Effectiveness of Exergames on Functional Physical Performance in Older Adults with Knee/Hip Osteoarthritis: A Randomized Controlled Trial
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design and Participants
2.2. Intervention Protocols
2.3. Outcome Variables
2.4. Statistical Analysis
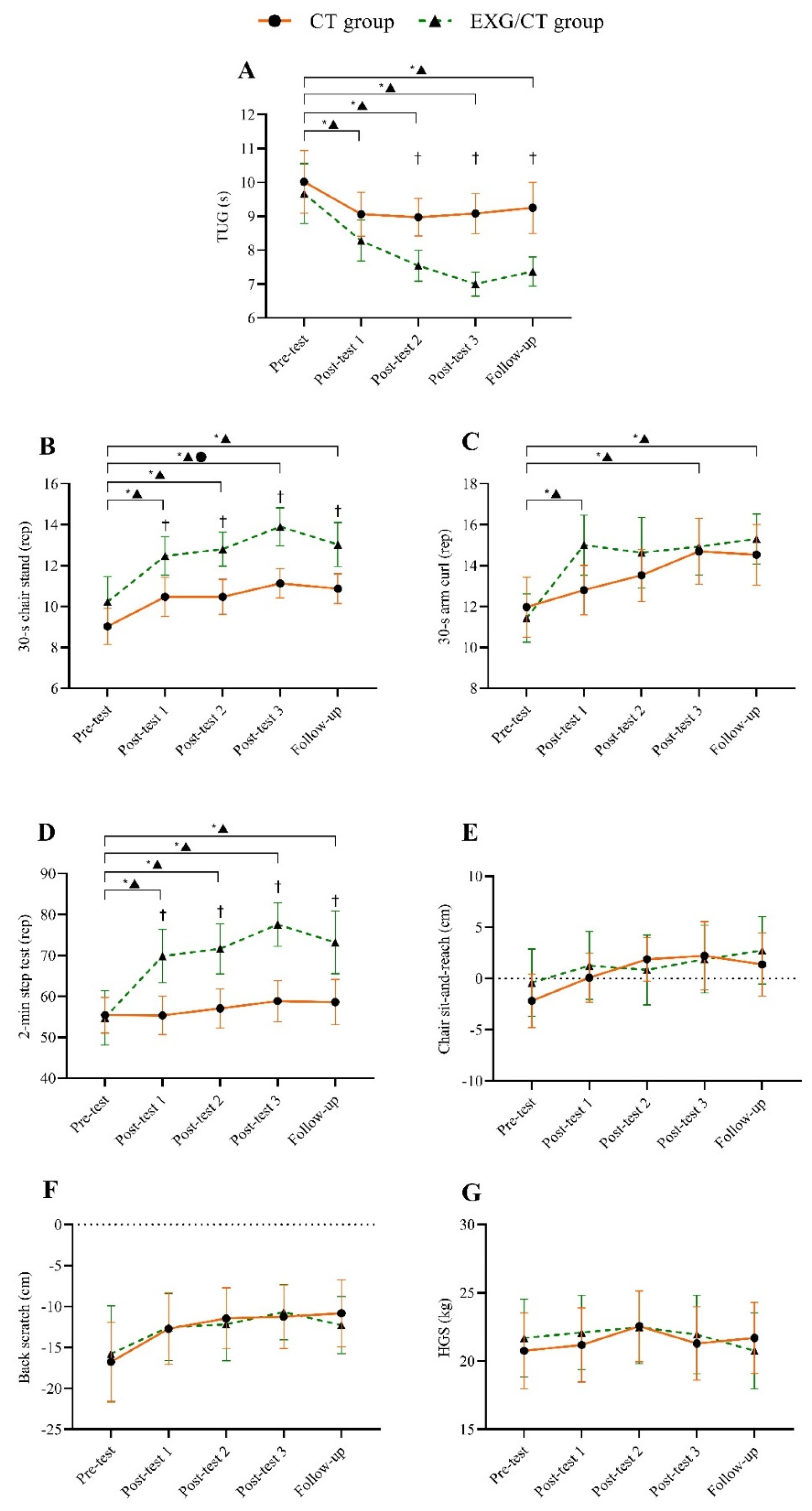
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| OA | Osteoarthritis |
| KOA | Knee osteoarthritis |
| HOA | Hip osteoarthritis |
| EXGs | Exergames |
| CT | Conventional therapy |
| TUG | Timed Up and Go |
| SFT | Senior Fitness Test |
| HGS | Handgrip strength |
| ES | Effect size |
References
- Steinmetz, J.D.; Culbreth, G.T.; Haile, L.M.; Rafferty, Q.; Lo, J.; Fukutaki, K.G.; Cruz, J.A.; Smith, A.E.; Vollset, S.E.; Brooks, P.M.; et al. Global, Regional, and National Burden of Osteoarthritis, 1990–2020 and Projections to 2050: A Systematic Analysis for the Global Burden of Disease Study 2021. Lancet Rheumatol. 2023, 5, e508–e522. [Google Scholar] [CrossRef] [PubMed]
- Allen, K.D.; Thoma, L.M.; Golightly, Y.M. Epidemiology of Osteoarthritis. Osteoarthr. Cartil. 2022, 30, 184–195. [Google Scholar] [CrossRef] [PubMed]
- Stasi, S.; Giannopapas, V.; Papagiannis, G.; Triantafyllou, A.; Papathanasiou, G.; Papagelopoulos, P.; Koulouvaris, P. Predictive and Classification Capabilities of the Timed up and Go as a Physical Performance Measure in Hip Osteoarthritis: A Retrospective Study of 606 Patients. Arch. Orthop. Trauma Surg. 2024, 144, 4171–4178. [Google Scholar] [CrossRef]
- Freiberger, E.; Sieber, C.C.; Kob, R. Mobility in Older Community-Dwelling Persons: A Narrative Review. Front. Physiol. 2020, 11, 881. [Google Scholar] [CrossRef] [PubMed]
- Ishijima, M.; Kaneko, H.; Hada, S.; Kinoshita, M.; Sadatsuki, R.; Liu, L.; Shimura, Y.; Arita, H.; Shiozawa, J.; Yusup, A.; et al. Osteoarthritis as a Cause of Locomotive Syndrome: Its Influence on Functional Mobility and Activities of Daily Living. Clin. Rev. Bone Miner. Metab. 2016, 14, 77–104. [Google Scholar] [CrossRef]
- Wojcieszek, A.; Kurowska, A.; Majda, A.; Liszka, H.; Gądek, A. The Impact of Chronic Pain, Stiffness and Difficulties in Performing Daily Activities on the Quality of Life of Older Patients with Knee Osteoarthritis. Int. J. Environ. Res. Public Health 2022, 19, 16815. [Google Scholar] [CrossRef]
- de Oliveira, F.N.; Damião, E.P.; Dos Santos, L.; Galvão, L.L.; Machado, H.R.; Silva, R.R.; Tribess, S.; Virtuoso Júnior, J.S.; de Assis Teles Santos, D. Prevalence and Factors Associated with Low Functional Mobility in Older Adults. Aging Med. Milton NSW 2024, 7, 292–300. [Google Scholar] [CrossRef]
- Moseng, T.; Vlieland, T.P.M.V.; Battista, S.; Beckwée, D.; Boyadzhieva, V.; Conaghan, P.G.; Costa, D.; Doherty, M.; Finney, A.G.; Georgiev, T.; et al. EULAR Recommendations for the Non-Pharmacological Core Management of Hip and Knee Osteoarthritis: 2023 Update. Ann. Rheum. Dis. 2024, 83, 730–740. [Google Scholar] [CrossRef]
- Hinman, R.S.; Hall, M.; Comensoli, S.; Bennell, K.L. Exercise & Sports Science Australia (ESSA) Updated Position Statement on Exercise and Physical Activity for People with Hip/Knee Osteoarthritis. J. Sci. Med. Sport 2023, 26, 37–45. [Google Scholar] [CrossRef]
- Coste, N.; Guiguet-Auclair, C.; Gerbaud, L.; Pereira, B.; Berland, P.; Gay, C.; Coudeyre, E. Perceived Barriers to and Facilitators of Physical Activity in People with Knee Osteoarthritis: Development of the Evaluation of the Perception of Physical Activity Questionnaire. Ann. Phys. Rehabil. Med. 2020, 63, 202–208. [Google Scholar] [CrossRef]
- Kilgour, A.H.M.; Rutherford, M.; Higson, J.; Meredith, S.J.; McNiff, J.; Mitchell, S.; Wijayendran, A.; Lim, S.E.R.; Shenkin, S.D. Barriers and Motivators to Undertaking Physical Activity in Adults over 70—A Systematic Review of the Quantitative Literature. Age Ageing 2024, 53, afae080. [Google Scholar] [CrossRef] [PubMed]
- Buyle, M.; Jung, Y.; Pavlou, M.; Gonzalez, S.C.; Bamiou, D.-E. The Role of Motivation Factors in Exergame Interventions for Fall Prevention in Older Adults: A Systematic Review and Meta-Analysis. Front. Neurol. 2022, 13, 903673. [Google Scholar] [CrossRef] [PubMed]
- Ren, Y.; Lin, C.; Zhou, Q.; Yingyuan, Z.; Wang, G.; Lu, A. Effectiveness of Virtual Reality Games in Improving Physical Function, Balance and Reducing Falls in Balance-Impaired Older Adults: A Systematic Review and Meta-Analysis. Arch. Gerontol. Geriatr. 2023, 108, 104924. [Google Scholar] [CrossRef]
- Chen, Y.; Zhang, Y.; Guo, Z.; Bao, D.; Zhou, J. Comparison between the Effects of Exergame Intervention and Traditional Physical Training on Improving Balance and Fall Prevention in Healthy Older Adults: A Systematic Review and Meta-Analysis. J. Neuroeng. Rehabil. 2021, 18, 164. [Google Scholar] [CrossRef]
- Hernandez-Martinez, J.; Ramos-Espinoza, F.; Muñoz-Vásquez, C.; Guzman-Muñoz, E.; Herrera-Valenzuela, T.; Branco, B.H.M.; Castillo-Cerda, M.; Valdés-Badilla, P. Effects of Active Exergames on Physical Performance in Older People: An Overview of Systematic Reviews and Meta-Analysis. Front. Public Health 2024, 12, 1250299. [Google Scholar] [CrossRef]
- Marques, L.M.; Uchida, P.M.; Barbosa, S.P. The Impact of Exergames on Emotional Experience: A Systematic Review. Front. Public Health 2023, 11, 1209520. [Google Scholar] [CrossRef]
- López-Nava, I.H.; Rodriguez, M.D.; García-Vázquez, J.P.; Perez-Sanpablo, A.I.; Quiñones-Urióstegui, I.; Meneses-Peñaloza, A.; Castillo, V.; Cuaya-Simbro, G.; Armenta, J.S.; Martínez, A.; et al. Current State and Trends of the Research in Exergames for the Elderly and Their Impact on Health Outcomes: A Scoping Review. J. Ambient. Intell. Humaniz. Comput. 2023, 14, 10977–11009. [Google Scholar] [CrossRef]
- Brepohl, P.C.A.; Leite, H. Virtual Reality Applied to Physiotherapy: A Review of Current Knowledge. Virtual Real. 2023, 27, 71–95. [Google Scholar] [CrossRef]
- Guede-Rojas, F.; Andrades-Torres, B.; Aedo-Díaz, N.; González-Koppen, C.; Muñoz-Fuentes, M.; Enríquez-Enríquez, D.; Carvajal-Parodi, C.; Mendoza, C.; Alvarez, C.; Fuentes-Contreras, J. Effects of Exergames on Rehabilitation Outcomes in Patients with Osteoarthritis. A Systematic Review. Disabil. Rehabil. 2025, 47, 1100–1113. [Google Scholar] [CrossRef]
- Wei, W.; Tang, H.; Luo, Y.; Yan, S.; Ji, Q.; Liu, Z.; Li, H.; Wu, F.; Yang, S.; Yang, X. Efficacy of Virtual Reality Exercise in Knee Osteoarthritis Rehabilitation: A Systematic Review and Meta-Analysis. Front. Physiol. 2024, 15, 1424815. [Google Scholar] [CrossRef]
- Kopec, J.A.; Heath, A.J.; Sayre, E.C.; Cibere, J.; Li, L.C.; Marra, C.A.; Liu, R.R.; Esdaile, J.M. Prevalence of Joint-Specific Osteoarthritis and Joint Pain in British Columbia, Canada. Rheumatol. Int. 2022, 42, 1623–1628. [Google Scholar] [CrossRef] [PubMed]
- Gibbs, A.J.; Gray, B.; Wallis, J.A.; Taylor, N.F.; Kemp, J.L.; Hunter, D.J.; Barton, C.J. Recommendations for the Management of Hip and Knee Osteoarthritis: A Systematic Review of Clinical Practice Guidelines. Osteoarthr. Cartil. 2023, 31, 1280–1292. [Google Scholar] [CrossRef]
- Wang, Q.; Runhaar, J.; Kloppenburg, M.; Boers, M.; Bijlsma, J.W.J.; Bierma-Zeinstra, S.M.A. the CREDO expert group Evaluation of the Diagnostic Performance of American College of Rheumatology, EULAR, and National Institute for Health and Clinical Excellence Criteria Against Clinically Relevant Knee Osteoarthritis: Data from the CHECK Cohort. Arthritis Care Res. 2024, 76, 511–516. [Google Scholar] [CrossRef] [PubMed]
- Bierma-Zeinstra, S.; Bohnen, A.; Ginai, A.; Prins, A.; Verhaar, J. Validity of American College of Rheumatology Criteria for Diagnosing Hip Osteoarthritis in Primary Care Research. J. Rheumatol. 1999, 26, 1129–1133. [Google Scholar]
- Sadeghi, H.; Jehu, D.A.; Daneshjoo, A.; Shakoor, E.; Razeghi, M.; Amani, A.; Hakim, M.N.; Yusof, A. Effects of 8 Weeks of Balance Training, Virtual Reality Training, and Combined Exercise on Lower Limb Muscle Strength, Balance, and Functional Mobility Among Older Men: A Randomized Controlled Trial. Sports Health 2021, 13, 606–612. [Google Scholar] [CrossRef]
- Jiménez, D.; Lavados, M.; Rojas, P.; Henríquez, C.; Silva, F.; Guillón, M.; Jiménez, D.; Lavados, M.; Rojas, P.; Henríquez, C.; et al. Performance of an Abbreviated Mini Mental Examination to Detect Dementia in Older People. Rev. Méd. Chile 2017, 145, 862–868. [Google Scholar] [CrossRef]
- Hawley-Hague, H.; Horne, M.; Skelton, D.A.; Todd, C. Review of How We Should Define (and Measure) Adherence in Studies Examining Older Adults’ Participation in Exercise Classes. BMJ Open 2016, 6, e011560. [Google Scholar] [CrossRef] [PubMed]
- Chodzko-Zajko, W.J.; Proctor, D.N.; Fiatarone Singh, M.A.; Minson, C.T.; Nigg, C.R.; Salem, G.J.; Skinner, J.S. Exercise and Physical Activity for Older Adults. Med. Sci. Sports Exerc. 2009, 41, 1510–1530. [Google Scholar] [CrossRef]
- Liguori, G. ACSMs Guidelines for Exercise Testing and Prescription, 11th ed.; LWW: Philadelphia, PA, USA, 2021; ISBN 978-1-975150-18-1. [Google Scholar]
- Chan, W.L.S.; Chan, C.W.L.; Lam, F.M.H.; Chan, H.H.W.; Chan, K.C.K.; Chan, J.S.K.; Chan, O.L.W.; Cheung, D.S.K. Feasibility, Safety, and Effects of a Nintendo Ring Fit AdventureTM Balance and Strengthening Exercise Program in Community-Dwelling Older Adults with a History of Falls: A Feasibility Randomized Controlled Trial. Geriatr. Gerontol. Int. 2024, 24, 334–341. [Google Scholar] [CrossRef]
- Sato, T.; Shimizu, K.; Shiko, Y.; Kawasaki, Y.; Orita, S.; Inage, K.; Shiga, Y.; Suzuki, M.; Sato, M.; Enomoto, K.; et al. Effects of Nintendo Ring Fit Adventure Exergame on Pain and Psychological Factors in Patients with Chronic Low Back Pain. Games Health J. 2021, 10, 158–164. [Google Scholar] [CrossRef]
- Podsiadlo, D.; Richardson, S. The Timed “Up & Go”: A Test of Basic Functional Mobility for Frail Elderly Persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar] [CrossRef]
- Svinøy, O.-E.; Hilde, G.; Bergland, A.; Strand, B.H. Timed Up and Go: Reference Values for Community-Dwelling Older Adults with and without Arthritis and Non-Communicable Diseases: The Tromsø Study. Clin. Interv. Aging 2021, 16, 335–343. [Google Scholar] [CrossRef] [PubMed]
- Rikli, R.E.; Jones, C.J. Development and Validation of Criterion-Referenced Clinically Relevant Fitness Standards for Maintaining Physical Independence in Later Years. Gerontologist 2013, 53, 255–267. [Google Scholar] [CrossRef]
- Rikli, R.E.; Jones, C.J. Senior Fitness Test Manual, 2nd ed.; Human Kinetics: Champaign, IL, USA, 2013. [Google Scholar]
- Fess, E. Grip Strength. In Clinical Assessment Recommendations, 2nd ed.; Casanova, J.S., Ed.; American Society of Hand Therapists: Chicago, IL, USA, 1992; pp. 41–45. [Google Scholar]
- Gupta, S.K. Intention-to-Treat Concept: A Review. Perspect. Clin. Res. 2011, 2, 109. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.C.; White, I.R.; Carlin, J.B.; Spratt, M.; Royston, P.; Kenward, M.G.; Wood, A.M.; Carpenter, J.R. Multiple Imputation for Missing Data in Epidemiological and Clinical Research: Potential and Pitfalls. BMJ 2009, 338, b2393. [Google Scholar] [CrossRef] [PubMed]
- Koller, M. Robustlmm: An R Package for Robust Estimation of Linear Mixed-Effects Models. J. Stat. Softw. 2016, 75, 1–24. [Google Scholar] [CrossRef]
- Bates, D.; Mächler, M.; Bolker, B.; Walker, S. Fitting Linear Mixed-Effects Models Using Lme4. J. Stat. Softw. 2015, 67, 1–48. [Google Scholar] [CrossRef]
- Lenth, R.V.; Banfai, B.; Bolker, B.; Buerkner, P.; Giné-Vázquez, I.; Herve, M.; Jung, M.; Love, J.; Miguez, F.; Piaskowski, J.; et al. Emmeans: Estimated Marginal Means, aka Least-Squares Means. R package version 1.11.0-004. 2025. Available online: https://rvlenth.github.io/emmeans/ (accessed on 17 April 2025).
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Routledge: New York, NY, USA, 1988; ISBN 978-0-203-77158-7. [Google Scholar]
- Anders, P.; Lehmann, T.; Müller, H.; Grønvik, K.B.; Skjæret-Maroni, N.; Baumeister, J.; Vereijken, B. Exergames Inherently Contain Cognitive Elements as Indicated by Cortical Processing. Front. Behav. Neurosci. 2018, 12, 102. [Google Scholar] [CrossRef]
- Müller, H.; Baumeister, J.; Bardal, E.M.; Vereijken, B.; Skjæret-Maroni, N. Exergaming in Older Adults: The Effects of Game Characteristics on Brain Activity and Physical Activity. Front. Aging Neurosci. 2023, 15, 1143859. [Google Scholar] [CrossRef]
- Teraz, K.; Šlosar, L.; Paravlić, A.H.; de Bruin, E.D.; Marusic, U. Impact of Motor-Cognitive Interventions on Selected Gait and Balance Outcomes in Older Adults: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Front. Psychol. 2022, 13, 837710. [Google Scholar] [CrossRef]
- Cacciata, M.; Stromberg, A.; Lee, J.-A.; Sorkin, D.; Lombardo, D.; Clancy, S.; Nyamathi, A.; Evangelista, L.S. Effect of Exergaming on Health-Related Quality of Life in Older Adults: A Systematic Review. Int. J. Nurs. Stud. 2019, 93, 30–40. [Google Scholar] [CrossRef]
- Cugusi, L.; Prosperini, L.; Mura, G. Exergaming for Quality of Life in Persons Living with Chronic Diseases: A Systematic Review and Meta-Analysis. PMR 2021, 13, 756–780. [Google Scholar] [CrossRef] [PubMed]
- Montero-Odasso, M.M.; Kamkar, N.; Pieruccini-Faria, F.; Osman, A.; Sarquis-Adamson, Y.; Close, J.; Hogan, D.B.; Hunter, S.W.; Kenny, R.A.; Lipsitz, L.A.; et al. Evaluation of Clinical Practice Guidelines on Fall Prevention and Management for Older Adults: A Systematic Review. JAMA Netw. Open 2021, 4, e2138911. [Google Scholar] [CrossRef]
- Coelho-Junior, H.J.; Rodrigues, B.; de Gonçalves, I.O.; Asano, R.Y.; Uchida, M.C.; Marzetti, E. The Physical Capabilities Underlying Timed “Up and Go” Test Are Time-Dependent in Community-Dwelling Older Women. Exp. Gerontol. 2018, 104, 138–146. [Google Scholar] [CrossRef]
- Ziegl, A.; Hayn, D.; Kastner, P.; Fabiani, E.; Šimunič, B.; Löffler, K.; Weidinger, L.; Brix, B.; Goswami, N.; Günter, S. Quantification of the Link between Timed Up-and-Go Test Subtasks and Contractile Muscle Properties. Sensors 2021, 21, 6539. [Google Scholar] [CrossRef]
- Alghadir, A.; Anwer, S.; Brismée, J.-M. The Reliability and Minimal Detectable Change of Timed Up and Go Test in Individuals with Grade 1—3 Knee Osteoarthritis. BMC Musculoskelet. Disord. 2015, 16, 174. [Google Scholar] [CrossRef] [PubMed]
- Zasadzka, E.; Borowicz, A.M.; Roszak, M.; Pawlaczyk, M. Assessment of the Risk of Falling with the Use of Timed up and Go Test in the Elderly with Lower Extremity Osteoarthritis. Clin. Interv. Aging 2015, 10, 1289–1298. [Google Scholar] [CrossRef]
- Lapierre, N.; Um Din, N.; Belmin, J.; Lafuente-Lafuente, C. Exergame-Assisted Rehabilitation for Preventing Falls in Older Adults at Risk: A Systematic Review and Meta-Analysis. Gerontology 2023, 69, 757–767. [Google Scholar] [CrossRef]
- Manlapaz, D.G.; Sole, G.; Jayakaran, P.; Chapple, C.M. Exergaming to Improve Balance and Decrease the Risk of Falling in Adults with Knee Osteoarthritis: A Mixed-Methods Feasibility Study. Physiother. Theory Pract. 2022, 38, 2428–2440. [Google Scholar] [CrossRef]
- Richards, R.; van den Noort, J.C.; van der Esch, M.; Booij, M.J.; Harlaar, J. Gait Retraining Using Real-Time Feedback in Patients with Medial Knee Osteoarthritis: Feasibility and Effects of a Six-Week Gait Training Program. Knee 2018, 25, 814–824. [Google Scholar] [CrossRef]
- Sadura-Sieklucka, T.; Czerwosz, L.T.; Kądalska, E.; Kożuchowski, M.; Księżopolska-Orłowska, K.; Targowski, T. Is Balance Training Using Biofeedback Effective in the Prophylaxis of Falls in Women over the Age of 65? Brain Sci. 2023, 13, 629. [Google Scholar] [CrossRef]
- Lee, K. Home-Based Exergame Program to Improve Physical Function, Fall Efficacy, Depression and Quality of Life in Community-Dwelling Older Adults: A Randomized Controlled Trial. Healthcare 2023, 11, 1109. [Google Scholar] [CrossRef]
- De Medeiros, C.S.P.; Farias, L.B.A.; do Santana, M.C.L.; Pacheco, T.B.F.; Dantas, R.R.; da Cavalcanti, F.A.C. A Systematic Review of Exergame Usability as Home-Based Balance Training Tool for Older Adults Usability of Exergames as Home-Based Balance Training. PLoS ONE 2024, 19, e0306816. [Google Scholar] [CrossRef] [PubMed]
- Gonçalves, A.; Muñoz, J.; Cameirão, M.S.; Gouveia, É.R.; Sousa, H.; Bermúdez i Badia, S. The Benefits of Custom Exergames for Fitness, Balance, and Health-Related Quality of Life: A Randomized Controlled Trial with Community-Dwelling Older Adults. Games Health J. 2021, 10, 245–253. [Google Scholar] [PubMed]
- Ringgenberg, N.; Mildner, S.; Hapig, M.; Hermann, S.; Kruszewski, K.; Martin-Niedecken, A.L.; Rogers, K.; Schättin, A.; Behrendt, F.; Böckler, S.; et al. ExerG: Adapting an Exergame Training Solution to the Needs of Older Adults Using Focus Group and Expert Interviews. J. Neuroeng. Rehabil. 2022, 19, 89. [Google Scholar] [CrossRef]
- Stanmore, E.K.; Mavroeidi, A.; de Jong, L.D.; Skelton, D.A.; Sutton, C.J.; Benedetto, V.; Munford, L.A.; Meekes, W.; Bell, V.; Todd, C. The Effectiveness and Cost-Effectiveness of Strength and Balance Exergames to Reduce Falls Risk for People Aged 55 Years and Older in UK Assisted Living Facilities: A Multi-Centre, Cluster Randomised Controlled Trial. BMC Med. 2019, 17, 49. [Google Scholar] [CrossRef] [PubMed]
- Manocchio, N.; Pirri, C.; Ljoka, C.; Sorbino, A.; Piacentini, N.; Monello, C.; Vita, G.; Foti, C. Long-Term Efficacy of Carboxymethyl-Chitosan in Advanced Knee Osteoarthritis: A Twelve-Month Follow-Up Study on Non-Responders to Hyaluronic Acid. Biomedicines 2025, 13, 270. [Google Scholar] [CrossRef]
- Tschopp, M.; Pfirrmann, C.W.A.; Fucentese, S.F.; Brunner, F.; Catanzaro, S.; Kühne, N.; Zwyssig, I.; Sutter, R.; Götschi, T.; Tanadini, M.; et al. A Randomized Trial of Intra-Articular Injection Therapy for Knee Osteoarthritis. Investig. Radiol. 2023, 58, 355. [Google Scholar] [CrossRef]


| Squats | While keeping feet shoulder-width apart and holding the ring at abdomen level, participants execute slow, controlled squats. An isometric hold is included at the midpoint of the movement to strengthen the lower limbs and improve muscle endurance. |
| Lateral inclination | Standing with feet aligned at shoulder width and arms raised while holding the ring, the participant performs slow, controlled side bends. An isometric pause at the end range maximizes muscle engagement, promoting flexibility and lateral-trunk stability. |
| Rotation with inclination | Performed in a semi-squat position with a slight forward lean, this exercise requires alternating trunk rotations while keeping the ring extended in front. At the peak of each turn, the participant holds the position briefly to reinforce core strength and stability. |
| Lunge with rotation | This exercise combines a forward lunge with a rotational component. As the participant steps into the lunge position, they rotate their torso toward the leading leg while keeping the ring elevated. A brief isometric pause at the peak of the twist enhances core control and balance. |
| Knee raises | This dynamic movement consists of lifting the knees alternately toward the chest while coordinating arm movements. It promotes lower-limb coordination, activates core muscles, and provides a cardiovascular stimulus. |
| Squats with extension | In this squat variation, the participant assumes a wider stance with toes slightly turned outward while holding the ring overhead. Squats are performed at a controlled pace, incorporating a brief isometric pause to reinforce lower-limb strength and postural stability. |
| Dorsal rotation | This exercise involves continuous upper-body twisting from side to side while maintaining an upright posture. The participant stands with feet shoulder-width apart and holds the ring at waist level. The movement enhances spinal flexibility and engages the core muscles. |
| Crescent moon | In this movement, the participant performs alternating trunk rotations while maintaining a lunge stance and holding the ring in front of the body. The exercise focuses on dynamic stability and core activation. |
| The chair | This exercise is based on a modified yoga posture where the participant maintains a static half-squat while controlling the movement of the arms through slow flexion and extension. It strengthens the lower body and enhances postural endurance. |
| The warrior | Inspired by yoga, this movement involves placing the legs in a staggered stance while performing lateral-trunk bends. The ring is held overhead to increase postural engagement and enhance flexibility. |
| Running path, monster’s lair, jogging bridge | These interactive running games require players to progress through different virtual environments filled with obstacles and challenges. Participants engage in on-the-spot jogging or marching while adjusting their pace, dodging barriers, and responding to in-game prompts. This activity encourages aerobic endurance and dynamic coordination. |
| Moto adductors | This exercise involves seated gameplay where the participant controls an in-game cart by applying variable pressure on the ring placed between the knees. The goal is to navigate obstacles and collect coins while improving lower-body endurance and control. |
| Trunk swinging | While holding the ring overhead, the participant performs quick, coordinated trunk movements to collect coins and dodge obstacles. This activity enhances reactivity, agility, and upper-body coordination. |
| Equilibrism | The objective is to collect coins appearing randomly as the avatar moves along a rail while carrying a horizontal bar. The participant simulates walking in place while holding the ring at waist level and must perform quick lateral-trunk inclinations to avoid obstacles, enhancing coordination and balance. |
| CT Group (n = 30) | EXG/CT Group (n = 30) | p-Value | |
|---|---|---|---|
| Age, years | 69.0 ± 5.55 | 68.73 ± 5.47 | 0.852 |
| Height, m | 1.54 ± 0.07 | 1.53 ± 0.07 | 0.621 |
| Weight, kg | 72.26 ± 11.09 | 70.70 ± 12.50 | 0.612 |
| BMI, kg/m2 | 30.17 ± 4.34 | 29.82 ± 4.44 | 0.761 |
| OA diagnosis, no. (%) | |||
| Knee | 15 (50) | 19 (63.3) | 0.298 |
| Hip | 6 (20) | 7 (23.3) | 0.756 |
| Knee and hip | 9 (30) | 4 (13.3) | 0.116 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Carvajal-Parodi, C.; Mendoza, C.; Alvarez, C.; Soto-Martínez, A.; Ulloa-Díaz, D.; Jorquera-Aguilera, C.; Guede-Rojas, F. Effectiveness of Exergames on Functional Physical Performance in Older Adults with Knee/Hip Osteoarthritis: A Randomized Controlled Trial. J. Clin. Med. 2025, 14, 2968. https://doi.org/10.3390/jcm14092968
Carvajal-Parodi C, Mendoza C, Alvarez C, Soto-Martínez A, Ulloa-Díaz D, Jorquera-Aguilera C, Guede-Rojas F. Effectiveness of Exergames on Functional Physical Performance in Older Adults with Knee/Hip Osteoarthritis: A Randomized Controlled Trial. Journal of Clinical Medicine. 2025; 14(9):2968. https://doi.org/10.3390/jcm14092968
Chicago/Turabian StyleCarvajal-Parodi, Claudio, Cristhian Mendoza, Cristian Alvarez, Adolfo Soto-Martínez, David Ulloa-Díaz, Carlos Jorquera-Aguilera, and Francisco Guede-Rojas. 2025. "Effectiveness of Exergames on Functional Physical Performance in Older Adults with Knee/Hip Osteoarthritis: A Randomized Controlled Trial" Journal of Clinical Medicine 14, no. 9: 2968. https://doi.org/10.3390/jcm14092968
APA StyleCarvajal-Parodi, C., Mendoza, C., Alvarez, C., Soto-Martínez, A., Ulloa-Díaz, D., Jorquera-Aguilera, C., & Guede-Rojas, F. (2025). Effectiveness of Exergames on Functional Physical Performance in Older Adults with Knee/Hip Osteoarthritis: A Randomized Controlled Trial. Journal of Clinical Medicine, 14(9), 2968. https://doi.org/10.3390/jcm14092968







