Factors Determining the Burden of a Caregiver Providing Care to a Post-Stroke Patient
Abstract
1. Introduction
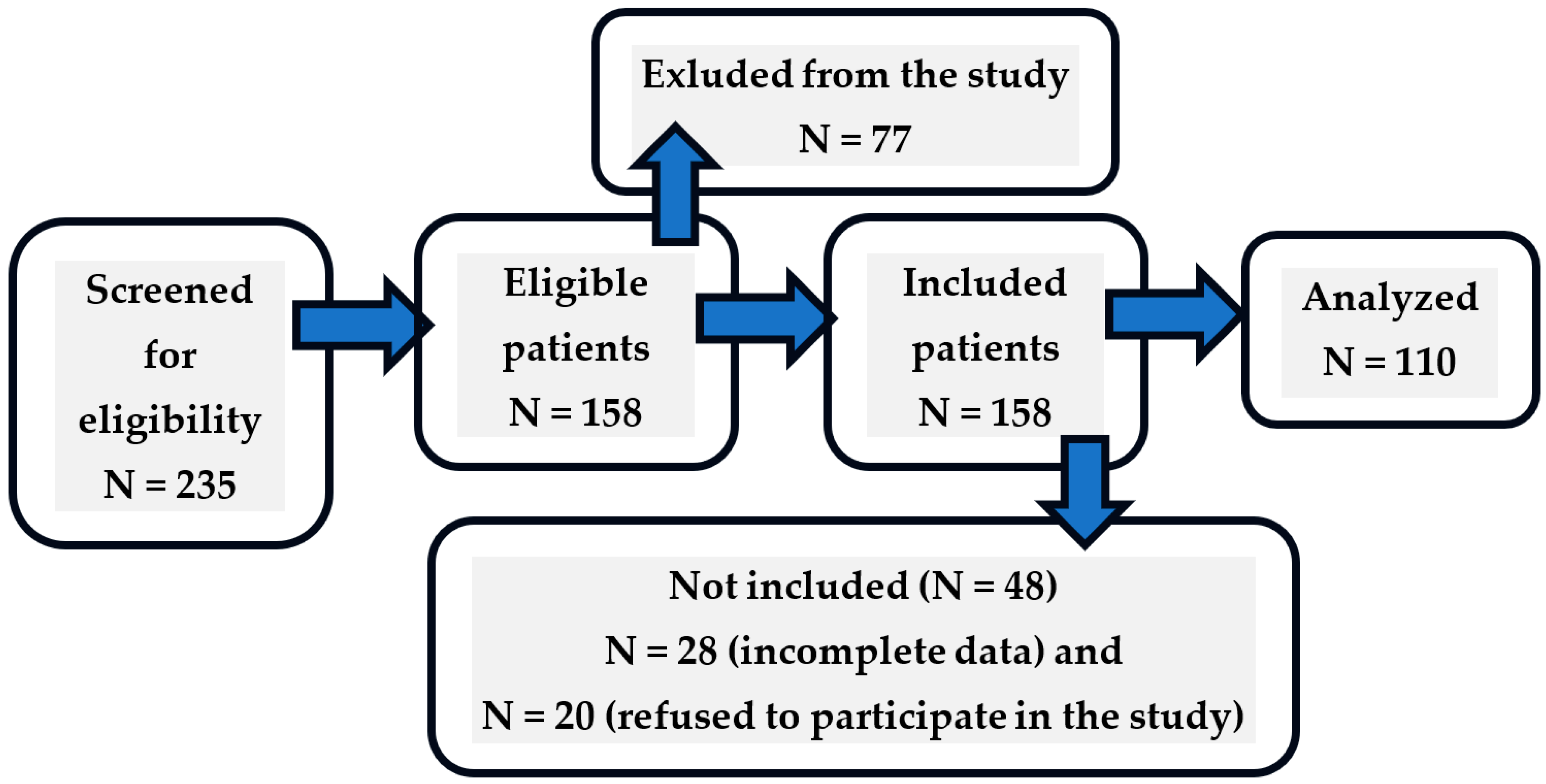
2. Materials and Methods
2.1. Organization of the Study
2.2. Inclusion and Exclusion Criteria
- The Caregiver Burden Scale (CBS) scale using a 22-item scale that was developed in Sweden [15] and is divided into five components as a result of the previous factor analysis: general strain, isolation, disappointment, emotional involvement, and environment. The items are scored from 1 to 4 (never, rarely, sometimes, and always, respectively) and cover questions about caregivers’ health, feelings of psychological well-being, relationships, social networks, physical workload, and environmental aspects. The total burden index consists of the average of all 22 items, with higher scores indicating a greater level of burden. In accordance with the recommendations of the scale’s authors, the following load categories were adopted: low (1.00–1.99 points), medium (2.00–2.99 points), and high (3.00–4.00 points). The results proved to have good design accuracy. There was adequate internal consistency for all subscales (α-Cronbach = 0.70–0.87), and the research by Jaracz et.al.: α-Cronbach = 0.92 [16]. Own research: α-Cronbach = 0.96;
- For information on the caregiver’s perception of QoL, the World Health Organization Quality of Life (WHOQOL-BREF) questionnaire was used. This instrument consists of four domains and aims to verify psychological well-being, physical capacity, social relationships, and the environment where the individual is inserted, containing a total of 26 questions. It also presents two more general questions about QoL. Higher scores indicate a better QoL. Responses were rated on a 5-point Likert scale [17]. Own research: α-Cronbach = 0.94;
- Beck Depression Inventory (BDI) The BDI is a 21-point screening questionnaire that is used to assess the severity of mood disorder (depression) symptoms. The scale consists of 21 questions that score from 0 to 3 points. The results that can be obtained in the BDI range from 0 to 63. The BDI is a questionnaire that has been standardized and validated to Polish conditions, and it is repeatedly used in studies to assess mood disorders [18]. Own research: α-Cronbach = 0.92;
- To assess the intensity of perceived stress among caregivers, we used the Polish adaptation of the Perceived Stress Scale (PPS-10) questionnaire [19], the original version of which was developed by Cohen et al. [20] and which contains 10 questions on various subjective feelings related to personal problems and events, behaviors, and ways of coping. In order to compare the results of the surveys, the overall PSS-10 scores were normalized (based on [19]), which took into account gender, age, education level, and occupation. The surveys were conducted in various locations in Central Poland. The normalization was carried out on a sample of healthy people numbering 1830. The respondents gave their answers by writing the appropriate number (0—never, 1—almost never, 2—sometimes, 3—quite often, 4—very often). The overall score of the scale is the sum of all the scores, the theoretical distribution of which is from 0 to 40. The higher the score, the greater the severity of the perceived stress. The overall index, after conversion to standardized units, is subject to interpretation according to the properties that characterize the so-called stena scale i.e., values on a scale of 1–10. Scores within 1–4 stena are treated as low scores, while scores within 7–10 stena are treated as high scores. Scores within 5–6 stena are treated as average, α-Cronbach’s > 70 [21]. Own research: α-Cronbach = 0.70;
- The Polish adaptation of the Mini-COPE questionnaire—a shortened version of the Coping Inventory-Mini-COPE [19], the original version of which was developed by C. S. Carver [22]—was used to measure coping strategies. The questionnaire is an abbreviated version of the Multidimensional Coping Inventory-COPE and consists of 28 statements comprising 14 coping strategies. Each scale includes 2 statements and 5 groups of strategies, to which the respondent responds on a scale from 0 (I almost never do this) to 3 (I almost always do this). The higher the score, the more often the respondent uses a particular strategy. Own research: α-Cronbach = 0.75;
- The modified Rankin Scale was used to measure the disability of post-stroke individuals. This scale has six categories ranging from 0 (no symptoms) to 5 (severe disability) [23]. It is a systematic method of assessing the patient’s ability, identifying skills or deficiencies in self-care. The modified Rankin Scale is a simple instrument with good acceptability for measuring the level of functional recovery of post-stroke individuals and used as a scale for activities of daily living (ADL). The participants’ sociodemographic data and the patients’ clinical information were gathered from the medical records and with the help of a semi-structured questionnaire.
- The Abbreviated Mental Test Score (AMTS), is a tool designed for the assessment of cognitive functions.;It consists of 10 short tasks—questions and commands addressed to the subject. For a correct answer or execution of a command, the examinee receives 1 point. The maximum number of points possible is 10, the minimum—0. On the basis of the obtained score, the efficiency of the cognitive functions of the person examined is assessed, classifying them into one of three levels of mental efficiency: a score of 7–10 points means a normal state, a score of 4–6 points—moderate impairment, and a score of 0–3 points—severe impairment of cognitive functions. The Polish adaptation of the questionnaire was used [24], the original version of which was developed by [25].
2.3. Statistical Methods
3. Results
3.1. Participant Characteristics Patients/Caregivers
3.2. Caregiver Burden According to CBS Scale
3.3. Determinants of Caregiver Burden
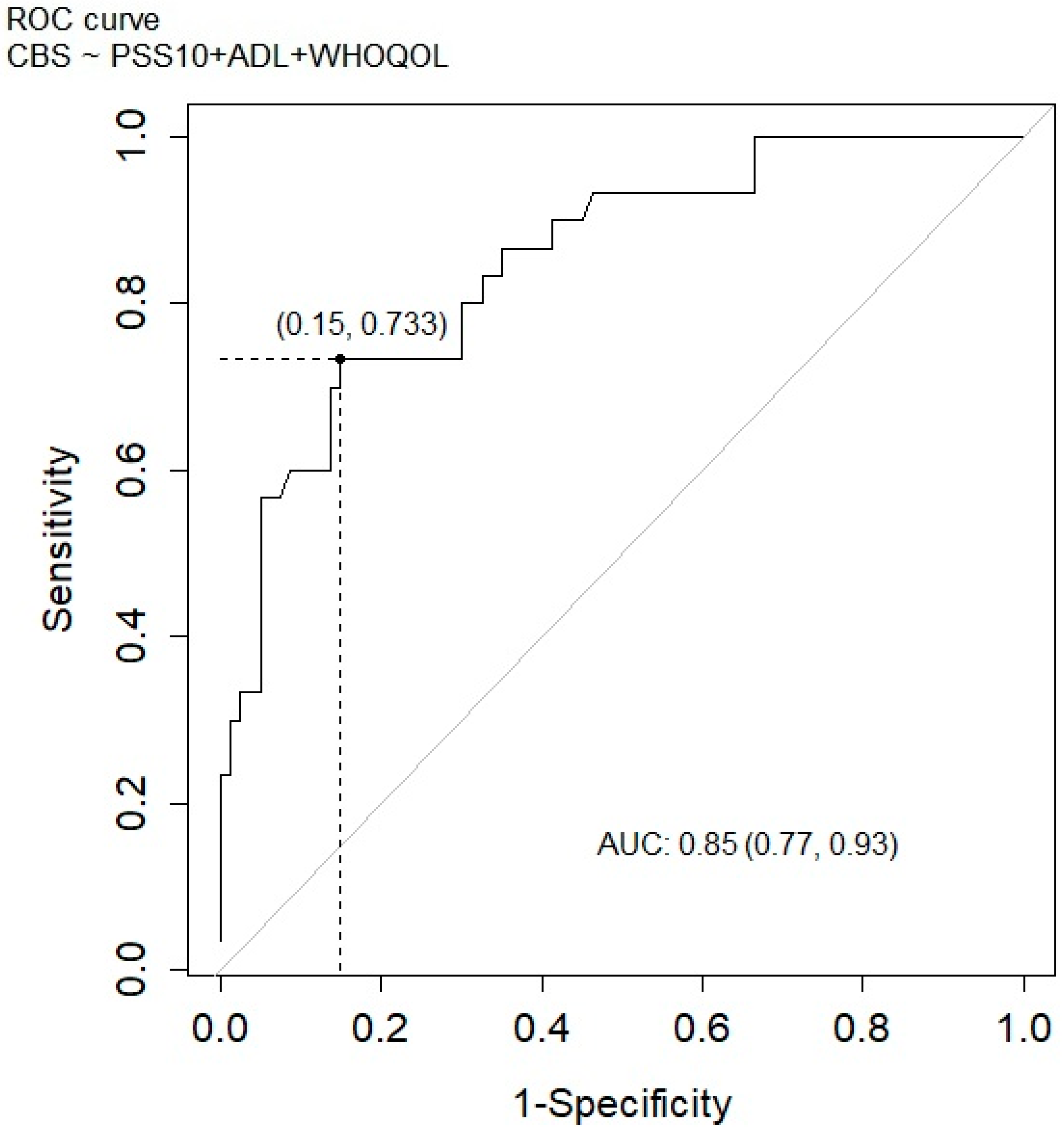
3.4. Multivariable Regression Analysis with Significant Factors Was Performed on High-Burden Caregiver
4. Discussion
4.1. Limitation
4.2. Benefits
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ADL | Activities of Daily Living |
| AMTS | Abbreviated Mental Test Score |
| AUC | Area under Receiver Operating Characteristic Curve |
| BDI | Beck Depression Inventory |
| CBS | Caregiver Burden Scale |
| GBD | Global Burden of Diseases, Injuries, and Risk Factors Study |
| mRS | The modified Rankin Scale |
| PPS-10 | Perceived Stress Scale |
| QoL | Quality of life |
| ROC | Receiver Operating Characteristic Curve |
| SD | Standard deviation |
| WHOQoL-BREF | WHO Quality of Life Brief Version |
References
- Cooper, C. GBD 2017 DALYs and HALE Collaborators Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990-2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1859–1922. [Google Scholar] [CrossRef]
- Krishnamurthi, R.V.; Ikeda, T.; Feigin, V.L. Global, Regional and Country-Specific Burden of Ischaemic Stroke, Intracerebral Haemorrhage and Subarachnoid Haemorrhage: A Systematic Analysis of the Global Burden of Disease Study 2017. Neuroepidemiology 2020, 54, 171–179. [Google Scholar] [CrossRef]
- Standing Committee for the Social Sciences (SCSS). Developing a New Understanding of Enabling Health and Wellbeing in Europe; European Science Foundation: Strasbourg, France, 2013; ISBN 978-2-918428-92-3. [Google Scholar]
- Lurbe-Puerto, K.; Maria-Engracia, L.; Baumann, M. Experiences of Caregiving, Satisfaction of Life, and Social Repercussions Among Family Caregivers, Two Years Post-Stroke. Soc. Work Health Care 2012, 51, 725–742. [Google Scholar] [CrossRef] [PubMed]
- Bucki, B. Health capability: An attempt to clarify an alternative approach for health sociology. Sc. Ann. Alexandru Ioan Cuza Univ. New Ser. Sociol Soc. Work. Sect 2014, 7, 19–31. [Google Scholar]
- Ruger, J.P. Health capability: Conceptualization and operationalization. Am. J. Public Health 2010, 100, 41–49. [Google Scholar] [CrossRef]
- Untas, A.; Koleck, M.; Rascle, N.; Bruchon-Schweitzer, M. Du modèle transactionnel à une approche dyadique en psychologie de la santé; From the transactional model to a dyadic approach in health psychology. Psychol. Française 2012, 57, 97–110. [Google Scholar] [CrossRef]
- Deepradit, S.; Powwattana, A.; Lagampan, S.; Thiangtham, W. Effectiveness of a family-based program for post-stroke patients and families: A cluster randomized controlled trial. Int. J. Nurs. Sci. 2023, 10, 446–455. [Google Scholar] [CrossRef]
- Rolland, J.S. Mastering family challenges: Coping with serious illness and disability. In Normal Family Processes, 4th ed.; Walsh, F., Ed.; Guilford: New York, NY, USA, 2012. [Google Scholar]
- Sherman, D.W. A Review of the Complex Role of Family Caregivers as Health Team Members and Second-Order Patients. Healthcare 2019, 7, 63. [Google Scholar] [CrossRef]
- Corallo, F.; Pria, D.; Di Blasi, A.; Bonanno, L.; De Cola, M.C.; Di Cara, M.; Rifici, C.; De Salvo, S.; Bramanti, P.; Marino, S.; et al. The effects of caregiver’s burden on dynamic structure in disorder of consciousness families: An observational study. Brain Behav. 2021, 11, e2305. [Google Scholar] [CrossRef]
- Norrving, B.; Barrick, J.; Davalos, A.; Dichgans, M.; Cordonnier, C.; Guekht, A.; Kutluk, K.; Mikulik, R.; Wardlaw, J.; Richard, E.; et al. Action Plan for Stroke in Europe 2018–2030. Eur. Stroke J. 2018, 3, 309–336. [Google Scholar] [CrossRef]
- Ielapi, N.; Licastro, N.; Catana, M.; Bracale, U.M.; Serra, R. Vascular Nursing and Vascular Surgery. Ann. Vasc. Surg. 2020, 68, 522–526. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.-W.; Sohn, M.K.; Lee, J.; Kim, D.Y.; Shin, Y.-I.; Oh, G.-J.; Lee, Y.-S.; Joo, M.C.; Lee, S.Y.; Han, J.; et al. Predictors of Burden for First-Ever Stroke Survivor’s Long-Term Caregivers: A Study of KOSCO. Medicina 2024, 60, 559. [Google Scholar] [CrossRef] [PubMed]
- Elmståhl, S.; Malmberg, B.; Annerstedt, L. Caregiver’s burden of patients 3 years after stroke assessed by a novel caregiver burden scale. Arch. Phys. Med. Rehabil. 1996, 77, 177–182. [Google Scholar] [CrossRef]
- Jaracz, K.; Grabowska-Fudala, B.; Kleka, P.; Tomczak, M.; Smelkowska, A.; Pawlicka, A.; Górna, K. Development and Psychometric Properties of the Caregiver Burden Scale in Polish Caregivers of Stroke Patients. Psychol. Res. Behav. Manag. 2022, 15, 665–675. [Google Scholar] [CrossRef]
- Jaracz, K.; Kalfoss, M.; Górna, K.; Baczyk, G. Quality of life in Polish respondents: Psychometric properties of the Polish WHOQOL-Bref. Scand. J. Caring Sci. 2006, 20, 251–260. [Google Scholar] [CrossRef]
- Beck, A.T.; Steer, R.A.; Brown, G.K. BDI-II, Beck Depression Inventory: Manual; Harcourt Brace: San Diego, CA, USA, 1996; ISBN 0158018389/9780158018386. [Google Scholar]
- Juczyński, Z.; Oginńska-Bulik, N.; Psychologicznych, P.T.P.P.T. Narzędzia Pomiaru Stresu i Radzenia Sobie ze Stresem; Pracownia Testów Psychologicznych Polskiego Towarzystw Psychologicznego: Warszawa, Poland, 2012; ISBN 9788360733479/8360733473. [Google Scholar]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A global measure of perceived stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.-H. Review of the psychometric evidence of the perceived stress scale. Asian Nurs. Res. 2012, 6, 121–127. [Google Scholar] [CrossRef]
- Carver, C.S. You want to measure coping but your protocol’s too long: Consider the brief COPE. Int. J. Behav. Med. 1997, 4, 92–100. [Google Scholar] [CrossRef]
- do Carmo, J.F.; Oliveira, E.R.A.; Morelato, R.L. Functional disability and associated factors in elderly stroke survivors in Vitória, Brazil. Rev. Bras. De Geriatr. E Gerontol. 2016, 19, 809–818. [Google Scholar] [CrossRef]
- Skalska, A.; Kocemba, J.W.; Grodzicki, T. Kompleksowa ocena geriatryczna. In Geriatria z Elementami Gerontologii Ogolnej: Podrecznik Dla Lekarzy i Studentow; VIA MEDICA: Gdansk, Poland, 2007; pp. 809–818. ISBN 9788360072912. [Google Scholar]
- Hodkinson, H.M. Evaluation of a mental test score for assessment of mental impairment in the elderly. 1972. Age Ageing 2012, 41 (Suppl. S3), iii35–iii40. [Google Scholar] [CrossRef]
- Pont, W.; Groeneveld, I.; Arwert, H.; Meesters, J.; Mishre, R.R.; Vliet Vlieland, T.; Goossens, P. Caregiver burden after stroke: Changes over time? Disabil. Rehabil. 2020, 42, 360–367. [Google Scholar] [CrossRef] [PubMed]
- Silva, E.; Luiz, J.; Canto, M.; Rissetti, J.; Eidt, N.; Ovando, A. Quality of life and burden of informal caregivers of post-stroke individuals. Cad. Bras. Ter. Ocup. 2022, 30, e3169. [Google Scholar] [CrossRef]
- Carleto, G.N.; Caldana, L.M. Correlation between quality of life of the aphasic patient and his family. Rev. Distúrbios Da Comun. 2014, 26, 630–640. [Google Scholar]
- da Costa, T.F.; de Freitas Macêdo Costa, K.N.; Martins, K.P.; das Graças Melo Fernandes, M.; da Silva Brito, S. Burden over family caregivers of elderly people with stroke. Esc. Anna Nery 2015, 19, 350–355. [Google Scholar] [CrossRef]
- Bhattacharjee, M.; Vairale, J.; Gawali, K.; Dalal, P.M. Factors affecting burden on caregivers of stroke survivors: Population-based study in Mumbai (India). Ann. Indian Acad. Neurol. 2012, 15, 113–119. [Google Scholar] [CrossRef]
- Yu, Y.; Hu, J.; Efird, J.T.; McCoy, T.P. Social support, coping strategies and health-related quality of life among primary caregivers of stroke survivors in China. J. Clin. Nurs. 2013, 22, 2160–2171. [Google Scholar] [CrossRef]
- Kaseke, F.; Gwanzura, L.; Kaseke, T.; Musarurwa, C.; Gori, E.; Nyengerai, T.; Stewart, A. Caregiver burden among informal caregivers of stroke survivors in Harare, Zimbabwe. S. Afr. J. Physiother. 2024, 80, 2080. [Google Scholar] [CrossRef]
- Sohkhlet, G.; Thakur, K.; David, S.I.; Verma, P.; Jadav, V.; Johnson, S.; Palal, D.; Borah, N.; Banerjee, A.; Nallapu, S.; et al. Stress in Caregivers of Stroke Patients During Rehabilitation: An Observational Study. Cureus 2023, 15, e37410. [Google Scholar] [CrossRef]
- Kazemi, A.; Azimian, J.; Mafi, M.; Allen, K.-A.; Motalebi, S.A. Caregiver burden and coping strategies in caregivers of older patients with stroke. BMC Psychol. 2021, 9, 51. [Google Scholar] [CrossRef]
- Rawat, M.; Sharma, R.; Goel, D. Burden of Stroke Survivors on Caregiver and Quality of Life. Int. J. Curr. Res. 2017, 9, 60683–60686. [Google Scholar]
- Baumann, M.; Lurbe-Puerto, K.; Alzahouri, K.; Aïach, P. Increased residual disability among poststroke survivors and the repercussions for the lives of informal caregivers. Top. Stroke Rehabil. 2011, 18, 162–171. [Google Scholar] [CrossRef] [PubMed]
- Tooth, L.; McKenna, K.; Barnett, A.; Prescott, C.; Murphy, S. Caregiver burden, time spent caring and health status in the first 12 months following stroke. Brain Inj. 2005, 19, 963–974. [Google Scholar] [CrossRef] [PubMed]
- Kruithof, W.J.; Visser-Meily, J.M.A.; Post, M.W.M. Positive caregiving experiences are associated with life satisfaction in spouses of stroke survivors. J. Stroke Cerebrovasc. Dis. Off. J. Natl. Stroke Assoc. 2012, 21, 801–807. [Google Scholar] [CrossRef] [PubMed]
- McPherson, C.J.; Wilson, K.G.; Chyurlia, L.; Leclerc, C. The caregiving relationship and quality of life among partners of stroke survivors: A cross-sectional study. Health Qual. Life Outcomes 2011, 9, 29. [Google Scholar] [CrossRef]
- Grant, J.S.; Elliott, T.R.; Weaver, M.; Glandon, G.L.; Raper, J.L.; Giger, J.N. Social support, social problem-solving abilities, and adjustment of family caregivers of stroke survivors. Arch. Phys. Med. Rehabil. 2006, 87, 343–350. [Google Scholar] [CrossRef]
| Characteristics | Caregivers | Patients | |||
|---|---|---|---|---|---|
| Total (n = 110) | Including Caregivers with High Levels of Burden (n = 30) | Total (n = 110) | Including Patients Who Are a High Burden on Their Caregivers (n = 30) | ||
| Gender | Female | 83 (75.5%) | 22 (73.3%) | 63 (57.3%) | 15 (50.0%) |
| Male | 27 (24.5%) | 8 (26.7%) | 47 (42.7%) | 15 (50.0%) | |
| Age | <50 | 32 (29.2%) | 8 (26.7%) | 5 (4.5%) | 1 (3.3%) |
| 51–60 | 36 (32.7%) | 9 (30.0%) | 6 (5.5%) | 0 (0.0%) | |
| 61–70 | 25 (22.7%) | 6 (20.0%) | 25 (22.7%) | 4 (13.3%) | |
| 71–80 | 15 (13.6%) | 7 (23.3%) | 35 (31.8%) | 8 (26.7%) | |
| >80 | 2 (1.8%) | 0 (0.0) | 39 (35.5%) | 17 (56.7%) | |
| Education | Primary | 2 (1.8%) | 1 (0.4%) | 17 (15.5%) | 6 (20.0%) |
| Vocational | 38 (34.5%) | 10 (33.3%) | 49 (44.5%) | 10 (33.3%) | |
| Secondary | 30 (27.3%) | 10 (33.3%) | 30 (27.3%) | 10 (33.3%) | |
| Higher | 40 (36.4%) | 9 (30.0) | 14 (12.7%) | 4 (13.3%) | |
| Marital status | Single | 23 (20.9%) | 6 (20.0%) | 52 (47.3%) | 12 (40.0%) |
| In a relationship | 87 (78.2%) | 24 (80.0%) | 58 (52.7%) | 18 (60.0%) | |
| Place of residence | Rural | 47 (42.7) | 13 (43.3) | 46 (41.8%) | 12 (40.0%) |
| City | 63 (57.3%) | 17 (56.7%) | 64 (58.2%) | 18 (60.0%) | |
| Source of income | Professional work | 68 (61.8%) | 17 (56.7%) | 0 (0.0%) | 3 (10.0%) |
| Pension | 37 (33.7%) | 10 (30.3%) | 102 (92.8%) | 26 (86.7%) | |
| Other (allowance; no income) | 5 (4.5%) | 3 (10.0%) | 8 (7.2%) | 1 (3.3%) | |
| Financial situation (mean ± SD) | 3.48 ± 0.62 | 3.33 ± 0.66 | 2.62 ± 0.66 | 2.66 ± 0.66 | |
| Duration of care (for patient) | 0.5 years | 17 (15.4%) | 2 (6.7%) | 17 (15.5%) | 3 (10.0%) |
| 0.5–1 years | 20 (18.2%) | 3 (10.0%) | 22 (20.0%) | 5 (16.7%) | |
| 1–2 years | 21 (19.1%) | 9 (30.0%) | 15 (13.6%) | 5 (16.7%) | |
| 2–5 years | 22 (20.0%) | 6 (20.0%) | 23 (20.9%) | 5 (16.7%) | |
| >5 years | 30 (27.3%) | 10 (33.3%) | 33 (30.0%) | 12 (40.0%) | |
| Average time spent per day on care | 1–2 h | 26 (23.6%) | 2 (6.6%) | Degree of disability (n = 99) | |
| 3–5 h | 27 (24.5%) | 8 (26.7) | mild | ||
| 5–10 h | 28 (25.5%) | 8 (26.7) | 14 (12.7%) | 0 (0.0%) | |
| >10 h | 29 (26.4%) | 12 (40.0) | moderate | ||
| Relationship | husband or wife | 38 (34.6%) | 9 (30.0%) | 12 (10.9%) | 2 (6.9%) |
| mother or father | 53 (48.2%) | 16 (53.3%) | severe | ||
| mother-in-law father-in-law | 5 (4.5%) 14 (12.7%) | 2 (6.7%) 3 (10.0%) | 73 (66.4%) | 27 (93.1%) | |
| Change in financial situation (mean value ± standard deviation) | 2.38 ± 0.62 | 2.07 ± 0.58 | |||
| Other indicators mean ± SD (range of scores: minimum value–maximum value) | |||||
| Caregiver Burden Scale | 2.39 ± 0.74 (1.00–3.73) | 3.26 ± 0.20 (3.00–3.72) | |||
| Beck Depression Inventory | 12.32 ± 9.29 (0–44) | 18.77 ± 10.02 (0–44) | |||
| Perceived Stress Scale | 20.91 ± 4.62 (3–29) | 23.40 ± 3.20 (14–28) | |||
| Total score (by WHOQOL-BREF) | 13.39 ± 1.97 (8.67–18.17) | 12.04 ± 2.03 (8.67–16.50) | |||
| The modified Rankin Scale | 3.76 ± 1.35 (0.00–5.00) | 4.47 ± 0.90 (2.00–5.00) | |||
| Activities of Daily Living Scale | 2.59 ± 2.20 (0.00–6.00) | 1.20 ± 1.47 (0.00–5.00) | |||
| Caregiver Burden Scale | M | SD | Me | Q1–Q3 | Min | Max | Level of Burden | ||
|---|---|---|---|---|---|---|---|---|---|
| Low | Medium | High | |||||||
| General burden | 2.64 | 0.82 | 2.81 | 2.00–3.38 | 1.00 | 4.00 | 26 (23.6%) | 34 (30.9%) | 50 (45.5%) |
| Social isolation | 2.42 | 0.96 | 2.67 | 1.67–3.33 | 1.00 | 4.00 | 39 (35.5%) | 28 (25.5%) | 43 (39.1%) |
| Disillusionment | 2.41 | 0.81 | 2.60 | 1.80–3.00 | 1.00 | 4.00 | 36 (32.7%) | 43 (39.1%) | 31 (28.2%) |
| Emotional involvement | 2.03 | 0.85 | 2.00 | 1.33–2.67 | 1.00 | 4.00 | 49 (44.5%) | 38 (34.5%) | 23 (20.9%) |
| Surrounding | 2.03 | 0.71 | 2.00 | 1.33–2.67 | 1.00 | 3.67 | 48 (43.6%) | 45 (40.9%) | 17 (15.5%) |
| Total | 2.39 | 0.74 | 2.45 | 1.73–3.00 | 1.00 | 3.73 | 36 (32.7%) | 44 (40.0%) | 30 (27.3%) |
| Caregiver Burden Scale | ||||||
|---|---|---|---|---|---|---|
| General Burden | Social Isolation | Disappointment | Emotional Involvement | Environment | ||
| Perceived Stress Scale ver. 10 | 0.546 *** | 0.501 *** | 0.461 *** | 0.397 *** | 0.313 *** | |
| MINI-COPE | Active coping | 0.117 | 0.120 | 0.032 | 0.111 | 0.068 |
| Planning | 0.089 | 0.063 | 0.039 | 0.000 | 0.044 | |
| Positive re-evaluation | 0.074 | −0.002 | 0.012 | 0.106 | −0.113 | |
| Acceptance | 0.016 | −0.033 | −0.042 | 0.045 | −0.023 | |
| Sense of humor | 0.061 | 0.113 | 0.097 | 0.136 | 0.067 | |
| Turning to religion | 0.044 | −0.098 | −0.050 | 0.033 | −0.028 | |
| Seeking emotional support | −0.199 * | −0.173 ǂ | −0.133 | −0.156 | −0.091 | |
| Seeking instrumental support | −0.041 | −0.087 | −0.062 | −0.118 | −0.052 | |
| Preoccupation with something else | 0.235 * | 0.278 ** | 0.219 * | 0.281 ** | 0.211 * | |
| Denial | 0.401 *** | 0.428 *** | 0.512 *** | 0.348 *** | 0.368 *** | |
| Discharging | 0.363 *** | 0.343 *** | 0.292 ** | 0.237 * | 0.180 ǂ | |
| Using psychoactive substances | 0.187 ǂ | 0.181 ǂ | 0.214 * | 0.132 | 0.070 | |
| Discontinuing activities | 0.412 *** | 0.339 *** | 0.470 *** | 0.242 * | 0.346 *** | |
| Blaming yourself | 0.400 *** | 0.342 *** | 0.418 *** | 0.197 * | 0.403 *** | |
| Beck Depression Scale | 0.561 *** | 0.472 *** | 0.500 *** | 0.327 *** | 0.406 *** | |
| WHOQOL-BREF | What is your quality of life? 1 | −0.390 *** | −0.340 *** | −0.393 *** | −0.175 ** | −0.299 *** |
| Are you satisfied with your life? 1 | −0.400 *** | −0.402 *** | −0.440 *** | −0.177 ** | −0.317 *** | |
| Somatic Domain | −0.368 *** | −0.269 ** | −0.331 *** | −0.270 ** | −0.357 *** | |
| Psychological Domain | −0.454 *** | −0.410 *** | −0.401 *** | −0.190 * | −0.385 *** | |
| Social Domain | −0.540 *** | −0.473 *** | −0.536 *** | −0.362 *** | −0.478 *** | |
| Environmental Domain | −0.486 *** | −0.464 *** | −0.522 *** | −0.286 ** | −0.414 *** | |
| Total | −0.532 *** | −0.483 *** | −0.542 *** | −0.314 ** | −0.475 *** | |
| The modified Rankin Scale | 0.382 *** | 0.484 *** | 0.423 *** | 0.235 * | 0.255 ** | |
| Activities of Daily Living Scale | −0.424 *** | −0.464 *** | −0.450 *** | −0.282 ** | −0.280 ** | |
| Abbreviated Mental Test Score | −0.460 *** | −0.530 *** | −0.492 *** | −0.447 *** | −0.316 * | |
| Coeff. | Standard Error | Wald’s Test | p-Value | Odds Ratio | 95% CI for Odds Ratio | Gini Index | ||
|---|---|---|---|---|---|---|---|---|
| 2.5% | 97.5% | |||||||
| General model based on standardized questionnaires—patients/caregivers | ||||||||
| PSS10 | 0.181 | 0.050 | 3.641 | <0.0001 | 1.198 | 1.096 | 1.334 | 10.864 |
| ADL | −0.437 | 0.159 | −2.738 | 0.006 | 0.646 | 0.458 | 0.863 | 8.632 |
| WHOQOL | −0.074 | 0.020 | −3.673 | <0.0001 | 0.928 | 0.889 | 0.963 | 16.103 |
| AIC = 97.219 LR test: χ2 = 61.273 df = 3 p < 0.0001 HL test: χ2 = 11.81 df = 8 p = 0.160 R2McFadden = 0.292 | ||||||||
| Caregivers | ||||||||
| Model I based on the domains of the MINI-COPE questionnaire | ||||||||
| (Intercept) | −3.351 | 0.724 | −4.629 | <0.0001 | ||||
| Venting | 0.848 | 0.379 | 2.235 | 0.0254 | 2.335 | 1.134 | 5.115 | 6.909 |
| Resignation | 1.308 | 0.407 | 3.213 | 0.0013 | 3.699 | 1.750 | 8.785 | 10.713 |
| AIC = 113.68 LR test: χ2 = 12.552 df = 1 p = 0.0004 HL test: χ2 = 11.471 df = 8 p = 0.1764 R2McFadden = 0.165 | ||||||||
| Model II based on the domains of the WHOQOL-BREF questionnaire | ||||||||
| Psychological | 0.574 | 0.196 | 2.929 | 0.0034 | 1.774 | 1. | 2.684 | 9.979 |
| Social | −0.257 | 0.107 | −2.389 | 0.0169 | 0.773 | 0.621 | 0.950 | 10.593 |
| Environmental | −0.386 | 0.179 | −2.149 | 0.0316 | 0.680 | 0.470 | 0.955 | 12.979 |
| AIC = 115.24 LR test: χ2 = 43.254 df = 3 p < 0.0001 HL test: χ2 = 7.119 df = 8 p = 0.524 R2McFadden = 0.152 | ||||||||
| Model based on self-reported survey | ||||||||
| SYT_MAT | −1.398 | 0.328 | −4.263 | <0.0001 | 0.247 | 0.119 | 0.437 | 4.629 |
| TIME | 0.498 | 0.224 | 2.221 | 0.0264 | 1.645 | 1.082 | 2.636 | 4.639 |
| DIS_NEU | 2.106 | 0.781 | 2.695 | 0.0070 | 8.215 | 1.849 | 42.030 | 4.375 |
| FEEL_ANG | 2.325 | 1.009 | 2.304 | 0.0212 | 10.230 | 1.587 | 94.655 | 3.524 |
| FEEL_PSYCH | 3.005 | 0.962 | 3.125 | 0.0018 | 20.181 | 3.534 | 174.109 | 5.227 |
| AIC = 94.702 LR test: χ2 = 67.791 df = 5 p < 0.0001 HL test: χ2 = 8.621 df = 7 p = 0.2811 R2McFadden = 0.343 | ||||||||
| Patients | ||||||||
| Model based on sociodemographic data | ||||||||
| (Intercept) | −3.571 | 1.075 | −3.321 | 0.0009 | ||||
| AGE | 0.639 | 0.250 | 2.558 | 0.0105 | 1.894 | 1.200 | 3.217 | 4.843 |
| AIC = 124.96 LR test: χ2 = 7.945 df = 1 p = 0.0048 HL test: χ2 = 3.314 df = 3 p = 0.3457 R2McFadden = 0.062 | ||||||||
| Model based on degree of disability | ||||||||
| (Intercept) | −3.565 | 1.066 | −3.344 | 0.0008 | ||||
| DISAB | 1.003 | 0.376 | 2.671 | 0.0075 | 2.726 | 1.462 | 6.736 | 4.914 |
| AIC = 120.85 LR test: χ2 = 12.061 df = 1 p = 0.0005 HR test: χ2 = 2.745 df = 2 p = 0.2535 R2McFadden = 0.094 | ||||||||
| Confusion Matrix | ||||||
|---|---|---|---|---|---|---|
| A Cut-Off Value of 0.273 | A Cut-Off Value of 0.5 | |||||
| Caregiver Burden Scale | Predicted | Total | Predicted | Total | ||
| High Level of Caregiver Burden | Low/Medium Level of Caregiver Burden | High Level of Caregiver Burden | Low/Medium Level of Caregiver Burden | |||
| Observed | ||||||
| High-level caregiver burden | 22 (TP) | 8 (FN) | 30 | 17 (TP) | 13 (FN) | 30 |
| Low/medium-level caregiver burden | 24 (FP) | 56 (TN) | 80 | 4 (FP) | 76 (TN) | 80 |
| Total | 46 | 64 | 110 | 21 | 89 | 110 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ryś, B.; Bąk, E. Factors Determining the Burden of a Caregiver Providing Care to a Post-Stroke Patient. J. Clin. Med. 2025, 14, 3008. https://doi.org/10.3390/jcm14093008
Ryś B, Bąk E. Factors Determining the Burden of a Caregiver Providing Care to a Post-Stroke Patient. Journal of Clinical Medicine. 2025; 14(9):3008. https://doi.org/10.3390/jcm14093008
Chicago/Turabian StyleRyś, Bogusława, and Ewelina Bąk. 2025. "Factors Determining the Burden of a Caregiver Providing Care to a Post-Stroke Patient" Journal of Clinical Medicine 14, no. 9: 3008. https://doi.org/10.3390/jcm14093008
APA StyleRyś, B., & Bąk, E. (2025). Factors Determining the Burden of a Caregiver Providing Care to a Post-Stroke Patient. Journal of Clinical Medicine, 14(9), 3008. https://doi.org/10.3390/jcm14093008





