Acanthamoeba Keratitis Management and Prognostic Factors: A Systematic Review
Abstract
1. Introduction
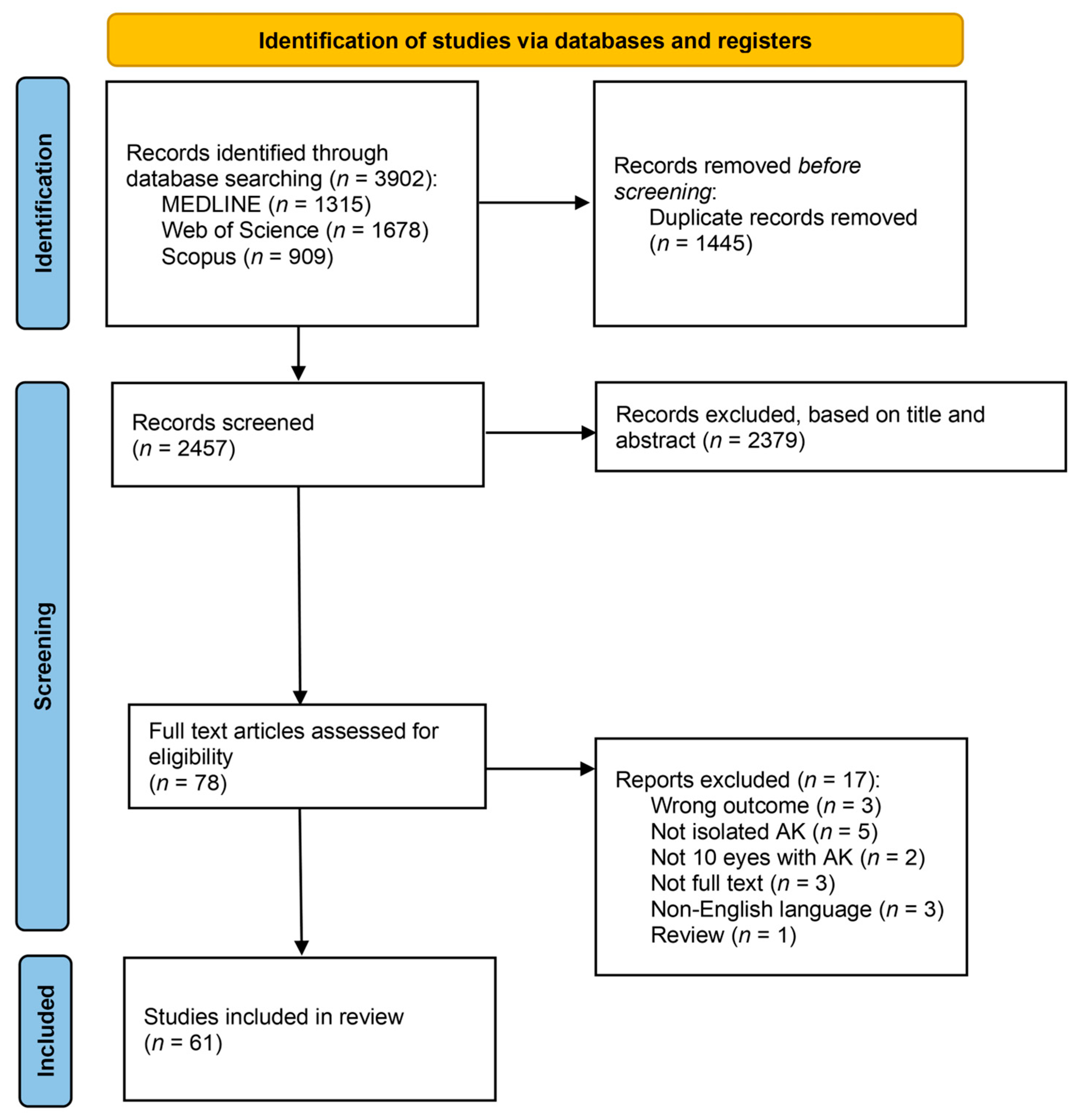
2. Materials and Methods
2.1. Search Strategy
- Study type: “randomized controlled trial”, “RCT”, “cohort studies”, “follow-up studies”, “longitudinal studies”, “prospective studies” or “retrospective studies”.
- Acanthamoeba: “Acanthamoeba”, “Ameba”, “Acanthamoeba Keratitis”, “Ameba Keratitis”, “Parasitic Keratitis”, “Acanthamoeba corneal infection”, “Ameba corneal infection”, “contact lens keratitis” or “contact lens associated keratitis”
- AK-related parameters: “treatment”, “surgery”, “follow-up”, “complications”, “prognosis”, “management” or “therapy”.
2.2. Eligibility Criteria
- Studies with a sample size of at least 10 eyes with isolated Acanthamoeba corneal infection.
- Outcome is one of the following AK-related parameters: type of treatment, need for surgery, type of surgery, follow-up, complications, prognosis or prognostic factors, and management strategies.
2.3. Study Selection, Data Collection Process and Data Items
2.4. Study Risk of Bias Assessment
3. Results
3.1. Study Selection
3.2. Study Characteristics
| Article | Study Design | Population (Country; Age (Mean); Sex (M, F)(%)) | No Patients/Eyes | Follow-Up (Months) |
|---|---|---|---|---|
| Pang et al. (2024) [40] | Retrospective cross-sectional | China, 41.5 y, M (55.3%), F (44.7%) | 109/109, results and outcomes were not available for 1 patient | 6.9 |
| List et al. (2021) [41] | Retrospective cohort | Austria, 31 y, M (54.5%), F (45.5%) | 42/44 | N/A |
| Megha et al. (2020) [38] | Prospective case series | North India; 33 y; M (72.7%), F (27.3%) | 11/11, 1 lost in follow-up | N/A |
| Jo et al. (2020) [42] | Retrospective cohort | Busan, South Korea; 21 y; M 12.5%, F 87.5% | 16/19 | 5.365 (range of 1–20) |
| Musayeva et al. (2020) [22] | Retrospective case series | Germany; 41.7 y; M 42.9%, F 57.1% | 28/28, 2 lost in follow-up | N/A |
| Papa et al. (2020) [43] | Retrospective cohort | UK (London); 13–33 y: 51.98% 34–76 y: 48.02%; M: 44.05%; F: 55.95% | 227/227 | At least 12 months after AAT |
| Lin et al. (2018) [44] | Retrospective interventional case series | Taiwan; 23.4 ± 11.1 (range 13–49) y; M (45.5%), F (54.5%) | 22/24 | 12 |
| McKelvie et al. (2018) [45] | Retrospective case series | New Zealand; 36 (15–66) y; M (44.2%); F (55.8%) | 52/58 | 9 |
| Lim et al. (2008) [18] | Prospective, double-masked, randomized comparative trial | London (Moorfields Eye Hospital); 31 y (IQR, 24 to 36 years); M (45.1%), F (52.94%) | 55/56, only 51 eyes were analyzed in the study | PHMB group: 2.7 ± 2.0 CHX group: 3.0 ± 1.2 |
| Wouters et al. (2022) [24] | Retrospective case–control | The Netherlands (Rotterdam) Control: 41 ± 17 y (15–70); M (58.5%); F (41.5%) Cases: 35 ± 17 y (11–74); M (46.43%), F (53.57%) | 109/109 | 18 ± 25 (range 1–207) |
| Thulasi et al. (2021) [23] | Descriptive, retrospective multicenter case series | EUA 47.4 y (16 to 80) M (20%); F(80%) | 15/15 | 7 |
| Rahimi et al. (2015) [26] | Prospective interventional case series | Iran 21.5 ± 4.6 y M (12.9%), F (87.1%) | 31/31 | 4 |
| Robaei et al. (2014) [25] | Retrospective cohort | London, UK CCT before diagnosis: 40.3 y; M (48.28%), F (51.72%) Not-CCT before diagnosis: 33.6 y; M (44.83%), F (55.17%) | 174/174 | CCT before diagnosis: 18.5 (6.5–44) Not-CCT before: 7.5 (4.5–24) |
| Bagga et al. (2021) [33] | Prospective, randomized, double-masked pilot clinical trial | India; 39.8 ± 14.3 y; M (61.1%), F (38.9%) | 23/23, only 18 patients completed the study | 2.8 ± 2.4 |
| Azuara-Blanco et al. (1997) [46] | Retrospective case series | UK 30.0 ± 7.4 y (19–40) M (60%), F (40%) | 10/10 | 7.3 (range 4–15) |
| Duguid et al. (1997) [21] | Retrospective case series | London, UK 32 y (16–64) M (57.1%), F (42.9%) | 105/111 | N/A |
| Hargrave et al. (1999) [34] | Prospective, multicenter noncomparative case series | EUA 33 y (18–72) N/A | 83/87, only 60 eyes had their data analyzed for treatment efficacy and safety | 15 |
| Carnt et al. (2016) [47] | Retrospective cohort. | London, UK 33 y (15–76) M (47.3%), F (54.0%) | 196/196, only 129 included in the multivariable analysis; eyes with scleritis or hypopyon at the start of AAT were excluded (as these conditions were strongly associated with previous corticosteroid use) | N/A |
| Höllhumer et al. (2020) [48] | Retrospective case review | Sydney, Australia 39 y (14–89) M (40%), F (60%) | 52/52 | 33 |
| Caruso et al. (2020) [35] | Prospective interventional case series study. | Naples, Italy 27.03 ± 10.61 y M (31.04%), F (68.96%) | 29/29 | At least 3 months after completion of treatment |
| Dart et al. (2024) [36] | Prospective, randomized, double-masked, active-controlled, multicenter phase 3 clinical trial | UK, Italy and Poland 36.7 ± 13.8 y (15–73) M (41.7%), F (58.3%) | 135/135, 127 full-analysis subset; 134 in the safety analysis subset | 12 |
| Blaser et al. (2024) [49] | Retrospective, single-center chart review | Switzerland 33 y (13–90) M (40.4%), F (59.6%) | 52/59, 46 were treated | N/A |
| Tew et al. (2020) [50] | Retrospective case series | Taiwan, 12–56 (28 y) M (50%), F (50%) | 107/107, 10 eyes with AK | Postoperative follow-up period was at least 1 month in all patients |
| Chen et al. (2004) [51] | Retrospective interventional case series | Taiwan 57.6 y (17–84) N/A | 108/108, 15/15 with AK | 12 |
| Laurik et al. (2019) [52] | Retrospective observational cohort | Germany 39.6 ± 13.3 y N/A | 23/23 | 27 ± 19.4 |
| Liu et al. (2020) [53] | Retrospective case series | Taiwan 27.1 ± 1.5 y (12–65) M (45.2%), F (54.8%) | 62/62 | N/A |
| Kitzmann et al. (2009) [54] | Retrospective, nonrandomized, comparative, interventional case series | USA TPK: 40 y; OPK: 30 y (13–72) M (40%), F (60%) | 30/31 | N/A |
| Qi et al. (2024) [55] | Retrospective cohort | China BB-DALK Group: 44.56 ± 15.5 y; M: 63.0% (17/27), F: 37.0% (10/27) PKP Group: 48.79 ± 15.7 y M: 45.8% (11/24), F: 54.2% (13/24) | 51/51 | BB-DALK 26.78 ± 21.11 (range, 0–78) PKP 27.29 ± 21.23 (range, 0–79) |
| Wang et al. (2023) [56] | Retrospective case series | China 45.54 ± 11.78 y (24–66) M (61.5%); F (38.5%) | 13/13 | 21.31 ± 19.59 (range, 12–82) |
| Zhang et al. (2023) [57] | Retrospective cohort | China 44.6 ± 12.4 y M (56.9%), F (43.1%) | 58/59 with stage 3 AK requiring keratoplasty | PK: 6.2 ± 3.7 LK: 6.2 ± 7.5 |
| Roozbahani et al. (2019) [58] | Retrospective case series | USA 49 ± 18 y (16–73 y) M (33%), F (66%) | 63/63 | 3 months after ending therapy |
| Sabatino et al. (2016) [59] | Retrospective, noncomparative case series | Italy 24.5 ± 7 y (15–37) M (45%), F (55%) | 11/11 | 25 ± 10 (range, 12–39) |
| Robaei et al. (2015) [60] | Retrospective case series | UK OPK: 44.3 ± 16.6 y; M (50%), F (50%) TPK: 43.0 ± 12.1 y; M (61.5%), F (38.5%) | 196/50 | 62 ± 3 |
| Bagga et al. (2020) [61] | Retrospective cohort | India 38.7 ± 8.6 y (25–56) M (50%), F (50%) | 23/23, 10 with advanced AK (infiltrate ≥ 8 mm) | 5 (IQR, 1.4–11.4) |
| Thebpatiphat et al. (2007) [62] | Retrospective case series | USA 38 y (13–75) M (55%), F (45%) | 20/20 | N/A |
| Butler et al. (2005) [63] | Retrospective case series | Australia 38.9 ± 14.0 y M (45%), F (55%) | 20/20 | 24.8 ± 21.5 (1–72) |
| Chin et al. (2015) [64] | Retrospective case series | Hong Kong 24.1 ± 8.01 y (13 to 38 y) M (30.8%), F (69.2%) | 13/15 | N/A |
| Alfonso-Muñoz et al. (2018) [65] | Retrospective case series | Spain 28.4 y M (60%), F (40%) | 10/10 Superficial stroma: 3/10 (30%) Deep stroma (ring infiltrates or corneal abscesses): 7/10 (70%) | 12 |
| Kaiserman et al. (2012) [66] | Retrospective cohort | Canada 34.2 ± 13.2 y M (51.2%), F (48.8%) | 41/42 | 19.7 ± 21.0 (median: 13) |
| Ikeda et al. (2012) [67] | Retrospective cross-sectional | Japan 26.4 ± 1.7 y M (39.3%), F (60.7%) | 103/104, 28/29 with AK | N/A |
| Patel et al. (2010) [68] | Retrospective case series | New Zealand 40 ± 13 y M (40%), F (60%) | 25/25, 1 lost in follow up | N/A |
| Shimmura-Tomita et al. (2018) [69] | Retrospective comparative case series | Japan Severe group: 37 y Mild group: 24 y M (50%), F (50%) | 10/10 | N/A |
| Zhang et al. (2014) [70] | Retrospective cohort | China 44 ± 12 y M (62%), F (38%) | 29/29 | N/A |
| Elmer et al. (2008) [39] | Retrospective case–control | USA 28.7 ± 14.9 y M (52.8%), F (47.2%) | 65/72 Cases: ≥0.1 logMAR or PKP Control: ≤0.1 logMAR | At least 3 months post-treatment completion |
| Radford et al. (1998) [71] | Multicenter retrospective cross-sectional | England 31.5 y (4 to 64) M (56%), F (44%) | 243/259 | 6 |
| Vilares-Morgado et al. (2024) [28] | Retrospective, single-center, longitudinal | Portugal 35.7 ± 13.8 y (14 to 66) M (28.7%), F (71.3%) | 46/51 BCVA final < 1 logMAR group: 31 (60.8%) BCVA final ≥ 1 logMAR group: 20 (39.2%) | 39 ± 30.2 (14–120) |
| Randag et al. (2019) [72] | Retrospective case series, multicenter nationwide survey | Netherlands 34 y (11 to 75) M (37.5%), F (62.5%) | 224/224 | 11.6 ± 27.4 |
| Bacon et al. (1993) [73] | Retrospective case series | UK; N/A; N/A | 72/77, 4 lost to follow up | 3 |
| G D’Aversa et al. (1995) [74] | Retrospective case series | USA; N/A; N/A | 12/14 | N/A |
| Claerhout et al. (2004) [75] | Retrospective case series | Belgium 32 y (19 to 64) M (71%), F (29%) | 14/14 Early treatment ≤18 days of symptom onset: 6/14 Late treatment >18 days: 8/14 | 34 (range 1–63) |
| Chew et al. (2011) [76] | Retrospective case series | USA 34 y (12 to 75) M (47%), F (53%) | 59/59 | 11.2 (range: 0.4–35.1) |
| Bouheraoua et al. (2013) [27] | Retrospective noncomparative interventional case series | France 43 y (14 to 90) M (28%), F (72%) | 42/44 | 10 (1–49) |
| Carnt et al. (2018) [13] | Retrospective cohort | UK; N/A; N/A | 194/194 | Bad Outcomes group: 32 (IQR: 15–58) Good Outcomes group: 7 (IQR: 4–1) |
| Chopra et al. (2020) [77] | Retrospective cohort | UK 41.5 ± 15.7 y (20 to 81) M (44.6%), F (55.4%) | 157/157 | At least 3 months after stopping treatment |
| Bonini et al. (2021) [78] | Retrospective case series | Italy 30 ± 13 y N/A | 35/40 | 146.4 ± 66 |
| Rahimi et al. (2014) [37] | Prospective intervencional case series | Iran 23 ± 6 y (14–36) M (16%), F (84%) | 25/27 | At least 6 months after ending treatment |
| Yamazoe et al. (2012) [79] | Retrospective case series | Japan 29.4 ± 8.9 y (16–49) M (71.4%), F (28.6%) | 34/35 Group 1: final VA of ≤ 0.10 logMar (22 eyes) Group 2: >0.10 logMar (13 eyes) | Group 1: Median 6.7 (IQR 5.2–11.8) Group 2:Median 9.5 (IQR 4.7–42.5) |
| Arnalich-Montiel et al. (2014) [80] | Prospective cohort | Spain; N/A; N/A | 17/17 | Median: 6 months |
| Park et al. (1997) [81] | Retrospective case series | USA; Steroid-treated: 36.2 14.0; M (50%), F (50%). Non-steroid treated: 27.8 9.0; M (33.3%), F (67.6%) | 38/38 | N/A |
| Landeo et al. (2015) [82] | Retrospective case series | Peru; 24.9 y; M (50%), F (50%) | 14/14 early treatment (<30 days): 5/14 late treatment (≥30 days): 9/14 | N/A |
| Sun et al. (2006) [83] | Retrospective, noncomparative, interventional case series | China; 26 y (ranged from 12 to 50); M (60%), F (40%) | 20/20 | 8.8 (range, 2.5–25.4) |
| Article | No Patients/Eyes | Medical Therapy, n (%) | Surgical Therapy, n (%) |
|---|---|---|---|
| Pang et al. (2024) [40] | 109/109, Results and outcomes were not available for 1 patient | CHX 0.02% + PHMB 0.02%, 109 (100%) (initially used hourly for the first week and tapered slowly over the following four weeks to dosing four times a day). Maintenance therapy: 0.02% CHX four times a day for three to six months. | N/A |
| List et al. (2021) [41] | 42/44 | Biguanide (0.02%), 42 (95.5%); Diamidine (0.1%), 40 (90.9%) | N/A |
| Megha et al. (2020) [38] | 11/11, 1 lost in follow-up | PHMB (0.02%), 10 (100%) (half hourly for 1 week, then hourly for 1 week and then gradually tapered according to the response) | N/A |
| Jo et al. (2020) [42] | 16/19 | PHMB 0.02%, 9 (47.4%) CHX 0.02%, 5 (26.3%) PHMB + CHX, 5 (26.3%) | N/A |
| Musayeva et al. (2020) [22] | 28/28, 2 lost in follow-up | PHMB 0.02% + propamidine 0.1% + voriconazole 0.1%: 26 (100%); 24 h/36 h: every 15 to 30 min in an alternating fashion during day and night. Application was then reduced to 4 times daily each in an alternating fashion during the day. Dexamethasone 0.13% after 24/36 h to reduce inflammation and corneal scarring | N/A |
| Papa et al. (2020) [43] | 227/227 | CHX 0.02% or PHMB 0.02% Propamidine 0.1% or hexamidine 0.1% (Monotherapy or association between drugs) | N/A |
| Lin et al. (2018) [44] | 22/24 | Ethanol pretreatment (30 s before Epithelial debridment) + PHMB (0.02%) + propamidine (0.1%), 24 (100%) | TED, 24 (100%) |
| McKelvie et al. (2018) [45] | 52/58 | Biguanide (PHMB 0.02% or CHX 0.02%) + Propamidine 0.1%, 58 (100%) Empiric topical CCT, 6 (10.3%) | N/A |
| Lim et al. (2008) [18] | 55/56, only 51 eyes were analyzed in the study | PHMB 0.02%, 23 (45%) CHX 0.02%, 28 (55%) | N/A |
| Wouters et al. (2022) [24] | 109/109 | Cases: CCT before AAT, 56 (51%) Controls: 53 (49%) | N/A |
| Thulasi et al. (2021) [23] | 15/15 | Oral Miltefosine (50 mg once or twice a day) as adjunctive therapy, 15 (100%) | N/A |
| Rahimi et al. (2015) [26] | 31/31 | Monotherapy with CHX 0.02%, 31 (100%) Topical CCT(at least 2 weeks after treatment with chlorhexidine), 26 (83.9%) CCT before diagnosis: 12 (38%) | N/A |
| Robaei et al. (2014) [25] | 174/174 | CTT before diagnosis: 87 (50%) (63 (73.3%) misdiagnosed as herpetic keratitis) (p < 0.001) No CCT before diagnosis: 87 (50%) (28 (32.2%) misdiagnosed as herpetic keratitis)(p < 0.001) | N/A |
| Bagga et al. (2021) [33] | 23/23, only 18 patients completed the study | VZ group: Topical 1% voriconazole monotherapy: 8 (44.4%) BG group: PHMB 0.02% + CHX 0.02%: 10 (55.5%) Both hourly during the day and every 2 h at night for 1 week, followed by gradual tapering. | N/A |
| Azuara-Blanco et al. (1997) [46] | 10/10 | PHMB 0.02% + propamidine 0.1%: 9 (90%) CHX 0.02% + propamidine: 1 (10%) (later switched to PHMB); Polymixin B sulfate and bacitracin zinc, 10 (100%) Prednisolone acetate 0.5%, 2–4 times daily, 10 (100%) | 2 OPK for visual rehabilitation due to scarring, 2 (20%) |
| Duguid et al. (1997) [21] | 105/111 | PHMB 0.02% + propamidine 0.1%, 111 (100%) Applied hourly, day and night for 2–3 days initially, then reduced based on response. Therapy continued for 6–8 weeks after resolution of inflammation. | N/A |
| Hargrave et al. (1999) [34] | 83/87, only 60 eyes had their data analyzed for treatment efficacy and safety | Propamidine isethionate 0.1% + neomycin-polymyxin B-gramicidin, 87 (100%) | N/A |
| Carnt et al. (2016) [47] | 196/196, only 129 were included in the multivariable analysis | CCT after start of AAT: 73 (56.6%) No CCT: 56 (43.4%) | N/A |
| Höllhumer et al. (2020) [48] | 52/52 | PHMB, CHX, Propamidine (28 (54%) used a triple combination; 23 (44%) used dual therapy; 1 (2%) monotherapy) Adjunctive therapy: Oral voriconazole: 9 (17%) | N/A |
| Caruso et al. (2020) [35] | 29/29 | CHX 0.02% and VE-TPGS 0.2%: 29 (100%) | N/A |
| Dart et al. (2024) [36] | 135/135, 127 in the full-analysis subset; 134 in the safety analysis subset | PHMB 0.08%: 66 (51.96%) PHMB 0.02% + propamidine: 61 (48.03%) Every hour for the first 19 days. Tapered to four times daily over the next months. | N/A |
| Blaser et al. (2024) [49] | 52/59, 46 were treated | Propamidine 0.1% + PHMB 0.02% hourly (48 h day/night) → hourly (72 h daytime) → tapered (~3×/day) for 12 months Dexamethasone 0.1% after 4 weeks | Initial TED, 46 (100%) |
| Tew et al. (2020) [50] | 107/107, 10 eyes with AK | N/A | TPK: 10 (100%) |
| Chen et al. (2004) [51] | 108/108, 15/15 with AK | N/A | PKP after medical treatment failure: 15 (100%) |
| Laurik et al. (2019) [52] | 23/23 | PHMB (0.02%) + propamidine (0.1%) + Neomicine (0.02%) (100%) | KP after intensive topical triple therapy failure (100%) Early PK (<5.3 months of symptom onset): 14/23 (61%) Delayed PK (after 5.3 months): 9/23 (39%) |
| Liu et al. (2020) [53] | 62/62 | Medically treated 40 (64.5%) | OPK: 10 (25%) TPK: 17 (77.3%) |
| Kitzmann et al. (2009) [54] | 30/31 | N/A | TKP: 22 (71%); OPK: 9 (29%) Ring infiltrate (TPK 82% vs. OPK 0%, p = 0.001) or epithelial defect (TPK 64% vs. OPK 22%, p = 0.05) |
| Qi et al. (2024) [55] | 51/51 | N/A | PKP: 24 (47%) (Cases with higher incidence of ring infiltrates, endothelial plaques, hypopyon, uveitis, and glaucoma (p = 0.007)) BB-DALK: 27 (53%) (Lower percentage of stage 3 disease (p = 0.003)) |
| Wang et al. (2023) [56] | 13/13 | N/A | Elliptical DALK: 13 (100%) |
| Zhang et al. (2023) [57] | 58/59 with stage 3 AK requiring keratoplasty | N/A | PKP: 36 (61%) LKP: 23 (39%) |
| Roozbahani et al. (2019) [58] | 63/63 | PHMB 0.02% + CHX 0.02% (or combined with propamidine) 51 (81%); neoadjuvant therapy: voriconazole, itraconazole or neomycin | TPK, 12 (19%) |
| Sabatino et al. (2016) [59] | 11/11 | N/A | Early therapeutic DALK (manual dissection or BB) (within 30 to 60 days from the onset of symptoms), 11(100%) |
| Robaei et al. (2015) [60] | 196/50 | N/A | TKP: 26 (52%); OKP: 24 (48%) |
| Bagga et al. (2020) [61] | 23/23, 10 with advanced AK (infiltrate ≥8 mm) | PHMB 0.02% + CHX 0.02%; prednisolone acetate 1% started after infection control | DALK: 23 (100%) (10 (43%) advanced AK/ 13 (57%) less severe AK) |
| Thebpatiphat et al. (2007) [62] | 20/20 | N/A | N/A |
| Butler et al. (2005) [63] | 20/20 | PHMB 0.02% + propamidine 0.1%, 20 (100%) CHX 0.02%: 9 (45%) Neosporin®: 8 (40%) | N/A |
| Chin et al. (2015) [64] | 13/15 | AAT:15 (100%) CCT: 9 (60%) | N/A |
| Alfonso-Muñoz et al. (2018) [65] | 10/10, superficial stroma: 3/10 (30%) deep stroma (ring infiltrates or corneal abscesses): 7/10 (70%) | CHX 0.02% + Propamidine 0.1%: 10 (100%) Adjunctive treatment: polymyxin B sulfate, neomycin sulfate and gramicidin: 3 (30%) oral antifungal treatment (itraconazole or fluconazole): 4 (40%) CCT: 6 (60%) due to pain and inflammation (average of 53 days after beginning the AAT) | N/A |
| Kaiserman et al. (2012) [66] | 41/42 | PHMB 0.02%: 37 (88.1%) Propamidine 0.1%: 20 (47.6%) CHX 0.02%: 13 (31%) Neomycin, Polymyxin B, Gramicidin (Neosporin®): 32 (76.2%) Combination Therapy: 85.7% of patients received combination therapy, mostly with three agents (57.1%) Topical CCT: 26 (61.9%) | KP: 7 (22.6%) |
| Ikeda et al. (2012) [67] | 103/104, 28/29 with AK | N/A | N/A |
| Patel et al. (2010) [68] | 25/25, 1 lost in follow up | PHMB 0.02% or CHX 0.02% + Propamidine CCT before diagnosis: 14 (56%) | N/A |
| Shimmura-Tomita et al. (2018) [69] | 10/10 | N/A | N/A |
| Zhang et al. (2014) [70] | 29/29 | N/A | N/A |
| Elmer et al. (2008) [39] | 65/72 | N/A | N/A |
| Radford et al. (1998) [71] | 243/259 | Propamidina + PHMB: 108 (50%). Propamidina + Neomicina + PHMB: 31 (14%). Propamidina + Clorexidina: 15 (7%). (197 (90%) were treated with PHMB and/or CHX) | N/A |
| Vilares-Morgado et al. (2024) [28] | 46/51 BCVA final < 1 logMAR group: 31 (60.8%) BCVA final ≥ 1 logMAR group: 20 (39.2%) | CHX (0.02%): 1 (2%) Propamidine (0.1%): 6 (12%) CHX + Propamidine: 41 (79%) Additional therapy: Oral Voriconazole: 1 (2%) Oral Miltefosine: 2 (4%) | TED: 22 (43%) KP: 18 (35%) for corneal perforation or treatment failure Evisceration/Enucleation: 12 (23.5%) |
| Randag et al. (2019) [72] | 224/224 | CHX monotherapy:220 (98%) CHX + PHMB/Propamidine:184 (82%) CCT after diagnosis: 92 (41%) | N/A |
| Bacon et al. (1993) [73] | 72/77, 4 lost to follow up | Propamidine + neomycin, 29 (39.7%); Propamidine + PHMB, 13 (17.8%); Propamidine + neomycin + PHMB, 12(16.4%); broader combinations in 22 eyes (30.1%) included paromomycin, itraconazole, and others. | 34 KP in 23 eyes: TPK: 21 in inflamed eyes OPK: 13 in uninflamed eyes |
| G D’Aversa et al. (1995) [74] | 12/14 | Propamidine isethionate + neomycin sulfate + clotrimazole, 11 (79%); neomycin-gramicidin-polymyxin, 2 (14%); broad-spectrum agents, 1 (7%) | TKP: 3 (21%) (1 for bacterial superinfection, 1 for large descemetocele, 1 after failed medical treatment) |
| Claerhout et al. (2004) [75] | 14/14, early treatment ≤18 days of symptom onset: 6/14 late treatment >18 days: 8/14 | Propamidine + chlorhexidine or PHMB 14 (100%) | N/A |
| Chew et al. (2011) [76] | 59/59 | PHMB 0.02%, Propamidine, and antibiotics (100%); oral antifungals (itraconazole/voriconazole) in severe cases; 61% treated with corticosteroids after AK diagnosis; | N/A |
| Bouheraoua et al. (2013) [27] | 42/44 | Hexamidine 0.1% + PHMB 0.02%: 44 (100%); Oral itraconazole in severe cases: 6/44 (14%); CCT after 2 weeks starting AAT: (66%). | AMT: 8 (18%) PKP: 4 (9%) Evisceration: 2 (4%) |
| Carnt et al. (2018) [13] | 194/194 | PHMB 0.02%, 184 (95%); Adjunctive agents including CHX and propamidine. Corticosteroids pre-AAT: 56 (29%) | N/A |
| Chopra et al. (2020) [77] | 157/157 | N/A | N/A |
| Bonini et al. (2021) [78] | 35/40 | propamidine isethionate 0.1% and 0.02% PHMB: (100%) | N/A |
| Rahimi et al. (2014) [37] | 25/27 | PHMB 0.02%: 27 (100%) | N/A |
| Yamazoe et al. (2012) [79] | 34/35 Group 1: final VA of ≤0.10 logMar (22 eyes) Group 2: >0.10 logMar (13 eyes) | CHX 0.02% hourly, gradually tapered | Group 2: KP: 3 (23%) (2 PKP, 1 DALK) |
| Arnalich-Montiel et al. (2014) [80] | 17/17 | N/A | N/A |
| Park et al. (1997) [81] | 38/38 | CCT, 19 Non-CCT, 17 CCT before diagnosis, 9 | N/A |
| Landeo et al. (2015) [82] | 14/14 | PHMB 0.02% and Propamidine 0.1% | N/A |
| Sun et al. (2006) [83] | 20/20 | CHX 0.02% + Neomycin (0.5%) Itraconazole in severe cases, 15 (75%) | N/A |
| Article | No Patients/Eyes | Good Prognosis | Poor Prognosis |
|---|---|---|---|
| Pang et al. (2024) [40] | 109/109, results and outcomes were not available for 1 patient | T4C genotype (p = 0.040) | T4D genotype (p = 0.013) |
| List et al. (2021) [41] | 42/44 | N/A | Greater time until diagnosis (p = 0.004); CCT use (OR = 7.33, 0.22–4.15); Older age (OR = 1.06); Poor BCVA at initial presentation (OR = 9.59); Increased follow-up time (OR = 1.02); Duration of symptoms (OR = 1.50). |
| Megha et al. (2020) [38] | 11/11, 1 lost in follow-up | N/A | N/A |
| Jo et al. (2020) [42] | 16/19 | Early diagnosis of AK (p = 0.638) | N/A |
| Musayeva et al. (2020) [22] | 28/28, 2 lost in follow-up | N/A | N/A |
| Papa et al. (2020) [43] | 227/227 | N/A | N/A |
| Lin et al. (2018) [44] | 22/24 | N/A | Symptom onset to treatment (37.3 days, mean,) (p = 0.020); RGP lenses: worse initial BCVA (p = 0.02) but more improvement in vision (p = 0.01). |
| McKelvie et al. (2018) [45] | 52/58 | N/A | Empirical CCT: associated with diagnostic delay 47 days (range 15–154 days): worse final BCVA ranging from 0.60 to PL |
| Lim et al. (2008) [18] | 55/56, only 51 eyes were analyzed in the study | N/A | Delay in treatment (p = 0.07) Median delay (21 days): all eyes successfully treated Median delay (56 days): all eyes unsuccessfully treated |
| Wouters et al. (2022) [24] | 109/109 | N/A | CCT use prior to diagnosis (OR: 4.3 (95%CI (1.7–11.0)) (p = 0.002) |
| Thulasi et al. (2021) [23] | 15/15 | N/A | N/A |
| Rahimi et al. (2015) [26] | 31/31 | N/A | VA > 0.1: Symptoms duration ≥21 days before diagnosis (p = 0.165) CCT use before diagnosis (p = 0.29) First BCVA ≤0.3 logMar (p = 0.29) Corneal stromal involvement at diagnosis (p = 0.05) |
| Robaei et al. (2014) [25] | 174/174 | N/A | Older patients (≥60 years) (OR 8.97, 95% CI: 2.13–37.79) |
| Bagga et al. (2021) [33] | 23/23, only 18 patients completed the study | N/A | N/A |
| Azuara-Blanco et al. (1997) [46] | 10/10 | Early diagnosis (<4 weeks of symptoms); Adjunctive CCT with anti-amoebic coverage. | N/A |
| Duguid et al. (1997) [21] | 105/111 | Early diagnosis (<28 days, p = 0.005); effective combined therapy with PHMB and propamidine | Delayed diagnosis (>2 months, p < 0.05) Secondary glaucoma Bacterial co-infections |
| Hargrave et al. (1999) [34] | 83/87, only 60 eyes had their data analyzed for treatment efficacy and safety | Strict adherence to protocol; avoidance of premature surgical interventions. | N/A |
| Carnt et al. (2016) [47] | 196/196, only 129 included in the multivariable analysis | N/A | CCT use before AAT (OR = 3.85, p = 0.012); Stage 3 AK; (OR = 5.89; p = 0.032). Older age > 33 years (OR = 4.02, p = 0.007). |
| Höllhumer et al. (2020) [48] | 52/52 | N/A | Treatment >21 days: mean VA of 0.86 ± 0.98 (p = 0.2) Stage 3: p = 0.04 |
| Caruso et al. (2020) [35] | 29/29 | N/A | N/A |
| Dart et al. (2024) [36] | 135/135, 127 in the full-analysis subset; 134 in the safety analysis subset | N/A | N/A |
| Blaser et al. (2024) [49] | 52/59, 46 were treated | N/A | N/A |
| Tew et al. (2020) [50] | 107/107, 10 eyes with AK | N/A | Delay in diagnosis: eight out of 10 (80%) of whom six had previously received CCT (1 enucleation) |
| Chen et al. (2004) [51] | 108/108, 15/15 with AK | Early intervention with PKP when medical treatment fails; Smaller graft sizes had better outcomes (<8.5 mm) | Delayed diagnosis (>2 months); Poor contact lens hygiene; Scleral extension of infection. |
| Laurik et al. (2019) [52] | 23/23 | N/A | N/A |
| Liu et al. (2020) [53] | 62/62 | N/A | Presence of ring infiltrate (with versus without): Initial VA: 1.51 ± 0.17 versus 1.71 ± 0.1, p = 0.2; Final VA: 0.41 ± 0.1 versus 1.17 ± 0.2, p = 0.002; Presence of complications (glaucoma, recurrence, dilated pupil/iris atrophy, graft rejection and graft failure) (p = 0.012) |
| Kitzmann et al. (2009) [54] | 30/31 | N/A | N/A |
| Qi et al. (2024) [55] | 51/51 | N/A | N/A |
| Wang et al. (2023) [56] | 13/13 | N/A | N/A |
| Zhang et al. (2023) [57] | 58/59 with stage 3 AK requiring keratoplasty | N/A | CCT use before diagnosis (p = 0.040) and hypopyon (p = 0.009) were risk factors for recurrence after LK |
| Roozbahani et al. (2019) [58] | 63/63 | N/A | Therapy 25 days after symptoms (p = 0.041); Poorer presenting vision BCVA ≥ 1 logMAR unit (p = 0.002) |
| Sabatino et al. (2016) [59] | 11/11 | N/A | N/A |
| Robaei et al. (2015) [60] | 196/50 | N/A | Age > 70 (p = 0.070) |
| Bagga et al. (2020) [61] | 23/23, 10: Advanced AK (infiltrate ≥8 mm) | N/A | Advanced keratitis with infiltrate ≥8 mm, posterior stromal involvement |
| Thebpatiphat et al. (2007) [62] | 20/20 | Superficial Cases: dendritiform keratitis or radial keratoneuritis (BCVA better than 0.18 logMAR units at 3 months) p = 0.00008 Early diagnosis statistically significantly shorter in the group with superficial pathology (p = 0.03) | Stage 3 AK and BCVA less than finger counting; p = 0.00008 |
| Butler et al. (2005) [63] | 20/20 | N/A | Delayed diagnosis correlated to a higher recurrence (>1 month, p < 0.05); Poor contact lens hygiene |
| Chin et al. (2015) [64] | 13/15 | N/A | Delayed treatment (>30 days) (early (0.4 ± 0.9 logMAR units) vs. Late (1 ± 1.35 logMAR units); p = 0.125 CCT use before diagnosis (p = 0.367); |
| Alfonso-Muñoz et al. (2018) [65] | 10/10 Superficial stroma: 3/10 (30%) Deep stroma (ring infiltrates or corneal abscesses): 7/10 (70%) | N/A | Deep stromal disease: OR: 10.27 (IC 95%): 2.91–36.17 Time until diagnosis: Superficial group (19 days); Deep group (56 days); p < 0.05 |
| Kaiserman et al. (2012) [66] | 41/42 | Neuritis (p = 0.04) and pseudodendrites (p = 0.05) Good initial visual acuity (p = 0.002) Infections related to swimming (p = 0.01) Absence of an epithelial defect (p = 0.03) Having been treated with chlorhexidine (p = 0.05) Not having received CCT (p = 0.003) | Treated with topical CCT (p = 0.04) Epithelial defect on presentation (p = 0.0006) Longer-length of treatment (9.4 ± 3.7 months vs. 7.1± 2.9 months, p = 0.03) Neosporin® prolongs the time of treatment (p = 0.03) |
| Ikeda et al. (2012) [67] | 103/104, 28/29 with AK | N/A | Higher Acanthamoeba DNA copy numbers (OR per category, 3.48; 95% CI, 1.04 –111.63, p = 0.05) Advanced AK stage (OR:2.8 per stage increase (95% CI, 1.07–7.30, P0.05)) |
| Patel et al. (2010) [68] | 25/25, 1 lost in follow up | Early diagnosis of AK (<21 days) | Late diagnostic (>21 days): All surgical interventions occurred in this group (n = 6) Use CCT before diagnosis: 64% (9/14) were in the late diagnosis group |
| Shimmura-Tomita et al. (2018) [69] | 10/10 | N/A | Older age (p = 0.04) CCT use before diagnosis (100% (severe stage) vs. 67% (mild stage)) Keratoprecipitates (p = 0.01) |
| Zhang et al. (2014) [70] | 29/29 | N/A | Late-disease stage on presentation (deep stromal keratitis, ring infiltrate or extracorneal complications): OR 10.50 (95% CI (1.07–103.51) (p = 0.044) (p = 0.154) Deep location of cysts ≥ 250 µm: OR: 11.38 (95% CI (1.17–110.42) p = 0.036; (p = 0.215) Clusters or chains of cysts observed with IVCM: OR:14.86 (95%CI (1.53–144.2) p = 0.020 |
| Elmer et al. (2008) [39] | 65/72 | N/A | Deep stromal disease or ring infiltrate: OR: 10.27 (2.91–36.17); p < 0.001 Duration between symptom onset and UIC presentation (>3 weeks): OR:2.55 (0.83–7.88); p = 0.10 Continued post-diagnosis steroid use: OR: 17.00 (95% CI, 3.19–90.66) (p = 0.02) |
| Radford et al. (1998) [71] | 243/259 | Early diagnosis of AK (<30 days) (170 eyes) (p < 0.01) | Late diagnosis of AK (>30 days) (67 eyes) (p < 0.01) Non-CL wearers (18 patients): delayed diagnosis and poorer visual outcomes compared to CL wearers, with only 10/18 (56%) achieving ≤ 0.30 LogMAR units |
| Vilares-Morgado et al. (2024) [28] | 46/51 BCVA final < 1 logMAR group: 31 (60.8%) BCVA final ≥ 1 logMAR group: 20 (39.2%) | Early diagnosis (≤14 days after symptom onset): p = 0.004 (OR 19.78; 95% CI 2.07–189.11; p = 0.010) Epithelial debridment: (OR 19.02; 95% CI 3.27–110.57; p = 0.001) Better initial BCVA (0.8 ± 0.7 logMAR units vs. 1.3 ± 0.9 logMAR units; p = 0.047) | Late diagnosis (>14 days from symptom onset): BCVA > 1: 31 (54.8%); BCVA ≥ 1: 17 (94.4%) |
| Randag et al. (2019) [72] | 224/224 | N/A | CCT use before diagnosis increased failure: OR: 3.308 95%(1.375–7.963); Advanced disease stage (Stage 3): OR: 3.847 95%(1.544–9.584) Advanced age: OR 1.052 95% (1.029–1.075) |
| Bacon et al. (1993) [73] | 72/77, 4 lost to follow up | Early diagnosis (<1 month) (p < 0.001), smaller ulcer size at presentation, and absence of microbial co-infection | Late diagnosis (>2 months), glaucoma, microbial co-infections, resistant strains, prolonged steroid use prior to correct diagnosis. TPK in inflamed eyes: Graft survival probability at 61 months: inflamed = 35%, uninflamed = 69%; OR = 7.34, p < 0.001; |
| G D’Aversa et al. (1995) [74] | 12/14 | Early diagnosis (<1 month of symptoms, p < 0.05); Absence of corticosteroid use | Late diagnosis (>5 months, p < 0.01); Bacterial superinfections contributed to treatment failures. |
| Claerhout et al. (2004) [75] | 14/14 Early Treatment ≤18 days of symptom onset: 6/14 Late Treatment >18 days: 8/14 | Early treatment (<18 days) | Late treatment (>18 days): more extensive deep stromal involvement (p = 0.022) |
| Chew et al. (2011) [76] | 59/59 | N/A | Initial VA (>0.40 vs. ≤0.40): OR: 4.3 (0.9–21.7) Time to diagnosis (≥21 vs. <21 days); OR: 1.6 (0.2–10.5) Steroid use before diagnosis: OR: 3.7 (0.4–15.7) Age (>50 vs. ≤50), yrs: OR: 2.3 (0.3–15.7) Diagnostic method (confirmed tissue diagnosis vs. clinical diagnosis) OR: 4.5 (0.8–25.1) Stromal involvement: (CRUDE OR:12.3 (2.4–62.7)) (adjusted: not estimable) |
| Bouheraoua et al. (2013) [27] | 42/44 | N/A | Higher rates of need for surgery: Time from symptom onset to diagnosis of >30 days: OR: 4.6 (0.3–83.5); p = 0.003 Initial visual acuity of ≤20/200: p = 0.01 Infiltrate size of >3 mm; p =0.03 Preperforating infiltrate; OR: 4.4; p < 0.001 Corneal neovascularization; OR: 7.0 (0.6–84.6); p < 0.001 Age ≥ 50 y: p = 0.001 |
| Carnt et al. (2018) [13] | 194/194 | N/A | Presence of SIC (scleritis and/or a stromal ring infiltrate): Older age (>34 years): (OR: 2.36; 95% CI: 1.21–4.57; p = 0.011) Pre-diagnosis corticosteroid use: (OR: 2.56; 95% CI: 1.28–5.10; p = 0.008) Bad outcomes: Aged >34 years, OR: 2.52; 95% CI: 1.28–4.94; p = 0.007 Corticosteroids used before giving AAT (OR: 2.42; 95% CI: 1.17–5.03; p = 0.017) Symptom duration >37 days before AAT OR: 1.89; 95% CI: 0.91–3.90 Advanced disease stage (Stage 3, OR = 2.87, p = 0.010); |
| Chopra et al. (2020) [77] | 157/157 | BCVA < 0 (N = 75): No previous steroid therapy: OR (2.91; 1.00–8.10; p = 0.041) Clinical epithelial appearance (OR: 6.11; 2.32–16.07; p < 0.001) IVCM—ACD (number/mm2) (44.7 ± 40.1): OR:0.99; 0.98–0.99; p = 0.001 IVCM—morphologic features location (epithelium only): (OR: 14.22; 3.92–51.64; p < 0.001) | BCVA 0.18 to 0.78 (N = 55): Presence of corneal ring infiltrates and Severe stromal involvement. (OR: 3.30; 1.23–8.84; p = 0.02) IVCM—morphologic features location (Epithelium and stroma): (OR: 12.00; 3.22–44.74; p < 0.001) IVCM—Higher ACD (number/mm2) (48.2 ± 46.4): OR: 0.99; 0.98–0.99; p = 0.005 |
| Bonini et al. (2021) [78] | 35/40 | Diagnosed early (<30 days) Prompt Acanthamoeba therapy (<30 days) (p < 0.01) | Severe corneal ulcer (stage III) had a significantly longer healing time (16.2 ± 3.7 months) (p < 0.05) |
| Rahimi et al. (2014) [37] | 25/27 | N/A | Deep stromal keratitis or a ring infiltrate: (OR), 28.0; 95% CI, 3.3–240.8, p = 0.001 Initial BCVA >0.3 logMar: OR, 8.6; 95% CI, 1.2–59.8, p = 0.003 |
| Yamazoe et al. (2012) [79] | 34/35 Group 1: final VA of ≤ 0.10 logMar (22 eyes) Group 2: >0.10 logMar (13 eyes) | N/A | Group 2 (>0.10 logMar) Initial BCVA > 0.50 logMAR: OR 25.5, 95% CI 3.4–186.7, p = 0.01 Diagnosis > 1 month: OR 1.03, 95% CI 1.00–1.06, p = 0.04 Presence of ring infiltrate: OR 33.6, 95% confidence interval (CI) 3.4–333.9, p = 0.01) |
| Arnalich-Montiel et al. (2014) [80] | 17/17 | N/A | Non-T4 genotype |
| Park et al. (1997) [81] | 38/38 | Early diagnosis (<1 month) Medical cure, p = 0.02 BCVA ≤ 0.48, p < 0.01 | Late diagnosis (≥1 month) |
| Landeo et al. (2015) [82] | 14/14 | Early treatment (<30 days) | Late treatment (≥30 days) Higher duration of therapy (p = 0.0045) Poorer final BCVA (p = 0.0125) |
| Sun et al. (2006) [83] | 20/20 | N/A | N/A |
| Article | No Patients/ Eyes | Good Oucome | Poor Outcome | Initial BCVA (logMAR Units) (Mean) | Final BCVA (logMAR Units) (Mean) | Improvement BCVA |
|---|---|---|---|---|---|---|
| Pang et al. (2024) [40] | 109/109, results and outcomes were not available for 1 patient | 22 (20%) | Corneal perforation, need for PKP, treatment >8 Months, BCVA ≥ 0.6 logMar, 86 (80%) | N/A | N/A | N/A |
| List et al. (2021) [41] | 42/44 | N/A | BCVA: ≥0.4 logMAR (54.5%), Need for KP (22.7%) | 0.99 ± 0.73 | 0.56 ± 0.72 | 0.39 ± 0.68, p = 0.001 |
| Megha et al. (2020) [38] | 11/11, 1 lost in follow-up | Ulcers healed with vascularized corneal opacity (63.6%) | Need for KP (corneal perforation), 3 (27%) | ≤0.60: 4 (40%) CF: 2 (20%) HM: 1 (10%) | 0–1: 4 (40%) LP-HM: 3 (30%) | N/A |
| Jo et al. (2020) [42] | 16/19 | N/A | PHMB 0.02% + CHX 0.02%: Corneal toxicity in 2 /5 (40%) | 0.78 ± 0.37 | 0.076 ± 0.07 | PHMB: 0.89 ± 0.47 (p = 0.007) CHX: 0.59 ± 0.35 (p = 0.048) PHMB + CHX: 0.50 ± 0.22 (p = 0.042) Without statistically significant difference between groups. |
| Musayeva et al. (2020) [22] | 28/28, 2 lost in follow-up | Medical cure (100%) | Need for KP (corneal scarring) (19.2%); Recurrence (repeated occurrence of symptoms and/or clinical signs of AK during or within 3 months after cessation of therapy); Stinging or burning sensation of the eye after application of the drops in 5 of 26 patients (19.2%) | 1.02 ± 0.913 logMAR Stage I: 0.650 ± 0.354 Stage II: 0.843 ± 0.667 Stage III: 1.33 ± 0.974 | 0.504 ± 0.859 Stage I: 0.100 ± 0.141 Stage II: 0.286 ± 0.513 Stage III: 0.890 ± 1.07 | p = 0.0004 Stage II: p = 0.028 Stage III: p = 0.1139 |
| Papa et al. (2020) [43] | 227/227 | Medical cure:138 (60.79%) No statistical difference among AAT (p = 0.528) | Need to switch therapy: Diamidine monotherapy: 88% (22/25) PHMB + Diamidine: 24.6% (28/114) PHMB monotherapy: 48% (24/50) Others 52.6% (20/38) VA ≥ 0.6 logMar and/or need for surgery—112/227 (49.3%) (p > 0.155) | N/A | N/A | Severe vision loss ≥1.30 logMar: PHMB monotherapy: 11/50 (22%) PHMB + diamidine: 31/114 (27.19%) Diamidine monotherapy: 4/25 (16%) Others: 10/38 (26.32) |
| Lin et al. (2018) [44] | 22/24 | Cure: 20 (83.3%) | Need for PK: 4 (16.7%) | <0.18: 2 (8.3%) 0.18–1: 14 (58.3%) >1: 8 (33.3%) | >20/30: 17 (70.8%) 20/30–20/200: 4 (16.7%) <20/200: 3 (12.5%) | N/A |
| McKelvie et al. (2018) [45] | 52/58 | N/A | 4 (with delayed diagnosis): 3 OPK; 1 TPK with posterior enucleation (perforated cornea) | N/A | N/A | Improvement: 74% Unchanged: 9% Worsened: 7% |
| Lim et al. (2008) [18] | 55/56, only 51 eyes completed the study | N/A | Treatment success: PHMB 0.02%: 18 (78.3%) CHX 0.02%: 24 (85.7%) (p = 0.49) | Need for KP: PHMB 3/23 (13%) CHX 2/28 (7%) (p = 0.65) Corneal scarring (p = 0.29) | N/A | N/A |
| Wouters et al. (2022) [24] | 109/109 | N/A | Emergency corneal grafting: No CCT: 7/53 (13%); CCT: 20/56 (36%) (p = 0.0078) >1 surgery: No CCT: 9/53 (17%); CCT:22/56 (36%) (p = <0.0001) Diagnostic delay: No CCT: 23 ± 39 (range 7–303) days; CCT:62 ± 62 (range 0–295) days (p = <0.001) Higher disease severity stage with CCT use (p < 0.001) | N/A | <0.6 LogMar: No CCT:44(83%); CCT:35(63%) ≥0.6 LogMar: No CCT:7/53 (13%); CCT:17/56 (30%); (p = 0.03) Adjusted OR: CCT prior to AAT = 4.3 (95%CI (1.7–11.0)) (p = 0.002) | N/A |
| Thulasi et al. (2021) [23] | 15/15 | Clinical cure: 14 (93%) | GI disturbance: 7/15 (47%) Elevated liver functions: 2/15 (13%) Inflammatory response: 11/15 (73.3%) (10 improving with CCT) Surgery needed: 5/15 (33%) (1 enucleation (epithelial down growth)) Recurrence of AK and need more cycles of miltefosine: 6/15 (40%) | N/A | <0.6 logMar: 9 (60%) 1.4 logMar: 1(6.7%) HM: 2(13%) LP: 1(6.7%) No LP: 1 (6.7%) | N/A |
| Rahimi et al. (2015) [26] | 31/31 | Improvement in signs and symptoms: 26 (83.9%) | Need for adding another anti-AK agent: 4 (12.9%) Corneal scar: 8 (25.8%) Required OPK: 3 (9.7%) | <0.5: 22 (71%) ≥0.5: 9 (29.0%) | ≥0.80: 22 (71%) <0.80: 9 (29%) | Better: 29/31 (93.5%) Same: 1/31 (3.22) Worse: 1/31 (3.22) |
| Robaei et al. (2014) [25] | 174/174 | N/A | Symptom duration (days) (Median (IQR): CCT: 37 (23–72.5); Not-CCT: 14 (7–28); p < 0.001 Scleritis, n (%): CCT: 44 (50.57%); Not-CCT: 16 (18.39%); p < 0.001 KP, n (%): CCT: 37 (42.53%); Not-CCT: 8 (9.20%); p < 0.001 Stage 3 AK: CCT: 31.8% vs. Not CCT: 15.5%, p = 0.037 | N/A | N/A | CCT group: (Final Visual Acuity ≥0.6 logMar or Corneal Perforation or Need for Keratoplasty) OR: 3.90 (1.78–8.55); p = 0.001 |
| Bagga et al. (2021) [33] | 23/23, only 18 patients completed the study | Complete resolution: BG (40%); VZ (50%) Ulcer size BG group: 5.7 (5.3–6.5) to 1 mm (IQR, 0–4.3 mm) (p = 0.02) VZ group: 4.5 (1.8–5.1) to 0.7 mm (IQR, 0–1.6 mm) (p < 0.05) | Worsened keratitis: BG (30%); VZ (12.5%); | BG group: 1.79 (IQR, 1.48–2.78) VZ group: 1.60 (IQR, 1.00–2.78) | BG group: 1.10 (IQR, 0.48–1.79) VZ group: 0.80 (IQR, 0.48–1.30) | BG group: p = 0.02 VZ group: p = 0.18 |
| Azuara-Blanco et al. (1997) [46] | 10/10 | N/A | N/A | From 0 to HM | ≤0.3 logMar: 8/10 (80%) CF: 2 /10 (20%) | Improved in 100% |
| Duguid et al. (1997) [21] | 105/111 | N/A | Need for OKP: 10 (9%); Clinical relapses (tapering therapy): 19 (17%) Treatment toxicity (26.1%) (Propamidine—superficial punctate keratopathy) Glaucoma: 4 (3.6%) leading to 2 enucleations | From 0.30 to 2.30 logmar | ≤0.30: 88(79.3%) ≥0.78: 18 (16.2%); included central scarring (52.2%), bacterial superinfection (30.4%), and recurrent disease (26.1%). | N/A |
| Hargrave et al. (1999) [34] | 83/87, only 60 eyes had data analyzed for treatment efficacy and safety | Successful treatment without recurrence of infection after cessation of therapy 50 (83%) | PK: 17 (28%) Enucleation: 7/17 (41%) (due to incomplete eradication of infection prior to surgery) (p < 0.001). Treatment failure; exacerbations occurred during maintenance therapy, indicating quantitative inadequacy: 10 (17%) Propamidine-related toxicity included superficial punctate keratopathy 3/60 (3%): discontinued therapy due to severe burning on drop instillation. | N/A | N/A | Improved 83% of eyes evaluated |
| Carnt et al. (2016) [47] | 196/196, only 129 included in the multivariable analysis | CCT use post-AAT and visual acuity ≥0.6, corneal perforation, or need for keratoplasty: OR: 1.08 (0.387–3.03); p = 0.881 | CCT before diagnosis: 32 (25%) suboptimal outcomes | ≥1 | ≤0.30 in 75% | N/A |
| Höllhumer et al. (2020) [48] | 52/52 | Voriconazole: Decreased the duration of AAT from the average of 12–9 months | Corneal scarring and vascularization, 32 (62%) Recurrence: 3 (5.8%) Need for surgery: 4 (7.7%) (1 TPK; 2 OPK; 1 DALK) | 1.02 [0,4] | 0.57 [−0.10 to 4.0] Stage 1: −0.03 ± 0.05 Stage 2: 0.50 ± 0.82 Stage 3: 1.32 ± 1.69, (p = 0.04). | 27/52 (52%) |
| Caruso et al. (2020) [35] | 29/29 | 18 (62%) ≤ 0.69 logMAR 15 (52%) ≤ 0.5 logMAR - Ocular inflammation improved at 2 weeks: 14 (48%) | 10% (3/29) worsened to LP or lower Scarring, 24% (7/29) 1 (PKP or AMT) | 1.76 ± 0.47. | 0.77 ± 0.48 at 3 months | Significantly at 2 weeks, stable at 3 months (0.77 logMAR units) |
| Dart et al. (2024) [36] | 135/135, 127 full-analysis subset; 134 in the safety analysis subset | Medical cure rate at 12 months: PHMB 0.02% + Propamidine, 86.6% PHMB 0.08%, 86.7% (p = 0.980) | Need for TPK PHMB 0.02+: 3/61 PHMB 0.08%: 5/66 Treatment failures: PHMB 0.02: 7 (11.5%) PHMB 0.08%: 10 (15.2%) Severe eye pain: 3 cases (2 in PHMB 0.02%, 1 in PHMB 0.08%) | N/A | Not statistically significant difference | N/A |
| Blaser et al. (2024) [49] | 52/59, 46 were treated | Treatment success rate without KP: 97.8% | 1: emergent PK due to conservative treatment failure | N/A | N/A | N/A |
| Tew et al. (2020) [50] | 107/107, 10 AK eyes | Graft clarity 1 y post-op: 5 (50%) AK Cure: 9 (90%) Anatomical success rate: 9 (90%) | N/A | N/A | N/A | N/A |
| Chen et al. (2004) [51] | 108/108, 15/15 with AK | Cure: 13 (86.7%) | Recurrence: 2(13.3%) Enucleation (scleral extension): 1 (6.67%) | 0.54–1.30: 1(6.7%) 1.30: 14(93.3%) | 0–0.48: 7 (63.6%) 0.54–1.30: 1 (9.1%) 1.30: 3 (27.3%) | Significant visual recovery observed in cases with clear grafts and no recurrence. |
| Laurik et al. (2019) [52] | 23/23 | Graft survival at 36 months: 78% (18/23) Early PK: 90% Late PK: 44% p = 0.167 | Glaucoma p = 0.34 Cataract p = 0.16 Anterior synechiae p = 0.13 | Early PK: 1.67 Late PK: 1.78 p = 0.418 | Early PK: 0.32 Late PK: 1.28 p = 0.015 | N/A |
| Liu et al. (2020) [53] | 62/62 | Medical cure: 52.4% | Post-op complications: TPK 82.4%; OPK 40%, p = 0.04 Glaucoma (p = 0.04): 58.8% TPK vs. 30% OPK; Recurrence: 2 eyes in TPK group | OPK: 1.57 ± 0.2 TPK: 1.79 ± 0.1 p = 0.52 | OPK: 0.76 ± 0.2 TPK: 1.11 ± 0.2 p = 0.29 | N/A |
| Kitzmann et al. (2009) [54] | 30/31 | Microbiological cure (>3 months without infection); Graft survival (TPK: 45.5% (1 y), 37.5% (10 y); OPK: 100% (1 y), 66.7% (10 y)) | Repeated KP: 8 (in TPK group); Complications: corneal thinning, hypopyon (TPK), peripheral neovascularization (OPK) | No statistical difference between groups | Group OPK: 0.1 Group TKP: 0.30 Less likely to obtain visual acuity of 0.3 logMar or better (p 0.07); | N/A |
| Qi et al. (2024) [55] | 51/51 | Graft survival (DALK: 89.5%; PKP: 61.1%); (p = 0.046) Endothelial cell loss: DALK (1899 ± 125); PKP (1608 ± 231) (p = 0.032) | Autoimmune rejection of graft: PKP (20.8%) Recurrence (p = 1.000) | DALK: 1.95 ± 0.61 PKP: 2.93 ± 0.39 p = 0.039 | At 1 Year: BB-DALK: 0.71 ± 0.59, PKP: 0.79 ± 0.66, p = 0.144 At 3 Years: BB-DALK: 0.71 ± 0.64, PKP: 0.93 ± 0.76, p = 0.010 | N/A |
| Wang et al. (2023) [56] | 13/13 | Graft survival: 92.3% | Intraoperative Descemet membrane perforation: 1 (7.7%) Graft Rejection: 1 (7.7%) Recurrence: 1 (7.7%) | Ranged from HM to 1.7 | 0.35 ± 0.27 | N/A |
| Zhang et al. (2023) [57] | 58/59 with stage 3 AK requiring keratoplasty | Successful treatment: PKP 91.7%; LK 91.3% | Graft rejection: PKP: 8 (22.2%); LK: 0; p = 0.044 Graft epitelial deffects: PKP: 3(8.3%); LK: 0 Graft autolysis: PKP: 1(2.8%); LK:0 Secondary glaucoma: PKP: 3(8.3%); LK: 1(4.3%) Graft infection: PKP: 0; LK:1(4.3%) Recurrence: PKP: 6(16.7%); LK: 4(17.4%); p = 0.604 | CF: PKP:16(44.4%); LK:18(78.3%); p = 0.016 HM: PKP:18(50.0%); LK: 4(17.4%) LP: PKP: 2(5.6%); LK:1(4.3%) | ≤0.48: PKP: 14(38.9%); LK: 15(65.2%); p = 0.032 1–0.48: PKP: 12(33.3%); LK: 6(26.1%) >1: PKP:10(27.8%); LK:2(8.7%) | N/A |
| Roozbahani et al. (2019) [58] | 63/63 | N/A | TPK complications: graft failure (75%), cataract (50%), uncontrolled glaucoma requiring surgery (17%); recurrence, 8% | TPK: 2.55 ± 1.12; Medical: 0.82 ± 0.79 | TPK: 1.83 ± 1.16; Medical: 0.43 ± 0.62 | N/A |
| Sabatino et al. (2016) [59] | 11/11 | Recurrence: 0%; Endothelial cell density at 12 months: 2064 ± 443 cells/mm²; Graft rejection: 0% | Membrane rupture: 1 (9%) | Range HM to 0.5 | 0.84 ± 0.14 | p < 0.1 |
| Robaei et al. (2015) [60] | 196/50 | N/A | Need other eye surgery, n (%): TPK: 23 (88.5%); OPK: 14 (58.3%) Need multiple eye surgery, n (%): TKP: 7 (1 because of recurrence); OPK: 3 (none because of recurrence) | N/A | ≤0.18: TPK: 54.2%, OPK: 26.5%; >1: TPK: 8.3%, OPK: 53.9% | TPK and Final VA >1 logMAR unit (OR: 12.78 (2.05 ± 79.72); p = 0.006) |
| Bagga et al. (2020) [61] | 23/23, 10: Advanced AK (infiltrate ≥8 mm) | 1 year graft survival: advanced AK: 32%; less severe: 91.6% | Graft Failure: Advanced AK (60%); less severe AK (15.4%); (OR: 8.25; p = 0.04) Complications in advanced AK: Descemet’s membrane detachment in 5/10 (50%); persistent epithelial defect in 3/10 (30%) Recurrence: Advanced AK: 2 cases (20%) Less severe AK: 1 case (7.7%) | Median: 2.78 (IQR, 1.79–3.0); | Median: 1.79 (IQR, 0.70–2.78) | Statistically significant improvement in BCVA for clear grafts; failure cases showed minimal improvement |
| Thebpatiphat et al. (2007) [62] | 20/20 | N/A | N/A | N/A | N/A | N/A |
| Butler et al. (2005) [63] | 20/20 | N/A | Complications: 16 (80%): corneal scarring (40%), recurrent disease (25%), cataract (15%), resistant disease requiring penetrating keratoplasty (10%), perforation (5%), bullous keratopathy (5%), and scleritis (5%) Need for PK: 7 (35%) | Ranged from 1 to CF | ≤0.30: 75% ≥0.78: 5% | 75% achieved 0.30 or better at last follow up Improvement in 90% (18 eyes) of cases; Worsened in two eyes (10%) |
| Chin et al. (2015) [64] | 13/15 | N/A | Treatment time: CCT group (162 ± 50.89 days) vs. non-CCT group (94 ± 45.24 days) (p = 0.012) | CCT group: 1.78 ± 0.60 Non CCT group: 0.62 ± 0.69 | CCT group: 0.87 ± 1.23(−0.1 to 3) Non CCT group: −0.03 ± 0.49 (−1 to 0) p = 0.367 | N/A |
| Alfonso-Muñoz et al. (2018) [65] | 10/10 Superficial stroma: 3/10 (30%) Deep stroma (ring infiltrates or corneal abscesses): 7/10 (70%) | Medical cure: 3/3 (100% in superficial stroma group) CCT after 53 days of AAT improved symptoms | KP: 6/7 (86%) (in the deep stroma group) (perforation risk or ocular spreading) | HM: 4/10 (40%) CF: 1/10 (10%) 0.16–0.2: 3/10 (30%) | 0.25–1 | Visual acuity improved in all cases after treatment |
| Kaiserman et al. (2012) [66] | 41/42 | N/A | N/A | 1.2 ± 0.6 | 0.87 ± 0.94 | N/A |
| Ikeda et al. (2012) [67] | 103/104, 28/29 with AK | N/A | Poor outcome defined: visual acuity ≥0.40 logMar at the last visit or a requirement of keratoplasty | N/A | N/A | N/A |
| Patel et al. (2010) [68] | 25/25, 1 lost in follow up | N/A | N/A | N/A | Early diagnostic group (<21 days): 0.30 Late diagnostic group (>21 days): 0.90 | N/A |
| Shimmura-Tomita et al. (2018) [69] | 10/10 | N/A | Severe group: 1 TPK; 3 with poor visual acuity (<0.2) at the last visit: 4 (40%) Mild Group: 6 good prognosis with final BCVA of 1.2: 6 (60%) | N/A | Mild Group: Full recovery (BCVA 1.2) in all cases | N/A |
| Zhang et al. (2014) [70] | 29/29 | N/A | Defined as the need for TPK | N/A | N/A | N/A |
| Elmer et al. (2008) [39] | 65/72 | Control: ≤0.1 logMAR | Case: ≥0.1 logMAR or PKP | N/A | N/A | N/A |
| Radford et al. (1998) [71] | 243/259 | N/A | N/A | N/A | ≤0.30: Propamidine + PHMB: 99 (92%) Propamidine + Neomicine + PHMB: 21 (70%) Propamidina + Clorexidina:15 (100%) | N/A |
| Vilares-Morgado et al. (2024) [28] | 46/51 BCVA final < 1 logMAR group: 31 (60.8%) BCVA final ≥ 1 logMAR group: 20 (39.2%) | BCVA final < 1 logMAR: 31 (60.8%) | BCVA final ≥ 1 logMAR: 20 (39.2%) 12 eyes (23.5%) undergoing evisceration/enucleation | Baseline BCVA: Group BCVA < 1: 0.8 ± 0.7 (n = 26 eyes); Group BCVA ≥1: 1.3 ± 0.9 (n = 12); p = 0.047 | N/A | N/A |
| Randag et al. (2019) [72] | 224/224 | ≤0.3 logMAR: 137 (61.2%) | Treatment failures (>0.30 logMAR and/or need for KP): 87 (38.8%) | N/A | >0.3: 56 (25%) | N/A |
| Bacon et al. (1993) [73] | 72/77, 4 lost to follow up | ≤0.3 logMAR units:58(79%) Recurrence caused graft failure in 9 of 21 inflamed cases | >0.48 logMAR units: 15 (21%) | N/A | N/A | Statistically significant improvement observed in 79% of cases, especially in early-diagnosed cases (p < 0.001) |
| G D’Aversa et al. (1995) [74] | 12/14 | Medical Cure: 11 (79%) | 2 (15%) had BCVA CF or worse, including 1 loss due to bacterial superinfection. | ≥1 | ≤0.40: 12 (85%) ≤1: 6(43%) 0.40 to 0.18: 6 (43%) CF or worse: 2 (14%) | N/A |
| Claerhout et al. (2004) [75] | 14/14 | N/A | Need for KP: Early group: 1/6 (17%) (for corneal necrosis) Late group:5/8 (62.5%): 2 TPK; 3 OPK | Worse in late group (p = 0.022) | Early group (<18 d): 5/6 (83%): ≤1 Late group (>18 days): 3 (37.5%): ≥1 | N/A |
| Chew et al. (2011) [76] | 59/59 | ≤0.1 logMAR: 45% ≤0.7 logMAR: 69% | PKP: 13 (22%) >0.7 logMAR: 16 (31%) | Ranged from 0 to 1.68 [mean: 0.68; SD = 0.54] | N/A | Improvement in BCVA in 69% of patients |
| Bouheraoua et al. (2013) [27] | 42/44 | Medical cure: 34(77%) | Need for surgery | 1.24 | Not surgical: 0.38: (n = 34) Surgical: 1.93: (n = 10) (p < 0.0001) | Improvement in 77% |
| Carnt et al. (2018) [13] | 194/194 | Better outcomes in early diagnosis and non-SIC cases: 101 (52%) | Final VA ≥ 0.60, and/or corneal perforation and/or KP and/or other ocular surgery, except biopsy, and/or duration of AAT ≥ 10.5 months: 93 (48%) | N/A | N/A | N/A |
| Chopra et al. (2020) [77] | 157/157 | N/A | N/A | N/A | N/A | N/A |
| Bonini et al. (2021) [78] | 35/40 | Diagnosed early (<30 days) had faster healing (7 months) and better visual outcomes | Diagnosed late (>30 days): prolonged healing (16.2 months for stage III) and higher surgery rates (41%). | N/A | N/A | Significant improvement in early-diagnosed cases; poor outcomes in advanced-stage cases despite treatment. |
| Rahimi et al. (2014) [37] | 25/27 | N/A | KP: 5 (18.5%) | ≤0.10: 4 (15%) 0.50 to 0.10: 11 (40%) ≥0.50: 12 (45%) | ≤0.10: 18 (66.7%) >0.10: 9 (33.3%) | 77.8%: improved 14.8%: worsened |
| Yamazoe et al. (2012) [79] | 34/35 Group 1: final VA of ≤ 0.10 logMar (22 eyes) Group 2: >0.10 logMar (13 eyes) | N/A | N/A | (Mean ±SD) Group 1: 0.47 ± 0.42 Group 2: 1.59 ± 0.79 | Group 1: ≤0.10 Group 2: >0.10 | N/A |
| Arnalich-Montiel et al. (2014) [80] | 17/17 | N/A | N/A | N/A | T4 genotype group: ≤0.10 Non-T4 genotype group: >0.10 | T4 genotype: no significant improvement; severe vision loss in all cases Non-T4 genotype: all cases improved to functional vision |
| Park et al. (1997) [81] | 38/38 | Medical cure CCT, 14 (73.3%); p = 0.58 Non-CCT, 13 (76.5%) CCT before diagnosis, 7 (77.8%); p = 0.67 | TPK Non-CCT, 4 (23.5%) CCT, 5 (26.3%), p = 0.26 CCT before diagnosis, 2 (22.2%), p = (0.21) TPK (n = 15): Graft survival 2 y Uninflamed, 100% Inflamed, 43% Recurrence, 4 | N/A | ≤0.48 Non-CCT vs.: CCT, p = 0.26 CCT before diagnosis, p = 0.30 | N/A |
| Landeo et al. (2015) [82] | 14/14 | N/A | Higher duration of treatment in late treatment cases (10 months vs. 6 months, p = 0.0045) | Early treatment group: 0.30 to 0.70 Late treatment group: 0.48 to CF | Early treatment group: 0.30 Late treatment group: 1.30 p = 0.0125 | N/A |
| Sun et al. (2006) [83] | 20/20 | N/A | N/A | N/A | ≤0.70 in 7 eyes | N/A |
3.3. Risk of Bias in Studies
3.4. Medical Therapy
3.4.1. Amebicides
3.4.2. Antifungals
3.4.3. Corticosteroids
3.4.4. Antiparasitics
3.4.5. Other Therapies
3.5. Surgical Therapy
3.5.1. Therapeutic Epithelial Debridment (TED)
3.5.2. Therapeutic or Tectonic Penetrating Keratoplasty (TPK)
3.5.3. Optical Penetrating Keratoplasty (OPK)
3.5.4. Deep Anterior Lamellar Keratoplasty (DALK)
3.6. Prognosis Factors
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AK | Acanthamoeba keratitis |
| BCVA | Best corrected visual acuity |
| ICVM | In vivo confocal microscopy |
| AAT | Anti-amoebic therapy |
| PHMB | Polyhexamethylene biguanide |
| CHX | Chlorexidine |
| CCT | Corticosteroids |
| TED | Therapeutic epithelial debridement |
| TPK | Therapeutic penetrating keratoplasty |
| OPK | Optical Penetrating Keratoplasty |
| DALK | Deep Anterior Lamellar Keratoplasty |
References
- Anita Raghavan, R.R. Acanthamoeba Keratitis - A Review. Indian J Ophthalmo 2024, 72, 473–482. [Google Scholar] [CrossRef]
- Roozbahani, M.; Hammersmith, K.M.; Rapuano, C.J.; Nagra, P.K.; Zhang, Q.; Siu, S.Y. Acanthamoeba Keratitis: Are Recent Cases More Severe? Cornea 2018, 37, 1381–1387. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Xu, X.; Wei, Z.; Cao, K.; Zhang, Z.; Liang, Q. The Global Epidemiology and Clinical Diagnosis of Acanthamoeba Keratitis. J. Infect. Public Health 2023, 16, 841–852. [Google Scholar] [CrossRef] [PubMed]
- Zhao, G.; Sun, S.; Zhao, J.; Xie, L. Genotyping of Acanthamoeba Isolates and Clinical Characteristics of Patients with Acanthamoeba Keratitis in China. J. Med. Microbiol. 2010, 59, 462–466. [Google Scholar] [CrossRef]
- Booton, G.C.; Visvesvara, G.S.; Byers, T.J.; Kelly, D.J.; Fuerst, P.A. Identification and Distribution of Acanthamoeba Species Genotypes Associated with Nonkeratitis Infections. J. Clin. Microbiol. 2005, 43, 1689–1693. [Google Scholar] [CrossRef]
- Carnt, N.; Minassian, D.C.; Dart, J.K.G. Acanthamoeba Keratitis Risk Factors for Daily Wear Contact Lens Users: A Case–Control Study. Ophthalmology 2023, 130, 48–55. [Google Scholar] [CrossRef]
- Sakr, S.I.; Nayel, A.A.; Khattab, A.L.; Elhamamsy, W.M.; Abozaid, I.A.; Awad, R.; Elkazaz, H.A.K.; Habeel, C.S.; Samaha, R.; Ghaith, A.A. Impact of Contact Lens Hygiene Risk Factors on the Prevalence of Contact Lens-Related Keratitis in Alexandria-Egypt. J. Ophthalmic Inflamm. Infect. 2024, 14, 1–10. [Google Scholar] [CrossRef]
- Scruggs, B.A.; Quist, T.S.; Zimmerman, M.B.; Salinas, J.L.; Greiner, M.A. Risk Factors, Management, and Outcomes of Acanthamoeba Keratitis: A Retrospective Analysis of 110 Cases. Am. J. Ophthalmol. Case Reports 2022, 25, 101372. [Google Scholar] [CrossRef]
- Roth, M.; Balasiu, A.; Daas, L.; Holtmann, C.; Servera, A.; Walckling, M.; MacKenzie, C.R.; Fuchsluger, T.A.; Geerling, G. Impact of Implementation of Polymerase Chain Reaction on Diagnosis, Treatment, and Clinical Course of Acanthamoeba Keratitis. Graefe’s Arch. Clin. Exp. Ophthalmol. 2023, 261, 1951–1959. [Google Scholar] [CrossRef]
- Garg, D.; Daigavane, S. A Comprehensive Review on Acanthamoeba Keratitis: An Overview of Epidemiology, Risk Factors, and Therapeutic Strategies. Cureus 2024, 16, e67803. [Google Scholar] [CrossRef]
- Szentmáry, N.; Daas, L.; Shi, L.; Laurik, K.L.; Lepper, S.; Milioti, G.; Seitz, B. Acanthamoeba Keratitis – Clinical Signs, Differential Diagnosis and Treatment. J. Curr. Ophthalmol. 2019, 31, 16–23. [Google Scholar] [CrossRef] [PubMed]
- Clarke, B.; Sinha, A.; Parmar, D.N.; Sykakis, E. Advances in the Diagnosis and Treatment of Acanthamoeba Keratitis. J. Ophthalmol. 2012, 2012, 484892. [Google Scholar] [CrossRef] [PubMed]
- Carnt, N.; Robaei, D.; Minassian, D.C.; Dart, J.K.G. Acanthamoeba Keratitis in 194 Patients: Risk Factors for Bad Outcomes and Severe Inflammatory Complications. Br. J. Ophthalmol. 2018, 102, 1431–1435. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.J.; Alipour, F.; Cruzat, A.; Posarelli, M.; Zheng, L.; Hamrah, P. Utility of In Vivo Confocal Microscopy in Diagnosis of Acanthamoeba Keratitis: A Comparison of Patient Outcomes. Cornea 2023, 42, 135–140. [Google Scholar] [CrossRef]
- Goh, J.W.Y.; Harrison, R.; Hau, S.; Alexander, C.L.; Tole, D.M.; Avadhanam, V.S. Comparison of in Vivo Confocal Microscopy, PCR and Culture of Corneal Scrapes in the Diagnosis of Acanthamoeba Keratitis. Cornea 2018, 37, 480–485. [Google Scholar] [CrossRef]
- Padzik, M.; Szaflik, J.P.; Baltaza, W.; Perkowski, K.; Dybicz, M.; Chomicz, L. In Vivo Confocal Microscopy and in Vitro Culture Techniques as Tools for Evaluation of Severe Acanthamoeba Keratitis Incidents. Ann. Parasitol. 2017, 63, 341–346. [Google Scholar] [PubMed]
- Lorenzo-Morales, J.; Khan, N.A.; Walochnik, J. An Update on Acanthamoeba Keratitis: Diagnosis, Pathogenesis and Treatment. Parasite 2015, 22, 10. [Google Scholar] [CrossRef]
- Lim, N.; Goh, D.; Bunce, C.; Xing, W.; Fraenkel, G.; Poole, T.R.G.; Ficker, L. Comparison of Polyhexamethylene Biguanide and Chlorhexidine as Monotherapy Agents in the Treatment of Acanthamoeba Keratitis. Am. J. Ophthalmol. 2008, 145, 130–135. [Google Scholar] [CrossRef]
- Büchele, M.L.C.; Nunes, B.F.; Filippin-Monteiro, F.B.; Caumo, K.S. Diagnosis and Treatment of Acanthamoeba Keratitis: A Scoping Review Demonstrating Unfavorable Outcomes. Contact Lens Anterior Eye 2023, 46, 101844. [Google Scholar] [CrossRef]
- Niro, A.; Pignatelli, F.; Fallico, M.; Sborgia, A.; Passidomo, F.; Gigliola, S.; Nacucchi, A.; Sborgia, G.; Boscia, G.; Alessio, G.; et al. Polyhexamethylene Biguanide Hydrochloride (PHMB)-Properties and Application of an Antiseptic Agent. A Narrative Review. Eur. J. Ophthalmol. 2023, 33, 655–666. [Google Scholar] [CrossRef]
- Duguid, I.G.M.; Dart, J.K.G.; Morlet, N.; Allan, B.D.S.; Matheson, M.; Ficker, L.; Tuft, S. Outcome of Acanthamoeba Keratitis Treated with Polyhexamethyl Biguanide and Propamidine. Ophthalmology 1997, 104, 1587–1592. [Google Scholar] [CrossRef] [PubMed]
- Musayeva, A.; Riedl, J.C.; Schuster, A.K.; Wasielica-Poslednik, J.; Pfeiffer, N.; Gericke, A. Topical Voriconazole as Supplemental Treatment for Acanthamoeba Keratitis. Cornea 2020, 39, 986–990. [Google Scholar] [CrossRef] [PubMed]
- Thulasi, P.; Saeed, H.N.; Rapuano, C.J.; Hou, J.H.; Appenheimer, A.B.; Chodosh, J.; Kang, J.J.; Morrill, A.M.; Vyas, N.; Zegans, M.E.; et al. Oral Miltefosine as Salvage Therapy for Refractory Acanthamoeba Keratitis. Am. J. Ophthalmol. 2021, 223, 75–82. [Google Scholar] [CrossRef] [PubMed]
- Wouters, K.A.; Verhoekx, J.S.N.; van Rooij, J.; Wubbels, R.; van Goor, A.T. Topical Corticosteroids in Acanthamoeba Keratitis: Friend or Foe? Eur. J. Ophthalmol. 2022, 32, 170–175. [Google Scholar] [CrossRef]
- Robaei, D.; Carnt, N.; Minassian, D.C.; Dart, J.K.G. The Impact of Topical Corticosteroid Use before Diagnosis on the Outcome of Acanthamoeba Keratitis. Ophthalmology 2014, 121, 1383–1388. [Google Scholar] [CrossRef]
- Rahimi, F.; Hashemian, S.M.N.; Tafti, M.F.; Mehjerdi, M.Z.; Safizadeh, M.S.; Pour, E.K.; Sefidan, B.B. Chlorhexidine Monotherapy with Adjunctive Topical Corticosteroids for Acanthamoeba Keratitis. J. Ophthalmic Vis. Res. 2015, 10, 106–111. [Google Scholar] [CrossRef]
- Bouheraoua, N.; Gaujoux, T.; Goldschmidt, P.; Chaumeil, C.; Laroche, L.; Borderie, V.M. Prognostic Factors Associated with the Need for Surgical Treatments in Acanthamoeba Keratitis. Cornea 2013, 32, 130–136. [Google Scholar] [CrossRef]
- Vilares-Morgado, R.; Ferreira, A.M.; Marques-Couto, P.; Madeira, C.; Moreira, R.; Torrão, L.; Neves-Cardoso, P.; Cunha, A.M.; Rebelo, S.; Pinheiro-Costa, J. Clinical Outcomes and Prognostic Factors in Acanthamoeba Keratitis. Contact Lens Anterior Eye 2024, 47, 102119. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, 71. [Google Scholar] [CrossRef]
- National Heart, L. and B.H.I. (NIH) Study Quality Assessment Tools. Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed on 13 January 2025).
- Higgins, J.; Savović, J.; Page, M.; Elbers, R.; Sterne, J. Chapter 8: Assessing Risk of Bias in a Randomized Trial [Last Updated October 2019]. In Cochrane Handbook for Systematic Reviews of Interventions, version 6.5; Higgins, J., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M., Welch, V., Eds.; Cochrane: London, UK, 2024. [Google Scholar]
- McGuinness, L.A.; Higgins, J.P.T. Risk-of-Bias VISualization (Robvis): An R Package and Shiny Web App for Visualizing Risk-of-Bias Assessments. Res. Synth. Methods 2021, 12, 55–61. [Google Scholar] [CrossRef]
- Bagga, B.; Sharma, S.; Gour, R.P.S.; Mohamed, A.; Joseph, J.; M Rathi, V.; Garg, P. A Randomized Masked Pilot Clinical Trial to Compare the Efficacy of Topical 1% Voriconazole Ophthalmic Solution as Monotherapy with Combination Therapy of Topical 0.02% Polyhexamethylene Biguanide and 0.02% Chlorhexidine in the Treatment of Acanthamoeba K. Eye 2021, 35, 1326–1333. [Google Scholar] [CrossRef] [PubMed]
- Hargrave, S.L.; McCulley, J.P.; Husseini, Z. Results of a Trial of Combined Propamidine Isethionate and Neomycin Therapy for Acanthamoeba Keratitis. Ophthalmology 1999, 106, 952–957. [Google Scholar] [CrossRef] [PubMed]
- Caruso, C.; Eletto, D.; Rinaldi, M.; Pacente, L.; Troisi, S.; Semeraro, F.; Dell’omo, R.; Costagliola, C. Effectiveness and Safety of Topical Chlorhexidine and Vitamin e Tpgs in the Treatment of Acanthamoeba Keratitis: A Survey on 29 Cases. J. Clin. Med. 2020, 9, 3775. [Google Scholar] [CrossRef] [PubMed]
- Dart, J.K.G.; Papa, V.; Rama, P.; Knutsson, K.A.; Ahmad, S.; Hau, S.; Sanchez, S.; Franch, A.; Birattari, F.; Leon, P.; et al. The Orphan Drug for Acanthamoeba Keratitis (ODAK) Trial: PHMB 0.08% (Polihexanide) and Placebo versus PHMB 0.02% and Propamidine 0.1%. Ophthalmology 2024, 131, 277–287. [Google Scholar] [CrossRef]
- Rahimi, F.; Rafizadeh, S.M.; Beheshtnejad, A.H.; Hashemian, M.N.; Zare, M.A.; Kohansal, S.; Shakib, A.; Valeshabad, A.K. Clinical Outcomes in Acanthamoeba Keratitis Treated with Polyhexamethylene Biguanide as Monotherapy. Iran. J. Ophthalmol. 2014, 26, 41–47. [Google Scholar]
- Megha, K.; Thakur, A.; Khurana, S.; Sehgal, R.; Gupta, A. Acanthamoeba Keratitis: A 4-Year Review from a Tertiary Care Hospital in North India. Nepal. J. Ophthalmol. 2020, 12, 83–90. [Google Scholar] [CrossRef]
- Tu, E.Y.; Joslin, C.E.; Sugar, J.; Shoff, M.E.; Booton, G.C. Prognostic Factors Affecting Visual Outcome in Acanthamoeba Keratitis. Ophthalmology 2008, 115, 1998–2003. [Google Scholar] [CrossRef]
- Pang, J.; Wei, Z.; Wang, L.; Guo, X.; Chen, Q.; Wei, Y.; Peng, Y.; Zhang, Z.; Zhang, Y.; Liu, J.; et al. Acanthamoeba Keratitis in China: Genotypic and Clinical Correlations. Transl. Vis. Sci. Technol. 2024, 13, 5. [Google Scholar] [CrossRef]
- List, W.; Glatz, W.; Riedl, R.; Mossboeck, G.; Steinwender, G.; Wedrich, A. Evaluation of Acanthamoeba Keratitis Cases in a Tertiary Medical Care Centre over 21 Years. Sci. Rep. 2021, 11, 1036. [Google Scholar] [CrossRef]
- Jo, Y.J.; Jang, S.K.; Lee, J.; Lee, J.S. A 5-Year Review of Acanthamoeba Keratitis Related to Wearing Contact Lenses in Korea. Eye Contact Lens 2020, 46, 223–227. [Google Scholar] [CrossRef]
- Papa, V.; Rama, P.; Radford, C.; Minassian, D.C.; Dart, J.K.G. Acanthamoeba Keratitis Therapy: Time to Cure and Visual Outcome Analysis for Different Antiamoebic Therapies in 227 Cases. Br. J. Ophthalmol. 2020, 104, 575–581. [Google Scholar] [CrossRef] [PubMed]
- Lin, I.H.; Tseng, S.H.; Huang, F.C.; Huang, Y.H. Effect of Ethanol Pretreatment in Acanthamoeba Keratitis: A Long-Term Follow-up Study. Infect. Drug Resist. 2018, 11, 937–943. [Google Scholar] [CrossRef] [PubMed]
- McKelvie, J.; Alshiakhi, M.; Ziaei, M.; Patel, D.V.; McGhee, C.N.J. The Rising Tide of Acanthamoeba Keratitis in Auckland, New Zealand: A 7-Year Review of Presentation, Diagnosis and Outcomes (2009–2016). Clin. Exp. Ophthalmol. 2018, 46, 600–607. [Google Scholar] [CrossRef]
- Azuara-Blanco, A.; Sadiq, A.S.; Hussain, M.; Lloyd, J.H.; Dua, H.S. Successful Medical Treatment of Acanthamoeba Keratitis. Int. Ophthalmol. 1997, 21, 223–227. [Google Scholar] [CrossRef] [PubMed]
- Carnt, N.; Robaei, D.; Watson, S.L.; Minassian, D.C.; Dart, J.K.G. The Impact of Topical Corticosteroids Used in Conjunction with Antiamoebic Therapy on the Outcome of Acanthamoeba Keratitis. Ophthalmology 2016, 123, 984–990. [Google Scholar] [CrossRef]
- Höllhumer, R.; Keay, L.; Watson, S.L. Acanthamoeba Keratitis in Australia: Demographics, Associated Factors, Presentation and Outcomes: A 15-Year Case Review. Eye 2020, 34, 725–732. [Google Scholar] [CrossRef]
- Blaser, F.; Bajka, A.; Grimm, F.; Metzler, S.; Herrmann, D.; Barthelmes, D.; Zweifel, S.A.; Said, S. Assessing PCR-Positive Acanthamoeba Keratitis—A Retrospective Chart Review. 2024, 1–11. Microorganisms 2024, 12, 1214. [Google Scholar] [CrossRef]
- Tew, T.B.; Chu, H.S.; Hou, Y.C.; Chen, W.L.; Wang, I.J.; Hu, F.R. Therapeutic Penetrating Keratoplasty for Microbial Keratitis in Taiwan from 2001 to 2014. J. Formos. Med. Assoc. 2020, 119, 1061–1069. [Google Scholar] [CrossRef]
- Chen, W.L.; Wu, C.Y.; Hu, F.R.; Wang, I.J. Therapeutic Penetrating Keratoplasty for Microbial Keratitis in Taiwan from 1987 to 2001. Am. J. Ophthalmol. 2004, 137, 736–743. [Google Scholar] [CrossRef]
- Laurik, K.L.; Szentmáry, N.; Daas, L.; Langenbucher, A.; Seitz, B. Early Penetrating Keratoplasty À Chaud May Improve Outcome in Therapy-Resistant Acanthamoeba Keratitis. Adv. Ther. 2019, 36, 2528–2540. [Google Scholar] [CrossRef]
- Liu, H.Y.; Chu, H.S.; Wang, I.J.; Chen, W.L.; Hou, Y.C.; Hu, F.R. Clinical Features and Outcomes of Acanthamoeba Keratitis in a Tertiary Hospital over 20- Year Period. J. Formos. Med. Assoc. 2020, 119, 211–217. [Google Scholar] [CrossRef] [PubMed]
- Kitzmann, A.S.; Goins, K.M.; Sutphin, J.E.; Wagoner, M.D. Keratoplasty for Treatment of Acanthamoeba Keratitis. Ophthalmology 2009, 116, 864–869. [Google Scholar] [CrossRef] [PubMed]
- Qi, X.; Mao, H.; Liu, J.; Dong, Y.; Du, M.; Liu, T.; Zhang, T.; Lu, X.; Gao, H. Comparison of Therapeutic Effects between Big-Bubble Deep Anterior Lamellar Keratoplasty and Penetrating Keratoplasty for Medically Unresponsive Acanthamoeba Keratitis. BMC Infect. Dis. 2024, 24, 276. [Google Scholar] [CrossRef]
- Wang, H.; Jhanji, V.; Ye, C.; Ren, Y.; Zheng, Q.; Li, J.; Zhao, Z.; Chen, W. Elliptical Deep Anterior Lamellar Keratoplasty in Severe Acanthamoeba Keratitis. Indian J. Ophthalmol. 2023, 71, 999–1004. [Google Scholar] [CrossRef]
- Zhang, T.; Xie, L.; Dong, Y.; Cheng, J. Therapeutic Keratoplasty for Severe Acanthamoeba Keratitis: Risk Factors, Clinical Features, and Outcomes of Postoperative Recurrence. Graefe’s Arch. Clin. Exp. Ophthalmol. 2023, 261, 1299–1309. [Google Scholar] [CrossRef]
- Roozbahani, M.; Hammersmith, K.M.; Rapuano, C.J.; Nagra, P.K.; Zhang, Q. Therapeutic Penetrating Keratoplasty for Acanthamoeba Keratitis: A Review of Cases, Complications and Predictive Factors. Int. Ophthalmol. 2019, 39, 2889–2896. [Google Scholar] [CrossRef]
- Sabatino, F.; Sarnicola, E.; Sarnicola, C.; Tosi, G.M.; Perri, P.; Sarnicola, V. Early Deep Anterior Lamellar Keratoplasty (DALK) for Acanthamoeba Keratitis Poorly Responsive to Medical Treatment. Cornea 2016, 35, 1–5. [Google Scholar] [CrossRef]
- Robaei, D.; Carnt, N.; Minassian, D.C.; Dart, J.K.G. Therapeutic and Optical Keratoplasty in the Management of Acanthamoeba Keratitis: Risk Factors, Outcomes, and Summary of the Literature. Ophthalmology 2015, 122, 17–24. [Google Scholar] [CrossRef]
- Bagga, B.; Garg, P.; Joseph, J.; Mohamed, A.; Kalra, P. Outcome of Therapeutic Deep Anterior Lamellar Keratoplasty in Advanced Acanthamoeba Keratitis. Indian J Ophthalmol. 2020, 68, 442–446. [Google Scholar] [CrossRef]
- Thebpatiphat, N.; Hammersmith, K.M.; Rocha, F.N.; Rapuano, C.J.; Ayres, B.D.; Laibson, P.R.; Eagle, R.C.; Cohen, E.J. Acanthamoeba Keratitis: A Parasite on the Rise. Cornea 2007, 26, 701–706. [Google Scholar] [CrossRef]
- Butler, T.K.H.; Males, J.J.; Robinson, L.P.; Wechsler, A.W.; Sutton, G.L.; Cheng, J.; Taylor, P.; McClellan, K. Six-Year Review of Acanthamoeba Keratitis in New South Wales, Australia: 1997-2002. Clin. Exp. Ophthalmol. 2005, 33, 41–46. [Google Scholar] [CrossRef] [PubMed]
- Chin, J.; Young, A.L.; Hui, M.; Jhanji, V. Acanthamoeba Keratitis: 10-Year Study at a Tertiary Eye Care Center in Hong Kong. Contact Lens Anterior Eye 2015, 38, 99–103. [Google Scholar] [CrossRef] [PubMed]
- Alfonso-Muñoz, E.A.; Roig-Revert, M.J.; Fernández-López, E.; Hernández-Díaz, M.; Araujo-Miranda, R.; Peris-Martínez, C. A Report of 10 Patients with Acanthamoeba Keratitis. Arch. la Soc. Española Oftalmol. (Engl. Ed.) 2018, 93, 497–502. [Google Scholar] [CrossRef]
- Kaiserman, I.; Bahar, I.; McAllum, P.; Srinivasan, S.; Elbaz, U.; Slomovic, A.R.; Rootman, D.S. Prognostic Factors in Acanthamoeba Keratitis. Can. J. Ophthalmol. 2012, 47, 312–317. [Google Scholar] [CrossRef]
- Ikeda, Y.; Miyazaki, D.; Yakura, K.; Kawaguchi, A.; Ishikura, R.; Inoue, Y.; Mito, T.; Shiraishi, A.; Ohashi, Y.; Higaki, S.; et al. Assessment of Real-Time Polymerase Chain Reaction Detection of Acanthamoeba and Prognosis Determinants of Acanthamoeba Keratitis. Ophthalmology 2012, 119, 1111–1119. [Google Scholar] [CrossRef]
- Patel, D.V.; Rayner, S.; McGhee, C.N.J. Resurgence of Acanthamoeba Keratitis in Auckland, New Zealand: A 7-Year Review of Presentation and Outcomes. Clin. Exp. Ophthalmol. 2010, 38, 15–20. [Google Scholar] [CrossRef]
- Shimmura-Tomita, M.; Takano, H.; Kinoshita, N.; Toyoda, F.; Tanaka, Y.; Takagi, R.; Kobayashi, M.; Kakehashi, A. Risk Factors and Clinical Signs of Severe Acanthamoeba Keratitis. Clin. Ophthalmol. 2018, 12, 2567–2573. [Google Scholar] [CrossRef]
- Zhang, X.; Sun, X.; Jiang, C.; Wang, Z.; Zhang, Y.; Deng, S.; Labbé, A. A New in Vivo Confocal Microscopy Prognostic Factor in Acanthamoeba Keratitis. J. Fr. Ophtalmol. 2014, 37, 130–137. [Google Scholar] [CrossRef]
- Radford, C.F.; Lehmann, O.J.; Dart, J.K. Acanthamoeba Keratitis: Multicentre Survey in England 1992-6. National Acanthamoeba Keratitis Study Group. Br. J. Ophthalmol. 1998, 82, 1387–1392. [Google Scholar] [CrossRef]
- Randag, A.C.; Van Rooij, J.; Van Goor, A.T.; Verkerk, S.; Wisse, R.P.L.; Saelens, I.E.Y.; Stoutenbeek, R.; Van Dooren, B.T.H.; Cheng, Y.Y.Y.; Eggink, C.A. The Rising Incidence of Acanthamoeba Keratitis: A 7-Year Nationwide Survey and Clinical Assessment of Risk Factors and Functional Outcomes. PLoS One 2019, 14, e0222067. [Google Scholar] [CrossRef]
- Bacon, A.S.; Frazer, D.G.; Dart, J.K.G.; Matheson, A.S.; Ficker, L.A.; Wright, P. A Review of 72 Consecutive Cases of Acanthamoeba Keratitis, 1984-1992. Eye 1993, 7, 719–725. [Google Scholar] [CrossRef] [PubMed]
- D’Aversa, G.; Stern, G.A.; Driebe, W.T. Diagnosis and Successful Medical Treatment of Acanthamoeba Keratitis. Arch Ophthalmol. 1995, 113, 1120–1123. [Google Scholar] [CrossRef] [PubMed]
- Claerhout, I.; Goegebuer, A.; Van Den Broecke, C.; Kestelyn, P. Delay in Diagnosis and Outcome of Acanthamoeba Keratitis. Graefe’s Arch. Clin. Exp. Ophthalmol. 2004, 242, 648–653. [Google Scholar] [CrossRef] [PubMed]
- Chew, H.F.; Yildiz, E.H.; Hammersmith, K.M.; Eagle, R.C.; Rapuano, C.J.; Laibson, P.R.; Ayres, B.D.; Jin, Y.P.; Cohen, E.J. Clinical Outcomes and Prognostic Factors Associated with Acanthamoeba Keratitis. Cornea 2011, 30, 435–441. [Google Scholar] [CrossRef]
- Chopra, R.; Mulholland, P.J.; Hau, S.C. In Vivo Confocal Microscopy Morphologic Features and Cyst Density in Acanthamoeba Keratitis. Am. J. Ophthalmol. 2020, 217, 38–48. [Google Scholar] [CrossRef]
- Bonini, S.; Di Zazzo, A.; Varacalli, G.; Coassin, M. Acanthamoeba Keratitis: Perspectives for Patients. Curr. Eye Res. 2021, 46, 771–776. [Google Scholar] [CrossRef]
- Yamazoe, K.; Yamamoto, Y.; Shimazaki-Den, S.; Shimazaki, J. Visual Outcome in Japanese Patients with Acanthamoeba Keratitis. Eye 2012, 26, 517–522. [Google Scholar] [CrossRef]
- Arnalich-Montiel, F.; Lumbreras-Fernańdez, B.; Martín-Navarro, C.M.; Valladares, B.; Lopez-Velez, R.; Morcillo-Laiz, R.; Lorenzo-Morales, J. Influence of Acanthamoeba Genotype on Clinical Course and Outcomes for Patients with Acanthamoeba Keratitis in Spain. J. Clin. Microbiol. 2014, 52, 1213–1216. [Google Scholar] [CrossRef]
- Park, D.H.; Palay, D.A.; Daya, S.M.; Stulting, R.D.; Krachmer, J.H.; Holland, E.J. The Role of Topical Corticosteroids in the Management of Acanthamoeba Keratitis. Cornea 1997, 16, 277–283. [Google Scholar] [CrossRef]
- Landeo, L.L. Diagnosis and Treatment of Acanthamoeba Keratitis. Oftalmol. Zh. 2015, 7–12. [Google Scholar] [CrossRef]
- Sun, X.; Zhang, Y.; Li, R.; Wang, Z.; Luo, S.; Gao, M.; Deng, S.; Chen, W.; Jin, X. Acanthamoeba Keratitis: Clinical Characteristics and Management. Ophthalmology 2006, 113, 412–416. [Google Scholar] [CrossRef] [PubMed]
- Martín-Navarro, C.M.; López-Arencibia, A.; Sifaoui, I.; Reyes-Batlle, M.; Valladares, B.; Martínez-Carretero, E.; Piñero, J.E.; Maciver, S.K.; Lorenzo-Morales, J. Statins and Voriconazole Induce Programmed Cell Death in Acanthamoeba Castellanii. Antimicrob. Agents Chemother. 2015, 59, 2817–2824. [Google Scholar] [CrossRef] [PubMed]
- Schuster, F.L.; Guglielmo, B.J.; Visvesvara, G.S. In-Vitro Activity of Miltefosine and Voriconazole on Clinical Isolates of Free-Living Amebas: Balamuthia Mandrillaris, Acanthamoeba Spp., and Naegleria Fowleri. J. Eukaryot. Microbiol. 2006, 53, 121–126. [Google Scholar] [CrossRef] [PubMed]
- Levine, M.T.; Chandrasekar, P.H. Adverse Effects of Voriconazole: Over a Decade of Use. Clin. Transplant. 2016, 30, 1377–1386. [Google Scholar] [CrossRef]
- Elder, M.J.; Kilvington, S.; Dart, J.K.G. A Clinicopathologic Study of in Vitro Sensitivity Testing and Acanthamoeba Keratitis. Investig. Ophthalmol. Vis. Sci. 1994, 35, 1059–1064. [Google Scholar]
- Balasubramanya, R.; Garg, P.; Sharma, S.; Vemuganti, G.K. Acanthamoeba Keratitis after LASIK. J. Refract. Surg. 2006, 22, 616–617. [Google Scholar] [CrossRef]
- Anwar, A.; Siddiqui, R.; Hameed, A.; Shah, M.R.; Khan, N.A. Synthetic Dihydropyridines as Novel Antiacanthamoebic Agents. Med. Chem. 2020, 16, 841–847. [Google Scholar] [CrossRef]
- Martín-Navarro, C.M.; Lorenzo-Morales, J.; Machin, R.P.; López-Arencibia, A.; García-Castellano, J.M.; de Fuentes, I.; Loftus, B.; Maciver, S.K.; Valladares, B.; Piñero, J.E. Inhibition of 3-Hydroxy-3-Methylglutaryl–Coenzyme A Reductase and Application of Statins as a Novel Effective Therapeutic Approach against Acanthamoeba Infections. Antimicrob. Agents Chemother. 2013, 57, 375–381. [Google Scholar] [CrossRef]
- Cristian, C.; Marco, C.d.V.; Arturo, K.; Claudio, P.; Miguel, S.; Rolf, R.; Remigio, L.; Leonidas, T. Accelerated Collagen Cross-Linking in the Management of Advanced Acanthamoeba Keratitis. Arq. Bras. Oftalmol. 2019, 82, 103–106. [Google Scholar] [CrossRef]
- Atalay, H.T.; Dogruman-Al, F.; Sarzhanov, F.; Özmen, M.C.; Tefon, A.B.; Arıbaş, Y.K.; Bilgihan, K. Effect of Riboflavin/Rose Bengal-Mediated PACK-CXL on Acanthamoeba Trophozoites and Cysts in Vitro. Curr. Eye Res. 2018, 43, 1322–1325. [Google Scholar] [CrossRef]
- Haapanen, S.; Barker, H.; Carta, F.; Supuran, C.T.; Parkkila, S. Novel Drug Screening Assay for Acanthamoeba Castellanii and the Anti-Amoebic Effect of Carbonic Anhydrase Inhibitors. J. Med. Chem. 2023, 67, 152–164. [Google Scholar] [CrossRef] [PubMed]
- Dudley, R.; Alsam, S.; Khan, N.A. Cellulose Biosynthesis Pathway Is a Potential Target in the Improved Treatment of Acanthamoeba Keratitis. Appl. Microbiol. Biotechnol. 2007, 75, 133–140. [Google Scholar] [CrossRef] [PubMed]
- Du, Q.; Schilde, C.; Birgersson, E.; Chen, Z.; McElroy, S.; Schaap, P. The Cyclic AMP Phosphodiesterase RegA Critically Regulates Encystation in Social and Pathogenic Amoebas. Cell. Signal. 2014, 26, 453–459. [Google Scholar] [CrossRef] [PubMed]
- Köhsler, M.; Leitsch, D.; Mbouaka, A.L.; Wekerle, M.; Walochnik, J. Transcriptional Changes of Proteins of the Thioredoxin and Glutathione Systems in Acanthamoeba Spp. under Oxidative Stress–an RNA Approach. Parasite 2022, 29, 24. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marques-Couto, P.; Monteiro, M.; Ferreira, A.M.; Pinheiro-Costa, J.; Vilares-Morgado, R. Acanthamoeba Keratitis Management and Prognostic Factors: A Systematic Review. J. Clin. Med. 2025, 14, 2528. https://doi.org/10.3390/jcm14072528
Marques-Couto P, Monteiro M, Ferreira AM, Pinheiro-Costa J, Vilares-Morgado R. Acanthamoeba Keratitis Management and Prognostic Factors: A Systematic Review. Journal of Clinical Medicine. 2025; 14(7):2528. https://doi.org/10.3390/jcm14072528
Chicago/Turabian StyleMarques-Couto, Pedro, Mariana Monteiro, Ana Margarida Ferreira, João Pinheiro-Costa, and Rodrigo Vilares-Morgado. 2025. "Acanthamoeba Keratitis Management and Prognostic Factors: A Systematic Review" Journal of Clinical Medicine 14, no. 7: 2528. https://doi.org/10.3390/jcm14072528
APA StyleMarques-Couto, P., Monteiro, M., Ferreira, A. M., Pinheiro-Costa, J., & Vilares-Morgado, R. (2025). Acanthamoeba Keratitis Management and Prognostic Factors: A Systematic Review. Journal of Clinical Medicine, 14(7), 2528. https://doi.org/10.3390/jcm14072528






