Psychometric Evaluation of the Polish Language Version of the Sleep Disturbance Scale for Children (SDSC)—A Pilot Study
Abstract
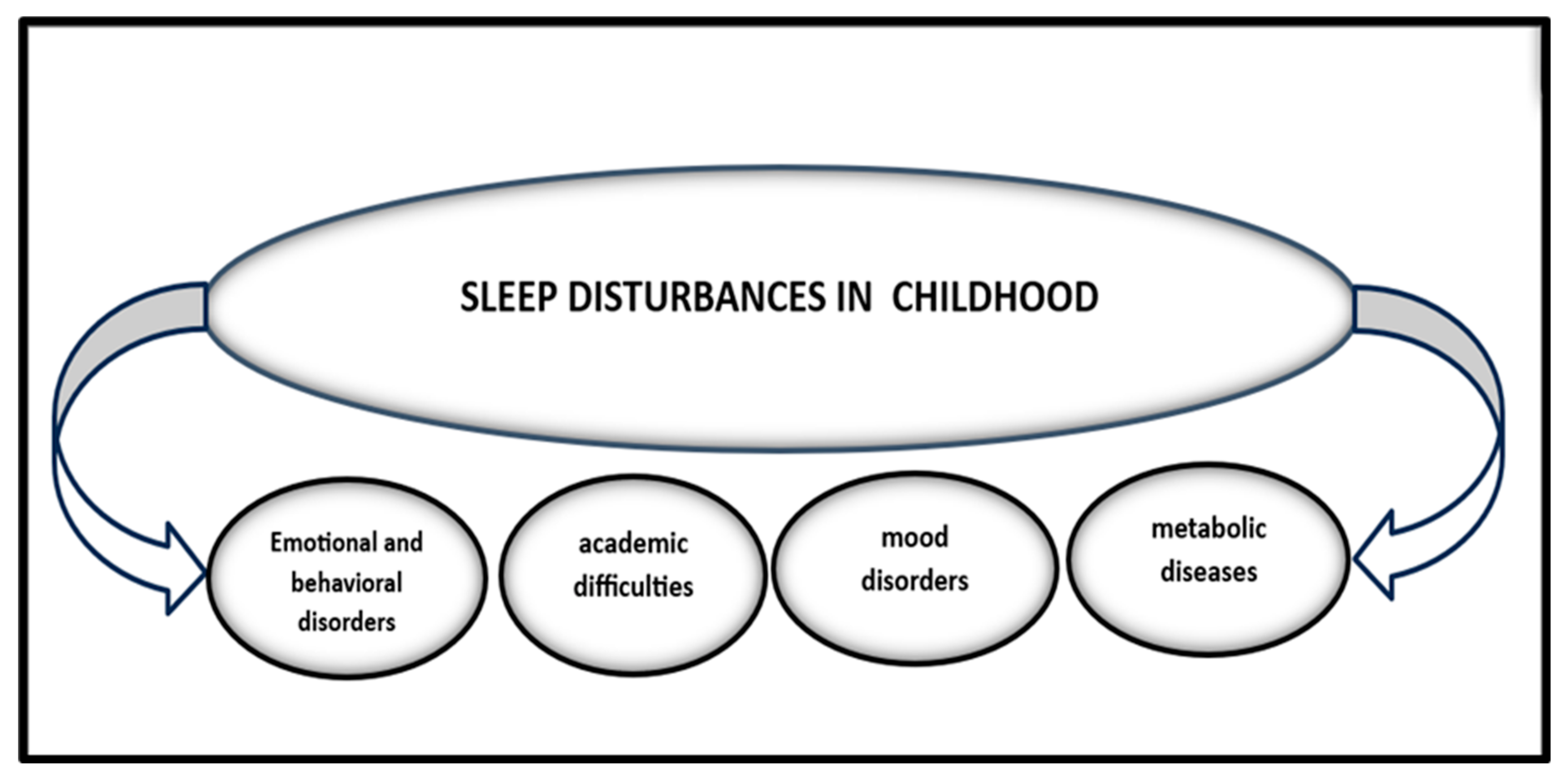
1. Introduction
- Questionnaires based on parent reports;
- Questionnaires for self-reporting by the patient [5].
- Children’s Sleep Habits Questionnaire (CSHQ): This tool is designed for parents of children aged 4 to 10 and helps screen the most common sleep disorders in this age group. It addresses issues such as difficulties falling asleep, delayed sleep onset, insufficient sleep duration, sleep-related anxieties, nighttime awakenings, parasomnias, and sleep-related breathing disorders [5,11].
- Nightmares Effects Questionnaire (NEQ): This questionnaire assesses the impact of nightmares on daytime functioning in adolescents. It consists of 30 items that evaluate six factors: emotion regulation, stress, aggressiveness, depression, attentiveness/concentration, anxiety, and hyperactivity [5].
2. Materials and Methods
- Disorders of initiating and maintaining sleep (DIMS) assessment in questions 1, 2, 3, 4, 5, 10, and 11;
- Sleep breathing disorders (SBD) in questions: 13, 14, 15
- Disorders related to arousal (DA disorders of arousal) in questions 17, 20, 21
- Sleep–wake transition disorders (SWTD) in questions 6, 7, 8, 12, 18, 19
- Disorders of excessive sleepiness (DOES disorders of excessive somnolence) questions: 22, 23, 24, 25 and 26
- excessive sweating during sleep (SHY sleep hyperhidrosis) questions: 9 and 16 [4].
2.1. Characteristics of the Study Group
2.2. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| SDSC | Sleep Disturbance Scale for Children |
| DIMS | disorders of initiating and maintaining sleep |
| SBD | sleep breathing disorders |
| SWTD | sleep–wake transition disorders |
| DOES | disorders of excessive somnolence |
| SHY | sleep hyperhidrosis |
References
- Bruni, O.; Ottaviano, S.; Guidetti, V.; Romoli, M.; Innocenzi, M.; Cortesi, F.; Giannotti, F. The Sleep Disturbance Scale for Children (SDSC). Construction and validation of an instrument to evaluate sleep disturbances in childhood and adolescence. J. Sleep Res. 1996, 5, 251–261. [Google Scholar] [CrossRef] [PubMed]
- Saffari, M.; Gholamrezaei, A.; Saneian, H.; Attari, A.; Bruni, O. Linguistic validation of the sleep disturbance scale for children (SDSC) in Iranian children with Persian language. Sleep Med. 2014, 15, 998–1001. [Google Scholar] [CrossRef] [PubMed]
- Trosman, I.; Ivanenko, A. Classification and Epidemiology of Sleep Disorders in Children and Adolescents. Child Adolesc. Psychiatr. Clin. N. Am. 2021, 30, 47–64. [Google Scholar] [CrossRef] [PubMed]
- Pagerols, M.; Bosch, R.; Prat, R.; Pagespetit, È.; Cilveti, R.; Chaparro, N.; Esteve, A.; Casas, M. The Sleep Disturbance Scale for Children: Psychometric properties and prevalence of sleep disorders in Spanish children aged 6–16 years. J. Sleep Res. 2023, 32, e13871. [Google Scholar] [CrossRef] [PubMed]
- Stuck, B.A.; Maurer, J.T.; Schlarb, A.A.; Schredl, M.; Gunter-Weeꞵ, H. Practice of Sleep Medicine, Sleep Disorders in Children and Adults; Springer Nature: Cham, Switzerland, 2021; pp. 261–263. [Google Scholar]
- Lokhandwala, S.; Spencer, R.M.C. Relations between sleep patterns early in life and brain development: A review. Dev. Cogn. Neurosci. 2022, 56, 101130. [Google Scholar] [CrossRef] [PubMed]
- Davidson-Urbain, W.; Servot, S.; Godbout, R.; Montplaisir, J.Y.; Touchette, E. La somnolence chez les adolescents: Étiologie et conséquences multiples [Sleepiness among adolescents: Etiology and multiple consequences]. L’Encephale 2023, 49, 87–93. [Google Scholar] [CrossRef]
- Jniene, A.; Errguig, L.; El Hangouche, A.J.; Rkain, H.; Aboudrar, S.; El Ftouh, M.; Dakka, T. Perception of Sleep Disturbances due to Bedtime Use of Blue Light-Emitting Devices and Its Impact on Habits and Sleep Quality among Young Medical Students. BioMed Res. Int. 2019, 2019, 7012350. [Google Scholar] [CrossRef]
- Royant-Parola, S.; Londe, V.; Tréhout, S.; Hartley, S. Nouveaux médias sociaux, nouveaux comportements de sommeil chez les adolescents [The use of social media modifies teenagers’ sleep-related behavior]. L’Encephale 2018, 44, 321–328. [Google Scholar] [CrossRef]
- Cooper, R.; Di Biase, M.A.; Bei, B.; Quach, J.; Cropley, V. Associations of Changes in Sleep and Emotional and Behavioral Problems From Late Childhood to Early Adolescence. JAMA Psychiatry 2023, 80, 585–596. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Silva, F.G.; Silva, C.R.; Braga, L.B.; Neto, A.S. Portuguese Children’s Sleep Habits Questionnaire—Validation and cross-cultural comparison. J. Pediatr. 2014, 90, 78–84. [Google Scholar] [CrossRef] [PubMed]
- Schwerdtle, B.; Kanis, J.; Kübler, A.; Schlarb, A.A. The Children’s Sleep Comic: Psychometrics of a Self-rating Instrument for Childhood Insomnia. Child. Psychiatry Hum. Dev. 2016, 47, 53–63. [Google Scholar] [CrossRef] [PubMed]
- Ateş, E.; Konal Korkmaz, E.; Temel, A.B. Turkish Version of the Sleep Self-Report Scale: Factorial Structure and Psychometric Properties for 8–12-Year Old Children. J. Sch. Health 2023, 93, 910–919. [Google Scholar] [CrossRef] [PubMed]
- Janssen, K.C.; Phillipson, S.; O’Connor, J.; Johns, M.W. Validation of the Epworth Sleepiness Scale for Children and Adolescents using Rasch analysis. Sleep Med. 2017, 33, 30–35. [Google Scholar] [CrossRef] [PubMed]
- Spruyt, K.; Gozal, D. Pediatric sleep questionnaires as diagnostic or epidemiological tools: A review of currently available instruments. Sleep Med. Rev. 2011, 15, 19–32. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Putois, B.; Leslie, W.; Gustin, M.P.; Challamel, M.J.; Raoux, A.; Guignard-Perret, A.; Weick, D.; Sauzeau, J.B.; Herbillon, V.; Zourou, F.; et al. The French Sleep Disturbance Scale for Children. Sleep Med. 2017, 32, 56–65. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Xu, P.; Chen, Y.; Chen, S.; Yao, Y.; Lin, X. Validation of the sleep disturbance scale for children (SDSC) in infants and toddlers from mainland China. Front. Psychiatry 2022, 13, 987304. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- de Souza, A.L.D.M.; Giacheti, C.M.; Do Couto, M.C.H.; Galina Spilla, C.S.; da Silva, N.C.; Proença, M.; Pinato, L. Sleep disturbance in children with attention-deficit hyperactivity disorder: Relationship with melatonin and behavior. Neurol. Res. 2024, 46, 803–811. [Google Scholar] [CrossRef] [PubMed]
- Romeo, D.M.; Bruni, O.; Brogna, C.; Ferri, R.; Galluccio, C.; De Clemente, V.; Di Jorio, M.; Quintiliani, M.; Ricci, D.; Mercuri, E. Application of the sleep disturbance scale for children (SDSC) in preschool age. Eur. J. Paediatr. Neurol. 2013, 17, 374–382. [Google Scholar] [CrossRef]
- Ferreira, V.R.; Carvalho, L.B.; Ruotolo, F.; de Morais, J.F.; Prado, L.B.; Prado, G.F. Sleep disturbance scale for children: Translation, cultural adaptation, and validation. Sleep Med. 2009, 10, 457–463. [Google Scholar] [CrossRef]
- Lecuelle, F.; Gustin, M.P.; Leslie, W.; Mindell, J.A.; Franco, P.; Putois, B. French validation of the sleep disturbance scale for children (SDSC) in young children (aged 6 months to 4 years). Sleep Med. 2020, 67, 56–65. [Google Scholar] [CrossRef]
- Spruyt, K.; Cluydts, R.; Verleye, G.B. Pediatric sleep disorders: Exploratory modulation of their relationships. Sleep 2004, 27, 495–501. [Google Scholar] [CrossRef]
- Simola, P.; Niskakangas, M.; Liukkonen, K.; Virkkula, P.; Pitkäranta, A.; Kirjavainen, T.; Aronen, E.T. Sleep problems and daytime tiredness in Finnish preschool-aged children-a community survey. Child Care Health Dev. 2010, 36, 805–811. [Google Scholar] [CrossRef] [PubMed]
- Ağca, S.; Görker, I.; Turan, F.N.; Öztürk, L. Validity and reliability of the Turkish version of Sleep Disturbance Scale for Children. Sleep Med. 2021, 84, 56–62. [Google Scholar] [CrossRef] [PubMed]
- Huang, M.M.; Qian, Z.; Wang, J.; Vaughn, M.G.; Lee, Y.L.; Dong, G.H. Validation of the sleep disturbance scale for children and prevalence of parent-reported sleep disorder symptoms in Chinese children. Sleep Med. 2014, 15, 923–928. [Google Scholar] [CrossRef] [PubMed]
- Ong, L.C.; Yang, W.W.; Wong, S.W.; AlSiddiq, F.; Khu, Y.S. Sleep habits and disturbances in Malaysian children with epilepsy. J. Paediatr. Child Health 2010, 46, 80–84. [Google Scholar] [CrossRef]
- Marriner, A.M.; Pestell, C.; Bayliss, D.M.; McCann, M.; Bucks, R.S. Confirmatory factor analysis of the Sleep Disturbance Scale for Children (SDSC) in a clinical sample of children and adolescents. J. Sleep Res. 2017, 26, 587–594. [Google Scholar] [CrossRef]
- Nair, L.S.R.; George, S.; Anandaraj, S.; Jose, D.; Philip, D.A.; Anjali, J.S. Translating and culturally adapting the sleep disturbance scale for children into Malayalam language: Enhancing pediatric health in the Indian context. J. Indian Soc. Pedod. Prev. Dent. 2024, 42, 309–315. [Google Scholar] [CrossRef] [PubMed]

| DIMS | SBD | DA | SWTD | SHY | DOES | Total | |
|---|---|---|---|---|---|---|---|
| Group size | 42 | 42 | 42 | 42 | 42 | 42 | 42 |
| Number of items | 7 | 3 | 3 | 6 | 5 | 2 | 26 |
| Mean | 12.19 | 4.024 | 4.048 | 8.69 | 7.67 | 2.93 | 39.555 |
| Standard deviation (SD) of the scale | 3.44 | 2.09 | 1.68 | 3.06 | 2.97 | 1.553 | 10.57 |
| Cronbach’s α value | 0.69 | 0.85 | 0.80 | 0.75 | 0.80 | 0.83 | 0.89 |
| −95% CI Cronbach’s | 0.52 | 0.75 | 0.67 | 0.62 | 0.68 | 0.68 | 0.84 |
| +95% CI Cronbach’s | 0.81 | 0.91 | 0.89 | 0.85 | 0.88 | 0.91 | 0.93 |
| Standard error (SE) of measurement | 1.93 | 0.81 | 0.759 | 1.52 | 1.33 | 0.65 | 3.51 |
| Average correlation | 0.22 | 0.71 | 0.57 | 0.36 | 0.44 | 0.77 | 0.25 |
| Cronbach’s alpha standardized (STD) | 0.66 | 0.88 | 0.80 | 0.77 | 0.79 | 0.87 | 0.89 |
| DIMS | SBD | DA | SWTD | DOES | SHY | Total | |
|---|---|---|---|---|---|---|---|
| DIMS | 1.00 | ||||||
| SBD | 0.13 | 1.00 | |||||
| DA | 0.51 | 0.17 | 1.00 | ||||
| SWTD | 0.30 | 0.36 | 0.42 | 1.00 | |||
| DOES | 0.44 | 0.07 | 0.16 | 0.47 | 1.00 | ||
| SHY | 0.28 | 0.52 | 0.41 | 0.56 | 0.20 | 1.00 | |
| Total | 0.78 | 0.36 | 0.60 | 0.72 | 0.67 | 0.69 | 1.00 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jączak-Goździak, M.; Bruni, O.; Żarowski, M. Psychometric Evaluation of the Polish Language Version of the Sleep Disturbance Scale for Children (SDSC)—A Pilot Study. J. Clin. Med. 2025, 14, 2458. https://doi.org/10.3390/jcm14072458
Jączak-Goździak M, Bruni O, Żarowski M. Psychometric Evaluation of the Polish Language Version of the Sleep Disturbance Scale for Children (SDSC)—A Pilot Study. Journal of Clinical Medicine. 2025; 14(7):2458. https://doi.org/10.3390/jcm14072458
Chicago/Turabian StyleJączak-Goździak, Małgorzata, Oliviero Bruni, and Marcin Żarowski. 2025. "Psychometric Evaluation of the Polish Language Version of the Sleep Disturbance Scale for Children (SDSC)—A Pilot Study" Journal of Clinical Medicine 14, no. 7: 2458. https://doi.org/10.3390/jcm14072458
APA StyleJączak-Goździak, M., Bruni, O., & Żarowski, M. (2025). Psychometric Evaluation of the Polish Language Version of the Sleep Disturbance Scale for Children (SDSC)—A Pilot Study. Journal of Clinical Medicine, 14(7), 2458. https://doi.org/10.3390/jcm14072458






