Telemedicine Hybrid Care Models in Gastroenterology Outpatient Care: Results from a German Tertiary Center
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Data Collection
2.3. Telemedicine Implementation
2.4. Outcome Measures
2.5. Statistical Analysis
2.6. Ethics Committee’s Approval
3. Results
3.1. Demographics and Baseline Characteristics
3.2. Disease Distribution and Medical Management
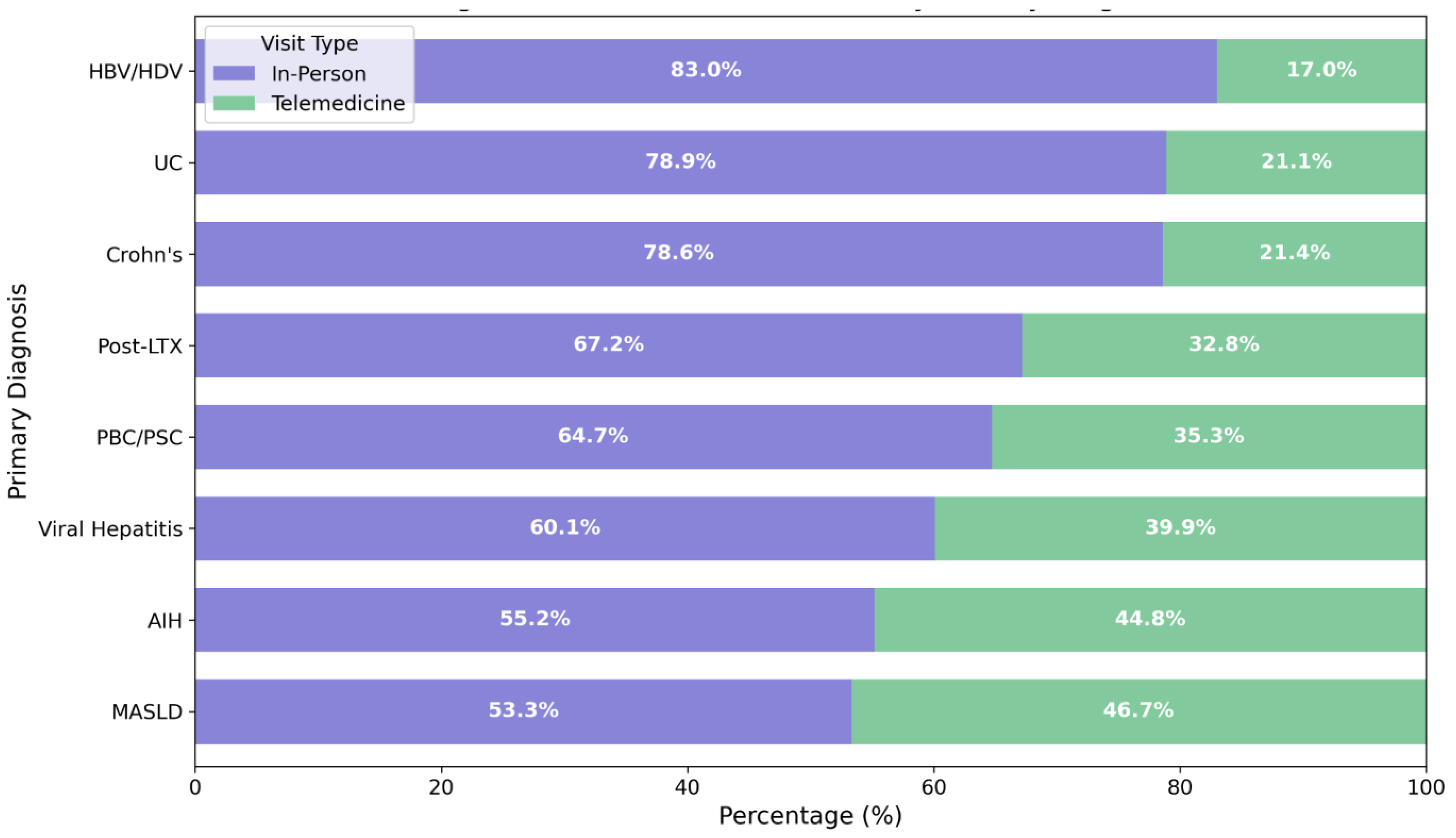
3.3. Appointment Distribution and Follow-Up Patterns
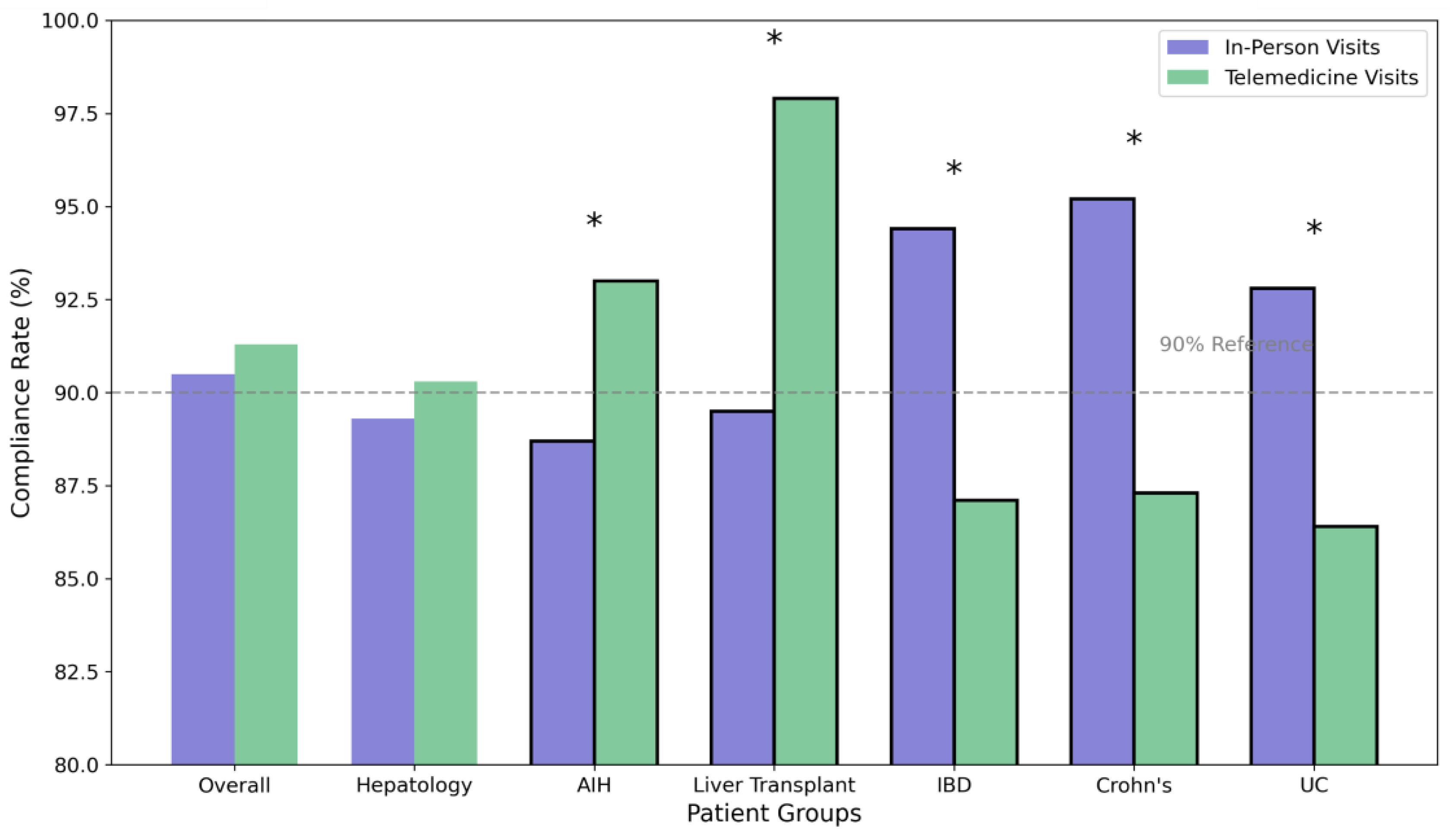
3.4. Appointment Compliance and Predictors of Success
3.5. Clinical Outcomes
4. Discussion
- Telemedicine-preferred: Stable MASLD patients, well-controlled post-transplant recipients beyond one year, and IBD patients in sustained remission. These patients can be primarily managed through telemedicine with annual in-person assessments.
- Hybrid care: Patients requiring regular monitoring but showing stable disease patterns. This includes most liver transplant recipients, compensated cirrhosis patients, and IBD/AIH/PBC patients on stable therapy. A structured alternating schedule of in-person and telemedicine visits appears optimal.
- In-person priority: Patients with HBV/HDV coinfection, decompensated cirrhosis, active IBD flares, or those requiring frequent procedural interventions should maintain primarily in-person care with telemedicine serving as supplementary support.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AIH | Autoimmune hepatitis |
| CI | Confidence interval |
| COVID-19 | Coronavirus disease 2019 |
| HBV | Hepatitis B virus |
| HDV | Hepatitis D virus |
| IBD | Liver transplant |
| INR | International normalized ratio |
| LTX | Liver transplant |
| MASLD | Metabolic-associated steatotic liver disease |
| MDR | Multidrug-resistant organisms |
| MELD | Model for End-Stage Liver Disease |
| OR | Odds ratio |
| ORBIS | Hospital’s electronic medical record system, as mentioned |
| PBC | Primary biliary cholangitis |
| PSC | Primary sclerosing cholangitis |
References
- Bohmer, M.M.; Buchholz, U.; Corman, V.M.; Hoch, M.; Katz, K.; Marosevic, D.V.; Bohm, S.; Woudenberg, T.; Ackermann, N.; Konrad, R.; et al. Investigation of a COVID-19 outbreak in Germany resulting from a single travel-associated primary case: A case series. Lancet Infect Dis 2020, 20, 920–928. [Google Scholar] [CrossRef] [PubMed]
- Hoehl, S.; Rabenau, H.; Berger, A.; Kortenbusch, M.; Cinatl, J.; Bojkova, D.; Behrens, P.; Boddinghaus, B.; Gotsch, U.; Naujoks, F.; et al. Evidence of SARS-CoV-2 infection in returning travelers from Wuhan, China. N. Engl. J. Med. 2020, 382, 1278–1280. [Google Scholar] [CrossRef] [PubMed]
- Priesemann, V.; Brinkmann, M.M.; Ciesek, S.; Cuschieri, S.; Czypionka, T.; Giordano, G.; Gurdasani, D.; Hanson, C.; Hens, N.; Iftekhar, E.; et al. Calling for pan-European commitment for rapid and sustained reduction in SARS-CoV-2 infections. Lancet 2021, 397, 92–93. [Google Scholar] [CrossRef]
- Aguas, M.; Del Hoyo, J.; Faubel, R.; Nos, P. Use of telemedicine in inflammatory bowel disease: A real monitoring option? Expert Rev. Gastroenterol. Hepatol. 2016, 10, 879–881. [Google Scholar] [CrossRef] [PubMed]
- Aldzhyan, V.; Tamamian, C.; Tabibian, J.H. Leveraging telemedicine in gastroenterology and hepatology: A narrative review. Mhealth 2023, 9, 36. [Google Scholar] [CrossRef]
- Schutze, B.; Kamler, M. Juristische Aspekte der Telemedizin in Deutschland. [Legal bearings of telemedicine in Germany]. Dtsch. Med. Wochenschr. 2007, 132, 453–457. [Google Scholar] [CrossRef]
- Schone, K. Telemedizin-juristische Aspekte. [Telemedicine--legal aspects]. Herzschrittmacherther. Elektrophysiol. 2005, 16, 143–149. [Google Scholar] [CrossRef]
- Guarino, M.; Cossiga, V.; Fiorentino, A.; Pontillo, G.; Morisco, F. Use of telemedicine for chronic liver disease at a single care center during the COVID-19 pandemic: Prospective observational study. J. Med. Internet Res. 2020, 22, e20874. [Google Scholar] [CrossRef]
- Peine, A.; Paffenholz, P.; Martin, L.; Dohmen, S.; Marx, G.; Loosen, S.H. Telemedicine in Germany during the COVID-19 pandemic: Multi-professional national survey. J. Med. Internet Res. 2020, 22, e19745. [Google Scholar] [CrossRef]
- Costantino, A.; Bortoluzzi, F.; Giuffre, M.; Vassallo, R.; Montalbano, L.M.; Monica, F.; Canova, D.; Checchin, D.; Fedeli, P.; Marmo, R.; et al. Correct use of telemedicine in gastroenterology, hepatology, and endoscopy during and after the COVID-19 pandemic: Recommendations from the italian association of hospital gastroenterologists and endoscopists (AIGO). Dig. Liver Dis. 2021, 53, 1221–1227. [Google Scholar] [CrossRef]
- Piao, C.; Terrault, N.A.; Sarkar, S. Telemedicine: An evolving field in hepatology. Hepatol. Commun. 2019, 3, 716–721. [Google Scholar] [CrossRef] [PubMed]
- Honer Zu Siederdissen, C.; Schultalbers, M.; Wubbolding, M.; Lechte, G.S.; Laser, H.; Cornberg, M.; Wedemeyer, H.; Maasoumy, B. Einfluss der COVID-19 Pandemie auf die Notfallversorung von Patienten mit Leberzirrhose—Erfahrungen eines tertiaren Zentrums. [Impact of the COVID-19 pandemic on patients with liver cirrhosis-the experience of a tertiary center in Germany]. Z. Gastroenterol. 2021, 59, 954–960. [Google Scholar] [CrossRef] [PubMed]
- Dong, M.D.; Steuwe, S.; Barry, L.A.; Siegel, C.A. The use of telemedicine in older patients with gastrointestinal diseases. Curr. Treat. Options Gastroenterol. 2022, 20, 594–604. [Google Scholar] [CrossRef]
- de Jong, M.; van der Meulen-de Jong, A.; Romberg-Camps, M.; Degens, J.; Becx, M.; Markus, T.; Tomlow, H.; Cilissen, M.; Ipenburg, N.; Verwey, M.; et al. Development and feasibility study of a telemedicine tool for all patients with IBD: Myibdcoach. Inflamm. Bowel Dis. 2017, 23, 485–493. [Google Scholar] [CrossRef] [PubMed]
- Boettler, T.; Newsome, P.N.; Mondelli, M.U.; Maticic, M.; Cordero, E.; Cornberg, M.; Berg, T. Care of patients with liver disease during the COVID-19 pandemic: EASL-ESCMID position paper. JHEP Rep. 2020, 2, 100113. [Google Scholar] [CrossRef]
- Jiang, S.X.; Schwab, K.; Enns, R.; Ko, H.H. Survey of the impact of COVID-19 on chronic liver disease patient care experiences and outcomes. J. Can. Assoc. Gastroenterol. 2023, 6, 8–16. [Google Scholar] [CrossRef]
- Van Enst, W.A.; Weng, Y.C.; Wanten, S.A.C.; Seyger, M.M.B.; Baerveldt, E.M.; Arents, B.W.M.; De Jong, E.; Van den Reek, J. Is telemedicine suitable for patients with chronic inflammatory skin conditions? A systematic review. Acta Derm. Venereol. 2024, 104, adv23901. [Google Scholar] [CrossRef]
- Kuriakose Kuzhiyanjal, A.J.; Nigam, G.B.; Antoniou, G.A.; Farraye, F.A.; Cross, R.K.; Limdi, J.K. Management of inflammatory bowel disease using e-health technologies: A systematic review and meta-analysis. J. Crohn’s Colitis 2023, 17, 1596–1613. [Google Scholar] [CrossRef]
- Crespo, J.; Cabezas, J.; Mateo Soler, M.; de la Cuadra-Grande, A.; Casado, M.A.; Lazarus, J.V.; Calleja, J.L. Current state of telemedicine in the field of Hepatology in Spain: Challenges, threats and next steps to follow for an intelligent digital transformation. Rev. Esp. Enferm. Dig. 2023, 115, 248–258. [Google Scholar] [CrossRef]
- Hakak, F.; Patel, R.N.; Gearry, R.B. Review article: Telecare in gastroenterology—Within the COVID-19 pandemic and beyond. Aliment. Pharmacol. Ther. 2024, 59, 1170–1182. [Google Scholar] [CrossRef]
- Kouanda, A.; Faggen, A.; Bayudan, A.; Kamal, F.; Avila, P.; Arain, M.; Dai, S.C.; Munroe, C.A. Impact of telemedicine on no-show rates in an ambulatory gastroenterology practice. Telemed. J. e-Health 2024, 30, 1026–1033. [Google Scholar] [CrossRef] [PubMed]
- Singal, A.K.; Kamath, P.S. Model for end-stage liver disease. J. Clin. Exp. Hepatol. 2013, 3, 50–60. [Google Scholar] [CrossRef]
- Czeisler, M.E.; Kennedy, J.L.; Wiley, J.F.; Facer-Childs, E.R.; Robbins, R.; Barger, L.K.; Czeisler, C.A.; Rajaratnam, S.M.W.; Howard, M.E. Delay or avoidance of routine, urgent and emergency medical care due to concerns about COVID-19 in a region with low COVID-19 prevalence: Victoria, Australia. Respirology 2021, 26, 707–712. [Google Scholar] [CrossRef] [PubMed]
- Splinter, M.J.; Velek, P.; Ikram, M.K.; Kieboom, B.C.T.; Peeters, R.P.; Bindels, P.J.E.; Ikram, M.A.; Wolters, F.J.; Leening, M.J.G.; de Schepper, E.I.T.; et al. Prevalence and determinants of healthcare avoidance during the COVID-19 pandemic: A population-based cross-sectional study. PLoS Med. 2021, 18, e1003854. [Google Scholar] [CrossRef]
- Sadik, N.; Salman, R. Defining telemedicine and engaging future medical practitioners. Comment on “Telemedicine in Germany during the COVID-19 pandemic: Multi-professional national survey”. J. Med. Internet Res. 2021, 23, e23363. [Google Scholar] [CrossRef]
- Lionis, C.; Papadakis, S.; Anastasaki, M.; Aligizakis, E.; Anastasiou, F.; Francque, S.; Gergianaki, I.; Mendive, J.M.; Marketou, M.; Muris, J.; et al. Practice recommendations for the management of MASLD in primary care: Consensus results. Diseases 2024, 12, 180. [Google Scholar] [CrossRef]
- Fard, S.J.; Ghodsbin, F.; Kaviani, M.J.; Jahanbin, I.; Bagheri, Z. The effect of follow up (telenursing) on liver enzymes in patients with nonalcoholic fatty liver disease: A randomized controlled clinical trial. Int. J. Community Based Nurs. Midwifery 2016, 4, 239–246. Available online: https://www.ncbi.nlm.nih.gov/pubmed/27382590 (accessed on 1 March 2025).
- Efe, C.; Simsek, C.; Batibay, E.; Caliskan, A.R.; Wahlin, S. Feasibility of telehealth in the management of autoimmune hepatitis before and during the COVID-19 pandemic. Expert Rev. Gastroenterol. Hepatol. 2020, 14, 1215–1219. [Google Scholar] [CrossRef] [PubMed]
- Coons, S.J.; Sheahan, S.L.; Martin, S.S.; Hendricks, J.; Robbins, C.A.; Johnson, J.A. Predictors of medication noncompliance in a sample of older adults. Clin. Ther. 1994, 16, 110–117. Available online: https://www.ncbi.nlm.nih.gov/pubmed/8205597 (accessed on 1 March 2025).
- Lahat, A.; Shatz, Z. Telemedicine in clinical gastroenterology practice: What do patients prefer? Therap. Adv. Gastroenterol. 2021, 14, 1756284821989178. [Google Scholar] [CrossRef]
- Krause, A.; Haberkorn, U.; Mier, W. Strategies for the treatment of HBV/HDV. Eur. J. Pharmacol. 2018, 833, 379–391. [Google Scholar] [CrossRef] [PubMed]
- Koh, C.; Da, B.L.; Glenn, J.S. HBV/HDV coinfection: A challenge for therapeutics. Clin. Liver Dis. 2019, 23, 557–572. [Google Scholar] [CrossRef]
- Rusignuolo, G.; Thimme, R.; Neumann-Haefelin, C. Chronische Hepatitis-B- und Hepatitis-D-Virusinfektion. [Chronic HBV and HDV infection]. Dtsch. Med. Wochenschr. 2024, 149, 948–954. [Google Scholar] [CrossRef] [PubMed]
- Alyazeedi, A.; Stewart, C.; Soiza, R.L.; Stewart, D.; Awaisu, A.; Ryan, C.; Alhail, M.; Aldarwish, A.; Myint, P.K. Enhancing medication management of older adults in Qatar: Healthcare professionals’ perspectives on challenges, barriers and enabling solutions. Ther. Adv. Drug Saf. 2024, 15, 20420986241272846. [Google Scholar] [CrossRef]
- Heida, A.; Dijkstra, A.; Muller Kobold, A.; Rossen, J.W.; Kindermann, A.; Kokke, F.; de Meij, T.; Norbruis, O.; Weersma, R.K.; Wessels, M.; et al. Efficacy of home telemonitoring versus conventional follow-up: A randomized controlled trial among teenagers with inflammatory bowel disease. J. Crohn’s Colitis 2018, 12, 432–441. [Google Scholar] [CrossRef]
- Sinha Gregory, N.; Shukla, A.P.; Noel, J.J.; Alonso, L.C.; Moxley, J.; Crawford, A.J.; Martin, P.; Kumar, S.; Leonard, J.P.; Czaja, S.J. The feasibility, acceptability, and usability of telehealth visits. Front. Med. 2023, 10, 1198096. [Google Scholar] [CrossRef]
- Brown, C.T.; Zinko, R.; Ngamassi, L.; Ndembe, E.; Furner, C. Barriers to intention to adopt telemedicine: The interplay between exposure, trust, and convenience. Health Mark. Q 2024, 42, 1–23. [Google Scholar] [CrossRef]
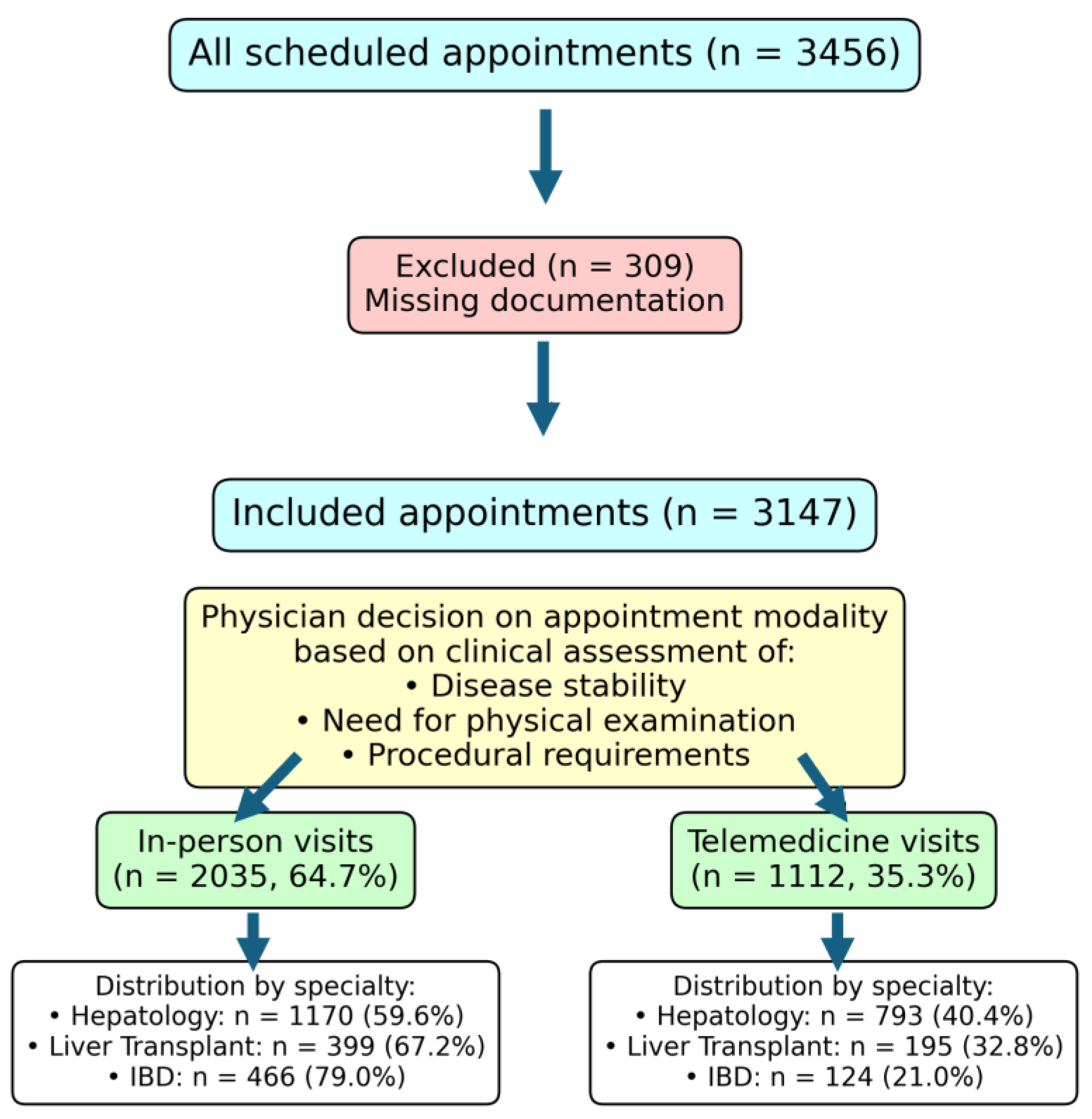
| Characteristic | Total (n = 3147) | Hepatology (n = 1963) | Liver Transplant (n = 594) | IBD (n = 590) |
|---|---|---|---|---|
| Age, median (range) | 51 (15–87) | 52 (15–87) | 58 (15–87) | 42 (18–86) |
| Male gender, n (%) | 1625 (51.6) | 983 (50.1) | 365 (61.5) | 277 (47.0) |
| Primary diagnosis, n (%) | ||||
| MASLD | 433 (13.8) | 366 (18.6) | 62 (10.4) | 5 (0.9) |
| Viral hepatitis | 1031 (32.8) | 857 (43.7) | 154 (25.9) | 20 (3.4) |
| AIH | 192 (6.10) | 137 (6.98) | 43 (7.24) | 12 (2.03) |
| Crohn’s disease | 294 (9.34) | 15 (0.76) | 0 | 279 (47.29) |
| Ulcerative colitis | 280 (8.90) | 19 (0.97) | 32 (5.39) | 229 (38.81) |
| Other | 1109 (35.2) | 706 (36.0) | 346 (58.3) | 57 (9.6) |
| Medications | ||||
| Median number (range) | 3 (0–19) | 2 (0–17) | 7 (0–19) | 3 (0–19) |
| Immunosuppression, n (%) | 776 (24.7) | 210 (10.7) | 340 (57.2) | 226 (38.3) |
| Clinical parameters | ||||
| MDR organisms present, n (%) | 282 (9.0) | 70 (3.6) | 182 (30.6) | 30 (5.1) |
| Required endoscopy, n (%) | 278 (8.8) | 110 (5.6) | 109 (18.4) | 59 (10.0) |
| Comorbidities | ||||
| Arterial hypertension, n (%) | 685 (21.77) | 420 (21.40) | 204 (34.34) | 61 (10.34) |
| Atrial fibrillation, n (%) | 69 (2.19) | 38 (1.94) | 28 (4.71) | 3 (0.51) |
| Renal insufficiency, n (%) | 192 (6.10) | 53 (2.70) | 135 (22.73) | 4 (0.68) |
| Diabetes, n (%) | 451 (14.33) | 268 (13.65) | 152 (25.59) | 31 (5.25) |
| Follow-up intervals | ||||
| Days between visits (previous appointment), median | 89 | 95 | 42 | 52 |
| Visit Type | ||||
| In-person, n (%) | 2035 (64.7) | 1170 (59.6) | 399 (67.2) | 466 (79.0) |
| Telemedicine, n (%) | 1112 (35.3) | 793 (40.4) | 195 (32.8) | 124 (21.0) |
| Laboratory testing | ||||
| Blood tests performed, n (%) | 1587 (50.4) | 909 (46.3) | 318 (53.5) | 360 (61.0) |
| Appointment Distribution | In-Person Visits | Telemedicine Visits |
|---|---|---|
| Full cohort, n (%) | 2035 (64.7%) | 1112 (35.3%) |
| Age, median | 51 | 53 |
| Hepatology, n (%) | 1170 (59.6%) | 793 (40.4%) |
| Viral hepatitis, n (%) | 620 (60.1%) | 411 (39.9%) |
| AIH, n (%) | 106 (55.2%) | 86 (44.8%) |
| PBC/PSC, n (%) | 161 (64.7%) | 88 (35.3%) |
| MASLD, n (%) | 231 (53.3%) | 202 (46.7%) |
| Liver transplant, n (%) | 399 (67.2%) | 195 (32.8%) |
| IBD, n (%) | 466 (79.0%) | 124 (21.0%) |
| Crohn’s disease, n (%) | 231 (78.6%) | 63 (21.4%) |
| Ulcerative colitis, n (%) | 221 (78.9%) | 59 (21.1%) |
| Follow-up scheduling | ||
| Required early follow-up, % | 12.4 | 8.7 |
| Emergency visits within 30 days, % | 4.0 | 3.8 |
| Laboratory monitoring | ||
| Tests ordered, % | 83.9 | 3.5 |
| Abnormal results requiring action, % | 15.2 | 14.8 |
| Outcome Measure | In-Person Visits | Telemedicine Visits | p-Value |
|---|---|---|---|
| Overall compliance rate, % | 90.5 | 91.3 | 0.428 |
| Compliance by specialty | |||
| Hepatology, % | 89.3 | 90.3 | 0.512 |
| Viral Hepatitis, % | 88.9 | 91.8 | 0.124 |
| AIH, % | 88.7 | 93.0 | 0.042 * |
| PBC/PSC, % | 89.4 | 90.9 | 0.682 |
| MASLD, % | 89.6 | 90.6 | 0.724 |
| Liver transplant, % | 89.5 | 97.9 | <0.001 * |
| IBD, % | 94.4 | 87.1 | 0.024 * |
| Crohn’s disease, % | 95.2 | 87.3 | 0.018 * |
| Ulcerative colitis, % | 92.8 | 86.4 | 0.032 * |
| Variable | Univariate Analysis | Multivariate Analysis | ||
|---|---|---|---|---|
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | |
| Clinic type | <0.01 * | <0.01 * | ||
| Hepatology | 1.00 (Reference) | 1.00 (Reference) | ||
| Liver transplant | 0.781 (0.64–0.95) | — | ||
| IBD | 0.358 (0.28–0.45) | — | ||
| Visit characteristics | ||||
| First visit | 0.061 (0.03–0.14) | <0.01 * | 1.910 (0.35–10.30) | |
| Days since last visit | 1.001 (1.000–1.002) | <0.01 * | 1.001 (1.00–1.00) | <0.05 * |
| Days until next visit | 1.003 (1.001–1.004) | <0.01 * | 0.999 (0.99–1.00) | |
| Follow-up type | <0.01 * | <0.01 * | ||
| In-person | 1.00 (Reference) | 1.00 (Reference) | ||
| Telephone | 1.406 (1.11–1.79) | — | ||
| Emergency/inpatient | 0.591 (0.38–0.92) | — | ||
| Pending | 1.330 (1.00–1.78) | — | ||
| Not attended | 1.563 (1.04–2.36) | — | ||
| Patient characteristics | ||||
| Age at visit | 1.009 (1.00–1.01) | <0.01 * | 1.002 (0.99–1.01) | |
| Main diagnosis | ||||
| Other | 1.00 (Reference) | 1.00 (Reference) | ||
| Ulcerative Colitis | 0.422 (0.31–0.58) | <0.01 * | 0.848 (0.57–1.26) | |
| Crohn’s Disease | 0.422 (0.31–0.57) | <0.01 * | 0.649 (0.37–1.15) | |
| HCV | 1.270 (1.01–1.51) | <0.05 * | 1.056 (0.80–1.39) | |
| AIH | 1.591 (1.17–2.17) | <0.01 * | 1.254 (0.90–1.75) | |
| MASLD | 1.737 (1.40–2.16) | <0.01 * | 1.333 (1.05–1.70) | <0.05 * |
| HBV/HDV coinfection | 0.370 (0.19–0.71) | <0.01 * | 0.380 (0.19–0.75) | <0.01 * |
| Post-transplant | 1.281 (1.00–1.64) | <0.05 * | 1.622 (1.11–2.36) | <0.05 * |
| Care requirements | ||||
| Required endoscopy during study period | 0.464 (0.34–0.63) | <0.01 * | 0.572 (0.41–0.81) | <0.01 * |
| Specialist vs. resident care | 0.818 (0.70–0.96) | <0.05 * | 1.038 (0.85–1.27) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abedin, N.; Kilbinger, C.; Queck, A.; Weiler, N.; Pathil, A.; Mihm, U.; Welsch, C.; Blumenstein, I.; Kubesch-Grün, A.; Zeuzem, S.; et al. Telemedicine Hybrid Care Models in Gastroenterology Outpatient Care: Results from a German Tertiary Center. J. Clin. Med. 2025, 14, 2471. https://doi.org/10.3390/jcm14072471
Abedin N, Kilbinger C, Queck A, Weiler N, Pathil A, Mihm U, Welsch C, Blumenstein I, Kubesch-Grün A, Zeuzem S, et al. Telemedicine Hybrid Care Models in Gastroenterology Outpatient Care: Results from a German Tertiary Center. Journal of Clinical Medicine. 2025; 14(7):2471. https://doi.org/10.3390/jcm14072471
Chicago/Turabian StyleAbedin, Nada, Christian Kilbinger, Alexander Queck, Nina Weiler, Anita Pathil, Ulrike Mihm, Christoph Welsch, Irina Blumenstein, Alica Kubesch-Grün, Stefan Zeuzem, and et al. 2025. "Telemedicine Hybrid Care Models in Gastroenterology Outpatient Care: Results from a German Tertiary Center" Journal of Clinical Medicine 14, no. 7: 2471. https://doi.org/10.3390/jcm14072471
APA StyleAbedin, N., Kilbinger, C., Queck, A., Weiler, N., Pathil, A., Mihm, U., Welsch, C., Blumenstein, I., Kubesch-Grün, A., Zeuzem, S., & Dultz, G. (2025). Telemedicine Hybrid Care Models in Gastroenterology Outpatient Care: Results from a German Tertiary Center. Journal of Clinical Medicine, 14(7), 2471. https://doi.org/10.3390/jcm14072471






