Endothelial Activation and Stress Index—A Novel and Simple Prognostic Tool in Coronary Artery Bypass Grafting
Abstract
1. Introduction
2. Material and Methods
2.1. Patient Sample Collection and EASIX Score
2.2. Surgical Procedure
3. Statistics
4. Results
4.1. Determination of Cut-Off Value EASIX ≥ 1.16
4.2. Baseline Characteristics
4.3. Intraoperative Data
4.4. Postoperative Outcomes
4.5. Mid- and Long-Term Outcomes
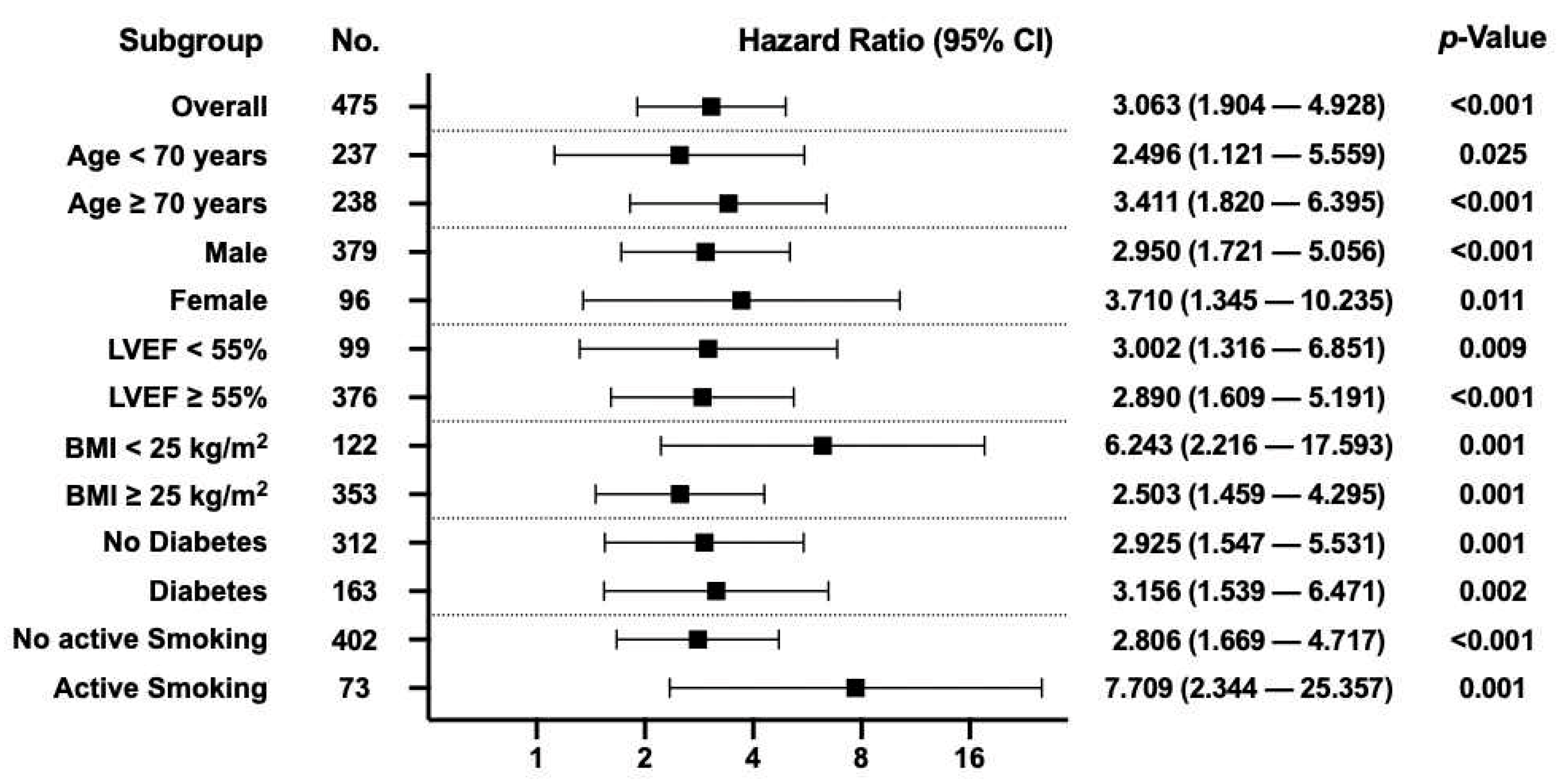
4.6. EASIX as Independent Risk Factor for Long-Term Mortality in CABG
5. Discussion
6. Limitations of the Study
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AF | Atrial Fibrillation |
| alloSCT | Allogeneic Hematopoietic Stem-Cell Transplantation |
| AUC | Area Under the Curve |
| CABG | Coronary Artery Bypass Grafting |
| CAD | Coronary Artery Disease |
| COPD | Chronic Obstructive Pulmonary Disease |
| CV | Cardiovascular |
| EASIX | Endothelial Activation and Stress Index |
| eGFR | Estimated Glomerular Filtration Rate |
| ESC | European Society of Cardiology |
| HR | Hazard Ratio |
| ICH-GCP | International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use—Good Clinical Practice |
| LDH | Lactate Dehydrogenase |
| LVEF | Left Ventricular Ejection Fraction |
| MI | Myocardial Infarction |
| NYHA | New York Heart Association |
| PAOD | Peripheral Arterial Obstructive Disease |
| PCI | Percutaneous Coronary Intervention |
| SD | Standard Deviation |
| STEMI | ST elevation myocardial infarction |
| YI | Youden Index |
References
- Penack, O.; Luft, T.; Peczynski, C.; Benner, A.; Sica, S.; Arat, M.; Itäla-Remes, M.; Corral, L.L.; Schaap, N.P.M.; Karas, M.; et al. Endothelial Activation and Stress Index (EASIX) to predict mortality after allogeneic stem cell transplantation: A prospective study. J. Immunother. Cancer 2024, 12, e007635. [Google Scholar] [CrossRef] [PubMed]
- Park, S.; Go, S.-I.; Lee, G.-W. The Endothelial Activation and Stress Index (EASIX) score is an independent prognostic factor in patients with diffuse large B-cell lymphoma. BMC Cancer 2022, 22, 816. [Google Scholar] [CrossRef]
- Song, G.-Y.; Jung, S.-H.; Kim, K.; Kim, S.J.; Yoon, S.E.; Lee, H.S.; Kim, M.; Ahn, S.-Y.; Ahn, J.-S.; Yang, D.-H.; et al. Endothelial activation and stress index (EASIX) is a reliable predictor for overall survival in patients with multiple myeloma. BMC Cancer 2020, 20, 803. [Google Scholar] [CrossRef] [PubMed]
- Kalicińska, E.; Biernat, M.; Rybka, J.; Zińczuk, A.; Janocha-Litwin, J.; Rosiek-Biegus, M.; Morawska, M.; Waszczuk-Gajda, A.; Drozd-Sokołowska, J.; Szukalski, Ł.; et al. Endothelial Activation and Stress Index (EASIX) as an Early Predictor for Mortality and Overall Survival in Hematological and Non-Hematological Patients with COVID-19: Multicenter Cohort Study. J. Clin. Med. 2021, 10, 4373. [Google Scholar] [CrossRef]
- Luft, T.; Wendtner, C.-M.; Kosely, F.; Radujkovic, A.; Benner, A.; Korell, F.; Kihm, L.; Bauer, M.F.; Dreger, P.; Merle, U. EASIX for Prediction of Outcome in Hospitalized SARS-CoV-2 Infected Patients. Front. Immunol. 2021, 12, 634416. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.; Jiang, Y.; He, M.; Xu, J. EASIX is an effective marker in predicting mortality of traumatic brain injury patients. Eur. J. Med. Res. 2024, 29, 300. [Google Scholar] [CrossRef]
- Shahian, D.M.; O’Brien, S.M.; Filardo, G.; Ferraris, V.A.; Haan, C.K.; Rich, J.B.; Normand, S.-L.T.; DeLong, E.R.; Shewan, C.M.; Dokholyan, R.S.; et al. The Society of Thoracic Surgeons 2008 Cardiac Surgery Risk Models: Part 1-Coronary Artery Bypass Grafting Surgery. Ann. Thorac. Surg. 2009, 88 (Suppl. 1), S2–S22. [Google Scholar] [CrossRef]
- Biancari, F.; Vasques, F.; Mikkola, R.; Martin, M.; Lahtinen, J.; Heikkinen, J. Validation of EuroSCORE II in Patients Undergoing Coronary Artery Bypass Surgery. Ann. Thorac. Surg. 2012, 93, 1930–1935. [Google Scholar] [CrossRef]
- Thygesen, K.; Alpert, J.S.; Jaffe, A.S.; Simoons, M.L.; Chaitman, B.R.; White, H.D. Third universal definition of myocardial infarction. J. Am. Coll. Cardiol. 2012, 60, 1581–1598. [Google Scholar] [CrossRef]
- Demir, F.A.; Ersoy, I.; Yılmaz, A.Ş.; Taylan, G.; Kaya, E.E.; Aydın, E.; Karakayalı, M.; Öğütveren, M.M.; Acar, A.T.; Hidayet, Ş. Serum glucose–potassium ratio predicts inhospital mortality in patients admitted to coronary care unit. Rev. Assoc. Med. Bras. 2024, 70, e20240508. [Google Scholar] [CrossRef]
- Tanriverdi, Z.; Gungoren, F.; Tascanov, M.B.; Besli, F.; Altiparmak, I.H. Comparing the Diagnostic Value of the C-Reactive Protein to Albumin Ratio with Other Inflammatory Markers in Patients with Stable Angina Pectoris. Angiology 2020, 71, 360–365. [Google Scholar] [CrossRef]
- Karakayali, M.; Altunova, M.; Yakisan, T.; Aslan, S.; Omar, T.; Artac, I.; Ilis, D.; Arslan, A.; Cagin, Z.; Karabag, Y.; et al. A Relação entre o Índice de Imuno-Inflamação Sistêmica e Isquemia com Artérias Coronárias Não Obstrutivas em Pacientes Submetidos à Angiografia Coronária. Arq. Bras. Cardiol. 2024, 121, e20230540. [Google Scholar] [CrossRef]
- Sündermann, S.H.; Bäck, C.; Bischoff-Ferrari, H.A.; Dehbi, H.-M.; Szekely, A.; Völler, H.; Niebauer, J. Preinterventional frailty assessment in patients scheduled for cardiac surgery or transcatheter aortic valve implantation: A consensus statement of the European Association for Cardio-Thoracic Surgery (EACTS) and the European Association of Preventive Cardiology (EAPC) of the European Society of Cardiology (ESC). Eur. J. Cardio-Thorac. Surg. 2023, 64, 146–181. [Google Scholar] [CrossRef]
- Krombholz-Reindl, P.; Winkler, A.; Vötsch, A.; Hitzl, W.; Schernthaner, C.; Hecht, S.; Seitelberger, R.; Gottardi, R. Thoracic sarcopenia measured by Hounsfield unit average calculation predicts morbidity and mortality in coronary artery bypass grafting. Eur. J. Cardio-Thorac. Surg. 2024, 66, ezae303. [Google Scholar] [CrossRef] [PubMed]
- Finke, D.; Hund, H.; Frey, N.; Luft, T.; Lehmann, L.H. EASIX (endothelial activation and stress index) predicts mortality in patients with coronary artery disease. In Clinical Research in Cardiology; Springer: Berlin/Heidelberg, Germany, 2024. [Google Scholar] [CrossRef]
- Byrne, R.A.; Rossello, X.; Coughlan, J.J.; Barbato, E.; Berry, C.; Chieffo, A.; Claeys, M.J.; Dan, G.-A.; Dweck, M.R.; Galbraith, M.; et al. 2023 ESC Guidelines for the management of acute coronary syndromes. Eur. Heart J. 2023, 44, 3720–3826. [Google Scholar] [CrossRef] [PubMed]
- Luckraz, H.; Norell, M.; Buch, M.; James, R.; Cooper, G. Structure and functioning of a multidisciplinary ‘Heart Team’ for patients with coronary artery disease: Rationale and recommendations from a joint BCS/BCIS/SCTS working group. Eur. J. Cardio-Thorac. Surg. 2015, 48, 524–529. [Google Scholar] [CrossRef]
- Sousa-Uva, M.; Neumann, F.-J.; Ahlsson, A.; Alfonso, F.; Banning, A.P.; Benedetto, U.; Byrne, R.A.; Collet, J.-P.; Falk, V.; Head, S.J.; et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur. J. Cardio-Thorac. Surg. 2019, 55, 4–90. [Google Scholar] [CrossRef]
- Erdfelder, E.; Faul, F.; Buchner, A. GPOWER: A general power analysis program. Behav. Res. Methods 2007, 39. [Google Scholar] [CrossRef]
- Widmer, R.J.; Lerman, A. Endothelial dysfunction and cardiovascular disease. Glob. Cardiol. Sci. Pract. 2014, 2014, 43. [Google Scholar] [CrossRef]
- Pacinella, G.; Ciaccio, A.M.; Tuttolomondo, A. Endothelial Dysfunction and Chronic Inflammation: The Cornerstones of Vascular Alterations in Age-Related Diseases. Int. J. Mol. Sci. 2022, 23, 15722. [Google Scholar] [CrossRef]
- O’Boyle, F.; Mediratta, N.; Fabri, B.; Pullan, M.; Chalmers, J.; McShane, J.; Shaw, M.; Poullis, M. Long-term survival after coronary artery bypass surgery stratified by EuroSCORE. Eur. J. Cardio-Thorac. Surg. 2012, 42, 101–107. [Google Scholar] [CrossRef] [PubMed]
- Sang, M.; Ma, X.; Zhu, F.; Zhu, C.; Ying, Z. Association between endothelial activation and stress index and 30-day mortality risk in acute myocardial infarction patients: A study based on the medical information mart for intensive care-IV database. BMC Cardiovasc. Disord. 2024, 24, 699. [Google Scholar] [CrossRef] [PubMed]


| Total | EASIX < 1.16 | EASIX ≥ 1.16 | p-Value | |
|---|---|---|---|---|
| No. (%) | ||||
| Total | 475 (100.0) | 355 (74.7) | 120 (25.3) | - |
| Sex (male) | 379 (79.8) | 278 (78.3) | 101 (84.2) | 0.167 |
| Age > 70 years | 238 (50.1) | 158 (44.5) | 80 (66.7) | <0.001 |
| BMI ≥ 25.0 kg/m2 | 353 (74.3) | 259 (73.0) | 94 (78.3) | 0.244 |
| Arterial Hypertension | 428 (90.1) | 318 (89.6) | 110 (91.7) | 0.508 |
| Diabetes Mellitus | 163 (34.3) | 117 (33.0) | 46 (38.3) | 0.284 |
| Dyslipidemia | 421 (88.6) | 311 (87.6) | 110 (91.7) | 0.226 |
| Familiar History of CV Disease | 123 (25.9) | 99 (27.9) | 24 (20.0) | 0.088 |
| PAOD | 59 (12.4) | 34 (9.6) | 25 (20.8) | 0.001 |
| COPD | 0.782 | |||
| I° | 51 (10.7) | 36 (10.1) | 15 (12.5) | |
| II° | 16 (3.4) | 12 (3.4) | 4 (3.3) | |
| III° | 5 (1.1) | 3 (0.8) | 2 (1.7) | |
| AF | 41 (8.6) | 23 (6.5) | 18 (15.0) | 0.004 |
| Active Smoker | 73 (15.4) | 64 (18.0) | 9 (7.5) | 0.006 |
| Prior Stroke | 43 (9.1) | 29 (8.2) | 14 (11.7) | 0.248 |
| Prior MI | 162 (34.1) | 111 (31.3) | 51 (42.5) | 0.025 |
| eGFR | <0.001 | |||
| ≥90 mL/min/BSA | 193 (40.3) | 175 (49.3) | 18 (15.0) | |
| 60–89 mL/min/BSA | 233 (49.1) | 170 (47.9) | 63 (52.5) | |
| 31–59 mL/min/BSA | 40 (8.4) | 10 (2.8) | 30 (25.0) | |
| ≤30 mL/min/BSA | 9 (1.9) | 0 (0.0) | 9 (7.5) | |
| NYHA | 0.684 | |||
| I | 138 (29.1) | 108 (30.4) | 30 (25.0) | |
| II | 182 (38.3) | 135 (38.0) | 47 (39.2) | |
| III | 88 (18.5) | 63 (17.7) | 25 (20.8) | |
| IV | 67 (14.1) | 49 (13.8) | 18 (15.0) | |
| LVEF | 0.317 | |||
| ≥55% | 376 (79.2) | 287 (80.8) | 89 (74.2) | |
| 41–54% | 56 (11.8) | 37 (10.4) | 19 (15.8) | |
| 31–40% | 22 (4.6) | 17 (4.8) | 5 (4.2) | |
| ≤30% | 21 (4.4) | 14 (3.9) | 7 (5.8) | |
| Median ± IQR | ||||
| Age (years) | 70.0 ± 14.0 | 68.0 ± 14.0 | 74.0 ± 11.0 | <0.001 |
| Height (cm) | 172.0 ± 11.0 | 172.0 ± 11.0 | 172.0 ± 11.0 | 0.928 |
| Weight (kg) | 82.0 ± 18.0 | 82.0 ± 19.0 | 80.5 ± 19.0 | 0.777 |
| BMI (kg/m2) | 27.9 ± 5.5 | 27.5 ± 5.6 | 27.3 ± 5.5 | 0.551 |
| EuroSCORE II | 1.6 ± 1.9 | 1.5 ± 1.4 | 2.6 ± 3.1 | <0.001 |
| Creatinine (mg/dl) | 1.0 ± 0.3 | 0.9 ± 0.2 | 1.3 ± 0.5 | <0.001 |
| eGFR (mL/min/BSA) | 77.4 ± 38.6 | 83.3 ± 37.8 | 59.4 ± 33.2 | <0.001 |
| Platelet Count (109/L) | 229.0 ± 77.0 | 242.0 ± 71.0 | 186.0 ± 65.8 | <0.001 |
| LDH (U/L) | 204.0 ± 50.0 | 198.0 ± 42.0 | 226.5 ± 70.0 | <0.001 |
| CRP (mg/dL) | 0.2 ± 0.5 | 0.2 ± 0.4 | 0.4 ± 0.8 | <0.001 |
| Hemoglobin (g/dL) | 14.2 ± 2.1 | 14.3 ± 1.9 | 13.7 ± 2.2 | 0.001 |
| Total | EASIX < 1.16 | EASIX ≥ 1.16 | p-Value | |
|---|---|---|---|---|
| No. (%) | ||||
| On-pump CABG | 435 (91.6) | 330 (93.0) | 105 (87.5) | 0.063 |
| CABG via Left Thoracotomy | 4 (0.8) | 2 (0.6) | 2 (1.7) | 0.839 |
| ITA Configuration | <0.001 | |||
| None | 41 (8.6) | 25 (7.0) | 16 (13.3) | |
| LIMA | 246 (51.8) | 175 (49.3) | 71 (59.2) | |
| RIMA | 35 (7.4) | 28 (7.9) | 7 (5.8) | |
| BIMA | 153 (32.2) | 127 (35.8) | 26 (21.7) | |
| IABP used | 7 (1.6) | 5 (1.4) | 2 (1.7) | 0.253 |
| ECMO used | 6 (1.3) | 5 (1.4) | 1 (0.8) | 0.626 |
| Mean ± SD | ||||
| Intraoperative packed red blood cells/patient | 0.3 ± 0.9 | 0.2 ± 0.9 | 0.4 ± 0.7 | 0.177 |
| Median ± IQR | ||||
| Perfusion Time (min) | 93.0 ± 49.0 | 94.0 ± 51.0 | 88.0 ± 45.8 | 0.090 |
| Aortic Cross-clamp Time (min) | 49.0 ± 27.0 | 50.0 ± 28.0 | 45.0 ± 27.5 | 0.028 |
| Arterial Bypass Grafts | 2.0 ± 1.0 | 2.0 ± 1.0 | 1.0 ± 1.0 | 0.001 |
| Venous Bypass Grafts | 1.0 ± 2.0 | 1.0 ± 2.0 | 2.0 ± 1.8 | 0.030 |
| Total | EASIX < 1.16 | EASIX ≥ 1.16 | p-Value | |
|---|---|---|---|---|
| No. (%) | ||||
| 30-day mortality | 9 (1.9) | 3 (0.8) | 6 (5.0) | 0.004 |
| Major Neurological Events | 8 (1.7) | 6 (1.7) | 2 (1.7) | 0.986 |
| Perioperative MI | 8 (1.7) | 4 (1.1) | 4 (3.3) | 0.104 |
| AKI requiring Hemodialysis | 7 (1.5) | 3 (0.8) | 4 (3.3) | 0.051 |
| Sternal Wound Infection | 17 (3.6) | 9 (2.5) | 8 (6.7) | 0.035 |
| AF (new onset) | 109 (22.9) | 78 (22.0) | 31 (25.8) | 0.384 |
| Reoperation due to Bleeding/Tamponade | 8 (1.7) | 7 (2.0) | 1 (0.8) | 0.402 |
| Prolonged Ventilation ≥ 48 h | 26 (5.5) | 15 (4.2) | 11 (9.2) | 0.040 |
| Reintubation Rate | 17 (3.6) | 11 (3.1) | 6 (5.0) | 0.332 |
| Reoperation/Reintervention due to Graft occlusion | 7 (1.5) | 4 (1.1) | 3 (2.5) | 0.280 |
| Median ± IQR | ||||
| Invasive Ventilation Time (h) | 5.0 ± 4.0 | 5.0 ± 3.0 | 6.0 ± 5.0 | 0.013 |
| Intensive Care Unit Stay (d) | 2.0 ± 2.0 | 2.0 ± 2.0 | 2.0 ± 3.8 | 0.002 |
| Cox Regression Analysis | Univariate | Multivariable | ||
|---|---|---|---|---|
| Hazard Ratio (95% CI) | p-Value | Hazard Ratio (95% CI) | p-Value | |
| Long-Term Mortality | ||||
| EASIX | 3.063 (1.904–4.928) | <0.001 | 2.652 (1.593–4.415) | <0.001 |
| Sex (male) | 0.892 (0.502–1.582) | 0.695 | ||
| Age | 1.420 (1.086–1.856) | 0.010 | 1.109 (0.795–1.549) | 0.542 |
| Weight | 0.952 (0.750–1.208) | 0.685 | ||
| Height | 1.201 (0.955–1.510) | 0.117 | ||
| BMI | 1.238 (1.000–1.533) | 0.050 | 1.336 (1.027–1.738) | 0.031 |
| EuroSCORE II | 1.389 (1.226–1.573) | <0.001 | 1.017 (0.808–1.280) | 0.886 |
| Arterial Hypertension | 7.494 (1.040–53.985) | 0.046 | 4.345 (0.600–31.455) | 0.146 |
| Diabetes mellitus | 1.565 (0.970–2.526) | 0.067 | 1.214 (0.716–2.058) | 0.472 |
| Dyslipidemia | 1.201 (0.549–2.628) | 0.646 | ||
| Family History of CV Disease | 0.789 (0.445–1.400) | 0.419 | ||
| Active Cancer | 2.258 (1.076–4.739) | 0.031 | 2.152 (0.974–4.752) | 0.058 |
| PAOD | 2.513 (1.434–4.404) | 0.001 | 1.410 (0.724–2.745) | 0.312 |
| COPD | 1.381 (0.983–1.940) | 0.063 | 0.990 (0.675–1.453) | 0.961 |
| Prior Stroke | 1.716 (0.850–3.464) | 0.132 | ||
| Prior MI | 1.379 (0.851–2.235) | 0.192 | ||
| Active Smoker | 1.205 (0.631–2.301) | 0.572 | ||
| Atrial fibrillation | 2.038 (1.041–3.990) | 0.038 | 1.495 (0.700–3.193) | 0.299 |
| Left Main Lesion | 1.251 (0.777–2.014) | 0.357 | ||
| NYHA | 1.570 (0.969–2.546) | 0.067 | 1.189 (0.901–1.571) | 0.221 |
| eGFR | 0.623 (0.475–0.817) | 0.001 | 0.761 (0.544–1.064) | 0.110 |
| CRP | 1.164 (0.982–1.379) | 0.079 | 1.165 (0.959–1.416) | 0.125 |
| Hemoglobin | 0.768 (0.654–0.901) | 0.001 | 0.725 (0.586–0.897) | 0.003 |
| LVEF | 0.475 (0.287–0.785) | 0.004 | 1.379 (1.077–1.767) | 0.011 |
| Mitral Valve Regurgitation | 1.400 (0.970–2.019) | 0.072 | 0.946 (0.618–1.449) | 0.800 |
| Tricuspid Valve Regurgitation | 1.281 (0.855–1.919) | 0.230 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Krombholz-Reindl, P.; Vötsch, A.; Linni, K.; Seitelberger, R.; Gottardi, R.; Lichtenauer, M.; Hammerer, M.; Boxhammer, E.; Winkler, A. Endothelial Activation and Stress Index—A Novel and Simple Prognostic Tool in Coronary Artery Bypass Grafting. J. Clin. Med. 2025, 14, 2857. https://doi.org/10.3390/jcm14082857
Krombholz-Reindl P, Vötsch A, Linni K, Seitelberger R, Gottardi R, Lichtenauer M, Hammerer M, Boxhammer E, Winkler A. Endothelial Activation and Stress Index—A Novel and Simple Prognostic Tool in Coronary Artery Bypass Grafting. Journal of Clinical Medicine. 2025; 14(8):2857. https://doi.org/10.3390/jcm14082857
Chicago/Turabian StyleKrombholz-Reindl, Philipp, Andreas Vötsch, Klaus Linni, Rainald Seitelberger, Roman Gottardi, Michael Lichtenauer, Matthias Hammerer, Elke Boxhammer, and Andreas Winkler. 2025. "Endothelial Activation and Stress Index—A Novel and Simple Prognostic Tool in Coronary Artery Bypass Grafting" Journal of Clinical Medicine 14, no. 8: 2857. https://doi.org/10.3390/jcm14082857
APA StyleKrombholz-Reindl, P., Vötsch, A., Linni, K., Seitelberger, R., Gottardi, R., Lichtenauer, M., Hammerer, M., Boxhammer, E., & Winkler, A. (2025). Endothelial Activation and Stress Index—A Novel and Simple Prognostic Tool in Coronary Artery Bypass Grafting. Journal of Clinical Medicine, 14(8), 2857. https://doi.org/10.3390/jcm14082857






