Age-Related Disparities in the Predictive Performance of the Shock Index for Massive Transfusion in Trauma Patients: A Retrospective Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
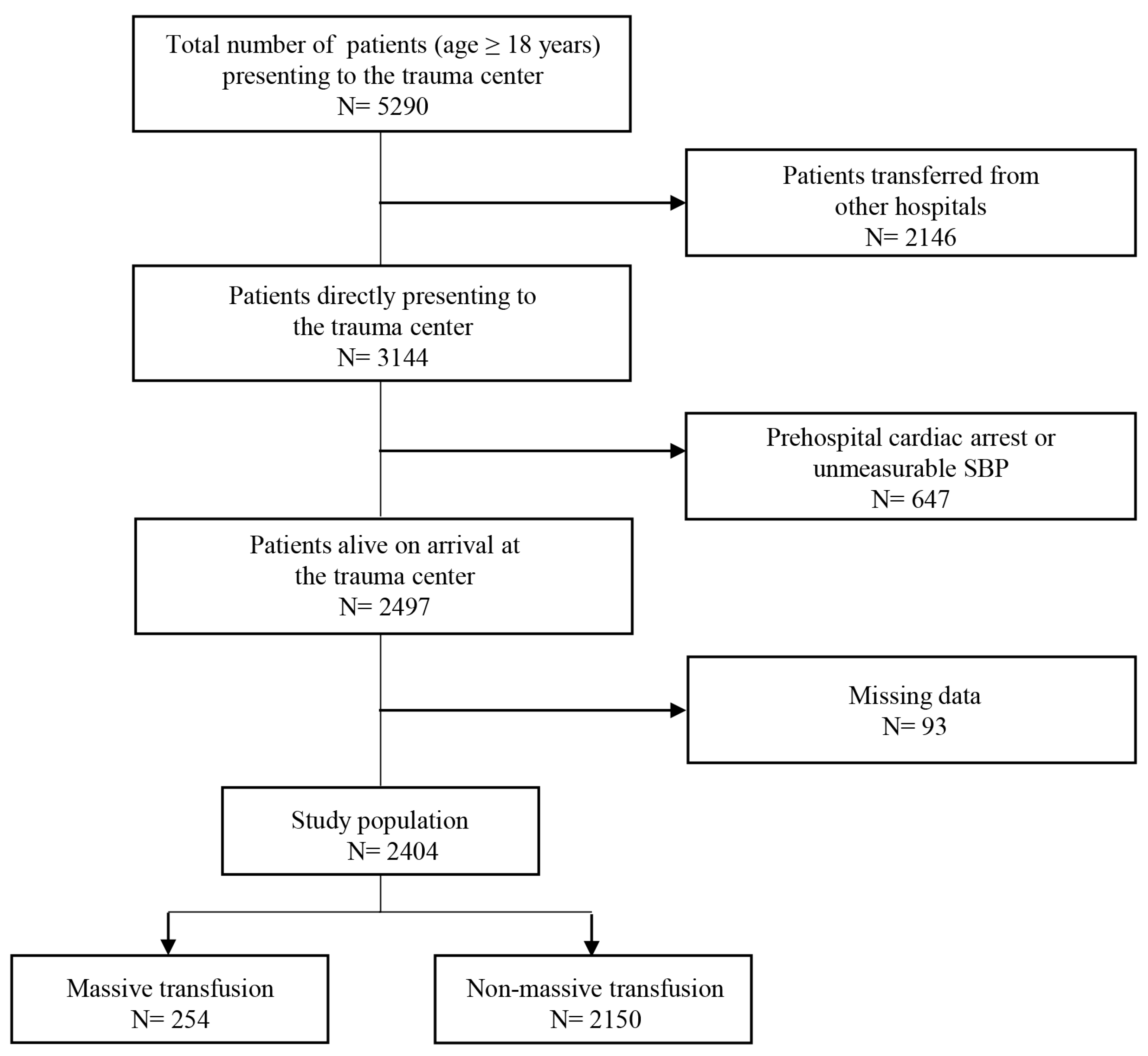
2.2. Patients
2.3. Data Collection
2.4. Outcome
2.5. Statistical Analysis
3. Results
3.1. Comparison of Patient Characteristics and Outcomes
3.2. Logistic Regression Analyses for the Association Between SI and MT
3.3. ROC Analysis of SI for Predicting MT
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pfeifer, R.; Tarkin, I.S.; Rocos, B.; Pape, H.C. Patterns of mortality and causes of death in polytrauma patients-has anything changed? Injury 2009, 40, 907–911. [Google Scholar] [CrossRef] [PubMed]
- Callcut, R.A.; Kornblith, L.Z.; Conroy, A.S.; Robles, A.J.; Meizoso, J.P.; Namias, N.; Meyer, D.E.; Haymaker, A.; Truitt, M.S.; Agrawal, V.; et al. The why and how our trauma patients die: A prospective multicenter western trauma association study. J. Trauma Acute Care Surg. 2019, 86, 864–870. [Google Scholar] [CrossRef] [PubMed]
- Maheshwari, K.; Nathanson, B.H.; Munson, S.H.; Hwang, S.; Yapici, H.O.; Stevens, M.; Ruiz, C.; Hunley, C.F. Abnormal shock index exposure and clinical outcomes among critically ill patients: A retrospective cohort analysis. J. Crit. Care 2020, 57, 5–12. [Google Scholar] [CrossRef] [PubMed]
- Rady, M.Y.; Smithline, H.A.; Blake, H.; Nowak, R.; Rivers, E. Comparison of the shock index and conventional vital signs to identify acute, critical illness in the emergency department. Ann. Emerg. Med. 1994, 24, 685–690. [Google Scholar] [CrossRef]
- Mutschler, M.; Nienaber, U.; Münzberg, M.; Wölfl, C.; Schoechl, H.; Paffrath, T.; Bouillon, B.; Maegele, M.; TraumaRegister DGU. The Shock Index revisited—A fast guide to transfusion requirement? A retrospective analysis on 21,853 patients derived from the TraumaRegister DGU. Crit. Care 2013, 17, R172. [Google Scholar] [CrossRef]
- Schroll, R.; Swift, D.; Tatum, D.; Couch, S.; Heaney, J.B.; Llado-Farrulla, M.; Zucker, S.; Gill, F.; Brown, G.; Buffin, N.; et al. Accuracy of shock index versus ABC score to predict need for massive transfusion in trauma patients. Injury 2018, 49, 15–19. [Google Scholar] [CrossRef]
- Vandromme, M.J.; Griffin, R.L.; Kerby, J.D.; McGwin, G., Jr.; Rue, L.W., 3rd; Weinberg, J.A. Identifying risk for massive transfusion in the relatively normotensive patient: Utility of the prehospital shock index. J. Trauma 2011, 70, 384–388. [Google Scholar]
- Cannon, C.M.; Braxton, C.C.; Kling-Smith, M.; Mahnken, J.D.; Carlton, E.; Moncure, M. Utility of the shock index in predicting mortality in traumatically injured patients. J. Trauma 2009, 67, 1426–1430. [Google Scholar]
- Newgard, C.D.; Cheney, T.P.; Chou, R.; Fu, R.; Daya, M.R.; O’Neil, M.E.; Wasson, N.; Hart, E.L.; Totten, A.M. Out-of-hospital circulatory measures to identify patients with serious injury: A systematic review. Acad. Emerg. Med. 2020, 27, 1323–1339. [Google Scholar]
- Shibahashi, K.; Sugiyama, K.; Okura, Y.; Hoda, H.; Hamabe, Y. Can the shock index be a reliable predictor of early mortality after trauma in older patients? a retrospective cohort study. Acute Med. Surg. 2019, 6, 385–391. [Google Scholar] [CrossRef]
- Zarzaur, B.L.; Croce, M.A.; Fischer, P.E.; Magnotti, L.J.; Fabian, T.C. New vitals after injury: Shock index for the young and age x shock index for the old. J. Surg. Res. 2008, 147, 229–236. [Google Scholar] [PubMed]
- Carsetti, A.; Antolini, R.; Casarotta, E.; Damiani, E.; Gasparri, F.; Marini, B.; Adrario, E.; Donati, A. Shock index as predictor of massive transfusion and mortality in patients with trauma: A systematic review and meta-analysis. Crit. Care 2023, 27, 85. [Google Scholar]
- Kristensen, A.K.; Holler, J.G.; Hallas, J.; Lassen, A.; Shapiro, N.I. Is shock index a valid predictor of mortality in emergency department patients with hypertension, diabetes, high age, or receipt of β- or calcium channel blockers? Ann. Emerg. Med. 2016, 67, 106–113. [Google Scholar] [PubMed]
- Stratton, J.R.; Levy, W.C.; Caldwell, J.H.; Jacobson, A.; May, J.; Matsuoka, D.; Madden, K. Effects of aging on cardiovascular responses to parasympathetic withdrawal. J. Am. Coll. Cardiol. 2003, 41, 2077–2083. [Google Scholar]
- DeMuro, J.P.; Simmons, S.; Jax, J.; Gianelli, S.M. Application of the shock index to the prediction of need for hemostasis intervention. Am. J. Emerg. Med. 2013, 31, 1260–1263. [Google Scholar]
- Rafieezadeh, A.; Prabhakaran, K.; Kirsch, J.; Klein, J.; Shnaydman, I.; Bronstein, M.; Con, J.; Zangbar, B. Shock index is a stronger predictor of outcomes in older compared to younger patients. J. Surg. Res. 2024, 300, 8–14. [Google Scholar]
- Hashmi, A.; Rhee, P.; Pandit, V.; Kulvatunyou, N.; Tang, A.; O’Keeffe, T.; Zangbar, B.; Wynne, J.; Gries, L.; Vercruysse, G.; et al. Shock index predicts mortality in geriatric trauma patients: An analysis of the national trauma data bank. J. Trauma Acute Care Surg. 2014, 76, 1111–1115. [Google Scholar]
- Rossaint, R.; Afshari, A.; Bouillon, B.; Cerny, V.; Cimpoesu, D.; Curry, N.; Duranteau, J.; Filipescu, D.; Grottke, O.; Grønlykke, L.; et al. The european guideline on management of major bleeding and coagulopathy following trauma: Sixth edition. Crit. Care 2023, 27, 80. [Google Scholar]
- Newgard, C.D.; Fischer, P.E.; Gestring, M.; Michaels, H.N.; Jurkovich, G.J.; Lerner, E.B.; Fallat, M.E.; Delbridge, T.R.; Brown, J.B.M.; Bulger, E.M.; et al. National guideline for the field triage of injured patients: Recommendations of the national expert panel on field triage, 2021. J. Trauma Acute Care Surg. 2022, 93, e49–e60. [Google Scholar]
- Heffernan, D.S.; Thakkar, R.K.; Monaghan, S.F.; Ravindran, R.; Adams, C.A., Jr.; Kozloff, M.S.; Gregg, S.C.; Connolly, M.D.; Machan, J.T.; Cioffi, W.G. Normal presenting vital signs are unreliable in geriatric blunt trauma victims. J. Trauma 2010, 69, 813–820. [Google Scholar]
- Lehmann, R.; Beekley, A.; Casey, L.; Salim, A.; Martin, M. The impact of advanced age on trauma triage decisions and outcomes: A statewide analysis. Am. J. Surg. 2009, 97, 571–574. [Google Scholar] [CrossRef] [PubMed]


| Younger Adult (n = 1531) | Older Adult (n = 873) | p-Value | |
|---|---|---|---|
| Age, years | 49.0 (33.0–58.0) | 73.0 (69.0–80.0) | <0.001 |
| Males, n (%) | 1203 (78.6) | 603 (69.1) | <0.001 |
| Mechanism of injury, n (%) | <0.001 | ||
| Traffic accident | 710 (46.4) | 403 (46.2) | |
| Fall from height | 427 (27.9) | 284 (32.5) | |
| Ground-level fall | 36 (2.4) | 57 (6.5) | |
| Struck by object | 100 (6.5) | 32 (3.7) | |
| Cutting or piercing | 238 (15.5) | 78 (8.9) | |
| Others | 20 (1.3) | 19 (2.2) | |
| Time from injury to TC arrival, (min) | 47.0 (35.0–64.0) | 46.5 (35.0–66.0) | 0.839 |
| Time from arrival of EMS on scene to TC arrival, (min) | 9.0 (6.0–13.0) | 9.0 (6.0–13.0) | 0.692 |
| EMS fluid administration, n (%) | 206 (13.5) | 83 (9.5) | 0.058 |
| Admission vital signs | |||
| SBP (mmHg) | 110.0 (90.0–130.0) | 120.0 (90.0–150.0) | <0.001 |
| DBP (mmHg) | 70.0 (60.0–80.0) | 80.0 (60.0–100.0) | <0.001 |
| HR (beats/min) | 92.0 (78.0–11.0) | 87.0 (74.0–101.0) | <0.001 |
| Shock index | 0.85 (0.66–1.14) | 0.70 (0.54–0.95) | <0.001 |
| Shock index > 1, n (%) | 498 (32.5) | 194 (22.2) | <0.001 |
| Age shock index | 37.3 (26.8–52.6) | 51.7 (40.5–73.1) | <0.001 |
| Total Glasgow Coma Scale score | 15.0 (11.0–15.0) | 14.0 (8.0–15.0) | <0.001 |
| Admission laboratory findings | |||
| Hemoglobin (g/dL) | 13.6 (12.3–14.8) | 12.4 (11.0–13.7) | <0.001 |
| Platelet (×103/μL) | 256.0 (214.0–300.0) | 207.0 (168.0–245.3) | <0.001 |
| PT INR | 1.05 (1.00–1.12) | 1.07 (1.01–1.16) | <0.001 |
| pH | 7.39 (7.34–7.43) | 7.41 (7.36–7.45) | <0.001 |
| Lactate (mmol/L) | |||
| >4.0, n (%) | 488 (32.7) | 220 (25.8) | 0.069 |
| AIS ≥ 3 injuries to body regions | |||
| Head | 521 (34.0) | 409 (46.8) | <0.001 |
| Face | 12 (0.8) | 5 (0.6) | 0.553 |
| Neck | 12 (0.8) | 6 (0.7) | 0.792 |
| Thorax | 548 (35.8) | 315 (36.1) | 0.887 |
| Abdomen/Pelvic contents | 234 (15.3) | 98 (11.2) | 0.006 |
| Spine | 126 (8.2) | 81 (9.3) | 0.378 |
| Upper extremities | 59 (3.9) | 21 (2.4) | 0.057 |
| Lower extremities | 324 (21.2) | 149 (17.1) | 0.015 |
| Outcomes of trauma | |||
| ISS | 17.0 (10.0–26.0) | 20.0 (13.0–27.0) | <0.001 |
| ISS ≥ 16, n (%) | 935 (61.1) | 602 (69.0) | <0.001 |
| 1 h PRBC, units | 0 (0–2.0) | 1.0 (0–3.0) | <0.001 |
| 1 h PRBC ≥ 3 units, n (%) | 251 (16.4) | 196 (22.5) | <0.001 |
| 24 h PRBC, units | 1.0 (0–4.0) | 2.0 (0–6.0) | <0.001 |
| 24 h PRBC ≥ 10 units, n (%) | 135 (8.8) | 119 (13.6) | <0.001 |
| In-hospital mortality, n (%) | 118 (7.7) | 215 (24.6) | <0.001 |
| MT (n = 254) | Non-MT (n = 2150) | p-Value | |
|---|---|---|---|
| Age, years | 63.0 (47.8–73.0) | 58.0 (43.0–69.0) | <0.001 |
| Males, n (%) | 182 (71.7) | 1624 (75.5) | 0.192 |
| Mechanism of injury, n (%) | 0.002 | ||
| Traffic accident | 142 (55.9) | 971 (45.2) | |
| Fall from height | 66 (26.0) | 645 (30.0) | |
| Ground-level fall | 3 (1.2) | 90 (4.2) | |
| Struck by object | 19 (7.5) | 113 (5.3) | |
| Cutting or piercing | 21 (8.3) | 295 (13.7) | |
| Others | 3 (1.2) | 36 (1.7) | |
| Time from injury to TC arrival, (min) | 43.0 (33.0–57.0) | 46.0 (34.0–64.0) | 0.008 |
| Time from arrival of EMS on scene to TC arrival, (min) | 8.0 (6.0–12.0) | 9.0 (6.0–13.0) | 0.098 |
| EMS fluid administration, n (%) | 54 (21.3) | 235 (10.9) | <0.001 |
| Admission vital signs | |||
| SBP (mmHg) | 80.0 (60.0–110.0) | 110.0 (90.0–140.0) | <0.001 |
| HR (beats/min) | 104.0 (84.0–122.3) | 89.0 (76.0–105.0) | <0.001 |
| Shock index | 1.3 (0.8–1.7) | 0.8 (0.6–1.0) | <0.001 |
| Shock index category, n (%) | <0.001 | ||
| <0.7 | 45 (17.7) | 842 (39.2) | |
| 0.7–1.0 | 43 (16.9) | 782 (36.4) | |
| >1.0 | 166 (65.4) | 526 (24.5) | |
| Total Glasgow Coma Scale score | 10.0 (5.0–15.0) | 15.0 (11.0–15.0) | <0.001 |
| Admission laboratory findings | |||
| Hemoglobin (g/dL) | 11.4 (10.2–13.0) | 13.4 (12.0–14.6) | <0.001 |
| Platelet (×103/μL) | 206.5 (157.8–251.0) | 241.0 (197.0–284.0) | <0.001 |
| PT INR | 1.21 (1.11–1.37) | 1.04 (0.99–1.11) | <0.001 |
| pH | 7.36 (7.28–7.42) | 7.40 (7.36–7.44) | <0.001 |
| Lactate (mmol/L) | |||
| >4.0, n (%) | 139 (54.7) | 569 (27.1) | <0.001 |
| AIS ≥ 3 injuries to body regions | |||
| Head | 127 (50.0) | 803 (37.3) | <0.001 |
| Face | 6 (2.4) | 11 (0.5) | 0.006 |
| Neck | 3 (1.2) | 15 (0.7) | 0.428 |
| Thorax | 139 (54.7) | 724 (33.7) | <0.001 |
| Abdomen/Pelvic contents | 84 (33.1) | 248 (11.5) | <0.001 |
| Spine | 22 (8.7) | 185 (8.6) | 1.000 |
| Upper extremities | 10 (3.9) | 70 (3.3) | 0.577 |
| Lower extremities | 92 (36.2) | 381 (17.7) | <0.001 |
| Outcomes of trauma | |||
| ISS | 29.0 (22.0–36.0) | 17.0 (10.0–25.0) | <0.001 |
| ISS ≥ 16, n (%) | 236 (92.9) | 1301 (60.5) | <0.001 |
| In-hospital mortality, n (%) | 113 (44.5) | 220 (10.2) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cho, Y.M.; Park, S. Age-Related Disparities in the Predictive Performance of the Shock Index for Massive Transfusion in Trauma Patients: A Retrospective Cohort Study. J. Clin. Med. 2025, 14, 2416. https://doi.org/10.3390/jcm14072416
Cho YM, Park S. Age-Related Disparities in the Predictive Performance of the Shock Index for Massive Transfusion in Trauma Patients: A Retrospective Cohort Study. Journal of Clinical Medicine. 2025; 14(7):2416. https://doi.org/10.3390/jcm14072416
Chicago/Turabian StyleCho, Young Mo, and Sungwook Park. 2025. "Age-Related Disparities in the Predictive Performance of the Shock Index for Massive Transfusion in Trauma Patients: A Retrospective Cohort Study" Journal of Clinical Medicine 14, no. 7: 2416. https://doi.org/10.3390/jcm14072416
APA StyleCho, Y. M., & Park, S. (2025). Age-Related Disparities in the Predictive Performance of the Shock Index for Massive Transfusion in Trauma Patients: A Retrospective Cohort Study. Journal of Clinical Medicine, 14(7), 2416. https://doi.org/10.3390/jcm14072416






