An Evaluation of Reference Bite Force Values: Investigating the Relationship Between Dental Prosthetic Restoration and Bite Force in a Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population and Sampling Strategy
2.2. Efforts to Address Potential Sources of Bias
2.3. Measurements
2.4. Fully Dentate
- PTG 1 Fully dentate, no missing teeth, only natural dentition
- PTG 2 Fully dentate, crown or fixed partial denture
2.5. Partially Dentate
- PTG 3 Partially dentate, no denture
- PTG 4 Partially dentate, removable denture
- PTG 5 Partially dentate in one jaw, and edentulous with a complete denture in the other jaw
2.6. Edentulous
- PTG 6 Edentulous, complete dentures in both jaws, supported by two interforaminal implants in the lower jaw
- PTG 7 Edentulous, complete dentures in both jaws
2.7. Statistical Considerations
2.8. Ethical Consideration
3. Results
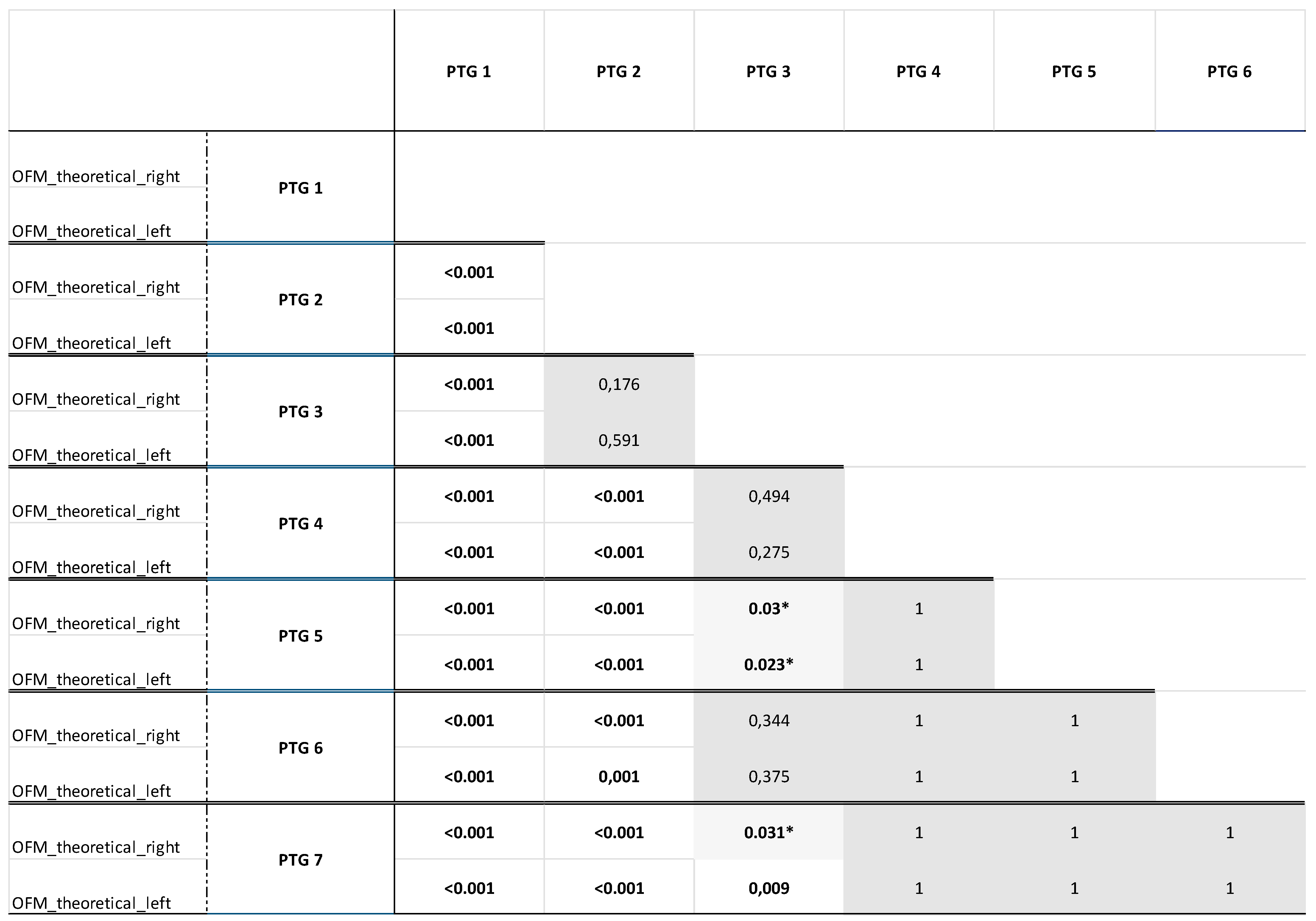
- Full dentition (PTG 1) was considered to be the gold standard regarding the evaluated bite forces, as it was shown that the bite forces of the fully dentate participants were higher than those of all other PTGs, from which they also differed significantly (p < 0.001).
- The fully dentate participants with crown(s) or fixed partial denture(s) (PTG 2) did not differ in terms of the measured bite forces from those with partial dentition without dentures (PTG 3) (Figure 4, grey highlighting).
- Similarly, there was no difference in the bite forces between the partially dentate participants without dentures (PTG 3) and the partially dentate participants with removable dentures (PTG 4) (Figure 4, grey highlighting) or the edentulous participants with complete dentures in both jaws supported by two interforaminal implants in the lower jaw (PTG 6) (Figure 4, grey highlighting). Based on the theoretical OFM measurements, no significant differences were observed between the PTGs “partially dentate in one jaw, edentulous with the complete denture in one jaw” (PTG 5) and “edentulous, complete dentures in both jaws” (PTG 7) (Figure 4, grey highlighting). This suggests that similar bite forces can be achieved with partial dentition, whether it is restored or not, as with partial dentition using removable dentures or further reduced dentition requiring greater prosthetic restoration.
- The same applies to all other prosthetic PTGs: there were no differences in the bite forces between the partially dentate participants with removable dentures (PTG 4), the participants partially dentate in one jaw and edentulous with complete dentures in the other jaw (PTG 5), the edentulous participants with complete dentures in both jaws (PTG 7), and the edentulous participants with complete dentures in both jaws, supported by two interforaminal implants in the lower jaw (PTG 6).
4. Discussion
4.1. Comparison of the Results
4.2. Study Limitations
4.3. Important Results of This Study
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| OFM | Occlusal Force Meter |
| PTG | Prosthetic treatment group |
References
- O’Keeffe, M.; Kelly, M.; O’Herlihy, E.; O’Toole, P.W.; Kearney, P.M.; Timmons, S.; O’Shea, E.; Stanton, C.; Hickson, M.; Rolland, Y.; et al. Potentially Modifiable Determinants of Malnutrition in Older Adults: A Systematic Review. Clin. Nutr. 2019, 38, 2477–2498. [Google Scholar] [CrossRef] [PubMed]
- Kawakami, Y.; Hamano, J. Changes in Body Mass Index, Energy Intake, and Fluid Intake over 60 Months Premortem as Prognostic Factors in Frail Elderly: A Post-Death Longitudinal Study. Int. J. Environ. Res. Public Health 2020, 17, 1823. [Google Scholar] [CrossRef] [PubMed]
- Weijenberg, R.A.F.; Lobbezoo, F.; Knol, D.L.; Tomassen, J.; Scherder, E.J.A. Increased Masticatory Activity and Quality of Life in Elderly Persons with Dementia--a Longitudinal Matched Cluster Randomized Single-Blind Multicenter Intervention Study. BMC Neurol. 2013, 13, 26. [Google Scholar] [CrossRef] [PubMed]
- Fujimoto, K.; Suito, H.; Nagao, K.; Ichikawa, T. Does Masticatory Ability Contribute to Nutritional Status in Older Individuals? Int. J. Environ. Res. Public Health 2020, 17, 7373. [Google Scholar] [CrossRef]
- Tan, H.; Peres, K.G.; Peres, M.A. Retention of Teeth and Oral Health-Related Quality of Life. J. Dent. Res. 2016, 95, 1350–1357. [Google Scholar] [CrossRef]
- Ritchie, C.S.; Joshipura, K.; Hung, H.-C.; Douglass, C.W. Nutrition as a Mediator in the Relation between Oral and Systemic Disease: Associations between Specific Measures of Adult Oral Health and Nutrition Outcomes. Crit. Rev. Oral Biol. Med. 2002, 13, 291–300. [Google Scholar] [CrossRef]
- Azzolino, D.; Passarelli, P.C.; De Angelis, P.; Piccirillo, G.B.; D’Addona, A.; Cesari, M. Poor Oral Health as a Determinant of Malnutrition and Sarcopenia. Nutrients 2019, 11, 2898. [Google Scholar] [CrossRef]
- Limpuangthip, N.; Komin, O. Association between Oral Hypofunction and General Health: A Systematic Review. BMC Oral Health 2023, 23, 591. [Google Scholar] [CrossRef]
- Kazemi, S.; Savabi, G.; Khazaei, S.; Savabi, O.; Esmaillzadeh, A.; Keshteli, A.H.; Adibi, P. Association between Food Intake and Oral Health in Elderly: SEPAHAN Systematic Review No. 8. Dent. Res. J. 2011, 8, S15–S20. [Google Scholar]
- Kim, H.-E.; Wallace, J.; Sohn, W. Factors Affecting Masticatory Performance of Older Adults Are Sex-Dependent: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 15742. [Google Scholar] [CrossRef]
- Fan, Y.; Shu, X.; Leung, K.C.M.; Lo, E.C.M. Association between Masticatory Performance and Oral Conditions in Adults: A Systematic Review and Meta-Analysis. J. Dent. 2023, 129, 104395. [Google Scholar] [CrossRef] [PubMed]
- Ikebe, K.; Matsuda, K.; Morii, K.; Furuya-Yoshinaka, M.; Nokubi, T.; Renner, R.P. Association of Masticatory Performance with Age, Posterior Occlusal Contacts, Occlusal Force, and Salivary Flow in Older Adults. Int. J. Prosthodont. 2006, 19, 475–481. [Google Scholar] [PubMed]
- Miyaura, K.; Matsuka, Y.; Morita, M.; Yamashita, A.; Watanabe, T. Comparison of Biting Forces in Different Age and Sex Groups: A Study of Biting Efficiency with Mobile and Non-mobile Teeth. J. Oral Rehabil. 1999, 26, 223–227. [Google Scholar] [CrossRef] [PubMed]
- Hatch, J.P.; Shinkai, R.S.A.; Sakai, S.; Rugh, J.D.; Paunovich, E.D. Determinants of Masticatory Performance in Dentate Adults. Arch. Oral Biol. 2001, 46, 641–648. [Google Scholar] [CrossRef]
- Ikebe, K.; Matsuda, K.; Kagawa, R.; Enoki, K.; Yoshida, M.; Maeda, Y.; Nokubi, T. Association of Masticatory Performance with Age, Gender, Number of Teeth, Occlusal Force and Salivary Flow in Japanese Older Adults: Is Ageing a Risk Factor for Masticatory Dysfunction? Arch. Oral Biol. 2011, 56, 991–996. [Google Scholar] [CrossRef]
- Sun, K.-T.; Chen, S.-C.; Li, Y.-F.; Chiang, H.-H.; Tsai, H.-H.; Li, C.-Y.; Tu, M.-G. Bite-Force Difference among Obese Adolescents in Central Taiwan. J. Formos. Med. Assoc. 2016, 115, 404–410. [Google Scholar] [CrossRef]
- Tsuga, K.; Carlsson, G.E.; Osterberg, T.; Karlsson, S. Self-Assessed Masticatory Ability in Relation to Maximal Bite Force and Dental State in 80-Year-Old Subjects. J. Oral Rehabil. 1998, 25, 117–124. [Google Scholar] [CrossRef]
- Kamegai, T.; Tatsuki, T.; Nagano, H.; Mitsuhashi, H.; Kumeta, J.; Tatsuki, Y.; Kamegai, T.; Inaba, D. A Determination of Bite Force in Northern Japanese Children. Eur. J. Orthod. 2005, 27, 53–57. [Google Scholar] [CrossRef]
- Bakke, M.; Holm, B.; Jensen, B.L.; Michler, L.; Möller, E. Unilateral, Isometric Bite Force in 8-68-Year-Old Women and Men Related to Occlusal Factors. Scand. J. Dent. Res. 1990, 98, 149–158. [Google Scholar] [CrossRef]
- Helkimo, E.; Carlsson, G.E.; Helkimo, M. Bite Force and State of Dentition. Acta Odontol. Scand. 1977, 35, 297–303. [Google Scholar] [CrossRef]
- Van der Bilt, A.; Olthoff, L.W.; Bosman, F.; Oosterhaven, S.P. Chewing Performance before and after Rehabilitation of Post-Canine Teeth in Man. J. Dent. Res. 1994, 73, 1677–1683. [Google Scholar] [CrossRef] [PubMed]
- Jockusch, J.; Hahnel, S.; Sobotta, B.B.A.J.; Nitschke, I. The Effect of a Masticatory Muscle Training Program on Chewing Efficiency and Bite Force in People with Dementia. Int. J. Environ. Res. Public Health 2022, 19, 3778. [Google Scholar] [CrossRef] [PubMed]
- Kapur, K.K.; Garrett, N.R. Studies of Biologic Parameters for Denture Design. Part II: Comparison of Masseter Muscle Activity, Masticatory Performance, and Salivary Secretion Rates between Denture and Natural Dentition Groups. J. Prosthet. Dent. 1984, 52, 408–413. [Google Scholar] [CrossRef] [PubMed]
- Michael, C.G.; Javid, N.S.; Colaizzi, F.A.; Gibbs, C.H. Biting Strength and Chewing Forces in Complete Denture Wearers. J. Prosthet. Dent. 1990, 63, 549–553. [Google Scholar] [CrossRef]
- Blamphin, C.N.; Brafield, T.R.; Jobbins, B.; Fisher, J.; Watson, C.J.; Redfern, E.J. A Simple Instrument for the Measurement of Maximum Occlusal Force in Human Dentition. Proc. Inst. Mech. Eng. Part H 1990, 204, 129–131. [Google Scholar] [CrossRef]
- Petersen, P.E.; Baez, R.J.; World Health Organization. Oral Health Surveys: Basic Methods, 5th ed.; World Health Organization: Geneva, Switzerland, 2013; ISBN 978-92-4-154864-9. [Google Scholar]
- Eichner, K. Über Eine Gruppeneinteilung Der Lückengebisse Für Die Prothetik. Dtsch. Zahnarztl. Z. 1955, 10, 1831–1834. [Google Scholar]
- Marxkors, R. Kriterien für die zahnärztliche Prothetik. Partielle Prothese. Ges. Für Strahlen-Und Umweltforsch. Und Technol. 1988, 25–26. [Google Scholar]
- Hirao, A.; Murata, S.; Kubo, A.; Hachiya, M.; Mitsumaru, N.; Asami, T. Association between Occlusal Force and Physical Functions in Preschool Children: A Comparison of Males and Females. J. Phys. Ther. Sci. 2015, 27, 3729–3732. [Google Scholar] [CrossRef]
- Al-Zarea, B.K. Maximum Bite Force Following Unilateral Fixed Prosthetic Treatment: A Within-Subject Comparison to the Dentate Side. Med. Princ. Pract. 2015, 24, 142–146. [Google Scholar] [CrossRef]
- Abu Alhaija, E.S.J.; Al Zo’ubi, I.A.; Al Rousan, M.E.; Hammad, M.M. Maximum Occlusal Bite Forces in Jordanian Individuals with Different Dentofacial Vertical Skeletal Patterns. Eur. J. Orthod. 2010, 32, 71–77. [Google Scholar] [CrossRef]
- Varga, S.; Spalj, S.; Lapter Varga, M.; Anic Milosevic, S.; Mestrovic, S.; Slaj, M. Maximum Voluntary Molar Bite Force in Subjects with Normal Occlusion. Eur. J. Orthod. 2011, 33, 427–433. [Google Scholar] [CrossRef] [PubMed]
- Nitschke, I.; Moede, C.; Hopfenmüller, W.; Sobotta, B.A.J.; Koenig, A.; Jockusch, J. Validation of a New Measuring Instrument for the Assessment of Bite Force. Diagnostics 2023, 13, 3498. [Google Scholar] [CrossRef] [PubMed]
- Nitschke, I.; Stark, H. Fünfte Deutsche Mundgesundheitsstudie (DMS V). Krankheits- Und Versorgungsprävalenzen Bei Jüngeren Erwachsenen (35-Bis 44-Jährige): Zahnverlust Und Prothetische Versorgung. Prothetische Leitversorgung. In Fünfte Deutsche Mundgesundheitsstudie (DMS V); Deutscher Zahnärzte Verlag: Köln, Germany, 2016; p. 350ff. ISBN 978-3-7691-0020-4. [Google Scholar]
- Schiffner, U.; Hoffmann, T.; Kerschbaum, T. Aufbau Der Zahnmedizinischen Erhebungsinstrumente. Prothetische Befunde. In Vierte Deutsche Mundgesundheitsstudie (DMS IV); Deutscher Zahnärzte Verlag: Köln, Germany, 2006; Volume 31, p. 105ff. [Google Scholar]
- IBM Corp. IBM SPSS Statistics for Windows, Version 29.0; IBM Corp.: Armonk, NY, USA, 2022. [Google Scholar]
- Schimmel, M. Ein praxisgerechter Kaufunktionstest. Z. Für Senioren-Zahnmed. 2014, 143–146. [Google Scholar]
- Braun, S.; Bantleon, H.P.; Hnat, W.P.; Freudenthaler, J.W.; Marcotte, M.R.; Johnson, B.E. A Study of Bite Force, Part 1: Relationship to Various Physical Characteristics. Angle Orthod. 1995, 65, 367–372. [Google Scholar] [CrossRef]
- Patil, S.R.; Maragathavalli, G.; Ramesh, D.N.S.V.; Naidu, G.S.; Alam, M.K.; AlZoubi, I.A. The Reliability of a New Device for Measuring the Maximum Bite Force. Biomed. Res. Int. 2022, 2022, 3272958. [Google Scholar] [CrossRef]
- Sano, M.; Shiga, H. Gender Differences in Masticatory Function in Elderly Adults with Natural Dentition. Odontology 2021, 109, 973–978. [Google Scholar] [CrossRef]
- Johnston, T.D. Theoretical Considerations in the Adaptation of Animal Communication Systems. J. Theor. Biol. 1976, 57, 43–72. [Google Scholar] [CrossRef]
- Osterberg, T.; Tsuga, K.; Rothenberg, E.; Carlsson, G.E.; Steen, B. Masticatory Ability in 80-Year-Old Subjects and Its Relation to Intake of Energy, Nutrients and Food Items. Gerodontology 2002, 19, 95–101. [Google Scholar] [CrossRef]
- Gibbs, C.H.; Anusavice, K.J.; Young, H.M.; Jones, J.S.; Esquivel-Upshaw, J.F. Maximum Clenching Force of Patients with Moderate Loss of Posterior Tooth Support: A Pilot Study. J. Prosthet. Dent. 2002, 88, 498–502. [Google Scholar] [CrossRef]
- Ikebe, K.; Nokubi, T.; Morii, K.; Kashiwagi, J.; Furuya, M. Association of Bite Force with Ageing and Occlusal Support in Older Adults. J. Dent. 2005, 33, 131–137. [Google Scholar] [CrossRef]
- Miyaura, K.; Morita, M.; Matsuka, Y.; Yamashita, A.; Watanabe, T. Rehabilitation of Biting Abilities in Patients with Different Types of Dental Prostheses. J. Oral Rehabil. 2000, 27, 1073–1076. [Google Scholar] [CrossRef] [PubMed]
- Schimmel, M.; Memedi, K.; Parga, T.; Katsoulis, J.; Müller, F. Masticatory Performance and Maximum Bite and Lip Force Depend on the Type of Prosthesis. Int. J. Prosthodont. 2017, 30, 565–572. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.H.J.; Vu, H.; Kim, H.-D. Gender and Age Group Modified Association of Dental Health Indicators with Total Occlusal Force among Korean Elders. BMC Oral Health 2021, 21, 571. [Google Scholar] [CrossRef] [PubMed]
- Fayad, M.I.; Alruwaili, H.H.T.; Khan, M.S.; Baig, M.N. Bite Force Evaluation in Complete Denture Wearer with Different Denture Base Materials: A Randomized Controlled Clinical Trial. J. Int. Soc. Prev. Community Dent. 2018, 8, 416–419. [Google Scholar] [CrossRef]
- Alqutaibi, A.Y.; Alnazzawi, A.A.; Farghal, A.E.; Bakr, R.M.; Mahmoud, I.I. Impact of Acrylic and Silicone-Based Soft-Liner Materials on Biting Force and Quality of Life of the Complete Denture Wearers: A Randomized Clinical Trial. J. Clin. Med. 2023, 12, 2073. [Google Scholar] [CrossRef]
- Sônego, M.V.; Neto, C.L.M.M.; Dos Santos, D.M.; Moreno, A.L.d.M.; Bertoz, A.P.d.M.; Goiato, M.C. Quality of Life, Satisfaction, Occlusal Force, and Halitosis after Direct and Indirect Relining of Inferior Complete Dentures. Eur. J. Dent. 2022, 16, 215–222. [Google Scholar] [CrossRef]
- Kurogi, T.; Murata, H.; Yamaguchi, E.; Kawai, Y.; Suzuki, A.; Koide, Y.; Kimoto, S.; Kondo, H.; Nomura, T.; Tsuboi, A.; et al. Effects of Denture Adhesives on Denture Retention and Occlusal Forces in Complete Denture Wearers: A Multicenter, Randomized Controlled Trial. J. Prosthodont. Res. 2023, 67, 548–555. [Google Scholar] [CrossRef]
- Tripathi, G.; Ponnanna, A.A.; Rajwadha, N.; Chhaparia, N.; Sharma, A.; Anant, M. Comparative Evaluation of Maximum Bite Force in Dentulous and Edentulous Individuals with Different Facial Forms. J. Clin. Diagn. Res. 2014, 8, ZC37–ZC40. [Google Scholar] [CrossRef]
- Rismanchian, M.; Bajoghli, F.; Mostajeran, Z.; Fazel, A.; Eshkevari, P. sadr Effect of Implants on Maximum Bite Force in Edentulous Patients. J. Oral Implantol. 2009, 35, 196–200. [Google Scholar] [CrossRef]
- Soni, R.; Yadav, H.; Pathak, A.; Bhatnagar, A.; Kumar, V. Comparative Evaluation of Biting Force and Chewing Efficiency of All-on-Four Treatment Concept with Other Treatment Modalities in Completely Edentulous Individuals. J. Ind. Prosthodont. Soc. 2020, 20, 312–320. [Google Scholar] [CrossRef]
- Sharma, A.J.; Nagrath, R.; Lahori, M. A Comparative Evaluation of Chewing Efficiency, Masticatory Bite Force, and Patient Satisfaction between Conventional Denture and Implant-Supported Mandibular Overdenture: An in Vivo Study. J. Ind. Prosthodont. Soc. 2017, 17, 361–372. [Google Scholar] [CrossRef] [PubMed]
- Possebon, A.P.d.R.; Schuster, A.J.; Bielemann, A.M.; Porto, B.L.; Boscato, N.; Faot, F. Evaluation of Bite Force and Masticatory Performance: Complete Denture vs Mandibular Overdenture Users. Braz. Dent. J. 2020, 31, 399–403. [Google Scholar] [CrossRef] [PubMed]
- Jockusch, J.; Hopfenmüller, W.; Nitschke, I. Chewing Function and Related Parameters as a Function of the Degree of Dementia: Is There a Link between the Brain and the Mouth? J. Oral Rehabil. 2021, 48, 1160–1172. [Google Scholar] [CrossRef] [PubMed]
- Fan, Y.; Shu, X.; Leung, K.C.M.; Lo, E.C.M. Associations of General Health Conditions with Masticatory Performance and Maximum Bite Force in Older Adults: A Systematic Review of Cross-Sectional Studies. J. Dent. 2022, 123, 104186. [Google Scholar] [CrossRef]
- Dibello, V.; Zupo, R.; Sardone, R.; Lozupone, M.; Castellana, F.; Dibello, A.; Daniele, A.; De Pergola, G.; Bortone, I.; Lampignano, L.; et al. Oral Frailty and Its Determinants in Older Age: A Systematic Review. Lancet Healthy Longev. 2021, 2, e507–e520. [Google Scholar] [CrossRef]
- Palinkas, M.; Nassar, M.S.P.; Cecílio, F.A.; Siéssere, S.; Semprini, M.; Machado-de-Sousa, J.P.; Hallak, J.E.C.; Regalo, S.C.H. Age and Gender Influence on Maximal Bite Force and Masticatory Muscles Thickness. Arch. Oral Biol. 2010, 55, 797–802. [Google Scholar] [CrossRef]
- Wolters, F.J.; Chibnik, L.B.; Waziry, R.; Anderson, R.; Berr, C.; Beiser, A.; Bis, J.C.; Blacker, D.; Bos, D.; Brayne, C.; et al. Twenty-Seven-Year Time Trends in Dementia Incidence in Europe and the United States: The Alzheimer Cohorts Consortium. Neurology 2020, 95, e519–e531. [Google Scholar] [CrossRef]
- Haraldson, T. Comparisons of Chewing Patterns in Patients with Bridges Supported on Osseointegrated Implants and Subjects with Natural Dentitions. Acta Odontol. Scand. 1983, 41, 203–208. [Google Scholar] [CrossRef]
- Lobbezoo, F.; Trulsson, M.; Jacobs, R.; Svensson, P.; Cadden, S.W.; van Steenberghe, D. Topical Review: Modulation of Trigeminal Sensory Input in Humans: Mechanisms and Clinical Implications. J. Orofac. Pain. 2002, 16, 9–21. [Google Scholar]
- Ranjan, M.; Singh, B.; Chatterjee, U.; Tushar; Sinha, D.K.; Verma, A. A Novel Indigenously Developed Device to Measure Bite Force. J. Pharm. Bioallied Sci. 2023, 15, S550–S553. [Google Scholar] [CrossRef]
- Martinez-Gomis, J.; Lujan-Climent, M.; Palau, S.; Bizar, J.; Salsench, J.; Peraire, M. Relationship between Chewing Side Preference and Handedness and Lateral Asymmetry of Peripheral Factors. Arch. Oral Biol. 2009, 54, 101–107. [Google Scholar] [CrossRef] [PubMed]
- Kawashima, M.; Yoshimi, K.; Nakagawa, K.; Yamaguchi, K.; Ishii, M.; Hasegawa, S.; Moritoyo, R.; Nakane, A.; Tohara, H. Usefulness and Validity of a Jaw-Closing Force Meter in Older Adults. Geriatrics 2022, 7, 145. [Google Scholar] [CrossRef] [PubMed]
- Ferrario, V.F.; Sforza, C.; Serrao, G.; Dellavia, C.; Tartaglia, G.M. Single Tooth Bite Forces in Healthy Young Adults. J. Oral Rehabil. 2004, 31, 18–22. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Ye, D. Measurement of biting force of normal teeth at different ages. Hua Xi Yi Ke Da Xue Xue Bao 1994, 25, 414–417. [Google Scholar]



| All Participants | PTG 1 | PTG 2 | PTG 3 | PTG 4 | PTG 5 | PTG 6 | PTG 7 | |
|---|---|---|---|---|---|---|---|---|
 |  |  |  |  |  |  | ||
| Fully dentate, no missing teeth, only natural dentition | Fully dentate, crown or fixed partial denture | Partially dentate, no denture | Partially dentate, removable denture | Partially dentate in one jaw, and edentulous with a complete denture in the other jaw | Edentulous, complete dentures in both jaws, supported by two interforaminal implants in the lower jaw | Edentulous, complete dentures in both jaws | ||
| (n = 198) | (n = 21) | (n = 40) | (n = 37) | (n = 46) | (n = 25) | (n = 12) | (n = 17) | |
| Sex (n%) | ||||||||
| Male | 98/49.5 | 9/42.9 | 17/42.5 | 25/67.6 | 21/45.7 | 12/48.0 | 4/33.3 | 10/58.8 |
| Female | 100/50.5 | 12/57.1 | 23/57.5 | 12/32.4 | 25/54.3 | 13/52.0 | 8/66.7 | 7/41.2 |
| Age (Years) | ||||||||
| Median (Range) | 72.0 (20–95) | 22 (20–33) | 69.5 (24–89) | 71 (33–93) | 75 (46–90) | 77 (34–94) | 81.5 (69–95) | 79 (47–94) |
| Mean ± SD | 66.1 ± 20.6 | 23.2 ± 3.7 | 64.5 ± 20.1 | 70.2 ± 14.2 | 72.7 ± 10.5 | 73.5 ±15.1 | 81.0 ± 8.5 | 74.1 ± 12.8 |
| All Participants | PTG 1 | PTG 2 | PTG 3 | PTG 4 | PTG 5 | PTG 6 | PTG 7 | |
|---|---|---|---|---|---|---|---|---|
 |  |  |  |  |  |  | ||
| Fully dentate, no missing teeth, only natural dentition | Fully dentate, crown or fixed partial denture | Partially dentate, no denture | Partially dentate, removable denture | Partially dentate in one jaw, and edentulous with a complete denture in the other jaw | Edentulous, complete dentures in both jaws, supported by two interforaminal implants in the lower jaw | Edentulous, complete dentures in both jaws | ||
| DMFT index | ||||||||
| DT | ||||||||
| Median (Range) | 0 (0–19) | 0 (0–1) | 0 (0–19) | 1 (0–15) | 0 (0–12) | 0 (0–6) | 0 (0–0) | 0 (0–0) |
| Mean ± SD | 1.2 ± 2.7 | 0.1 ± 0.3 | 1.0 ± 3.2 | 2.6 ± 3.6 | 1.7 ± 2.8 | 0.7 ± 1.6 | 0 ± 0 | 0 ± 0 |
| MT | ||||||||
| Median (Range) | 13 (0–32) | 2 (0–6) | 5 (0–17) | 8 (1–31) | 15.5 (2–27) | 28 (18–31) | 32 (30–32) | 32 (32–32) |
| Mean ± SD | 14.9 ± 10.7 | 2.1 ± 2.0 | 6.1 ± 3.3 | 9.5 ± 6.1 | 15.8 ± 4.7 | 26.6 ± 3.8 | 32.0 ± 0 | 31.9 ± 0.5 |
| FT | ||||||||
| Median (Range) | 8 (0–26) | 1 (0–5) | 13.5 (3–23) | 16 (0–26) | 11 (0–22) | 1 (0–13) | 0 (0–0) | 0 (0–0) |
| Mean ± SD | 8.4 ± 7.2 | 1.3 ± 1.5 | 13.0 ± 5.2 | 14.0 ± 6.8 | 10.9 ± 5.0 | 3.4 ± 3.6 | 0 ± 0 | 0 ± 0 |
| DMFT | ||||||||
| Median (Range) | 28 (0–32) | 4 (0–11) | 20.5 (6–30) | 28 (16–32) | 29 (19–32) | 32 (23–32) | 32 (30–32) | 32 (30–32) |
| Mean ± SD | 24.5 ± 9.2 | 3.6 ± 2.7 | 20.2 ± 6.2 | 26.1 ± 5.2 | 28.4 ± 3.5 | 30.6 ± 2.3 | 32.0 ± 0 | 31.9 ± 0.5 |
| Number of support zones | ||||||||
| Median (Range) | 4 (0–4) | |||||||
| Mean ± SD | 3.7 ± 0.8 | |||||||
| (n/%) | ||||||||
| None | 4/2.0 | 3/8.1 | 1/2.2 | |||||
| One | 2/1.0 | 1/2.7 | 1/4.0 | |||||
| Two | 12/6.1 | 7/18.9 | 3/6.5 | 2/8.0 | ||||
| Three | 10/5.1 | 1/2.5 | 7/18.9 | 1/2.2 | 1/4.0 | |||
| Four | 170/85.9 | 21/100 | 39/97.5 | 19/51.4 | 41/89.1 | 21/84.0 | 12/100 | 17/100 |
| Eichner index (n/%) (n = 198) | ||||||||
| A1 | 53/26.6 | 21/100 | ||||||
| A2 | 16/8.0 | 11/29.7 | 1/2.2 | |||||
| A3 | 9/4.5 | 6/16.2 | 1/2.2 | |||||
| B1 | 13/6.5 | 32/80.0 | 9/24.3 | 2/4.3 | 1/4.0 | |||
| B2 | 24/12.1 | 4/10.0 | 7/18.9 | 16/34.8 | ||||
| B3 | 11/5.5 | 2/5.0 | 1/2.7 | 10/21.7 | ||||
| B4 | 9/4.5 | 1/2.5 | 1/2.7 | 8/17.4 | ||||
| C1 | 11/5.5 | 1/2.5 | 8/17.4 | 2/8.0 | 1/8.3 | |||
| C2 | 34/17.1 | 2/5.4 | 22/88.0 | 10/83.3 | ||||
| C3 | 18/9.0 | 17/100 | 1/8.3 | |||||
| Denture quality according to Marxkors (n/%) (n = 100) | ||||||||
| 1 | 47/47.0 | * | * | * | 27/58.7 | 9/36.0 | 5/29.4 | 6/50.0 |
| 2 | 27/27.0 | 11/23.9 | 9/36.0 | 2/11.8 | 5/41.7 | |||
| 3 | 18/18.0 | 6/13.0 | 4/16.0 | 7/41.2 | 1/8.3 | |||
| 4 | 8/8.0 | 2/4.3 | 3/12.0 | 3/17.6 | ||||
| All Participants | PTG 1 | PTG 2 | PTG 3 | PTG 4 | PTG 5 | PTG 6 | PTG 7 | |
|---|---|---|---|---|---|---|---|---|
 |  |  |  |  |  |  | ||
| Fully dentate, no missing teeth, only natural dentition | Fully dentate, crown or fixed partial denture | Partially dentate, no denture | Partially dentate, removable denture | Partially dentate in one jaw, and edentulous with a complete denture in the other jaw | Edentulous, complete dentures in both jaws, supported by two interforaminal implants in the lower jaw | Edentulous, complete dentures in both jaws | ||
| OFM right (in N) | n = 193 | n = 33 * | n = 45 * | |||||
| Median (Range) | 142 (0–1163) | 490 (109–1163) | 257 (19–901) | 158 (17–779) | 104 (14–657) | 59 (0–288) | 75 (32–152) | 38 (0–184) |
| Mean ± SD | 214 ± 218 | 574 ± 260 | 310 ± 187 | 212 ± 180 | 129 ± 121 | 77 ± 74 | 83 ± 38 | 60 ± 56 |
| OFM left (in N) | n = 190 | n = 31 * | n = 45 * | n = 24 * | ||||
| Median (Range) | 124 (0–1093) | 440 (197–1093) | 255 (27–666) | 171 (26–625) | 81 (15–586) | 68 (0–259) | 87 (26–162) | 44 (0–131) |
| Mean ± SD | 197 ± 195 | 520 ± 236 | 277 ± 164 | 203 ± 149 | 121 ± 119 | 77 ± 66 | 89 ± 44 | 50 ± 43 |
| Mean OFM right/left (in N) | n = 194 | |||||||
| Mean ± SD | 204 ± 199 | 547 ± 240 | 294 ± 164 | 203 ± 142 | 125 ± 111 | 75 ± 69 | 86 ± 40 | 55 ± 45 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nitschke, I.; Moede, C.; Koenig, A.; Sobotta, B.A.J.; Hopfenmüller, W.; Jockusch, J. An Evaluation of Reference Bite Force Values: Investigating the Relationship Between Dental Prosthetic Restoration and Bite Force in a Cross-Sectional Study. J. Clin. Med. 2025, 14, 2723. https://doi.org/10.3390/jcm14082723
Nitschke I, Moede C, Koenig A, Sobotta BAJ, Hopfenmüller W, Jockusch J. An Evaluation of Reference Bite Force Values: Investigating the Relationship Between Dental Prosthetic Restoration and Bite Force in a Cross-Sectional Study. Journal of Clinical Medicine. 2025; 14(8):2723. https://doi.org/10.3390/jcm14082723
Chicago/Turabian StyleNitschke, Ina, Celine Moede, Andreas Koenig, Bernhard A. J. Sobotta, Werner Hopfenmüller, and Julia Jockusch. 2025. "An Evaluation of Reference Bite Force Values: Investigating the Relationship Between Dental Prosthetic Restoration and Bite Force in a Cross-Sectional Study" Journal of Clinical Medicine 14, no. 8: 2723. https://doi.org/10.3390/jcm14082723
APA StyleNitschke, I., Moede, C., Koenig, A., Sobotta, B. A. J., Hopfenmüller, W., & Jockusch, J. (2025). An Evaluation of Reference Bite Force Values: Investigating the Relationship Between Dental Prosthetic Restoration and Bite Force in a Cross-Sectional Study. Journal of Clinical Medicine, 14(8), 2723. https://doi.org/10.3390/jcm14082723







