Investigating the Impact of Acetabular Dysplasia on Sexual Dysfunction and Psychological Well-Being in Women
Abstract
1. Introduction
2. Materials and Methods
2.1. Power Analysis
2.2. Statistical Analysis
3. Results
4. Discussion
5. Limitations and Future Plans
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Breidel, K.E.; Coobs, B.R. Evaluating and managing acetabular dysplasia in adolescents and young adults. JAAPA 2019, 32, 32–37. [Google Scholar] [CrossRef]
- Simionescu, A.A.; Cirstoiu, M.M.; Cirstoiu, C.; Stanescu, A.M.A.; Crețu, B. Current evidence about developmental dysplasia of the hip in pregnancy. Medicina 2021, 57, 655. [Google Scholar] [CrossRef] [PubMed]
- Loder, R.T.; Skopelja, E.N. The epidemiology and demographics of hip dysplasia. Int. Sch. Res. Notices 2011, 2011, 238607. [Google Scholar]
- Brockwell, J.; O’Hara, J.N.; Young, D.A. Acetabular dysplasia: Aetiological classification. In Hip Joint Restoration: Worldwide Advances in Arthroscopy, Arthroplasty, Osteotomy and Joint Preservation Surgery; Springer: New York, NY, USA, 2017; pp. 631–642. [Google Scholar]
- Wilkin, G.P.; Ibrahim, M.M.; Smit, K.M.; Beaulé, P.E. A contemporary definition of hip dysplasia and structural instability: Toward a comprehensive classification for acetabular dysplasia. J. Arthroplasty 2017, 32, S20–S27. [Google Scholar] [PubMed]
- Sankar, W.N.; Duncan, S.T.; Baca, G.R.; Beaulé, P.E.; Millis, M.B.; Kim, Y.J.; Peters, C.L.; Podeszwa, D.A.; Schoenecker, P.L.; Sierra, R.J.; et al. Descriptive epidemiology of acetabular dysplasia: The Academic Network of Conservational Hip Outcomes Research (ANCHOR) periacetabular osteotomy. JAAOS-J. Am. Acad. Orthop. Surg. 2017, 25, 150–159. [Google Scholar] [CrossRef] [PubMed]
- Nunley, R.M.; Prather, H.; Hunt, D.; Schoenecker, P.L.; Clohisy, J.C. Clinical presentation of symptomatic acetabular dysplasia in skeletally mature patients. J. Bone Jt. Surg. Am. 2011, 93 (Suppl. S2), 17–21. [Google Scholar] [CrossRef]
- Burnett, R.S.J.; Della Rocca, G.; Prather, H.; Curry, M.; Maloney, W.J.; Clohisy, J.C. Clinical presentation of patients with tears of the acetabular labrum. J. Bone Jt. Surg. Am. 2006, 88, 1448–1457. [Google Scholar] [CrossRef]
- Gambling, T.S.; Long, A. Psycho-social impact of developmental dysplasia of the hip and of differential access to early diagnosis and treatment: A narrative study of young adults. SAGE Open Med. 2019, 7, 2050312119836010. [Google Scholar] [CrossRef]
- Gatchel, R.J. A biopsychosocial overview of pretreatment screening of patients with pain. Clin. J. Pain. 2001, 17, 192–199. [Google Scholar] [CrossRef]
- Dezateux, C.; Rosendahl, K. Developmental dysplasia of the hip. Lancet 2007, 369, 1541–1552. [Google Scholar] [CrossRef]
- Prather, H.; Dugan, S.; Fitzgerald, C.; Hunt, D. Review of anatomy, evaluation, and treatment of musculoskeletal pelvic floor pain in women. PMR 2009, 1, 346–358. [Google Scholar]
- Shankar, D.S.; Ramos, N.L.; Dold, A.P.; Cichelli, K.A.; Youm, T. Pelvic Floor Dysfunction from an Orthopedic Perspective: A Review of the Literature. SN Compr. Clin. Med. 2022, 4, 249. [Google Scholar] [CrossRef]
- Verbeek, M.; Hayward, L. Pelvic floor dysfunction and its effect on quality of sexual life. Sex. Med. Rev. 2019, 7, 559–564. [Google Scholar]
- Schussler, E.E.; Weatherton, M.; Chen Musgrove, M.M.; Brigati, J.R.; England, B.J. Student perceptions of instructor supportiveness: What characteristics make a difference? CBE Life Sci. Educ. 2021, 20, ar29. [Google Scholar] [PubMed]
- Falkenhorst, J.; Hamacher, R.; Bauer, S. New therapeutic agents in gastrointestinal stromal tumours. Curr. Opin. Oncol. 2019, 31, 322–328. [Google Scholar] [PubMed]
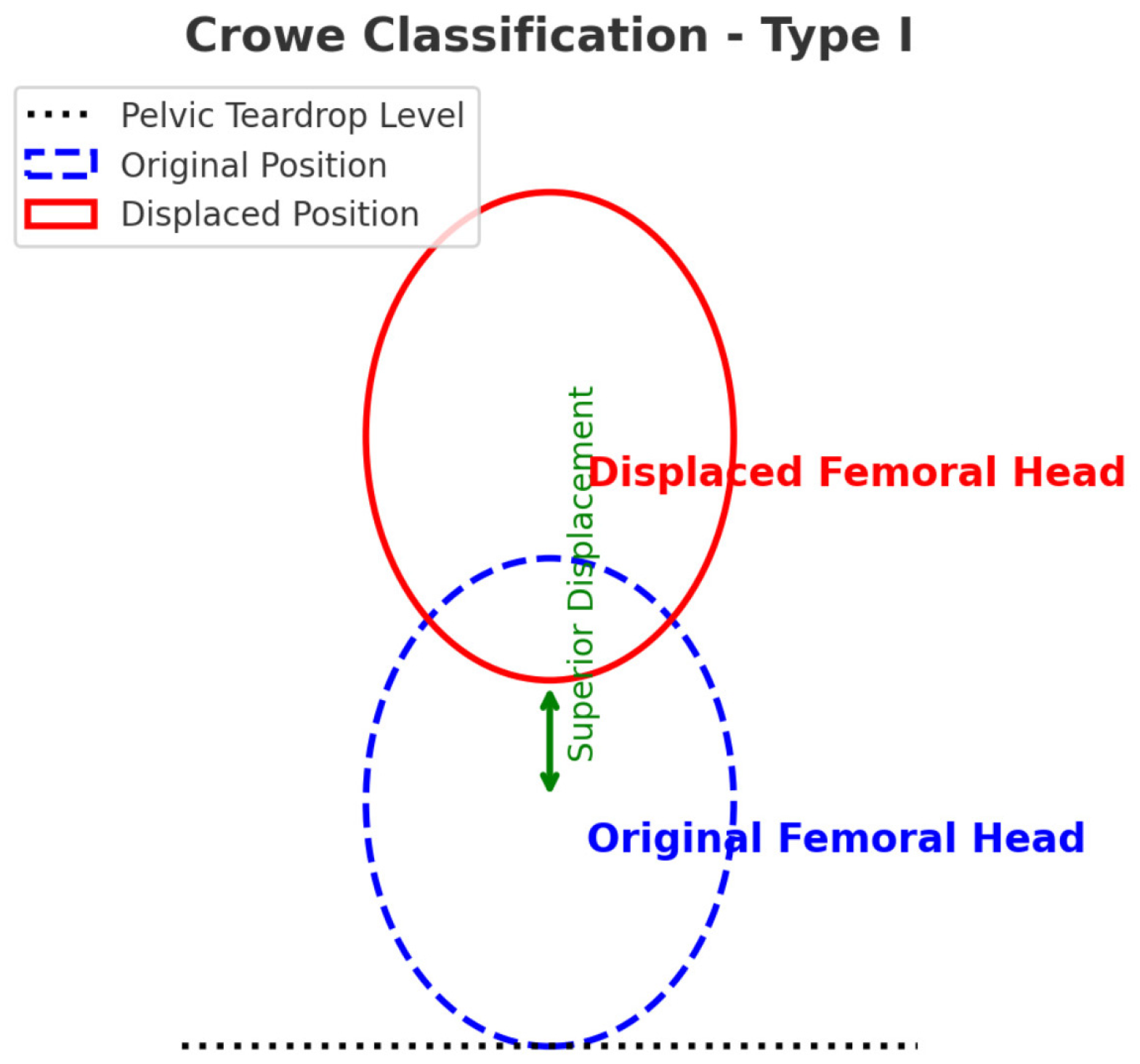
- Amstutz, H.C.; Antoniades, J.T.; Le Duff, M.J. Results of metal-on-metal hybrid hip resurfacing for Crowe type-I and II developmental dysplasia. J. Bone Jt. Surg. Am. 2007, 89, 339–346. [Google Scholar]
- Rust, J.; Golombok, S. The GRISS: A psychometric instrument for the assessment of sexual dysfunction. Arch. Sex. Behav. 1986, 15, 157–165. [Google Scholar] [CrossRef]
- Beck, A.T.; Epstein, N.; Brown, G.; Steer, R.A. An inventory for measuring clinical anxiety: Psychometric properties. J. Consult. Clin. Psychol. 1988, 56, 893. [Google Scholar]
- De Hundt, M.; Vlemmix, F.; Bais, J.; Hutton, E.K.; de Groot, C.J.; Mol, B.W.; Kok, M. Risk factors for developmental dysplasia of the hip: A meta-analysis. Eur. J. Obstet. Gynecol. Reprod. Biol. 2012, 165, 8–17. [Google Scholar] [CrossRef]
- Ganz, R.; Parvizi, J.; Beck, M.; Leunig, M.; Nötzli, H.; Siebenrock, K.A. Femoroacetabular impingement: A cause for osteoarthritis of the hip. Clin. Orthop. Relat. Res. 2003, 417, 112–120. [Google Scholar]
- Jacobsen, J.S.; Nielsen, D.B.; Sørensen, H.; Søballe, K.; Mechlenburg, I. Changes in walking and running in patients with hip dysplasia. Acta Orthop. 2013, 84, 265–270. [Google Scholar]
- Agricola, R.; Heijboer, M.P.; Bierma-Zeinstra, S.M.; Verhaar, J.A.; Weinans, H.; Waarsing, J.H. Cam impingement causes osteoarthritis of the hip: A nationwide prospective cohort study (CHECK). Ann. Rheum. Dis. 2013, 72, 918–923. [Google Scholar] [PubMed]
- Safran, M.R. Microinstability of the hip—Gaining acceptance. JAAOS-J. Am. Acad. Orthop. Surg. 2019, 27, 12–22. [Google Scholar]
- Yoon, B.-H.; Lee, K.-H.; Noh, S.; Ha, Y.C.; Lee, Y.K.; Koo, K.H. Sexual activity after total hip replacement in Korean patients: How they do, what they want, and how to improve. Clin. Orthop. Surg. 2013, 5, 269–277. [Google Scholar]
- Valenzuela, R.G.; Cabanela, M.E.; Trousdale, R.T. Sexual activity, pregnancy, and childbirth after periacetabular osteotomy. Clin. Orthop. Relat. Res. 2004, 418, 146–152. [Google Scholar]
- Masui, T.; Hasegawa, Y.; Yamaguchi, J.; Kanoh, T.; Ishiguro, N. Childbirth and sexual activity after eccentric rotational acetabular osteotomy. Clin. Orthop. Relat. Res. 2007, 459, 195–199. [Google Scholar] [PubMed]
- Klit, J.; Hartig-Andrease, C.; Jacobsen, S.; Søballe, K.; Troelsen, A. Periacetabular osteotomy: Sporting, social and sexual activity 9-12 years post surgery. Hip Int. 2014, 24, 27–31. [Google Scholar]
- Neonakis, E.; Perna, F.; Traina, F.; Faldini, O.; Antoniou, G.; Kyriakopoulos, G.; Triantafyllopoulos, I.K.; Megaloikonomos, P.D.; Faldini, C. Total hip arthroplasty and sexual activity: A systematic review. Musculoskelet. Surg. 2020, 104, 17–24. [Google Scholar]
- Niedenfuehr, J.; Stevens, D.M. A scoping review: Sexual activity and functioning before and after surgery for femoroacetabular impingement (FAI), labral tears, and hip dysplasia. Sex. Med. Rev. 2023, 11, 349–358. [Google Scholar]
- Basile, G. The autobiographical narrative as a damage assessment means: Injuries to profound subjective sensitivities–personalization and objectivization of medicolegal relevance. Clin. Ter. 2022, 173, 585–589. [Google Scholar]
- Nisar, A.; Augustine, A.; Horrey, L.; Craig, D.; Meek, R.; Patil, S. Psychosocial aspects of hip disease in the young adult. Hip Int. 2013, 23, 417–423. [Google Scholar] [CrossRef] [PubMed]
- Reddy, N.; Martinez, J.R.; Mulligan, E.; Nakonezny, P.; Wells, J. Sleep quality and nocturnal pain in patients with femoroacetabular impingement and acetabular dysplasia. BMC Musculoskelet. Disord. 2020, 21, 1–7. [Google Scholar]
- Foster, S.N.; Spitznagle, T.M.; Tuttle, L.J.; Sutcliffe, S.; Steger-May, K.; Lowder, J.L.; Meister, M.R.; Ghetti, C.; Wang, J.; Mueller, M.J.; et al. Hip and Pelvic floor muscle strength in women with and without urgency and frequency-predominant lower urinary tract symptoms. J. Womens Health Phys. Therap. 2021, 45, 126–134. [Google Scholar] [CrossRef]
- Kwan, K.S.; Roberts, L.J.; Swalm, D.M. Sexual dysfunction and chronic pain: The role of psychological variables and impact on quality of life. Eur. J. Pain. 2005, 9, 643–652. [Google Scholar] [CrossRef]
- Jacobsen, J.S.; Søballe, K.; Thorborg, K.; Bolvig, L.; Storgaard Jakobsen, S.; Hölmich, P.; Mechlenburg, I. Patient-reported outcome and muscle–tendon pain after periacetabular osteotomy are related: 1-year follow-up in 82 patients with hip dysplasia. Acta Orthop. 2019, 90, 40–45. [Google Scholar] [PubMed]
- Incze-Bartha, Z.; Incze-Bartha, S.; Simon-Szabó, Z.; Feier, A.M.; Vunvulea, V.; Nechifor-Boila, A.I.; Pastorello, Y.; Denes, L. Finite element analysis of various osteotomies used in the treatment of developmental hip dysplasia in children. J. Pers. Med. 2024, 14, 189. [Google Scholar] [CrossRef]
- Clohisy, J.C.; Ackerman, J.; Baca, G.; Baty, J.; Beaulé, P.E.; Kim, Y.J.; Millis, M.B.; Podeszwa, D.A.; Schoenecker, P.L.; Sierra, R.J.; et al. Patient-reported outcomes of periacetabular osteotomy from the prospective ANCHOR cohort study. J. Bone Jt. Surg. Am. 2017, 99, 33–41. [Google Scholar] [CrossRef]
- Machrowska, A.; Karpiński, R.; Maciejewski, M.; Jonak, J.; Krakowski, P. Application of eemd-dfa algorithms and ann classification for detection of knee osteoarthritis using vibroarthrography. Appl. Comput. Sci. 2024, 20, 90–108. [Google Scholar]

| AD Positive (n = 55) | AD Negative (n = 70) | p | |
|---|---|---|---|
| Age, mean, SD (years) | 45.58 ± 14.09 | 46.17 ± 14.25 | 0.72 |
| Osteoarthritis, n (%) | 23 (41.8) | 13 (18.5) | 0.012 |
| Osteonecrosis of the femoral head | 3 (5.4) | 2 (2.8) | 0.116 |
| Developmental hip dysplasia | 6 (10.8) | 3 (4.2) | 0.102 |
| Legg–Calvé–Perthes disease | 2 (3.6) | 1 (1.4) | 0.385 |
| Sequelae of septic arthritis | 7 (12.7) | 2 (2.8) | 0.014 |
| VAS score, mean ± SD | 8.15 ± 1.1 | 1.26 ± 1.06 | <0.001 |
| Beck Depression Inventory Score ± SD | 12.3 ± 11.0 | 6.1 ± 6.7 | 0.02 |
| AD Positive Mean ± SD (n = 55) | AD Negative Mean ± SD (n = 70) | p | |
|---|---|---|---|
| Extension | 15.6 ± 4.6 | 16.9 ± 6.8 | 0.2 |
| Flexion | 137.1 ± 8.4 | 119.7 ± 7.9 | <0.001 |
| Abduction | 44.1 ± 5.01 | 44.25 ± 5.3 | 0.9 |
| Adduction | 13.1 ± 2.8 | 10.3 ± 3.8 | <0.001 |
| Internal rotation | 49.8 ± 7.7 | 45.8 ± 6.1 | 0.1 |
| External rotation | 47.8 ± 6.9 | 50.25 ± 12.75 | <0.001 |
| AD Positive Mean ± SD (n = 55) | AD Negative Mean ± SD (n = 70) | p | |
|---|---|---|---|
| Frequency | 3.3 ± 1.5 | 4.01 ± 1.8 | 0.04 |
| Communication | 2.76 ± 2.1 | 2.54 ± 1.9 | 0.46 |
| Satisfaction | 6.15 ± 2.08 | 6.75 ± 2.71 | 0.32 |
| Avoidance | 5.15 ± 4.16 | 4.32 ± 3.62 | 0.21 |
| Touch | 7.55 ± 1.70 | 8.27 ± 1.75 | 0.03 |
| Vaginismus | 6.03 ± 3.36 | 5.42 ± 2.76 | 0.2 |
| Anorgasmia | 7.03 ± 3.68 | 5.15 ± 2.86 | 0.01 |
| Total | 37.97 ± 18,58 | 36.56 ± 17.4 | 0.03 |
| B | OR | 95% CI | p | |
|---|---|---|---|---|
| Age | 0.18 ± 0.04 | 4.6 | 0.1 ± 0.2 | 0.01 |
| BMI | 0.35 ± 0.06 | 5.2 | 0.2 ± 0.4 | 0.01 |
| Birth history | −6.15 ± 2.08 | 0.3 | −0.5 ± 0.4 | 0.76 |
| Osteoarthritis | 0.45 ± 0.08 | 3.8 | 0.3 ± 0.5 | 0.04 |
| Osteonecrosis of the femoral head | 0.62 ± 0.09 | 2.9 | 0.4 ± 0.6 | 0.02 |
| Developmental hip dysplasia | 1.10 ± 0.12 | 6.5 | 0.8 ± 1.2 | 0.01 |
| Legg–Calvé–Perthes disease | 0.75 ± 0.10 | 3.2 | 0.5 ± 0.9 | 0.03 |
| Sequelae of septic arthritis | 0.92 ± 0.11 | 4.1 | 0.7 ± 1.0 | 0.05 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ağlamış, Ö.; Akkaya, S.K.; Erol, B.; Yılmaz Ergani, S. Investigating the Impact of Acetabular Dysplasia on Sexual Dysfunction and Psychological Well-Being in Women. J. Clin. Med. 2025, 14, 2385. https://doi.org/10.3390/jcm14072385
Ağlamış Ö, Akkaya SK, Erol B, Yılmaz Ergani S. Investigating the Impact of Acetabular Dysplasia on Sexual Dysfunction and Psychological Well-Being in Women. Journal of Clinical Medicine. 2025; 14(7):2385. https://doi.org/10.3390/jcm14072385
Chicago/Turabian StyleAğlamış, Özgür, Selver Kübra Akkaya, Burcu Erol, and Seval Yılmaz Ergani. 2025. "Investigating the Impact of Acetabular Dysplasia on Sexual Dysfunction and Psychological Well-Being in Women" Journal of Clinical Medicine 14, no. 7: 2385. https://doi.org/10.3390/jcm14072385
APA StyleAğlamış, Ö., Akkaya, S. K., Erol, B., & Yılmaz Ergani, S. (2025). Investigating the Impact of Acetabular Dysplasia on Sexual Dysfunction and Psychological Well-Being in Women. Journal of Clinical Medicine, 14(7), 2385. https://doi.org/10.3390/jcm14072385






