Atypical Femur Fractures—An Analysis of 69 Patients from 15 Years
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Recruitment
2.2. Data Collection
2.3. Statistical Analysis
2.4. Outcome Measures
3. Results
3.1. Patient Demographics
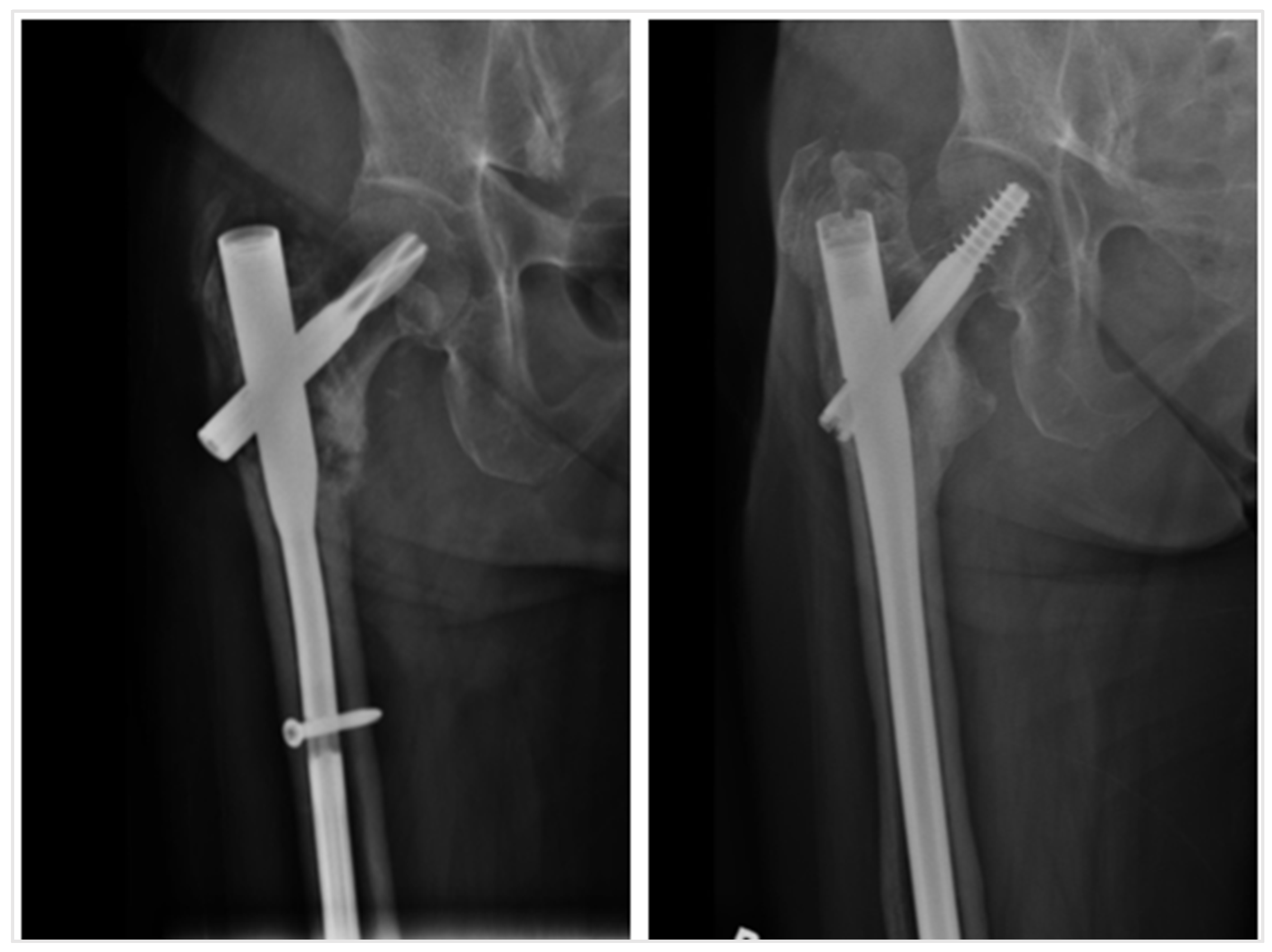
3.2. Fixation Method and Non-Union Rates
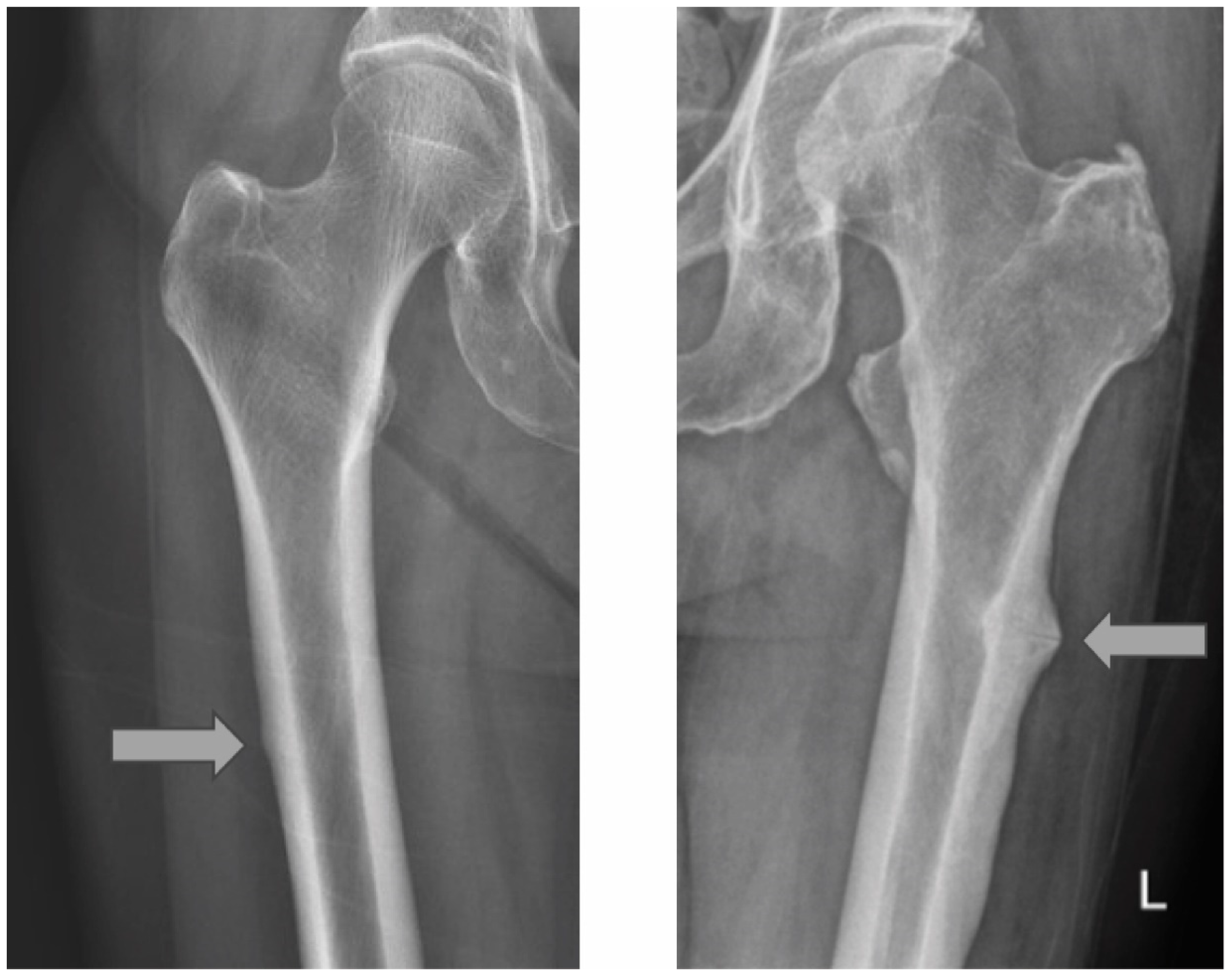
3.3. Location of AFFs and Non-Union Rates
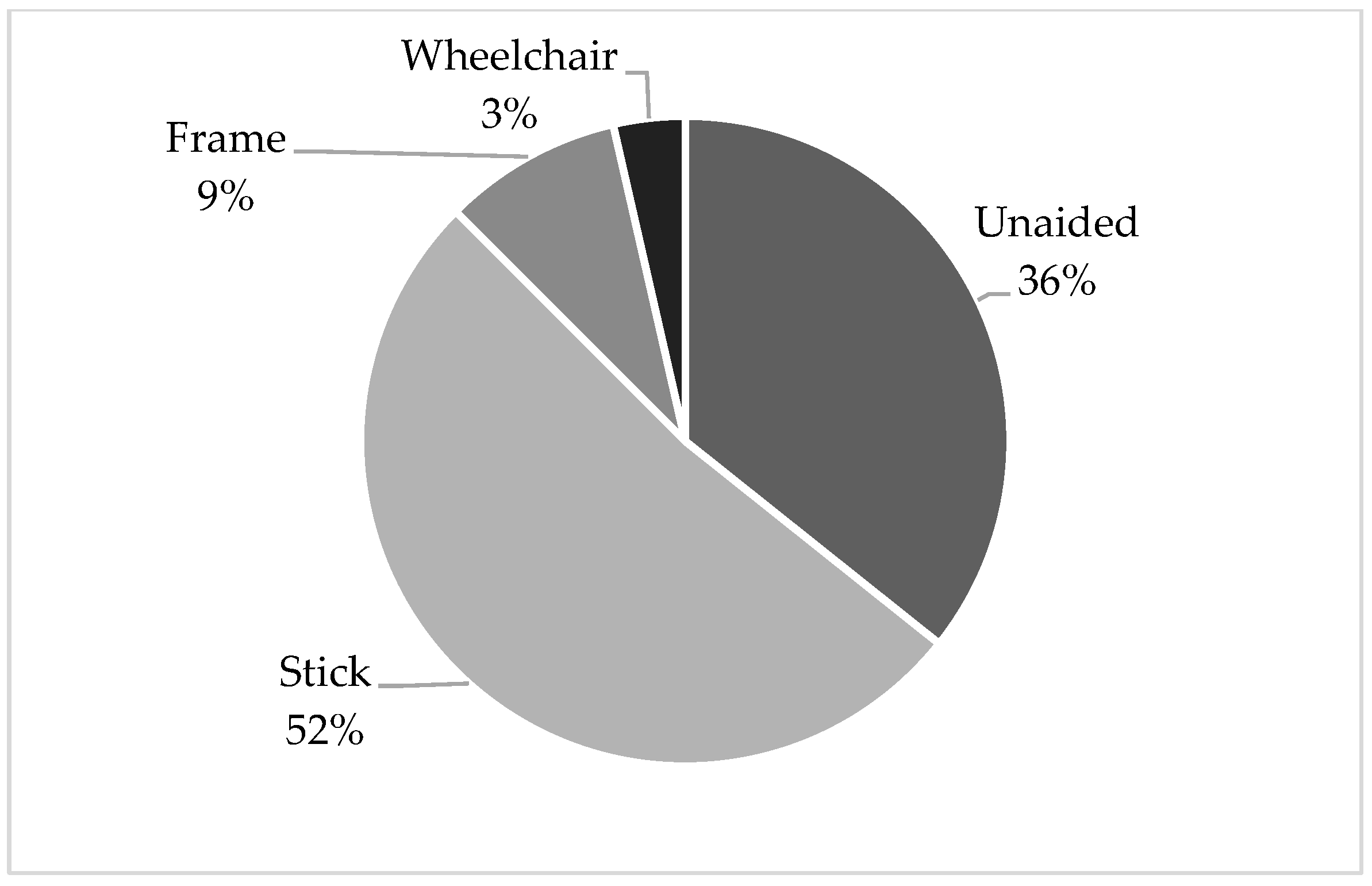
3.4. Mobility Status 1 Year Post-Operation
3.5. Prophylactic Nailing
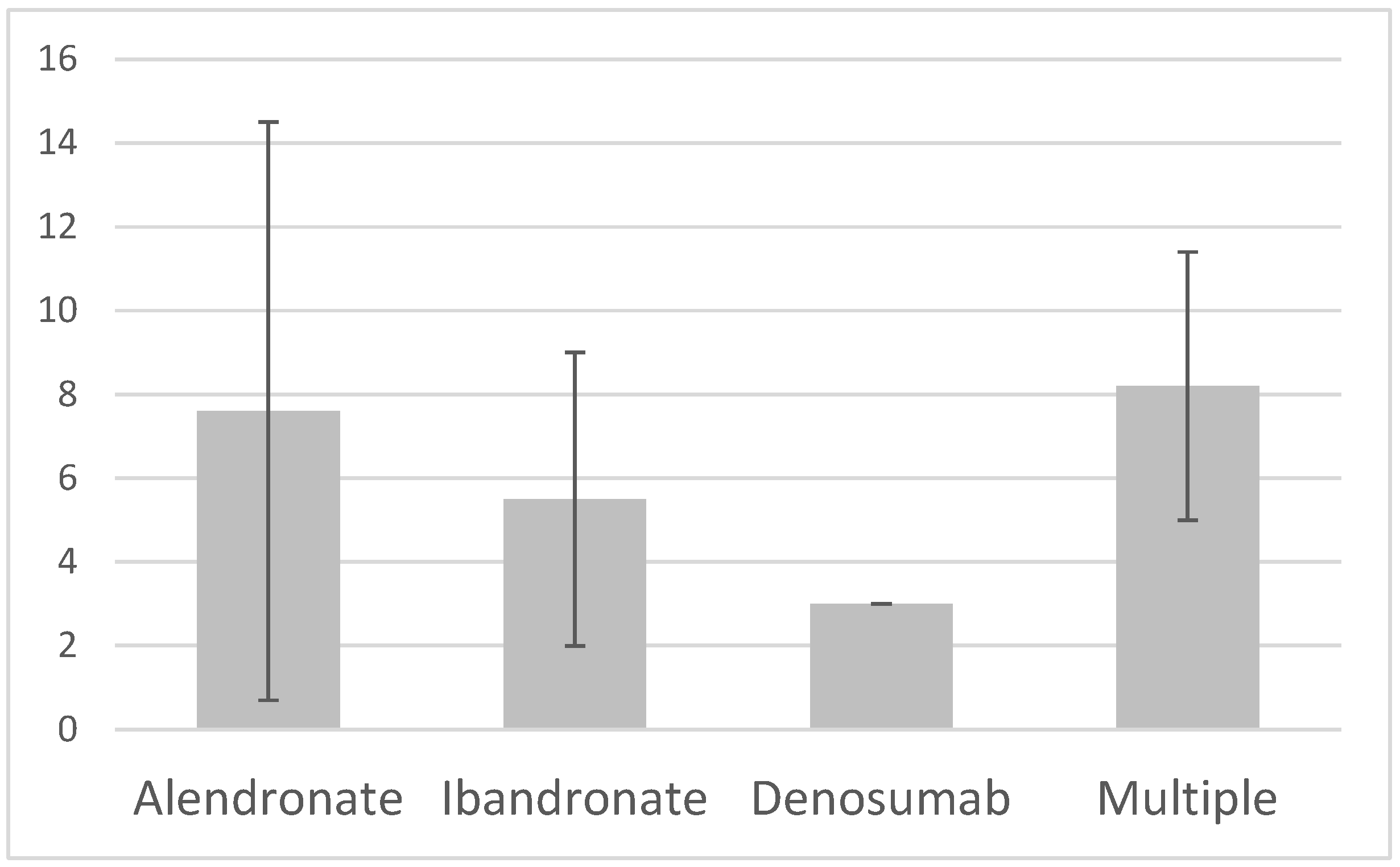
3.6. Pharmacological Agents Used for Osteoporosis
3.7. Drug Holidays
4. Discussion
4.1. Comparable Non-Union Rates in the Literature
4.2. Non-Union Rates Between Diaphyseal and Subtrochanteric AFFs
4.3. Mobility at 1 Year Post-Operation
4.4. Significance of Prophylactic Nailing to the Contralateral Femur
4.5. Time Leading to AFF in Different Anti-Resorptive Agents
4.6. The Importance of Stewardship in the Use of Anti-Resorptive Agents
4.7. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ACCI | Age-Adjusted Charlson Comorbidity Index |
| AFF | Atypical femur fracture |
| CMS | Clinical Management System |
| FLS | Fracture liaison service |
References
- Burge, R.; Dawson-Hughes, B.; Solomon, D.H.; Wong, J.B.; King, A.; Tosteson, A. Incidence and Economic Burden of Osteoporosis-Related Fractures in the United States, 2005–2025. J. Bone Miner. Res. 2007, 22, 465–475. [Google Scholar] [CrossRef] [PubMed]
- Wong, R.M.Y.; Zu, Y.; Chau, W.W.; Tso, C.Y.; Liu, W.H.; Ng, R.W.K.; Chow, S.K.H.; Cheung, W.H.; Tang, N.; Ho, K.K.W. High Charlson Comorbidity Index Score Is Associated with Early Fracture-Related Complication for Internal Fixation of Neck of Femur Fractures. Sci. Rep. 2022, 12, 4749. [Google Scholar] [CrossRef] [PubMed]
- Wong, R.M.Y.; Ko, S.Y.; Chau, W.-W.; Lee, L.C.Y.; Chow, S.K.H.; Cheung, W.H.; Law, S.W. The First Reported Fracture Liaison Service (FLS) for Vertebral Fractures in China: Is Muscle the Missing Gap? Arch. Osteoporos. 2021, 16, 168. [Google Scholar] [CrossRef] [PubMed]
- Wong, R.M.Y.; Law, S.W.; Lee, K.B.; Chow, S.K.H.; Cheung, W.H. Secondary Prevention of Fragility Fractures: Instrumental Role of a Fracture Liaison Service to Tackle the Risk of Imminent Fracture. Hong Kong Med. J. 2019, 25, 235–242. [Google Scholar] [CrossRef]
- Wong, R.M.Y.; Cheung, W.-H.; Chow, S.K.H.; Ng, R.W.K.; Li, W.; Hsu, A.Y.-C.; Wong, K.K.; Ho, A.W.-H.; Choi, S.-H.; Fang, C.X.; et al. Recommendations on the Post-Acute Management of the Osteoporotic Fracture—Patients with “Very-High” Re-Fracture Risk. J. Orthop. Transl. 2022, 37, 94–99. [Google Scholar] [CrossRef]
- Reid, I.R.; Billington, E.O. Drug Therapy for Osteoporosis in Older Adults. Lancet 2022, 399, 1080–1092. [Google Scholar] [CrossRef]
- Dempster, D.W.; Brown, J.P.; Fahrleitner-Pammer, A.; Kendler, D.; Rizzo, S.; Valter, I.; Wagman, R.B.; Yin, X.; Yue, S.V.; Boivin, G. Effects of Long-Term Denosumab on Bone Histomorphometry and Mineralization in Women With Postmenopausal Osteoporosis. J. Clin. Endocrinol. Metab. 2018, 103, 2498–2509. [Google Scholar] [CrossRef]
- Shane, E.; Burr, D.; Abrahamsen, B.; Adler, R.A.; Brown, T.D.; Cheung, A.M.; Cosman, F.; Curtis, J.R.; Dell, R.; Dempster, D.W.; et al. Atypical Subtrochanteric and Diaphyseal Femoral Fractures: Second Report of a Task Force of the American Society for Bone and Mineral Research. J. Bone Miner. Res. 2014, 29, 1–23. [Google Scholar] [CrossRef]
- Black, D.M.; Geiger, E.J.; Eastell, R.; Vittinghoff, E.; Li, B.H.; Ryan, D.S.; Dell, R.M.; Adams, A.L. Atypical Femur Fracture Risk versus Fragility Fracture Prevention with Bisphosphonates. N. Engl. J. Med. 2020, 383, 743–753. [Google Scholar] [CrossRef]
- Iizuka, Y.; Iizuka, H.; Kaneko, T.; Mieda, T.; Takechi, R.; Suzuki, H.; Sorimachi, Y.; Suto, T.; Tachibana, M.; Yoneyama, T.; et al. Bone Turnover Markers and the Factors Associated with Atypical Femur Fractures among Japanese Patients. Injury 2016, 47, 2484–2489. [Google Scholar] [CrossRef]
- Black, D.M.; Abrahamsen, B.; Bouxsein, M.L.; Einhorn, T.; Napoli, N. Atypical Femur Fractures: Review of Epidemiology, Relationship to Bisphosphonates, Prevention, and Clinical Management. Endocr. Rev. 2019, 40, 333–368. [Google Scholar] [CrossRef] [PubMed]
- Donnelly, E.; Saleh, A.; Unnanuntana, A.; Lane, J.M. Atypical Femoral Fractures: Epidemiology, Etiology, and Patient Management. Curr. Opin. Support. Palliat. Care 2012, 6, 348–354. [Google Scholar] [CrossRef] [PubMed]
- Coen, G. Adynamic Bone Disease: An Update and Overview. J. Nephrol. 2005, 18, 117–122. [Google Scholar]
- Haarhaus, M.; Evenepoel, P.; European Renal Osteodystrophy (EUROD) workgroup; Chronic Kidney Disease Mineral and Bone Disorder (CKD-MBD) working group of the European Renal Association–European Dialysis and Transplant Association (ERA-EDTA). Differentiating the Causes of Adynamic Bone in Advanced Chronic Kidney Disease Informs Osteoporosis Treatment. Kidney Int. 2021, 100, 546–558. [Google Scholar] [CrossRef]
- Nguyen, H.H.; Lakhani, A.; Shore-Lorenti, C.; Zebaze, R.; Vincent, A.J.; Milat, F.; Ebeling, P.R. Asian Ethnicity Is Associated with Atypical Femur Fractures in an Australian Population Study. Bone 2020, 135, 115319. [Google Scholar] [CrossRef]
- Lee, Y.-K.; Ahn, S.; Kim, K.M.; Suh, C.S.; Koo, K.-H. Incidence Rate of Atypical Femoral Fracture after Bisphosphonates Treatment in Korea. J. Korean Med. Sci. 2018, 33, e38. [Google Scholar] [CrossRef]
- Abrahamsen, B.; Eiken, P.; Eastell, R. Cumulative Alendronate Dose and the Long-Term Absolute Risk of Subtrochanteric and Diaphyseal Femur Fractures: A Register-Based National Cohort Analysis. J. Clin. Endocrinol. Metab. 2010, 95, 5258–5265. [Google Scholar] [CrossRef]
- Cho, J.-W.; Oh, C.-W.; Leung, F.; Park, K.-C.; Wong, M.K.; Kwek, E.; Kim, H.-J.; Oh, J.-K. Healing of Atypical Subtrochanteric Femur Fractures After Cephalomedullary Nailing: Which Factors Predict Union? J. Orthop. Trauma. 2017, 31, 138–145. [Google Scholar] [CrossRef]
- Yoon, B.-H.; Kim, M.; Roh, Y.H. Does the Nonunion Rate of Atypical Femoral Fractures Differ According to Fracture Site?: A Meta-Analysis. Clin. Orthop. Surg. 2024, 16, 533–541. [Google Scholar] [CrossRef]
- Schultz, D.S.; Gass, H.M.; Barfield, W.R.; Demos, H.A.; Hartsock, L.A. Surgical Complications Associated With Atypical Femur Fractures Attributed to Bisphosphonate Use. J. Surg. Orthop. Adv. 2018, 27, 14–20. [Google Scholar]
- Wong, R.M.Y.; Ho, W.T.; Wai, L.S.; Li, W.; Chau, W.W.; Chow, K.-H.S.; Cheung, W.-H. Fragility Fractures and Imminent Fracture Risk in Hong Kong: One of the Cities with Longest Life Expectancies. Arch. Osteoporos. 2019, 14, 104. [Google Scholar] [CrossRef] [PubMed]
- Wong, R.M.Y.; Qin, J.; Chau, W.W.; Tang, N.; Tso, C.Y.; Wong, H.W.; Chow, S.K.-H.; Leung, K.-S.; Cheung, W.-H. Prognostic Factors Related to Ambulation Deterioration after 1-Year of Geriatric Hip Fracture in a Chinese Population. Sci. Rep. 2021, 11, 14650. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.-J.; Yoo, J.J.; Oh, K.-J.; Yoo, J.-H.; Rhyu, K.H.; Nam, K.W.; Suh, D.-H. Surgical Outcome of Intramedullary Nailing in Patients with Complete Atypical Femoral Fracture: A Multicenter Retrospective Study. Injury 2017, 48, 941–945. [Google Scholar] [CrossRef] [PubMed]
- Koh, A.; Guerado, E.; Giannoudis, P.V. Atypical Femoral Fractures Related to Bisphosphonate Treatment: Issues and Controversies Related to Their Surgical Management. Bone Jt. J. 2017, 99-B, 295–302. [Google Scholar] [CrossRef]
- Fang, C.; Shen, W.Y.; Wong, J.S.H.; Yee, D.K.-H.; Yung, C.S.-Y.; Fang, E.; Lai, Y.S.; Woo, S.B.; Cheung, J.; Chau, J.Y.-M.; et al. Should Nails Be Locked Dynamically or Statically in Atypical Femoral Fractures?—A Radiological Analysis of Time to Union and Reoperations in 236 Displaced Fractures with 4 Years Average Follow-Up. Injury 2023, 54, 110909. [Google Scholar] [CrossRef]
- Wu, C.C. The Effect of Dynamization on Slowing the Healing of Femur Shaft Fractures after Interlocking Nailing. J. Trauma 1997, 43, 263–267. [Google Scholar] [CrossRef]
- Wu, C.C.; Shih, C.H. Effect of Dynamization of a Static Interlocking Nail on Fracture Healing. Can. J. Surg. 1993, 36, 302–306. [Google Scholar]
- Pihlajamäki, H.K.; Salminen, S.T.; Böstman, O.M. The Treatment of Nonunions Following Intramedullary Nailing of Femoral Shaft Fractures. J. Orthop. Trauma 2002, 16, 394–402. [Google Scholar] [CrossRef]
- Lynch, J.R.; Taitsman, L.A.; Barei, D.P.; Nork, S.E. Femoral Nonunion: Risk Factors and Treatment Options. J. Am. Acad. Orthop. Surg. 2008, 16, 88–97. [Google Scholar] [CrossRef]
- Wolinsky, P.R.; McCarty, E.; Shyr, Y.; Johnson, K. Reamed Intramedullary Nailing of the Femur: 551 Cases. J. Trauma 1999, 46, 392–399. [Google Scholar] [CrossRef]
- Vaughn, J.; Gotha, H.; Cohen, E.; Fantry, A.J.; Feller, R.J.; Van Meter, J.; Hayda, R.; Born, C.T. Nail Dynamization for Delayed Union and Nonunion in Femur and Tibia Fractures. Orthopedics 2016, 39, e1117–e1123. [Google Scholar] [CrossRef] [PubMed]
- Papakostidis, C.; Psyllakis, I.; Vardakas, D.; Grestas, A.; Giannoudis, P.V. Femoral-Shaft Fractures and Nonunions Treated with Intramedullary Nails: The Role of Dynamisation. Injury 2011, 42, 1353–1361. [Google Scholar] [CrossRef] [PubMed]
- Basumallick, M.N.; Bandopadhyay, A. Effect of Dynamization in Open Interlocking Nailing of Femoral Fractures. A Prospective Randomized Comparative Study of 50 Cases with a 2-Year Follow-Up. Acta Orthop. Belg. 2002, 68, 42–48. [Google Scholar] [PubMed]
- Tigani, D.; Fravisini, M.; Stagni, C.; Pascarella, R.; Boriani, S. Interlocking Nail for Femoral Shaft Fractures: Is Dynamization Always Necessary? Int. Orthop. 2005, 29, 101–104. [Google Scholar] [CrossRef]
- Kim, S.M.; Rhyu, K.H.; Lim, S.J. Salvage of Failed Osteosynthesis for an Atypical Subtrochanteric Femoral Fracture Associated with Long-Term Bisphosphonate Treatment Using a 95° Angled Blade Plate. Bone Jt. J. 2018, 100-B, 1511–1517. [Google Scholar] [CrossRef]
- Oh, C.-W.; Oh, J.-K.; Park, K.-C.; Kim, J.-W.; Yoon, Y.-C. Prophylactic Nailing of Incomplete Atypical Femoral Fractures. Sci. World J. 2013, 2013, 450148. [Google Scholar] [CrossRef]
- Min, B.-W.; Koo, K.-H.; Park, Y.-S.; Oh, C.-W.; Lim, S.-J.; Kim, J.-W.; Lee, K.-J.; Lee, Y.-K. Scoring System for Identifying Impending Complete Fractures in Incomplete Atypical Femoral Fractures. J. Clin. Endocrinol. Metab. 2017, 102, 545–550. [Google Scholar] [CrossRef]
- Saita, Y.; Ishijima, M.; Kaneko, K. Atypical Femoral Fractures and Bisphosphonate Use: Current Evidence and Clinical Implications. Ther. Adv. Chronic Dis. 2015, 6, 185–193. [Google Scholar] [CrossRef]
- Odvina, C.V.; Zerwekh, J.E.; Rao, D.S.; Maalouf, N.; Gottschalk, F.A.; Pak, C.Y.C. Severely Suppressed Bone Turnover: A Potential Complication of Alendronate Therapy. J. Clin. Endocrinol. Metab. 2005, 90, 1294–1301. [Google Scholar] [CrossRef]
- Zanchetta, M.B.; Diehl, M.; Buttazzoni, M.; Galich, A.; Silveira, F.; Bogado, C.E.; Zanchetta, J.R. Assessment of Bone Microarchitecture in Postmenopausal Women on Long-Term Bisphosphonate Therapy With Atypical Fractures of the Femur. J. Bone Miner. Res. 2014, 29, 999–1004. [Google Scholar] [CrossRef]
- Reid, I.R. Bisphosphonate Holidays. Drug Ther. Bull. 2021, 59, 35–36. [Google Scholar] [CrossRef] [PubMed]
- Naylor, K.E.; Bradburn, M.; Paggiosi, M.A.; Gossiel, F.; Peel, N.F.A.; McCloskey, E.V.; Walsh, J.S.; Eastell, R. Effects of Discontinuing Oral Bisphosphonate Treatments for Postmenopausal Osteoporosis on Bone Turnover Markers and Bone Density. Osteoporos. Int. 2018, 29, 1407–1417. [Google Scholar] [CrossRef] [PubMed]
- Curtis, J.R.; Saag, K.G.; Arora, T.; Wright, N.C.; Yun, H.; Daigle, S.; Matthews, R.; Delzell, E. Duration of Bisphosphonate Drug Holidays and Associated Fracture Risk. Med. Care 2020, 58, 419–426. [Google Scholar] [CrossRef] [PubMed]
- Adler, R.A. Treating Osteoporosis in Patients with Atypical Femoral Fracture. J. Bone Miner. Res. 2024, 39, 1711–1715. [Google Scholar] [CrossRef]
- van de Laarschot, D.M.; McKenna, M.J.; Abrahamsen, B.; Langdahl, B.; Cohen-Solal, M.; Guañabens, N.; Eastell, R.; Ralston, S.H.; Zillikens, M.C. Medical Management of Patients After Atypical Femur Fractures: A Systematic Review and Recommendations From the European Calcified Tissue Society. J. Clin. Endocrinol. Metab. 2020, 105, 1682–1699. [Google Scholar] [CrossRef]
| Characteristics | Total Cases (n = 69) |
|---|---|
| Age (years) a | 73.8 ± 9.7 |
| Female | 65 (94.2%) |
| BMI | 23.8 ± 3.9 kg/m2 |
| Current smoker | 5 (7.2%) |
| Diabetes mellitus | 15 (21.7%) |
| Heart failure | 3 (4.3%) |
| Chronic kidney disease | 3 (4.3%) |
| Malignancy b | 6 (8.7%) |
| ACCI c | 3.4 ± 1.2 |
| History of anti-resorptive agent use | 66 (95.6%) |
| Indication for anti-resorptive agent | |
| Primary osteoporosis | 53 (76.8%) |
| Fragility fracture | 7 (10.1%) |
| Union | Non-Union | Total | |
|---|---|---|---|
| Long cephalomedullary device | 51 (98.1%) | 1 (1.9%) | 52 |
| Short cephalomedullary device | 14 (87.5%) | 2 (12.5%) | 16 |
| Plate with screws | 0 (0%) | 1 (100%) | 1 |
| Total | 65 (94.2%) | 4 (5.8%) | 69 |
| Union | Non-Union | Total | |
|---|---|---|---|
| Subtrochanteric | 44 (93.6%) | 3 (6.4%) | 47 |
| Diaphyseal | 21 (95.5%) | 1 (4.5%) | 22 |
| Total | 65 (94.2%) | 4 (5.8%) | 69 |
| Total Cases (n = 69) | |
|---|---|
| Cases with documented use of anti-resorptive drugs | 66 (95.6%) |
| Type of anti-resorptive agent | |
| Alendronate only | 29 (42.0%) |
| Ibandronate only | 6 (8.6%) |
| Denosumab only | 3 (4.3%) |
| History of using more than one drug | 10 (14.4%) |
| Unknown | 18 (26.1%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kwan, C.K.; Tang, N.; Fong, M.K.; Liu, W.H.; Tso, C.Y.; Liu, C.; Wong, P.Y.; Zhang, N.; Cheung, W.H.; Wong, R.M.Y. Atypical Femur Fractures—An Analysis of 69 Patients from 15 Years. J. Clin. Med. 2025, 14, 2404. https://doi.org/10.3390/jcm14072404
Kwan CK, Tang N, Fong MK, Liu WH, Tso CY, Liu C, Wong PY, Zhang N, Cheung WH, Wong RMY. Atypical Femur Fractures—An Analysis of 69 Patients from 15 Years. Journal of Clinical Medicine. 2025; 14(7):2404. https://doi.org/10.3390/jcm14072404
Chicago/Turabian StyleKwan, Cheuk Kin, Ning Tang, Man Ki Fong, Wing Hong Liu, Chi Yin Tso, Chaoran Liu, Pui Yan Wong, Ning Zhang, Wing Hoi Cheung, and Ronald Man Yeung Wong. 2025. "Atypical Femur Fractures—An Analysis of 69 Patients from 15 Years" Journal of Clinical Medicine 14, no. 7: 2404. https://doi.org/10.3390/jcm14072404
APA StyleKwan, C. K., Tang, N., Fong, M. K., Liu, W. H., Tso, C. Y., Liu, C., Wong, P. Y., Zhang, N., Cheung, W. H., & Wong, R. M. Y. (2025). Atypical Femur Fractures—An Analysis of 69 Patients from 15 Years. Journal of Clinical Medicine, 14(7), 2404. https://doi.org/10.3390/jcm14072404








