASA (I/II) | 14/16 | 10/20 | † 0.430 |
| Height (cm) | 170 (161–177) | 169 (162–174) | * 0.796 |
| Weight (kg) | 81 (65–87) | 78 (73–86) | * 0.589 |
| Surgery length (min) | 78 (65–99) | 75 (65–91) | * 0.695 |
| Anesthesia length (min) | 94 (78–113) | 90 (78–108) | * 0.673 |
| Group EOIB (n = 30) | Group M-TAPA (n = 30) | p | |
|---|---|---|---|
| At rest | |||
| 1st hour | 1 (0–2) | 0 (0–1) | 0.019 |
| 2nd hour | 1 (1–3) | 1 (0–1) | 0.015 |
| 4th hour | 1 (1–2) | 1 (0–2) | 0.066 |
| 8th hour | 1 (0–2) | 1 (0–2) | 0.381 |
| 16th hour | 1 (0–1) | 0 (0–1) | 0.177 |
| 24th hour | 0 (0–1) | 0 (0–1) | 0.736 |
| During movement | |||
| 1st hour | 2 (1–3) | 1 (0–2) | 0.045 |
| 2nd hour | 3 (1–3) | 1 (0–2) | 0.042 |
| 4th hour | 2 (1–2) | 2 (1–2) | 0.085 |
| 8th hour | 2 (1–2) | 1 (0–2) | 0.341 |
| 16th hour | 1 (0–2) | 1 (0–1) | 0.211 |
| 24th hour | 0 (0–1) | 0 (0–1) | 0.910 |
| Group EOIB (n = 30) | Group M-TAPA (n = 30) | p | |
|---|---|---|---|
| Rescue analgesia (Y/N) | 12/18 | 5/25 | 0.043 |
| Rescue dose (mg) | 0 (0–60) | 0 (0–0) | * 0.046 |
| Group EOIB (n = 30) | MTAPA Block (n = 30) | p | |
|---|---|---|---|
| Nausea (Y/N) | 10/20 | 5/25 | 0.136 |
| Vomiting (Y/N) | 4/26 | 3/27 | 1 |
| Itching (Y/N) | 6/24 | 2/28 | 0.254 |
| Postoperative QoR-15 | 138 (128–140) | 139 (137–140) | * 0.062 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ciftci, B.; Alver, S.; Gölboyu, B.E.; Haksal, M.C.; Tulgar, S.; De Cassai, A.; Alici, H.A. A Comparison of Two Fascial Plane Blocks for Abdominal Analgesia in Laparoscopic Cholecystectomy Surgery (M-TAPA vs. External Oblique Intercostal Plane Block): A Prospective Randomized Study. J. Clin. Med. 2025, 14, 3050. https://doi.org/10.3390/jcm14093050
Ciftci B, Alver S, Gölboyu BE, Haksal MC, Tulgar S, De Cassai A, Alici HA. A Comparison of Two Fascial Plane Blocks for Abdominal Analgesia in Laparoscopic Cholecystectomy Surgery (M-TAPA vs. External Oblique Intercostal Plane Block): A Prospective Randomized Study. Journal of Clinical Medicine. 2025; 14(9):3050. https://doi.org/10.3390/jcm14093050
Chicago/Turabian StyleCiftci, Bahadir, Selcuk Alver, Birzat Emre Gölboyu, Mustafa Celalettin Haksal, Serkan Tulgar, Alessandro De Cassai, and Haci Ahmet Alici. 2025. "A Comparison of Two Fascial Plane Blocks for Abdominal Analgesia in Laparoscopic Cholecystectomy Surgery (M-TAPA vs. External Oblique Intercostal Plane Block): A Prospective Randomized Study" Journal of Clinical Medicine 14, no. 9: 3050. https://doi.org/10.3390/jcm14093050
APA StyleCiftci, B., Alver, S., Gölboyu, B. E., Haksal, M. C., Tulgar, S., De Cassai, A., & Alici, H. A. (2025). A Comparison of Two Fascial Plane Blocks for Abdominal Analgesia in Laparoscopic Cholecystectomy Surgery (M-TAPA vs. External Oblique Intercostal Plane Block): A Prospective Randomized Study. Journal of Clinical Medicine, 14(9), 3050. https://doi.org/10.3390/jcm14093050






