Clinical Characteristics and Management of Patients Admitted to the Supportive Care Clinic and Predisposing Factors of Unplanned Hospital Readmission: Single-Center Experience
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Definition and Purpose of Supportive Care Clinic
2.3. Definition of Unplanned Hospital Readmission
2.4. Data Collection
2.5. Outcomes
2.6. Statistical Analysis
3. Results
3.1. Baseline Characteristics
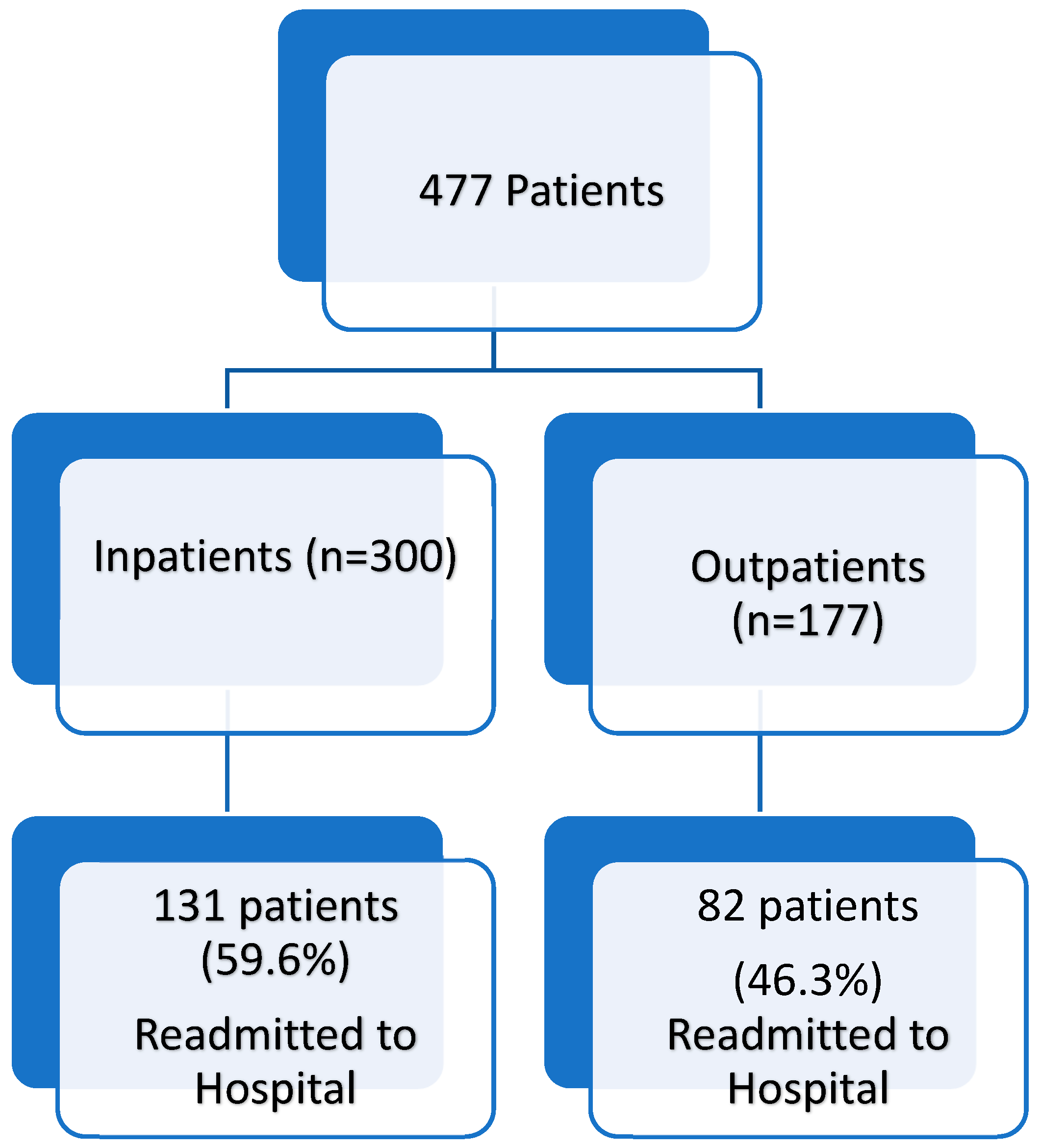
3.2. Unplanned Hospital Readmissions
3.3. Overall Survival
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wu, I.Q.; Lim, F.L.W.I.; Koh, L.P. Outpatient Care. In The Comprehensive Cancer Center: Development, Integration, and Implementation; Aljurf, M., Majhail, N.S., Koh, M.B.C., Kharfan-Dabaja, M.A., Chao, N.J., Eds.; Springer International Publishing: Cham, Swizerland, 2022; pp. 21–33. [Google Scholar] [CrossRef]
- Raiss, M.E.; Mehta, K.K.; Zhang, X.; Kabacinski, A.; Martorana, D.; Mischo, J.; Stopeck, A.; La Torre, G.N. Factors associated with avoidable 30-day readmissions in patients with cancer: A single institution study. Support. Care Cancer 2025, 33, 206. [Google Scholar] [CrossRef] [PubMed]
- Tennison, J.M.; Rianon, N.J.; Manzano, J.G.; Munsell, M.F.; George, M.C.; Bruera, E. Thirty-day hospital readmission rate, reasons, and risk factors after acute inpatient cancer rehabilitation. Cancer Med. 2021, 10, 6199–6206. [Google Scholar] [CrossRef]
- Zuckerman, R.B.; Sheingold, S.H.; Orav, E.J.; Ruhter, J.; Epstein, A.M. Readmissions, observation, and the hospital readmissions reduction program. N. Engl. J. Med. 2016, 374, 1543–1551. [Google Scholar] [CrossRef] [PubMed]
- Merkow, R.P.; Ju, M.H.; Chung, J.W.; Hall, B.L.; Cohen, M.E.; Williams, M.V.; Tsai, T.C.; Ko, C.Y.; Bilimoria, K.Y. Underlying reasons associated with hospital readmission following surgery in the United States. JAMA 2015, 313, 483–495. [Google Scholar] [CrossRef]
- Jukić, M.; Antišić, J.; Pogorelić, Z. Incidence and causes of 30-day readmission rate from discharge as an indicator of quality care in pediatric surgery. Acta Chir. Belg. 2023, 123, 26–30. [Google Scholar] [CrossRef] [PubMed]
- Guven, D.C.; Ceylan, F.; Cakir, I.Y.; Cesmeci, E.; Sayinalp, B.; Yesilyurt, B.; Guner, G.; Yildirim, H.C.; Aktepe, O.H.; Arik, Z.; et al. Evaluation of early unplanned readmissions and predisposing factors in an oncology clinic. Support. Care Cancer 2021, 29, 4159–4164. [Google Scholar] [CrossRef]
- Wong, E.L.Y.; Cheung, A.W.L.; Leung, M.C.M.; Yam, C.H.K.; Chan, F.W.K.; Wong, F.Y.Y.; Yeoh, E.-K. Unplanned readmission rates, length of hospital stay, mortality, and medical costs of ten common medical conditions: A retrospective analysis of Hong Kong hospital data. BMC Health Serv. Res. 2011, 11, 149. [Google Scholar] [CrossRef]
- Solomon, R.; Egorova, N.; Adelson, K.; Smith, C.B.; Franco, R.; Bickell, N.A. Thirty-Day Readmissions in Patients with Metastatic Cancer: Room for Improvement? J. Oncol. Pract. 2019, 15, e410–e419. [Google Scholar] [CrossRef]
- Fulton, J.J.; LeBlanc, T.W.; Cutson, T.M.; Porter Starr, K.N.; Kamal, A.; Ramos, K.; Freiermuth, C.E.; McDuffie, J.R.; Kosinski, A.; Adam, S.; et al. Integrated outpatient palliative care for patients with advanced cancer: A systematic review and meta-analysis. Palliat Med. 2019, 33, 123–134. [Google Scholar] [CrossRef]
- Bakitas, M.A.; Tosteson, T.D.; Li, Z.; Lyons, K.D.; Hull, J.G.; Li, Z.; Dionne-Odom, J.N.; Frost, J.; Dragnev, K.H.; Hegel, M.T.; et al. Early Versus Delayed Initiation of Concurrent Palliative Oncology Care: Patient Outcomes in the ENABLE III Randomized Controlled Trial. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2015, 33, 1438–1445. [Google Scholar] [CrossRef]
- Groenvold, M.; Petersen, M.A.; Damkier, A.; Neergaard, M.A.; Nielsen, J.B.; Pedersen, L.; Sjøgren, P.; Strömgren, A.S.; Vejlgaard, T.B.; Gluud, C.; et al. Randomised clinical trial of early specialist palliative care plus standard care versus standard care alone in patients with advanced cancer: The Danish Palliative Care Trial. Palliat. Med. 2017, 31, 814–824. [Google Scholar] [CrossRef] [PubMed]
- Hui, D.; Anderson, L.; Tang, M.; Park, M.; Liu, D.; Bruera, E. Examination of referral criteria for outpatient palliative care among patients with advanced cancer. Support. Care Cancer 2020, 28, 295–301. [Google Scholar] [CrossRef] [PubMed]
- Devi, P.S. A Timely Referral to Palliative Care Team Improves Quality of Life. Indian J. Palliat. Care 2011, 17, S14–S16. [Google Scholar] [CrossRef]
- Quaidoo, T.G.; Adu, B.; Iddrisu, M.; Osei-Tutu, F.; Baaba, C.; Quiadoo, Y.; Poku, C.A. Unlocking timely palliative care: Assessing referral practices and barriers at a ghanaian teaching hospital. BMC Palliat. Care 2024, 23, 90. [Google Scholar] [CrossRef]
- Hui, D.; Mori, M.; Watanabe, S.M.; Caraceni, A.; Strasser, F.; Saarto, T.; Cherny, N.; Glare, P.; Kaasa, S.; Bruera, E. Referral criteria for outpatient specialty palliative cancer care: An international consensus. Lancet Oncol. 2016, 17, e552–e559. [Google Scholar] [CrossRef]
- Meisenberg, B.R.; Graze, L.; Brady-Copertino, C.J. A supportive care clinic for cancer patients embedded within an oncology practice. J. Community Support. Oncol. 2014, 12, 205–208. [Google Scholar] [CrossRef] [PubMed]
- Hui, D.; Heung, Y.; Bruera, E. Timely Palliative Care: Personalizing the Process of Referral. Cancers 2022, 14, 1047. [Google Scholar] [CrossRef]
- Montero, A.J.; Stevenson, J.; Guthrie, A.E.; Best, C.; Goodman, L.M.; Shrotriya, S.; Azzouqa, A.G.; Parala, A.; Lagman, R.; Bolwell, B.J.; et al. Reducing Unplanned Medical Oncology Readmissions by Improving Outpatient Care Transitions: A Process Improvement Project at the Cleveland Clinic. J. Oncol. Pract. 2016, 12, e594–e602. [Google Scholar] [CrossRef]
- Manzano, J.G.; Gadiraju, S.; Hiremath, A.; Lin, H.Y.; Farroni, J.; Halm, J. Unplanned 30-Day Readmissions in a General Internal Medicine Hospitalist Service at a Comprehensive Cancer Center. J. Oncol. Pract. 2015, 11, 410–415. [Google Scholar] [CrossRef]
- Leung, C.K.; Walton, N.C.; Kheder, E.; Zalpour, A.; Wang, J.; Zavgorodnyaya, D.; Kondody, S.; Zhao, C.; Lin, H.; Bruera, E.; et al. Understanding Potentially Preventable 7-day Readmission Rates in Hospital Medicine Patients at a Comprehensive Cancer Center. Am. J. Med. Qual. Off. J. Am. Coll. Med. Qual. 2024, 39, 14–20. [Google Scholar] [CrossRef]
- Johnson, P.C.; Xiao, Y.; Wong, R.L.; D’Arpino, S.; Moran, S.M.C.; Lage, D.E.; Temel, B.; Ruddy, M.; Traeger, L.N.; Greer, J.A.; et al. Potentially Avoidable Hospital Readmissions in Patients with Advanced Cancer. J. Oncol. Pract. 2019, 15, e420–e427. [Google Scholar] [CrossRef] [PubMed]
- Donzé, J.D.; Lipsitz, S.; Schnipper, J.L. Risk Factors and Patterns of Potentially Avoidable Readmission in Patients With Cancer. J. Oncol. Pract. 2017, 13, e68–e76. [Google Scholar] [CrossRef]
- Stabellini, N.; Nazha, A.; Agrawal, N.; Huhn, M.; Shanahan, J.; Hamerschlak, N.; Waite, K.; Barnholtz-Sloan, J.S.; Montero, A.J. Thirty-Day Unplanned Hospital Readmissions in Patients with Cancer and the Impact of Social Determinants of Health: A Machine Learning Approach. JCO Clin. Cancer Inform. 2023, 7, e2200143. [Google Scholar] [CrossRef] [PubMed]
- Koubaity, M.; Lechon, A.S.; Amighi, K.; Van Nuffelen, M.; Moreau, M.; Meert, A.P.; De Vriese, C. Drug-related problems and risk factors related to unplanned hospital readmission among cancer patients in Belgium. Support. Care Cancer Off. J. Multinatl. Assoc. Support. Care Cancer 2021, 29, 3911–3919. [Google Scholar] [CrossRef]
- Tang, Q.; Li, X.; Sun, C.R. Predictive value of serum albumin levels on cancer survival: A prospective cohort study. Front. Oncol. 2024, 14, 1323192. [Google Scholar] [CrossRef] [PubMed]
- Bütepage, G.; Carlqvist, P.; Jacob, J.; Toft Hornemann, A.; Vertuani, S. Overall survival of individuals with metastatic cancer in Sweden: A nationwide study. BMC Public Health 2022, 22, 1913. [Google Scholar] [CrossRef]
- Fernandez, F.G.; Khullar, O.; Force, S.D.; Jiang, R.; Pickens, A.; Howard, D.; Ward, K.; Gillespie, T. Hospital readmission is associated with poor survival after esophagectomy for esophageal cancer. Ann. Thorac. Surg. 2015, 99, 292–297. [Google Scholar] [CrossRef]
- Caro, J.J.; Salas, M.; Ward, A.; Goss, G. Anemia as an independent prognostic factor for survival in patients with cancer: A systemic, quantitative review. Cancer 2001, 91, 2214–2221. [Google Scholar] [CrossRef]
- Quinn, Z.L.; Vershvovsky, M.; Xu, A.; Zibelli, A.M. Unplanned hospital admissions are a marker of decreased overall survival in patients with solid tumor malignancies. J. Clin. Oncol. 2020, 38, e19118. [Google Scholar] [CrossRef]
- Roberts, T.J.; McGuire, J.; Temel, J.S.; Lage, D.E.; Greer, J.A.; Mulvey, T.M. Mortality among oncology patients with multiple unplanned hospital admissions. J. Clin. Oncol. 2023, 41, 6578. [Google Scholar] [CrossRef]
- Keller, U. Nutritional Laboratory Markers in Malnutrition. J. Clin. Med. 2019, 8, 775. [Google Scholar] [CrossRef]
- Macciò, A.; Madeddu, C.; Gramignano, G.; Mulas, C.; Tanca, L.; Cherchi, M.C.; Floris, C.; Omoto, I.; Barracca, A.; Ganz, T. The role of inflammation, iron, and nutritional status in cancer-related anemia: Results of a large, prospective, observational study. Haematologica 2015, 100, 124–132. [Google Scholar] [CrossRef] [PubMed]
- Burhenn, P.; Sun, C.L.; Scher, K.S.; Hsu, J.; Pandya, P.; Chui, C.Y.; Arsenyan, A.; Mitani, D.; Morrison, R.; Katheria, V.; et al. Predictors of hospital readmission among older adults with cancer. J. Geriatr. Oncol. 2020, 11, 1108–1114. [Google Scholar] [CrossRef] [PubMed]
- Sonaglioni, A.; Lonati, C.; Tescaro, L.; Nicolosi, G.L.; Proietti, M.; Lombardo, M.; Harari, S. Prevalence and clinical outcome of main echocardiographic and hemodynamic heart failure phenotypes in a population of hospitalized patients 70 years old and older. Aging Clin. Exp. Res. 2022, 34, 1081–1094. [Google Scholar] [CrossRef] [PubMed]
- McNichols, C.C.; Peterson, A.K.; Reynolds, S. The effect of occupational therapy services on hospital readmission for patients with cancer in acute care settings: A retrospective data analysis. J. Cancer Surviv. 2024. [Google Scholar] [CrossRef] [PubMed]
- Yam, C.H.; Wong, E.L.; Chan, F.W.; Leung, M.C.; Wong, F.Y.; Cheung, A.W.; Yeoh, E.K. Avoidable readmission in Hong Kong--system, clinician, patient or social factor? BMC Health Serv. Res. 2010, 10, 311. [Google Scholar] [CrossRef]
| Characteristic | Treated as Outpatients (n = 177) | Treated as Inpatients (n = 300) | Univariate Analysis p-Value | Multivariate Analysis OR (95% CI) p Value |
|---|---|---|---|---|
| Median Age (IQR) | 59 (52–68) | 61 (51–67) | 0.909 | (-) |
| Sex | 0.059 | 0.421 | ||
| Male | 78 (44.1%) | 159 (53%) | ||
| Female | 99 (55.9%) | 141 (47%) | ||
| Primary Diagnosis | 0.203 | (-) | ||
| Other * GI Cancers | 34 (19.2%) | 66 (22.0%) | ||
| Colorectal Cancers | 21 (11.9%) | 44 (14.7%) | ||
| Lung Cancer | 34 (19.2%) | 64 (21.3) | ||
| Breast Cancer | 17 (9.6%) | 25 (8.3%) | ||
| Other ** Cancers | 32 (18.1%) | 52 (17.3%) | ||
| Gynecologic Cancers | 26 (14.7%) | 31 (10.3%) | ||
| Genitourinary Cancers | 13 (7.3%) | 18 (6.0%) | ||
| Disease Stage | <0.001 | 2.52 (95% CI 1.48–4.29) p = 0.001 | ||
| Metastatic | 127 (71.8%) | 261 (87%) | ||
| Non-Metastatic | 50 (28.2%) | 39 (13%) | ||
| Number of Comorbidities | 0.069 | 0.316 | ||
| <3 | 146 (82.5%) | 226 (75.3%) | ||
| ≥3 | 31 (17.5%) | 74 (24.7%) | ||
| ECOG Performance Status | <0.001 | 1.58 (95% CI 1.04–2.42) p = 0.034 | ||
| <2 | 98 (55.4%) | 105 (35%) | ||
| ≥2 | 79 (44.6%) | 195 (65%) | ||
| Number of Regularly Used Drugs | 0.040 | 0.096 | ||
| <5 | 148 (83.6%) | 223 (74.3%) | ||
| ≥5 | 29 (16.4%) | 72 (24.0%) | ||
| Unknown | 0 | 5 (1.7%) | ||
| Type of Cancer Treatment | 0.779 | (-) | ||
| Chemotherapy | 110 (62.1%) | 193 (64.3%) | ||
| Radiotherapy | 16 (9.0%) | 16 (5.4%) | ||
| Others *** | 31 (17.5) | 46 (15.3%) | ||
| No Active Treatment | 20 (11.3%) | 45 (15%) | ||
| Indication for Follow-Up | 0.073 | 0.152 | ||
| Symptom Palliation | 135 (76.3%) | 206 (68.7%) | ||
| Infection and/or Interventional Procedure | 42 (23.7%) | 95 (31.3%) | ||
| Hemoglobin Level | ||||
| Mean (sd) (g/dL) | 10.7 (2.1) | 10.2 (2.2) | 0.03 | 0.89 |
| Albumin Level | ||||
| Mean (sd) (g/dL) | 3.39 (0.59) | 3.03 (0.58) | <0.001 | 0.42 (95% CI 0.29–0.61) p <0.001 |
| (a) | ||||||||
| 95% CI | ||||||||
| Variables | B | S.E. | Wald | df | p-Value | OR | Lower | Upper |
| Age (Years) | 0.011 | 0.008 | 2.11 | 1 | 0.146 | 1.01 | 0.996 | 1.03 |
| Sex | −0.191 | 0.188 | 1.03 | 1 | 0.309 | 0.83 | 0.57 | 1.20 |
| Male | ||||||||
| Female | ||||||||
| Type of Cancer Treatment | ||||||||
| Chemotherapy (Ref) | ||||||||
| Radiotherapy | −0.098 | 0.379 | 0.067 | 1 | 0.102 | 0.91 | 0.43 | 1.91 |
| Others * | −0.452 | 0.257 | 3.093 | 1 | 0.64 | 0.39 | 1.05 | |
| No Active Treatment | 0.407 | 0.297 | 1.872 | 1 | 1.50 | 0.84 | 2.69 | |
| Albumin (g/dL) | −0.687 | 0.165 | 17.38 | 1 | <0.001 | 0.50 | 0.36 | 0.70 |
| Disease Stage | 0.639 | 0.237 | 7.28 | 1 | 0.007 | 1.89 | 1.20 | 3.02 |
| Metastatic | ||||||||
| Non-Metastatic | ||||||||
| ECOG Performance Status | 0.426 | 0.190 | 5.03 | 1 | 0.025 | 1.53 | 1.06 | 2.22 |
| <2 | ||||||||
| ≥2 | ||||||||
| Hemoglobin (g/dL) | −0.006 | 0.043 | 0.022 | 1 | 0.88 | 0.99 | 0.91 | 1.08 |
| (b) | ||||||||
| 95% CI | ||||||||
| Variables | B | S.E. | Wald | df | p-Value | OR | Lower | Upper |
| Age (Years) | 0.008 | 0.008 | 0.882 | 1 | 0.345 | 1.008 | 0.99 | 1.02 |
| Type of Cancer Treatment | ||||||||
| Chemotherapy (Ref) | ||||||||
| Radiotherapy | 0.017 | 0.430 | 0.002 | 1 | 0.171 | 1.02 | 0.44 | 2.35 |
| Others * | −0.434 | 0.275 | 2.48 | 1 | 0.66 | 0.39 | 1.13 | |
| No Active Treatment | 0.382 | 0.321 | 1.42 | 1 | 1.54 | 0.83 | 2.87 | |
| Albumin (g/dL) | −0.614 | 0.169 | 13.18 | 1 | <0.001 | 0.54 | 0.39 | 0.75 |
| Disease Stage | 0.401 | 0.259 | 2.40 | 1 | 0.121 | 0.67 | 0.40 | 1.11 |
| Metastatic | ||||||||
| Non-Metastatic | ||||||||
| ECOG Performance Status | 0.149 | 0.222 | 0.45 | 1 | 0.502 | 0.87 | 0.57 | 1.33 |
| <2 | ||||||||
| ≥2 | ||||||||
| Constant | 2.405 | 0.553 | 18.91 | 1 | <0.001 | 11.08 | ||
| (a) | ||||||||
| 95% CI | ||||||||
| Variables | B | S.E. | Wald | df | p-Value | HR | Lower | Upper |
| Age (Years) | −0.001 | 0.004 | 0.07 | 1 | 0.798 | 0.99 | 0.99 | 1.007 |
| Sex | 0.266 | 0.108 | 6.07 | 1 | 0.016 | 0.77 | 0.62 | 0.95 |
| Male | ||||||||
| Female | ||||||||
| Number of Regularly Used Drugs | 0.063 | 0.131 | 0.23 | 1 | 0.630 | 1.07 | 0.82 | 1.38 |
| <5 | ||||||||
| ≥5 | ||||||||
| Number of Comorbidities | −0.035 | 0.133 | 0.071 | 1 | 0.770 | 0.97 | 0.74 | 1.25 |
| <3 | ||||||||
| ≥3 | ||||||||
| Type of Cancer Treatment | ||||||||
| Chemotherapy (Ref) | ||||||||
| Radiotherapy | −0.411 | 0.239 | 2.95 | 1 | 0.010 | 0.66 | 0.42 | 1.06 |
| Others * | <0.001 | 0.151 | <0.001 | 1 | 1.00 | 0.75 | 1.34 | |
| No Active Treatment | 0.362 | 0.160 | 5.11 | 1 | 1.44 | 1.05 | 1.96 | |
| Albumin (g/dL) | −0.720 | 0.091 | 62.92 | 1 | <0.001 | 0.43 | 0.36 | 0.51 |
| Disease Stage | 0.668 | 0.155 | 18.48 | 1 | <0.001 | 1.95 | 1.44 | 2.65 |
| Metastatic | ||||||||
| Non-Metastatic | ||||||||
| ECOG Performance Status | 1.377 | 0.124 | 124.23 | 1 | <0.001 | 3.96 | 3.11 | 5.05 |
| <2 | ||||||||
| ≥2 | ||||||||
| Unplanned Hospital Readmission | 0.436 | 0.114 | 14.56 | 1 | <0.001 | 1.55 | 1.24 | 1.93 |
| Yes | ||||||||
| No | ||||||||
| Hemoglobin (Mean) (g/dL) | −0.068 | 0.026 | 7.00 | 1 | 0.008 | 0.93 | 0.89 | 0.98 |
| Indication for Follow-Up | −0.091 | 0.122 | 0.564 | 1 | 0.45 | 0.913 | 0.72 | 1.16 |
| Symptom Palliation | ||||||||
| Infection and/or Interventional Procedure | ||||||||
| (b) | ||||||||
| 95% CI | ||||||||
| Variables | B | S.E. | Wald | df | p-Value | HR | Lower | Upper |
| Sex | 0.249 | 0.111 | 5.03 | 1 | 0.025 | 1.28 | 1.03 | 1.59 |
| Male | ||||||||
| Female | ||||||||
| Type of Cancer Treatment | ||||||||
| Chemotherapy (Ref) | ||||||||
| Radiotherapy | −0.300 | 0.242 | 1.53 | 1 | 0.192 | 0.74 | 0.46 | 1.19 |
| Others * | 0.056 | 0.152 | 0.13 | 1 | 1.06 | 0.78 | 1.43 | |
| No Active Treatment | 0.264 | 0.164 | 2.58 | 1 | 1.39 | 0.94 | 1.80 | |
| Albumin (g/dL) | −0.391 | 0.100 | 15.18 | 1 | <0.001 | 0.68 | 0.56 | 0.82 |
| Disease Stage | 0.423 | 0.161 | 6.94 | 1 | 0.008 | 1.53 | 1.11 | 2.09 |
| Metastatic | ||||||||
| Non-Metastatic | ||||||||
| ECOG Performance Status | 1.230 | 0.130 | 91.32 | 1 | <0.001 | 3.45 | 2.68 | 4.45 |
| <2 | ||||||||
| ≥2 | ||||||||
| Unplanned Hospital Readmission | 0.260 | 0.118 | 4.88 | 1 | 0.027 | 1.30 | 1.03 | 1.63 |
| Yes | ||||||||
| No | ||||||||
| Hemoglobin (Mean) (g/dL) | −0.025 | 0.27 | 0.86 | 1 | 0.35 | 0.98 | 0.93 | 1.03 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baş, O.; Tokatlı, M.; Güdük, N.; Erdoğan, D.; Boyraz, N.E.; Çengelci, Ç.; Guven, D.C.; Dizdar, Ö.; Türker, F.A.; Aksoy, S. Clinical Characteristics and Management of Patients Admitted to the Supportive Care Clinic and Predisposing Factors of Unplanned Hospital Readmission: Single-Center Experience. J. Clin. Med. 2025, 14, 2679. https://doi.org/10.3390/jcm14082679
Baş O, Tokatlı M, Güdük N, Erdoğan D, Boyraz NE, Çengelci Ç, Guven DC, Dizdar Ö, Türker FA, Aksoy S. Clinical Characteristics and Management of Patients Admitted to the Supportive Care Clinic and Predisposing Factors of Unplanned Hospital Readmission: Single-Center Experience. Journal of Clinical Medicine. 2025; 14(8):2679. https://doi.org/10.3390/jcm14082679
Chicago/Turabian StyleBaş, Onur, Mert Tokatlı, Naciye Güdük, Dilara Erdoğan, Nur Evşan Boyraz, Çağla Çengelci, Deniz Can Guven, Ömer Dizdar, Fatma Alev Türker, and Sercan Aksoy. 2025. "Clinical Characteristics and Management of Patients Admitted to the Supportive Care Clinic and Predisposing Factors of Unplanned Hospital Readmission: Single-Center Experience" Journal of Clinical Medicine 14, no. 8: 2679. https://doi.org/10.3390/jcm14082679
APA StyleBaş, O., Tokatlı, M., Güdük, N., Erdoğan, D., Boyraz, N. E., Çengelci, Ç., Guven, D. C., Dizdar, Ö., Türker, F. A., & Aksoy, S. (2025). Clinical Characteristics and Management of Patients Admitted to the Supportive Care Clinic and Predisposing Factors of Unplanned Hospital Readmission: Single-Center Experience. Journal of Clinical Medicine, 14(8), 2679. https://doi.org/10.3390/jcm14082679







