The Utility of Blood Cultures in Non-Febrile Patients and Patients with Antibiotics Therapy in Internal Medicine Departments
Abstract
1. Background
2. Methodology
2.1. Search Strategy
2.2. Study Design
2.3. Study Settings
2.4. Definitions
2.5. Statistical Analysis
3. Results
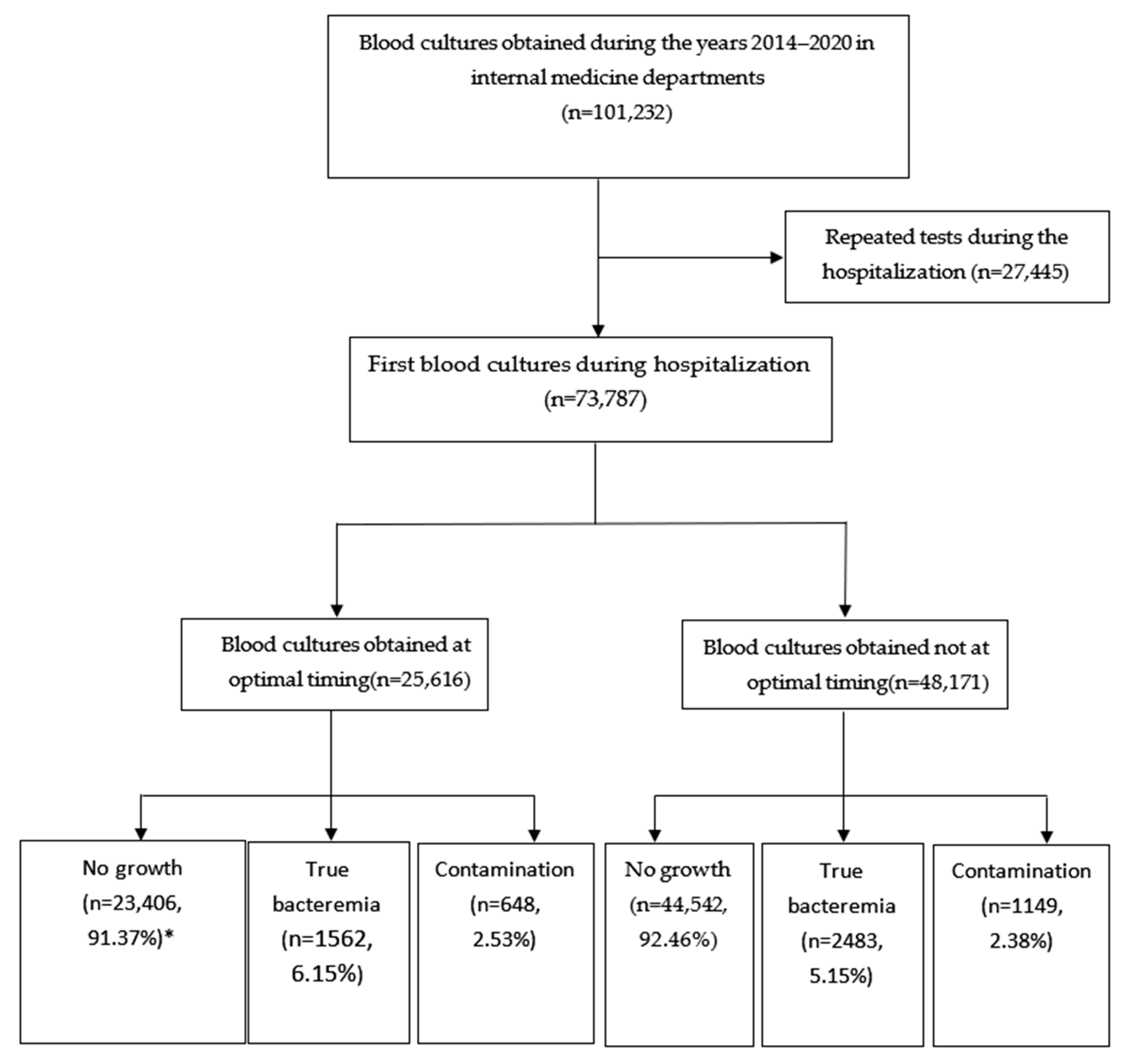
3.1. Patient Population
3.2. Bacteriological Results
3.3. Multivariable Analysis
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tabriz, M.S.; Riederer, K.; Baran, J., Jr.; Khatib, R. Repeating blood cultures during hospital stay: Practice pattern at a teaching hospital and a proposal for guidelines. Clin. Microbiol. Infect. 2004, 10, 624–627. [Google Scholar] [PubMed]
- Thomson, R.B.; Corbin, C.; Tan, J.S. Timing of Blood Culture Collection from Febrile Patients, Abstract C-227. In Proceedings of the Abstracts of the 89th Annual Meeting of the American Society for Microbiology, New Orleans, LA, USA, 14–19 May 1989; American Society for Microbiology: Washington, DC, USA, 1989; p. 431. [Google Scholar]
- Riedel, S.; Bourbeau, P.; Swartz, B.; Brecher, S.; Carroll, K.C.; Stamper, P.D.; Dunne, W.M.; McCardle, T.; Walk, N.; Fiebelkorn, K.; et al. Timing of specimen collection for blood cultures from febrile patients with bacteremia. J. Clin. Microbiol. 2008, 46, 1381–1385. [Google Scholar] [CrossRef] [PubMed]
- Kee, P.P.L.; Chinnappan, M.; Nair, A.; Yeak, D.; Chen, A.; Starr, M.; Daley, A.J.; Cheng, A.C.; Burgner, D. Diagnostic yield of timing blood culture collection relative to fever. Pediatr. Infect. Dis. J. 2016, 35, 846–850. [Google Scholar] [PubMed]
- Lee, A.; Merrett, S.; Reller, L.B.; Weinstein, M.P. Detection of bloodstream infections in adults: How many blood cultures are needed? J. Clin. Microbiol. 2007, 45, 3546–3548. [Google Scholar] [PubMed]
- Miller, J.M.; Binnicker, M.J.; Campbell, S.; Carroll, K.C.; Chapin, K.C.; Gilligan, P.H.; Gonzalez, M.D.; Jerris, R.C.; Kehl, S.C.; Patel, R.; et al. A Guide to Utilization of the Microbiology Laboratory for Diagnosis of Infectious Diseases: 2018 Update by the Infectious Diseases Society of America and the American Society for Microbiology. Clin. Infect. Dis. 2018, 67, e1–e94. [Google Scholar] [CrossRef] [PubMed]
- Neves, L.; Marra, A.R.; Camargo, T.Z.; dos Santos, M.C.; Zulin, F.; da Silva, P.C.; de Moura, N.A.; da Silva Victor, E.; Pasternak, J.; dos Santos, O.F.P.; et al. Correlation between mass and volume of collected blood with positivity of blood cultures. BMC Res. Notes 2015, 8, 383. [Google Scholar]
- [Dataset]NHSN Terminology NHSN CDC. Available online: https://www.cdc.gov/nhsn/cdaportal/terminology/index.html (accessed on 20 December 2023).
- Walker, G.A.; Runde, D.; Rolston, D.M.; Wiener, D.; Lee, J. Emergency department rectal temperatures in over 10 years: A retrospective observational study. World J. Emerg. Med. 2013, 4, 107–112. [Google Scholar] [CrossRef] [PubMed]
- Kresovich-Wendler, K.; Levitt, M.A.; Yearly, L. An evaluation of clinical predictors to determine need for rectal temperature measurement in the emergency department. Am. J. Emerg. Med. 1989, 7, 391–394. [Google Scholar] [CrossRef] [PubMed]
- O’Grady, N.P.; Alexander, E.; Alhazzani, W.; Alshamsi, F.; Cuellar-Rodriguez, J.; Jefferson, B.K.; Kalil, A.C.; Pastores, S.M.; Patel, R.; Van Duin, D.; et al. Society of Critical Care Medicine and the Infectious Diseases Society of America Guidelines for evaluating new fever in adult patients in the ICU. Crit. Care Med. 2023, 51, 1570–1586. [Google Scholar] [CrossRef] [PubMed]
- Weinstein, M.P. Current Blood Culture Methods and Systems: Clinical Concepts, Technology, and Interpretation of Results. Clin. Infect. Dis. 1996, 23, 40–46. [Google Scholar] [CrossRef] [PubMed]
- Michael, L.W. Detection of bacteremia: Blood cultures and other diagnostic tests. In UpToDate; Connor, R.F., Ed.; Wolters Kluwer: Hong Kong, China, 2024. [Google Scholar]
- Coburn, B.; Morris, A.M.; Tomlinson, G.; Detsky, A.S. Does this adult patient with suspected bacteremia require blood cultures? JAMA—J. Am. Med. Assoc. 2012, 308, 502–511. [Google Scholar] [CrossRef] [PubMed]
- Jones, G.R.; Lowes, J.A. The systemic inflammatory response syndrome as a predictor of bacteraemia and outcome from sepsis. QJM 1996, 89, 515–522. [Google Scholar] [PubMed]
- Shapiro, N.I.; Wolfe, R.E.; Wright, S.B.; Moore, R.; Bates, D.W. Who needs a blood culture? A prospectively derived and validated prediction rule. J. Emerg. Med. 2008, 35, 255–264. [Google Scholar] [CrossRef] [PubMed]
- Leekha, S.; Terrell, C.L.; Edson, R.S. General principles of antimicrobial therapy. Mayo Clin. Proc. 2011, 86, 156–167. [Google Scholar] [CrossRef] [PubMed]
- Lamy, B.; Sundqvist, M.; Idelevich, E.A.; ESCMID Study Group for Bloodstream Infections. Endocarditis and Sepsis (ESGBIES) Bloodstream infections—Standard and progress in pathogen diagnostics. Clin. Microbiol. Infect. Off. Publ. Eur. Soc. Clin. Microbiol. Infect. Dis. 2020, 26, 142–150. [Google Scholar]
| Characteristics | Optimal Timing, n = 25,616 (34.7%) | Non Optimal Timing, n = 48,171 (65.3%) | SMD |
|---|---|---|---|
| Age (y) | 64.4 ± 18.4 | 65.7 ± 18.1 | 0.052 |
| Gender | |||
| Male, n (%) | 14,804 (57.8%) | 28,600 (59.4%) | 0.031 |
| Comorbidities | |||
| CHF*, n (%) | 4775 (18.64%) | 11,893 (24.68%) | 0.152 |
| Stroke, n (%) | 6286 (24.54%) | 11,906 (24.71%) | 0.067 |
| Dementia, n (%) | 2011 (0.8%) | 2854 (5.92%) | 0.013 |
| Chronic pulmonary disease, n (%) | 6048 (23.61%) | 13,674 (28.4%) | 0.071 |
| Rheumatological disease, n (%) | 886 (3.46%) | 1972 (4.1%) | 0.079 |
| Diabetes mellitus, n (%) | 9665 (37.73%) | 19,199 (3.96%) | 0.066 |
| Diabetes mellitus with chronic complications, n (%) | 3535 (13.8%) | 7326 (15.2%) | 0.032 |
| Peripheral Vascular disease, n (%) | 3540 (13.82%) | 7820 (16.23%) | 0.041 |
| Malignancy, n (%) | 4768 (18.6%) | 9365 (19.44%) | 0.132 |
| Renal disease, n (%) | 5966 (23.29%) | 14,166 (29.4%) | 0.011 |
| Vital signs | |||
| Pulse (bpm*) | 100.7 ± 26.4 | 90.2 ± 19.6 | 0.458 |
| Systolic Blood pressure (mmHg*) | 134.1 ± 22.5 | 132.2 ± 23.0 | 0.083 |
| Blood tests | |||
| White blood cells (mm3/mL*) | 11.39 ± 7.2 | 12.24 ± 9.5 | 0.159 |
| C-reactive protein (mg/dL*) | 15.29 ± 13.78 | 12.72 ± 11.19 | 0.133 |
| Primary diagnosis | |||
| Symptoms, Signs, And Ill-Defined Conditions, n (%) | 5376 (20.99%) | 10,344 (21.47%) | 0.279 |
| Diseases of Respiratory system, n (%) | 3959 (15.46%) | 7000 (14.53%) | 0.074 |
| Diseases of Circulatory system, n (%) | 3739 (14.6%) | 7122 (14.78) | 0.042 |
| Infectious and Parasitic Diseases, n (%) | 3581 (13.98%) | 6927 (14.38%) | 0.010 |
| Diseases of Genitourinary system, n (%) | 1490 (5.82%) | 2799 (5.81%) | 0.035 |
| Others, n (%) | 1345 (5.25%) | 2413 (5.01%) | 0.068 |
| Injury and Poisoning, n (%) | 1291 (5.04%) | 2446 (5.08%) | |
| Diseases of Digestive system, n (%) | 1133 (4.42%) | 2416 (5.02%) | 0.054 |
| Diseases of Skin and subcutaneous tissue, n (%) | 794 (3.10%) | 1329 (2.76%) | |
| Endocrine, Nutritional and Metabolic Diseases, And Immunity Disorders, n (%) | 730 (2.85%) | 1331 (2.76%) | 0.033 |
| Diseases musculoskeletal and connective tissue, n (%) | 693 (2.71%) | 1269 (2.63%) | 0.012 |
| Diseases of CNS, n (%) | 625 (2.44%) | 1190 (2.47%) | 0.016 |
| Neoplasms | 558 (2.18%) | 1027 (2.13%) | 0.010 |
| Diseases of blood and blood forming organ | 302 (1.18%) | 561 (1.16%) | 0.008 |
| Bacteriological Yield | Optimal Timing, n = 25,616 (34.7%) | Not Optimal Timing, n = 48,174 (65.3%) | p-Value |
|---|---|---|---|
| No growth, n (%) | 23,406 (91.37%) | 44,542 (92.46%) | <0.001 |
| Positive—true bacteremia *, n (%) | 1562 (6.15%) | 2483 (5.15%) | |
| Positive—contamination **, n (%) | 648 (2.53%) | 1149 (2.38%) |
| Characteristic | Odds Ratio | 95% CI for Odds Ratio | p-Value | |
|---|---|---|---|---|
| Lower | Upper | |||
| Age (years) | 0.99 | 0.99 | 0.99 | <0.001 |
| Pulse (bpm), per 10 bpm | 1.28 | 1.27 | 1.30 | <0.001 |
| Systolic Blood Pressure (mmHg), per 10 mmHg | 1.06 | 1.05 | 1.07 | <0.001 |
| C-reactive protein (mg/dL) per 5 mg/dL | 1.10 | 1.09 | 1.11 | <0.001 |
| White blood cells (106/mL) | 0.99 | 0.98 | 0.99 | <0.001 |
| Congestive heart failure | 0.86 | 0.81 | 0.91 | <0.001 |
| Dementia | 1.23 | 1.14 | 1.34 | <0.001 |
| COPD * | 0.85 | 0.81 | 0.90 | <0.001 |
| Rheumatological disease | 0.85 | 0.76 | 0.94 | 0.003 |
| Diabetes Mellitus with chronic complications | 0.93 | 0.88 | 0.97 | <0.05 |
| Hemiplegia/Paraplegia | 1.30 | 1.22 | 1.40 | <0.001 |
| Renal disease | 0.79 | 0.75 | 0.83 | <0.001 |
| Malignancy | 0.92 | 0.87 | 0.98 | 0.007 |
| Moderate to severe liver disease | 0.79 | 0.66 | 0.95 | 0.013 |
| AIDS * | 0.53 | 0.36 | 0.77 | 0.001 |
| Characteristic | Odds Ratio | 95% CI for the Odds Ratio | p-Value | |
|---|---|---|---|---|
| Lower | Upper | |||
| Optimal timing | 1.23 | 1.12 | 1.35 | <0.001 |
| Age (years) | 1.01 | 1.00 | 1.01 | <0.001 |
| Pulse (bpm), per 10 bpm | 1.05 | 1.04 | 1.07 | <0.001 |
| Systolic Blood Pressure (mmHg), per 10 mmHg | 0.88 | 0.86 | 0.90 | <0.001 |
| C-reactive protein (mg/dL) per 5 mg/dL | 1.06 | 1.04 | 1.07 | 0.043 |
| White blood cells (106/mL) | 1.01 | 1.00 | 1.01 | <0.001 |
| Diabetes Mellitus with chronic complications | 1.38 | 1.22 | 1.44 | <0.001 |
| Renal disease | 1.15 | 1.04 | 1.28 | 0.006 |
| Moderate to severe liver disease | 2.21 | 1.67 | 2.93 | 0.001 |
| Any Malignancy | 1.20 | 1.07 | 1.33 | <0.001 |
| AIDS * | 2.32 | 1.32 | 4.05 | 0.003 |
| Characteristic | Odds Ratio | 95% CI for the Odds Ratio | p-Value | |
|---|---|---|---|---|
| Lower | Upper | |||
| Optimal timing | 1.17 | 1.03 | 1.34 | 0.018 |
| Age (years) | 1.01 | 1.00 | 1.01 | <0.001 |
| Gender—male | 0.86 | 0.75 | 0.98 | 0.024 |
| Systolic Blood Pressure (mmHg), per 10 mmHg | 0.95 | 0.92 | 0.98 | <0.001 |
| C-reactive protein (mg/dL) per 5 mg/dL | 0.96 | 0.93 | 0.99 | 0.024 |
| CVA * | 1.25 | 1.07 | 1.45 | 0.004 |
| Dementia | 0.76 | 0.58 | 0.99 | 0.041 |
| COPD * | 0.79 | 0.68 | 0.93 | 0.003 |
| Renal disease | 0.79 | 0.68 | 0.93 | 0.004 |
| Rheumatological disease | 0.48 | 0.30 | 0.79 | 0.003 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cojocaru, Y.; Hassan, L.; Nesher, L.; Shafat, T.; Novack, V. The Utility of Blood Cultures in Non-Febrile Patients and Patients with Antibiotics Therapy in Internal Medicine Departments. J. Clin. Med. 2025, 14, 2373. https://doi.org/10.3390/jcm14072373
Cojocaru Y, Hassan L, Nesher L, Shafat T, Novack V. The Utility of Blood Cultures in Non-Febrile Patients and Patients with Antibiotics Therapy in Internal Medicine Departments. Journal of Clinical Medicine. 2025; 14(7):2373. https://doi.org/10.3390/jcm14072373
Chicago/Turabian StyleCojocaru, Yaniv, Lior Hassan, Lior Nesher, Tali Shafat, and Victor Novack. 2025. "The Utility of Blood Cultures in Non-Febrile Patients and Patients with Antibiotics Therapy in Internal Medicine Departments" Journal of Clinical Medicine 14, no. 7: 2373. https://doi.org/10.3390/jcm14072373
APA StyleCojocaru, Y., Hassan, L., Nesher, L., Shafat, T., & Novack, V. (2025). The Utility of Blood Cultures in Non-Febrile Patients and Patients with Antibiotics Therapy in Internal Medicine Departments. Journal of Clinical Medicine, 14(7), 2373. https://doi.org/10.3390/jcm14072373







