Evaluation of the Effectiveness of Animated Images in First Aid for Infants with Foreign Body Airway Obstruction: A Simulation Study
Abstract
1. Introduction
2. Materials and Methods
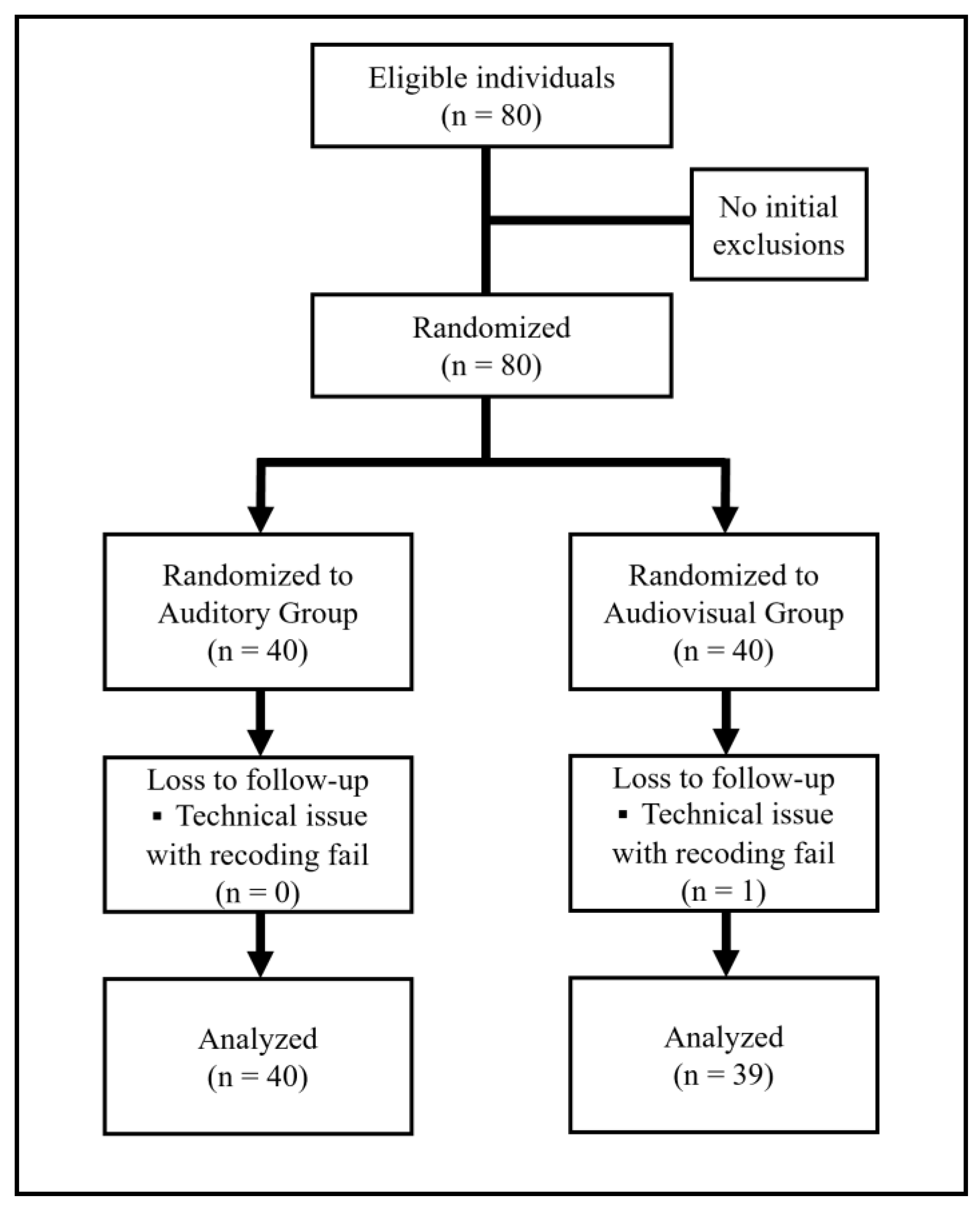
2.1. Study Design and Setting
2.2. Selection of Participants
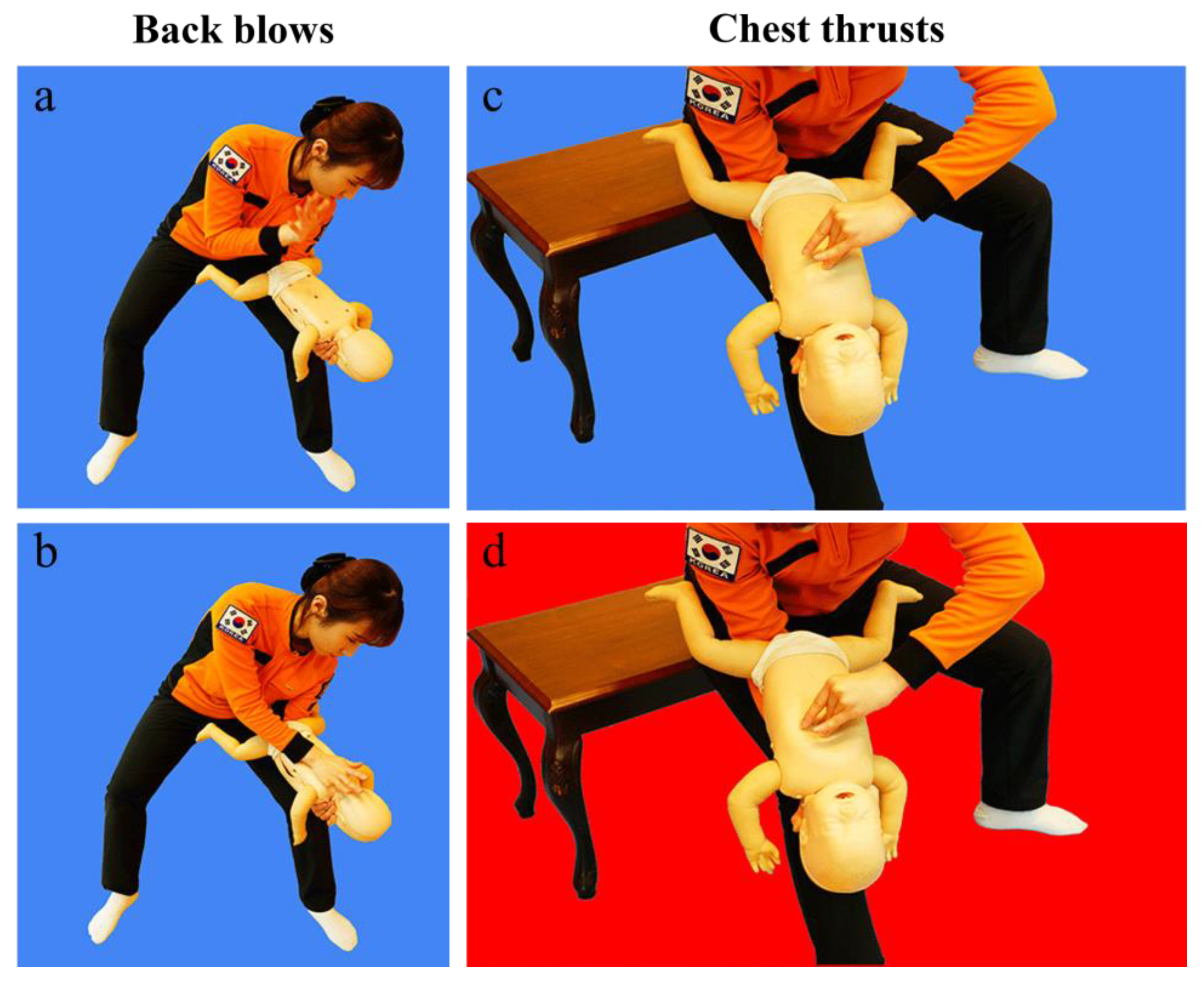
2.3. Interventions
2.4. Randomization
2.5. Outcomes
2.6. Statistical Analysis
3. Results
3.1. General Characteristics
3.2. Comparative Analysis of the Auditory and Audiovisual Groups
3.3. Analysis According to Prior Relevant Training Experience
3.3.1. Comparative Analysis of the Auditory and Audiovisual Groups with Prior Relevant Training
3.3.2. Comparative Analysis of the Auditory and Audiovisual Groups Without Prior Relevant Training
3.4. Analysis According to Sex
3.4.1. Comparative Analysis of the Auditory and Audiovisual Groups Among Male Participants
3.4.2. Comparative Analysis of the Auditory and Audiovisual Groups Among Female Participants
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| FBAO | Foreign body airway obstruction |
| IP | Instruction Performance |
| GIFs | Graphics interchange formats |
Appendix A
| Auditory group |
|
| Audiovisual group |
|
References
- Igarashi, Y.; Norii, T.; Sung-Ho, K.; Nagata, S.; Yoshino, Y.; Hamaguchi, T.; Nagaosa, R.; Nakao, S.; Tagami, T.; Yokobori, S. Airway obstruction time and outcomes in patients with foreign body airway obstruction: Multicenter observational choking investigation. Acute Med. Surg. 2022, 9, e741. [Google Scholar] [CrossRef] [PubMed]
- Topjian, A.A.; Raymond, T.T.; Atkins, D.; Chan, M.; Duff, J.P.; Joyner, B.L., Jr.; Lasa, J.J.; Lavonas, E.J.; Levy, A.; Mahgoub, M.; et al. Part 4: Pediatric basic and advanced life support: 2020 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2020, 142, S469–S523. [Google Scholar] [CrossRef]
- Igarashi, Y.; Suzuki, K.; Norii, T.; Motomura, T.; Yoshino, Y.; Kitagoya, Y.; Ogawa, S.; Yokobori, S.; Yokota, H. Do video calls improve dispatcher-assisted first aid for infants with foreign body airway obstruction? A randomized controlled trial/simulation study. J. Nippon. Med. Sch. 2022, 89, 526–532. [Google Scholar] [CrossRef]
- Aldridge, E.S.; Perera, N.; Ball, S.; Birnie, T.; Morgan, A.; Whiteside, A.; Bray, J.; Finn, J. Barriers to CPR initiation and continuation during the emergency call relating to out-of-hospital cardiac arrest: A descriptive cohort study. Resuscitation 2024, 195, 110104. [Google Scholar] [CrossRef] [PubMed]
- Duckett, S.A.; Bartman, M.; Roten, R.A. Choking. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2025. Available online: https://www.ncbi.nlm.nih.gov/books/NBK499941/ (accessed on 15 April 2025).
- Bieliński, J.R.; Huntley, R.; Dunne, C.L.; Timler, D.; Nadolny, K.; Jaskiewicz, F. Do We Actually Help Choking Children? The Quality of Evidence on the Effectiveness and Safety of First Aid Rescue Manoeuvres: A Narrative Review. Medicina 2024, 60, 1827. [Google Scholar] [CrossRef] [PubMed]
- Galmarini, E.; Marciano, L.; Schulz, P.J. The effectiveness of visual-based interventions on health literacy in health care: A systematic review and meta-analysis. BMC Health Serv. Res. 2024, 24, 718. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bielski, K.; Böttiger, B.W.; Pruc, M.; Gasecka, A.; Sieminski, M.; Jaguszewski, M.J.; Smereka, J.; Gilis-Malinowska, N.; Peacock, F.W.; Szarpak, L. Outcomes of audio-instructed and video-instructed dispatcher-assisted cardiopulmonary resuscitation: A systematic review and meta-analysis. Ann. Med. 2022, 54, 464–471. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lee, H.S.; You, K.; Jeon, J.P.; Kim, C.; Kim, S. The effect of video-instructed versus audio-instructed dispatcher-assisted cardiopulmonary resuscitation on patient outcomes following out of hospital cardiac arrest in Seoul. Sci. Rep. 2021, 11, 15555. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Butcher, N.J.; Monsour, A.; Mew, E.J.; Chan, A.-W.; Moher, D.; Mayo-Wilson, E.; Terwee, C.B.; Chee-A-Tow, A.; Baba, A.; Gavin, F.; et al. Guidelines for Reporting Outcomes in Trial Reports: The CONSORT-Outcomes 2022 Extension. JAMA 2022, 328, 2252–2264. [Google Scholar] [CrossRef] [PubMed]
- Ekim, A.; Altun, A. Foreign body aspirations in childhood: A retrospective review. J. Pediatr. Nurs. 2023, 72, e174–e178. [Google Scholar] [CrossRef] [PubMed]
- Woloshin, S.; Yang, Y.; Fischhoff, B. Communicating health information with visual displays. Nat. Med. 2023, 29, 1085–1091. [Google Scholar] [CrossRef] [PubMed]
- Ohk, T.; Cho, J.; Yang, G.; Ahn, M.; Lee, S.; Kim, W.; Lee, T. Effectiveness of a dispatcher-assisted CPR using an animated image: Simulation study. Am. J. Emerg. Med. 2024, 78, 132–139. [Google Scholar] [CrossRef] [PubMed]
- Luczak, A. Effect of body position on relieve of foreign body from the airway. AIMS Public Health 2019, 6, 154–159. [Google Scholar] [CrossRef] [PubMed]
- Resuscitation Council UK. Paediatric Basic Life Support Guidelines. Available online: https://www.resus.org.uk/library/2021-resuscitation-guidelines/paediatric-basic-life-support-guidelines (accessed on 12 April 2025).
- Pan, D.F.; Li, Z.J.; Ji, X.Z.; Yang, L.T.; Liang, P.F. Video-assisted bystander cardiopulmonary resuscitation improves the quality of chest compressions during simulated cardiac arrests: A systemic review and meta-analysis. World J. Clin. Cases 2022, 10, 11442–11453. [Google Scholar] [CrossRef]
- Couper, K.; Abu Hassan, A.; Ohri, V.; Patterson, E.; Tang, H.T.; Bingham, R.; Olasveengen, T.; Perkins, G.D. Removal of foreign body airway obstruction: A systematic review of interventions. Resuscitation 2020, 156, 174–181. [Google Scholar] [CrossRef]
- Bohnstedt-Pedersen, N.H.; Linderoth, G.; Helios, B.; Christensen, H.C.; Thomsen, B.K.; Bekker, L.; Gram, J.K.B.; Vaeggemose, U.; Gehrt, T.B. Medical dispatchers’ experience with live video during emergency calls: A national questionnaire study. BMC Health Serv. Res. 2024, 24, 1442. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Matsuyama, T.; Scapigliati, A.; Pellis, T.; Greif, R.; Iwami, T. Willingness to perform bystander cardiopulmonary resuscitation: A scoping review. Resusc. Plus. 2020, 4, 100043. [Google Scholar] [CrossRef]
- Aldridge, E.S.; Perera, N.; Ball, S.; Finn, J.; Bray, J. A scoping review to determine the barriers and facilitators to initiation and performance of bystander cardiopulmonary resuscitation during emergency calls. Resusc. Plus. 2022, 11, 100290. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Norii, T.; Igarashi, Y.; Yoshino, Y.; Nakao, S.; Yang, M.; Albright, D.; Sklar, D.P.; Crandall, C. The effects of bystander interventions for foreign body airway obstruction on survival and neurological outcomes: Findings of the MOCHI registry. Resuscitation 2024, 199, 110198. [Google Scholar] [CrossRef]
- Vincent, A.; Semmer, N.K.; Becker, C.; Beck, K.; Tschan, F.; Bobst, C.; Schuetz, P.; Marsch, S.; Hunziker, S. Does stress influence the performance of cardiopulmonary resuscitation? A narrative review of the literature. J. Crit. Care 2021, 63, 223–230. [Google Scholar] [CrossRef]
- Yu, X.; Miao, L.; Zhu, J.; Liang, J.; Dai, L.; Li, X.; Li, Q.; Rao, R.; Yuan, C.; Wang, Y.; et al. Social and environmental risk factors for unintentional suffocation among infants in China: A descriptive analysis. BMC Pediatr. 2021, 21, 465. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Begović, I.; Štefanović, I.M.; Vrsalović, R.; Geber, G.; Kereković, E.; Lučev, T.; Baudoin, T. Parental awareness of the dangers of foreign body inhalation in children. Acta Clin. Croat. 2022, 61 (Suppl. 4), 26–33. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chen, K.Y.; Ko, Y.C.; Hsieh, M.J.; Chiang, W.C.; Ma, M.H.M. Interventions to improve the quality of bystander cardiopulmonary resuscitation: A systematic review. PLoS ONE 2019, 14, e0211792. [Google Scholar] [CrossRef]
- Park, D.H.; Park, G.J.; Kim, Y.M.; Chai, H.S.; Kim, S.C.; Kim, H.; Lee, S.W. Barriers to successful dispatcher-assisted cardiopulmonary resuscitation in out-of-hospital cardiac arrest in Korea. Resusc. Plus 2024, 19, 100725. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Magnusson, C.; Ollis, L.; Munro, S.; Maben, J.; Coe, A.; Fitzgerald, O.; Taylor, C. Video livestreaming from medical emergency callers’ smartphones to emergency medical dispatch centres: A scoping review of current uses, opportunities, and challenges. BMC Emerg. Med. 2024, 24, 99. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
| Assessment items | Definitions | |
|---|---|---|
| Adequacy of | ① Infant position | Prone for back blow and supine for chest thrust |
| ② Supporting arm posture | Alignment of the supporting arm and infant body axis | |
| ③ Hand posture of the supporting arm | Adequacy of infant chin support | |
| ④ Head tilt | The head is located lower than the body | |
| ⑤ Location of back blows | Upper back above the axillary line | |
| ⑥ Number of back blows | Back blow five times | |
| ⑦ Hand part for back blows | Use the heel of hand | |
| ⑧ Location of chest thrusts | The lower half of the sternum | |
| ⑨ Number of chest thrusts | Chest thrust five times | |
| ⑩ Repeating two maneuvers | Repeat the back blow and chest thrust maneuvers | |
| Instruction Performance score | Sum of ①–⑩ | |
| Time to first back blow | Time from dispatcher instruction to the first back blow | |
| Time to finish the first cycle (five back blows and five chest thrusts) | Time from dispatcher instruction to the fifth chest thrust | |
| Time from the second to the third cycle | Time from the first back blow of the second cycle to when the participant finished the fifth chest thrust of the third cycle | |
| Time to finish the third cycle | Time from dispatcher instruction to the fifth chest thrust of the third cycle | |
| Auditory Group (n = 40) | Audiovisual Group (n = 39) | Total (n = 79) | p-Value | ||
|---|---|---|---|---|---|
| Sex | Male | 19 (47.5%) | 13 (32.5%) | 32 (40.5%) | 0.171 |
| Female | 21 (52.5%) | 26 (66.7%) | 47 (59.5%) | ||
| Age | 30.43 ± 3.11 | 30.50 ± 2.47 | 30.46 ± 2.79 | 0.787 | |
| Prior training | No | 25 (62.5%) | 19 (48.7%) | 44 (55.7%) | 0.178 |
| Yes | 15 (37.5%) | 21 (53.8%) | 36 (45.6%) | ||
| Prior training timing (year) | 4.88 ± 2.30 | 5.67 ± 2.46 | 5.32 ± 2.39 | 0.310 | |
| Assessment Items | Auditory (n = 40) | Audiovisual (n = 39) | p-Value | |
|---|---|---|---|---|
| Adequacy of | ① Infant position | 31 (77.5%) | 39 (100.0%) | 0.002 |
| ② Supporting arm posture | 12 (30.0%) | 27 (69.2%) | <0.001 | |
| ③ Hand posture of the supporting arm | 10 (25.0%) | 15 (38.5%) | 0.233 | |
| ④ Head tilt | 12 (30.0%) | 39 (100.0%) | <0.001 | |
| ⑤ Location of back blows | 22 (55.0%) | 31 (79.5%) | 0.138 | |
| ⑥ Number of back blows | 29 (72.5%) | 34 (87.2%) | 0.105 | |
| ⑦ Hand part for back blows | 19 (47.5%) | 31 (79.5%) | 0.009 | |
| ⑧ Location of chest thrusts | 32 (80.0%) | 30 (76.9%) | 0.136 | |
| ⑨ Number of chest thrusts | 40 (100.0%) | 34 (87.2%) | 0.026 | |
| ⑩ Repeating two maneuvers | 36 (90.0%) | 38 (97.4%) | 0.175 | |
| Instruction Performance score | 6.13 ± 2.27 | 8.15 ± 1.31 | <0.001 | |
| Time to first back blow | 52.88 ± 12.56 | 53.05 ± 10.95 | 0.498 | |
| Time to finish the first cycle | 77.38 ± 14.03 | 112.58 ± 144.38 | 0.118 | |
| Time from the second to the third cycle * | 19.31 ± 4.40 | 22.29 ± 4.64 | 0.332 | |
| Time to finish the third cycle * | 112.53 ± 17.99 | 128.76 ± 17.64 | 0.332 | |
| Prior Training Group | No Prior Training Group | ||||||
|---|---|---|---|---|---|---|---|
| Auditory (n = 15) | Audiovisual (n = 20) | p-Value | Auditory (n = 25) | Audiovisual (n = 19) | p-Value | ||
| Adequacy of | ① Infant position | 13 (86.7%) | 20 (100.0%) | 0.093 | 18 (72.0%) | 19 (100.0%) | 0.012 |
| ② Supporting arm posture | 8 (53.3%) | 12 (60.0%) | 0.693 | 4 (16.0%) | 15 (78.9%) | <0.001 | |
| ③ Hand posture of the supporting arm | 6 (40.0%) | 7 (35.0%) | 0.668 | 4 (16.0%) | 8 (42.1%) | 0.054 | |
| ④ Head tilt | 5 (33.3%) | 20 (100.0%) | <0.001 | 7 (28.0%) | 19 (100.0%) | <0.001 | |
| ⑤ Location of back blows | 11 (73.3%) | 16 (80.0%) | 0.621 | 11 (44.0%) | 15 (78.9%) | 0.079 | |
| ⑥ Number of back blows | 9 (60.0%) | 18 (90.0%) | 0.036 | 20 (80.0%) | 16 (84.2%) | 0.720 | |
| ⑦ Hand part for back blows | 10 (66.7%) | 18 (90.0%) | 0.088 | 9 (36.0%) | 13 (68.4%) | 0.059 | |
| ⑧ Location of chest thrusts | 14 (93.3%) | 17 (85.0%) | 0.129 | 18 (72.0%) | 13 (68.4%) | 0.298 | |
| ⑨ Number of chest thrusts | 15 (100.0%) | 18 (90.0%) | 0.207 | 25 (100.0%) | 16 (84.2%) | 0.040 | |
| ⑩ Repeating two maneuvers | 13 (86.7%) | 19 (95.0%) | 0.383 | 23 (92.0%) | 19 (100.0%) | 0.207 | |
| Instruction Performance score | 6.93 ± 2.15 | 8.25 ± 1.33 | 0.263 | 5.63 ± 2.24 | 8.05 ± 1.31 | 0.014 | |
| Time to the first back blow | 50.13 ± 9.50 | 52.85 ± 12.10 | 0.559 | 54.52 ± 14.01 | 53.26 ± 9.95 | 0.256 | |
| Time to finish the first cycle | 74.73 ± 11.48 | 132.29 ± 199.14 | 0.128 | 78.96 ± 15.36 | 9.079 ± 12.32 | 0.670 | |
| Time from the second to the third cycle * | 19.38 ± 3.89 | 22.53 ± 4.95 | 0.490 | 19.26 ± 4.75 | 22.05 ± 4.43 | 0.492 | |
| Time to finish the third cycle * | 111.00 ± 17.45 | 128.58 ± 20.86 | 0.285 | 113.96 ± 18.52 | 128.95 ± 14.30 | 0.755 | |
| Male | Female | ||||||
|---|---|---|---|---|---|---|---|
| Auditory (n = 19) | Audiovisual (n = 13) | p-Value | Auditory (n = 21) | Audiovisual (n = 26) | p-Value | ||
| Adequacy of | ① Infant position | 15 (78.9%) | 13 (100.0%) | 0.081 | 16 (76.2%) | 26 (100.0%) | 0.008 |
| ② Supporting arm posture | 8 (42.1%) | 7 (53.8%) | 0.529 | 4 (19.0%) | 20 (76.9%) | <0.001 | |
| ③ Hand posture of the supporting arm | 6 (31.6%) | 6 (46.2%) | 0.419 | 4 (19.0%) | 9 (34.6%) | 0.294 | |
| ④ Head tilt | 10 (52.6%) | 13 (100.0%) | 0.002 | 2 (9.5%) | 26 (100.0%) | 0.001 | |
| ⑤ Location of back blows | 11 (61.1%) | 11 (84.6%) | 0.165 | 11 (61.1%) | 20 (74.1%) | 0.374 | |
| ⑥ Number of back blows | 14 (73.7%) | 12 (92.3%) | 0.005 | 15 (71.4%) | 22 (84.6%) | 0.282 | |
| ⑦ Hand part for back blows | 11 (61.1%) | 11 (84.6%) | 0.165 | 8 (40.0%) | 20 (76.9%) | 0.029 | |
| ⑧ Location of chest thrusts | 15 (93.8%) | 11 (91.7%) | 0.840 | 17 (89.5%) | 19 (73.1%) | 0.264 | |
| ⑨ Number of chest thrusts | 19 (100.0%) | 11 (84.6%) | 0.082 | 21 (100.0%) | 23 (88.5%) | 0.112 | |
| ⑩ Repeating two maneuvers | 17 (89.5%) | 12 (92.3%) | 0.840 | 19 (90.5%) | 26 (100.0%) | 0.112 | |
| Instruction Performance score | 6.63 ± 2.36 | 8.23 ± 1.48 | 0.039 | 5.65 ± 2.13 | 8.12 ± 1.24 | 0.009 | |
| Time to the first back blow | 53.68 ± 15.11 | 53.31 ± 9.54 | 0.294 | 52.14 ± 10.06 | 52.92 ± 11.77 | 0.830 | |
| Time to finish the first cycle | 78.79 ± 17.10 | 93.38 ± 10.68 | 0.304 | 76.10 ± 10.82 | 121.81 ± 17.91 | 0.124 | |
| Time from the second to the third cycle * | 19.58 ± 3.63 | 24.00 ± 4.64 | 0.163 | 18.05 ± 5.36 | 21.35 ± 4.39 | 0.926 | |
| Time to finish the third cycle * | 115.24 ± 21.60 | 134.75 ± 15.91 | 0.311 | 110.11 ± 14.19 | 126.00 ± 18.0 | 0.301 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ohk, T.; Cho, J.; Cho, H.; Yang, G.; You, K.; Lee, T. Evaluation of the Effectiveness of Animated Images in First Aid for Infants with Foreign Body Airway Obstruction: A Simulation Study. J. Clin. Med. 2025, 14, 2839. https://doi.org/10.3390/jcm14082839
Ohk T, Cho J, Cho H, Yang G, You K, Lee T. Evaluation of the Effectiveness of Animated Images in First Aid for Infants with Foreign Body Airway Obstruction: A Simulation Study. Journal of Clinical Medicine. 2025; 14(8):2839. https://doi.org/10.3390/jcm14082839
Chicago/Turabian StyleOhk, Taekgeun, Junhwi Cho, Hyunseok Cho, Goeun Yang, Kicheol You, and Taehun Lee. 2025. "Evaluation of the Effectiveness of Animated Images in First Aid for Infants with Foreign Body Airway Obstruction: A Simulation Study" Journal of Clinical Medicine 14, no. 8: 2839. https://doi.org/10.3390/jcm14082839
APA StyleOhk, T., Cho, J., Cho, H., Yang, G., You, K., & Lee, T. (2025). Evaluation of the Effectiveness of Animated Images in First Aid for Infants with Foreign Body Airway Obstruction: A Simulation Study. Journal of Clinical Medicine, 14(8), 2839. https://doi.org/10.3390/jcm14082839







