Evaluating Variations in Spinopelvic Parameters from Sitting to Standing: A Comparative Analysis of 1447 Older Adults Across Age, BMI, and Gender Subgroups
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Patient Cohort
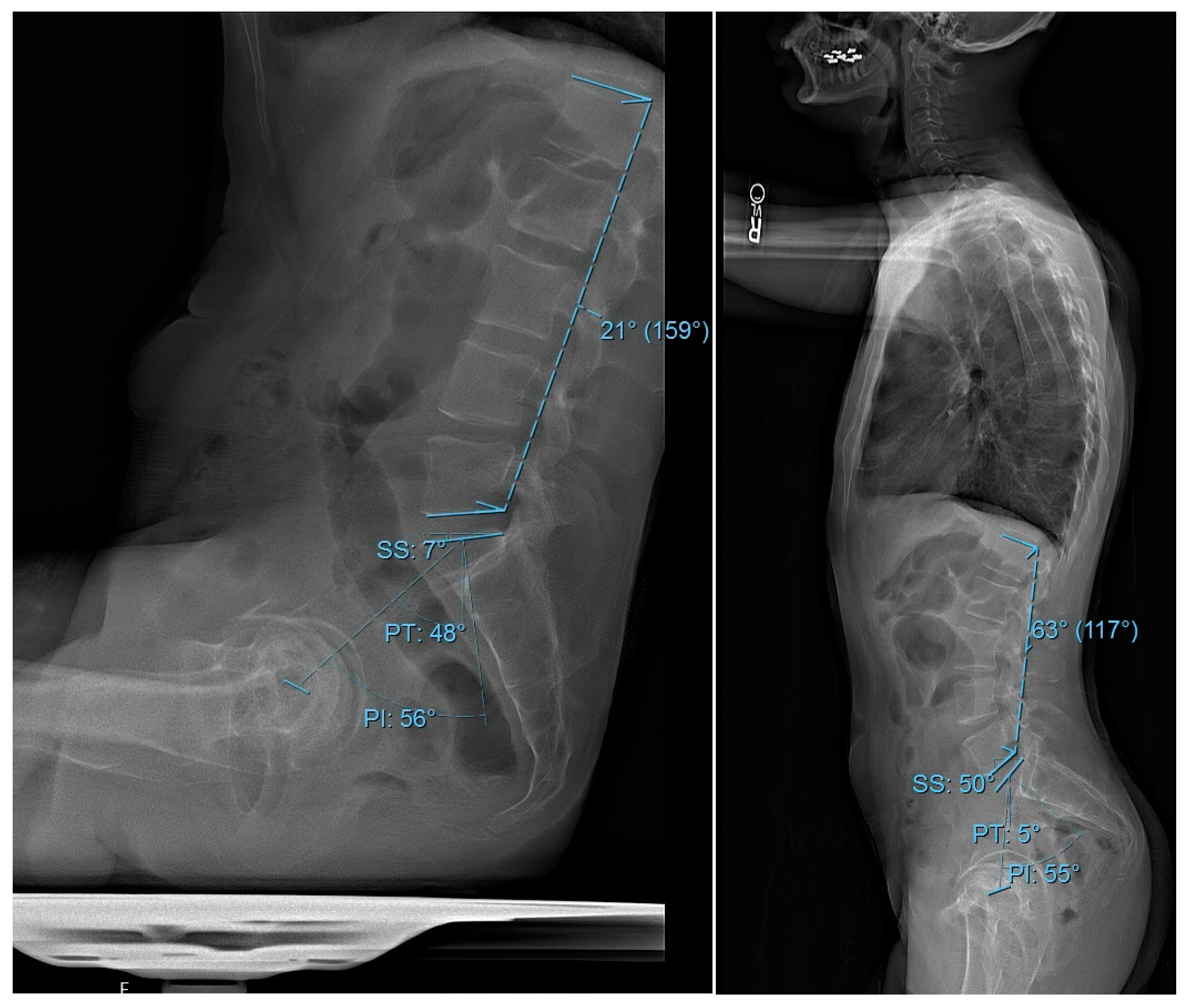
2.2. Data Collection
2.3. Primary Outcome
2.4. Statistical Analysis
3. Results
3.1. Demographic Characteristics
3.2. Subgroup Analysis
3.2.1. Stratification by Age
3.2.2. Stratification by BMI
3.2.3. Stratification by Gender
3.3. Multiple Regression Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ASD | Adult Spinal Deformity |
| ASA | American Society of Anesthesiologists |
| BMI | Body Mass Index |
| CCI | Charlson Comorbidity Index |
| HOA | Hip Osteoarthritis |
| HR | Hip Replacement |
| HSS | Hospital for Special Surgery |
| IQR | Interquartile Range |
| IRB | Institutional Review Board |
| LL | Lumbar Lordosis |
| NIH | National Institute of Health |
| OA | Osteoarthritis |
| PI | Pelvic Incidence |
| PI-LL | Pelvic Incidence minus Lumbar Lordosis |
| PT | Pelvic Tilt |
| PROMS | Patient-Reported Outcome Measures |
| REDCap | Research Electronic Data Capture |
| SD | Standard Deviation |
| SIJ | Sacroiliac Joint |
| SS | Sacral Slope |
| XR | X-ray |
References
- Glassman, S.D.; Bridwell, K.; Dimar, J.R.; Horton, W.; Berven, S.; Schwab, F. The Impact of Positive Sagittal Balance in Adult Spinal Deformity. Spine 2005, 30, 2024–2029. [Google Scholar] [CrossRef] [PubMed]
- Schwab, F.; Lafage, V.; Patel, A.; Farcy, J.-P. Sagittal Plane Considerations and the Pelvis in the Adult Patient. Spine 2009, 34, 1828–1833. [Google Scholar] [CrossRef] [PubMed]
- Jackson, R.P.; McManus, A.C. Radiographic Analysis of Sagittal Plane Alignment and Balance in Standing Volunteers and Patients with Low Back Pain Matched for Age, Sex, and Size. A prospective controlled clinical study. Spine 1994, 19, 1611–1618. [Google Scholar] [CrossRef] [PubMed]
- Diebo, B.G.; Varghese, J.J.; Lafage, R.; Schwab, F.J.; Lafage, V. Sagittal alignment of the spine: What do you need to know? Clin. Neurol. Neurosurg. 2015, 139, 295–301. [Google Scholar] [CrossRef]
- Schuna, J.M.; Johnson, W.D.; Tudor-Locke, C. Adult self-reported and objectively monitored physical activity and sedentary behavior: NHANES 2005–2006. Int. J. Behav. Nutr. Phys. Act. 2013, 10, 126. [Google Scholar] [CrossRef]
- Loyen, A.; Verloigne, M.; Van Hecke, L.; Hendriksen, I.; Lakerveld, J.; Steene-Johannessen, J.; Koster, A.; Donnelly, A.; Ekelund, U.; Deforche, B.; et al. Variation in population levels of sedentary time in European adults according to cross-European studies: A systematic literature review within DEDIPAC. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 71. [Google Scholar] [CrossRef]
- Hey, H.W.D.; Teo, A.Q.A.; Tan, K.-A.; Ng, L.W.N.; Lau, L.-L.; Liu, K.-P.G.; Wong, H.-K. How the spine differs in standing and in sitting—Important considerations for correction of spinal deformity. Spine J. 2017, 17, 799–806. [Google Scholar] [CrossRef]
- Nishida, N.; Izumiyama, T.; Asahi, R.; Iwanaga, H.; Yamagata, H.; Mihara, A.; Nakashima, D.; Imajo, Y.; Suzuki, H.; Funaba, M.; et al. Changes in the global spine alignment in the sitting position in an automobile. Spine J. 2020, 20, 614–620. [Google Scholar] [CrossRef]
- Endo, K.; Suzuki, H.; Nishimura, H.; Tanaka, H.; Shishido, T.; Yamamoto, K. Sagittal lumbar and pelvic alignment in the standing and sitting positions. J. Orthop. Sci. 2012, 17, 682–686. [Google Scholar] [CrossRef]
- Cho, I.Y.; Park, S.Y.; Park, J.H.; Kim, T.K.; Jung, T.W.; Lee, H.M. The Effect of Standing and Different Sitting Positions on Lumbar Lordosis: Radiographic Study of 30 Healthy Volunteers. Asian Spine J. 2015, 9, 762–769. [Google Scholar] [CrossRef]
- Lord, M.J.; Small, J.M.; Dinsay, J.M.; Watkins, R.G. Lumbar Lordosis. Effects of sitting and standing. Spine 1997, 22, 2571–2574. [Google Scholar] [CrossRef] [PubMed]
- De Carvalho, D.E.; Soave, D.; Ross, K.; Callaghan, J.P. Lumbar Spine and Pelvic Posture Between Standing and Sitting: A Radiologic Investigation Including Reliability and Repeatability of the Lumbar Lordosis Measure. J. Manip. Physiol. Ther. 2010, 33, 48–55. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, H.; Endo, K.; Sawaji, Y.; Matsuoka, Y.; Nishimura, H.; Takamatsu, T.; Murata, K.; Seki, T.; Konishi, T.; Aihara, T.; et al. Radiographic Assessment of Spinopelvic Sagittal Alignment from Sitting to Standing Position. Spine Surg. Relat. Res. 2018, 2, 290–293. [Google Scholar] [CrossRef] [PubMed]
- Yoshimoto, H.; Sato, S.; Masuda, T.; Kanno, T.; Shundo, M.; Hyakumachi, T.; Yanagibashi, Y. Spinopelvic Alignment in Patients with Osteoarthrosis of the Hip: A radiographic comparison to patients with low back pain. Spine 2005, 30, 1650–1657. [Google Scholar] [CrossRef]
- Chavarria, J.C.; Douleh, D.G.; York, P.J. The Hip-Spine Challenge. J. Bone Jt. Surg. 2021, 103, 1852–1860. [Google Scholar] [CrossRef]
- DelSole, E.M.; Vigdorchik, J.M.; Schwarzkopf, R.; Errico, T.J.; Buckland, A.J. Total Hip Arthroplasty in the Spinal Deformity Population: Does Degree of Sagittal Deformity Affect Rates of Safe Zone Placement, Instability, or Revision? J. Arthroplast. 2017, 32, 1910–1917. [Google Scholar] [CrossRef]
- Balmaceno-Criss, M.; Daher, M.; McDermott, J.R.; Rezk, A.; Baroudi, M.; Gregorczyk, J.A.; Laperche, J.; Lafage, R.; Bodner, R.J.; Cohen, E.M.; et al. Hip-spine syndrome in adult spinal deformity patients. Semin. Spine Surg. 2023, 35, 101066. [Google Scholar] [CrossRef]
- In, T.-S.; Jung, J.-H.; Jung, K.-S.; Cho, H.-Y. Spinal and Pelvic Alignment of Sitting Posture Associated with Smartphone Use in Adolescents with Low Back Pain. Int. J. Environ. Res. Public Health 2021, 18, 8369. [Google Scholar] [CrossRef]
- Diebo, B.G.; Alsoof, D.; Balmaceno-Criss, M.; Daher, M.; Lafage, R.; Passias, P.G.; Ames, C.P.; Shaffrey, C.I.; Burton, D.C.; Deviren, V.; et al. Hip Osteoarthritis in Patients Undergoing Surgery for Severe Adult Spinal Deformity: Prevalence and impact on spine surgery outcomes. J. Bone Jt. Surg. 2024, 106, 1171–1180. [Google Scholar] [CrossRef]
- Su, C.A.; Kusin, D.J.; Li, S.Q.B.; Ahn, U.M.; Ahn, N.U. The Association Between Body Mass Index and the Prevalence, Severity, and Frequency of Low Back Pain: Data from the osteoarthritis initiative. Spine 2018, 43, 848–852. [Google Scholar] [CrossRef]
- Yasuda, T.; Togawa, D.; Hasegawa, T.; Yamato, Y.; Kobayashi, S.; Yoshida, G.; Banno, T.; Arima, H.; Oe, S.; Hoshino, H.; et al. Relationship between Knee Osteoarthritis and Spinopelvic Sagittal Alignment in Volunteers over 50 Years of Age. Asian Spine J. 2020, 14, 495–501. [Google Scholar] [CrossRef] [PubMed]
- Hey, H.W.D.; Wong, C.G.; Lau, E.T.-C.; Tan, K.-A.; Lau, L.-L.; Liu, K.-P.G.; Wong, H.-K. Differences in erect sitting and natural sitting spinal alignment—Insights into a new paradigm and implications in deformity correction. Spine J. 2017, 17, 183–189. [Google Scholar] [CrossRef] [PubMed]
- Sun, Z.; Zhou, S.; Wang, W.; Zou, D.; Li, W. Differences in standing and sitting spinopelvic sagittal alignment for patients with posterior lumbar fusion: Important considerations for the changes of unfused adjacent segments lordosis. BMC Musculoskelet. Disord. 2020, 21, 760. [Google Scholar] [CrossRef]
- Glattes, R.C.; Bridwell, K.H.; Lenke, L.G.; Kim, Y.J.; Rinella, A.; Edwards, C. Proximal Junctional Kyphosis in Adult Spinal Deformity Following Long Instrumented Posterior Spinal Fusion: Incidence, outcomes, and risk factor analysis. Spine 2005, 30, 1643–1649. [Google Scholar] [CrossRef]
- Janjua, M.B.; Tishelman, J.C.; Vasquez-Montes, D.; Vaynrub, M.; Errico, T.J.; Buckland, A.J.; Protopsaltis, T. The value of sitting radiographs: Analysis of spine flexibility and its utility in preoperative planning for adult spinal deformity surgery. J. Neurosurgery Spine 2018, 29, 414–421. [Google Scholar] [CrossRef]
- Kohn, M.D.; Sassoon, A.A.; Fernando, N.D. Classifications in Brief: Kellgren-Lawrence Classification of Osteoarthritis. Clin. Orthop. Relat. Res. 2016, 474, 1886–1893. [Google Scholar] [CrossRef]
- Tsagkaris, C.; Widmer, J.; Wanivenhaus, F.; Redaelli, A.; Lamartina, C.; Farshad, M. The sitting vs standing spine. North Am. Spine Soc. J. (NASSJ) 2022, 9, 100108. [Google Scholar] [CrossRef]
- Tan, T.H.; Tan, J.-H.M.; Hey, H.W.D.M. Changes in Spinopelvic Parameters Between Standing and Sitting Postures: A Systematic Review and Meta-analysis. Clin. Spine Surg. A Spine Publ. 2023, 37, 97–113. [Google Scholar] [CrossRef]
- Legaye, J.; Duval-Beaupère, C.; Hecquet, J.; Marty, C. Pelvic incidence: A fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur. Spine J. 1998, 7, 99–103. [Google Scholar] [CrossRef]
- Buckland, A.J.; Steinmetz, L.; Zhou, P.; Vasquez-Montes, D.; Kingery, M.; Stekas, N.D.; Ayres, E.W.; Varlotta, C.G.; Lafage, V.; Lafage, R.; et al. Spinopelvic Compensatory Mechanisms for Reduced Hip Motion (ROM) in the Setting of Hip Osteoarthritis. Spine Deform. 2019, 7, 923–928. [Google Scholar] [CrossRef]
- Tomizawa, K.; Inami, S.; Moridaira, H.; Ueda, H.; Sekimoto, I.; Kanto, T.; Taneichi, H. Decrease in pelvic incidence after adult spinal deformity surgery is a predictive factor for progression of hip joint osteoarthritis. BMC Musculoskelet. Disord. 2024, 25, 504. [Google Scholar] [CrossRef] [PubMed]
- Ramchandran, S.; Ramch, S. Ran Pelvic Incidence (PI) is more Easily Understood as the Pelvic Base Angle (PBA). Spine Res. 2017, 3, 8. [Google Scholar] [CrossRef]
- Kleck, C.J.; Noshchenko, A.; Burger, E.L.; Cain, C.M.J.; Patel, V.V. Postoperative pelvic incidence (PI) change may impact sagittal spinopelvic alignment (SSA) after instrumented surgical correction of adult spine deformity (ASD). Spine Deform. 2021, 9, 1093–1104. [Google Scholar] [CrossRef]
- Lee, J.-H.; Na, K.-H.; Kim, J.-H.; Jeong, H.-Y.; Chang, D.-G. Is pelvic incidence a constant, as everyone knows? Changes of pelvic incidence in surgically corrected adult sagittal deformity. Eur. Spine J. 2015, 25, 3707–3714. [Google Scholar] [CrossRef]
- Casaroli, G.; Bassani, T.; Brayda-Bruno, M.; Luca, A.; Galbusera, F. What do we know about the biomechanics of the sacroiliac joint and of sacropelvic fixation? A literature review. Med. Eng. Phys. 2020, 76, 1–12. [Google Scholar] [CrossRef]
- Cecchinato, R.; Redaelli, A.; Martini, C.; Morselli, C.; Villafañe, J.H.; Lamartina, C.; Berjano, P. Long fusions to S1 with or without pelvic fixation can induce relevant acute variations in pelvic incidence: A retrospective cohort study of adult spine deformity surgery. Eur. Spine J. 2017, 26 (Suppl. S4), 436–441. [Google Scholar] [CrossRef]
- Oba, H.; Ebata, S.; Takahashi, J.; Ikegami, S.; Koyama, K.; Haro, H.; Kato, H.; Ohba, T. Loss of Pelvic Incidence Correction After Long Fusion Using Iliac Screws for Adult Spinal Deformity: Cause and effect on clinical outcome. Spine 2019, 44, 195–202. [Google Scholar] [CrossRef]
- Arshad, R.; Pan, F.; Reitmaier, S.; Schmidt, H. Effect of age and sex on lumbar lordosis and the range of motion. A systematic review and meta-analysis. J. Biomech. 2019, 82, 1–19. [Google Scholar] [CrossRef]
- Dreischarf, M.; Albiol, L.; Rohlmann, A.; Pries, E.; Bashkuev, M.; Zander, T.; Duda, G.; Druschel, C.; Strube, P.; Putzier, M.; et al. Age-Related Loss of Lumbar Spinal Lordosis and Mobility—A Study of 323 Asymptomatic Volunteers. PLoS ONE 2014, 9, e116186. [Google Scholar] [CrossRef]
- Hammerberg, E.M.; Wood, K.B. Sagittal Profile of the Elderly. J. Spinal Disord. Technol. 2003, 16, 44–50. [Google Scholar] [CrossRef]
- Zhou, S.; Sun, Z.; Li, W.; Wang, W.; Su, T.; Du, C.; Li, W. The standing and sitting sagittal spinopelvic alignment of Chinese young and elderly population: Does age influence the differences between the two positions? Eur. Spine J. 2020, 29, 405–412. [Google Scholar] [CrossRef] [PubMed]
- Nishimura, T.; Miyachi, R. Relationship between low back pain and lumbar and hip joint movement in desk workers. J. Phys. Ther. Sci. 2020, 32, 680–685. [Google Scholar] [CrossRef] [PubMed]
- Pizones, J.; García-Rey, E. Pelvic motion the key to understanding spine–hip interaction. EFORT Open Rev. 2020, 5, 522–533. [Google Scholar] [CrossRef] [PubMed]
- Buckland, A.J.; Burapachaisri, A.; Stekas, N.; Vasquez-Montes, D.; Protopsaltis, T.; Vigdorchik, J. Obesity Alters Spinopelvic Alignment Changes from Standing to Relaxed Sitting: The Influence of the Soft-tissue Envelope. Arthroplast. Today 2020, 6, 590–595.e1. [Google Scholar] [CrossRef]
- Haffer, H.; Wang, Z.; Hu, Z.; Becker, L.; Müllner, M.; Hipfl, C.; Pumberger, M.; Palmowski, Y. Does obesity affect acetabular cup position, spinopelvic function and sagittal spinal alignment? A prospective investigation with standing and sitting assessment of primary hip arthroplasty patients. J. Orthop. Surg. Res. 2021, 16, 640. [Google Scholar] [CrossRef]
- Gilleard, W.; Smith, T. Effect of obesity on posture and hip joint moments during a standing task, and trunk forward flexion motion. Int. J. Obes. 2007, 31, 267–271. [Google Scholar] [CrossRef]
- Romero-Vargas, S.; Zárate-Kalfópulos, B.; Otero-Cámara, E.; Rosales-Olivarez, L.; Alpízar-Aguirre, A.; Morales-Hernández, E.; Reyes-Sánchez, A. The impact of body mass index and central obesity on the spino-pelvic parameters: A correlation study. Eur. Spine J. 2013, 22, 878–882. [Google Scholar] [CrossRef]
- Loppini, M.; Longo, U.G.; Ragucci, P.; Trenti, N.; Balzarini, L.; Grappiolo, G. Analysis of the Pelvic Functional Orientation in the Sagittal Plane: A Radiographic Study with EOS 2D/3D Technology. J. Arthroplast. 2017, 32, 1027–1032. [Google Scholar] [CrossRef]
- Sardar, Z.M.; Cerpa, M.; Kelly, M.; Bourret, S.; Hasegawa, K.; Wong, H.-K.; Liu, G.; Hey, H.W.D.; Riahi, H.; Le Huec, J.-C.; et al. Age and Gender Based Spinopelvic and Regional Spinal Alignment in Asymptomatic Adult Volunteers: Results of the Multi-Ethnic Alignment Normative Study (MEANS). Spine 2022, 47, 1382–1390. [Google Scholar] [CrossRef]
- Hay, O.; Dar, G.; Abbas, J.; Stein, D.; May, H.; Masharawi, Y.; Peled, N.; Hershkovitz, I. The Lumbar Lordosis in Males and Females, Revisited. PLoS ONE 2015, 10, e0133685. [Google Scholar] [CrossRef]
- Whitcome, K.K.; Shapiro, L.J.; Lieberman, D.E. Fetal load and the evolution of lumbar lordosis in bipedal hominins. Nature 2007, 450, 1075–1078. [Google Scholar] [CrossRef] [PubMed]
- Warashina, H.; Kato, M.; Kitamura, S.; Kusano, T.; Hasegawa, Y. The progression of osteoarthritis of the hip increases degenerative lumbar spondylolisthesis and causes the change of spinopelvic alignment. J. Orthop. 2019, 16, 275–279. [Google Scholar] [CrossRef] [PubMed]
- Balmaceno-Criss, M.; Lafage, R.; Alsoof, D.; Daher, M.; Hamilton, D.K.; Smith, J.S.; Eastlack, R.K.; Fessler, R.G.; Gum, J.L.; Gupta, M.C.; et al. Impact of Hip and Knee Osteoarthritis on Full Body Sagittal Alignment and Compensation for Sagittal Spinal Deformity. Spine 2024, 49, 743–751. [Google Scholar] [CrossRef]
- Hooker, Q.L.; Lanier, V.M.; van Dillen, L.R. Consistent differences in lumbar spine alignment between low back pain subgroups and genders during clinical and functional activity sitting tests. Musculoskelet. Sci. Pract. 2021, 52, 102336. [Google Scholar] [CrossRef]

| Variable | Overall 1 |
|---|---|
| Number of Patients | 1447 |
| Age (years) | 63.59 (10.85) |
| BMI (kg/m2) | 28.81 (5.70) |
| Gender (%) Female | 795 (54.9) |
| Male | 652 (45.1) |
| Standing PI (°) | 51.67 (10.75) |
| Standing PT (°) | 14.21 (8.99) |
| Standing SS | 37.46 (8.59) |
| Standing LL (°) | 48.49 (12.21) |
| Standing PI-LL (°) | 3.18 (12.63) |
| Sitting PI (°) | 56.19 (10.75) |
| Sitting PT (°) | 33.41 (11.41) |
| Sitting SS (°) | 22.78 (8.79) |
| Sitting LL (°) | 30.05 (11.92) |
| Sitting PI-LL (°) | 26.14 (13.97) |
| ΔPI (°) | −4.52 (5.68) |
| ΔPT (°) | −19.20 (11.00) |
| ΔSS (°) | 14.67 (10.18) |
| ΔLL (°) | 18.44 (13.29) |
| Variable | Group 1 1 | Group 2 1 | Group 3 1 | p-Value |
|---|---|---|---|---|
| Number of Patients | 490 | 531 | 426 | |
| Age (years) | 51.88 (7.11) | 64.65 (2.84) | 75.72 (5.05) | <0.001 |
| BMI (kg/m2) | 29.94 (6.13) | 28.71 (5.63) | 27.65 (5.00) | <0.001 |
| Gender (%) Female | 260 (53.1) | 280 (52.7) | 255 (59.9) | 0.052 |
| Male | 230 (46.9) | 251 (47.3) | 171 (40.1) | |
| ΔPI (°) | −4.90 [−8.17, −1.50] | −3.90 [−7.90, −0.70] | −4.20 [−7.27, −0.60] | 0.027 |
| ΔPT (°) | −23.00 [−30.87, −14.03] | −18.10 [−24.85, −11.10] | −15.20 [−22.08, −8.60] | <0.001 |
| ΔSS (°) | 17.15 [9.90, 25.20] | 13.70 [7.65, 20.75] | 10.45 [5.22, 16.70] | <0.001 |
| ΔLL (°) | 24.95 [14.18, 33.18] | 17.90 [9.35, 26.00] | 12.90 [4.60, 20.20] | <0.001 |
| Variable | Group 1 1 | Group 2 1 | Group 3 1 | p-Value |
|---|---|---|---|---|
| Number of Patients | 397 | 498 | 546 | |
| Age (years) | 64.96 (10.75) | 64.89 (11.53) | 61.51 (9.88) | <0.001 |
| BMI (kg/m2) | 22.47 (1.90) | 27.48 (1.42) | 34.63 (4.07) | <0.001 |
| Gender (%) Female | 295 (74.3) | 235 (47.2) | 263 (48.2) | <0.001 |
| Male | 102 (25.7) | 263 (52.8) | 283 (51.8) | |
| ΔPI (°) | −3.90 [−7.40, −1.00] | −3.85 [−6.90, −0.52] | −5.05 [−9.10, −1.50] | <0.001 |
| ΔPT (°) | −16.40 [−24.80, −9.70] | −18.10 [−25.15, −10.83] | −20.10 [−28.58, −12.60] | <0.001 |
| ΔSS (°) | 11.80 [6.40, 19.80] | 13.95 [7.32, 21.78] | 14.65 [8.03, 22.90] | 0.003 |
| ΔLL (°) | 16.70 [8.40, 25.60] | 19.00 [9.03, 27.98] | 18.50 [8.90, 28.48] | 0.065 |
| Variable | Female 1 | Male 1 | p-Value |
|---|---|---|---|
| Number of Patients | 795 | 652 | |
| Age (years) | 64.26 (10.69) | 62.77 (11.00) | 0.009 |
| BMI (kg/m2) | 27.95 (5.99) | 29.86 (5.14) | <0.001 |
| ΔPI (°) | −4.40 [−7.90, −1.20] | −4.10 [−7.70, −0.70] | 0.178 |
| ΔPT (°) | −17.40 [−25.00, −10.60] | −19.80 [−28.22, −11.78] | 0.001 |
| ΔSS (°) | 12.60 [6.60, 20.40] | 15.50 [8.10, 23.20] | <0.001 |
| ΔLL (°) | 17.30 [8.40, 25.75] | 19.40 [9.90, 29.20] | 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Durbas, A.; Subramanian, T.; Simon, C.; Allen, M.R.J.; Samuel, J.; Colón, L.F.; Mazzucco, M.R.; Pagan, C.; Karasavvidis, T.; Vigdorchik, J.; et al. Evaluating Variations in Spinopelvic Parameters from Sitting to Standing: A Comparative Analysis of 1447 Older Adults Across Age, BMI, and Gender Subgroups. J. Clin. Med. 2025, 14, 2952. https://doi.org/10.3390/jcm14092952
Durbas A, Subramanian T, Simon C, Allen MRJ, Samuel J, Colón LF, Mazzucco MR, Pagan C, Karasavvidis T, Vigdorchik J, et al. Evaluating Variations in Spinopelvic Parameters from Sitting to Standing: A Comparative Analysis of 1447 Older Adults Across Age, BMI, and Gender Subgroups. Journal of Clinical Medicine. 2025; 14(9):2952. https://doi.org/10.3390/jcm14092952
Chicago/Turabian StyleDurbas, Atahan, Tejas Subramanian, Chad Simon, Myles R. J. Allen, Justin Samuel, Luis Felipe Colón, Michael R. Mazzucco, Cale Pagan, Theofilos Karasavvidis, Jonathan Vigdorchik, and et al. 2025. "Evaluating Variations in Spinopelvic Parameters from Sitting to Standing: A Comparative Analysis of 1447 Older Adults Across Age, BMI, and Gender Subgroups" Journal of Clinical Medicine 14, no. 9: 2952. https://doi.org/10.3390/jcm14092952
APA StyleDurbas, A., Subramanian, T., Simon, C., Allen, M. R. J., Samuel, J., Colón, L. F., Mazzucco, M. R., Pagan, C., Karasavvidis, T., Vigdorchik, J., Cunningham, M. E., Kim, H. J., & Lovecchio, F. C. (2025). Evaluating Variations in Spinopelvic Parameters from Sitting to Standing: A Comparative Analysis of 1447 Older Adults Across Age, BMI, and Gender Subgroups. Journal of Clinical Medicine, 14(9), 2952. https://doi.org/10.3390/jcm14092952







