Physiotherapist Online Assessment in Patients with Stroke: Protocol for a Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Methods
2.1. Eligibility Criteria
2.2. Inclusion Criteria
2.2.1. Population
2.2.2. Index Test
2.2.3. Comparator Test
2.2.4. Primary Outcomes
2.2.5. Secondary Outcomes
2.3. Exclusion Criteria
3. Study Design
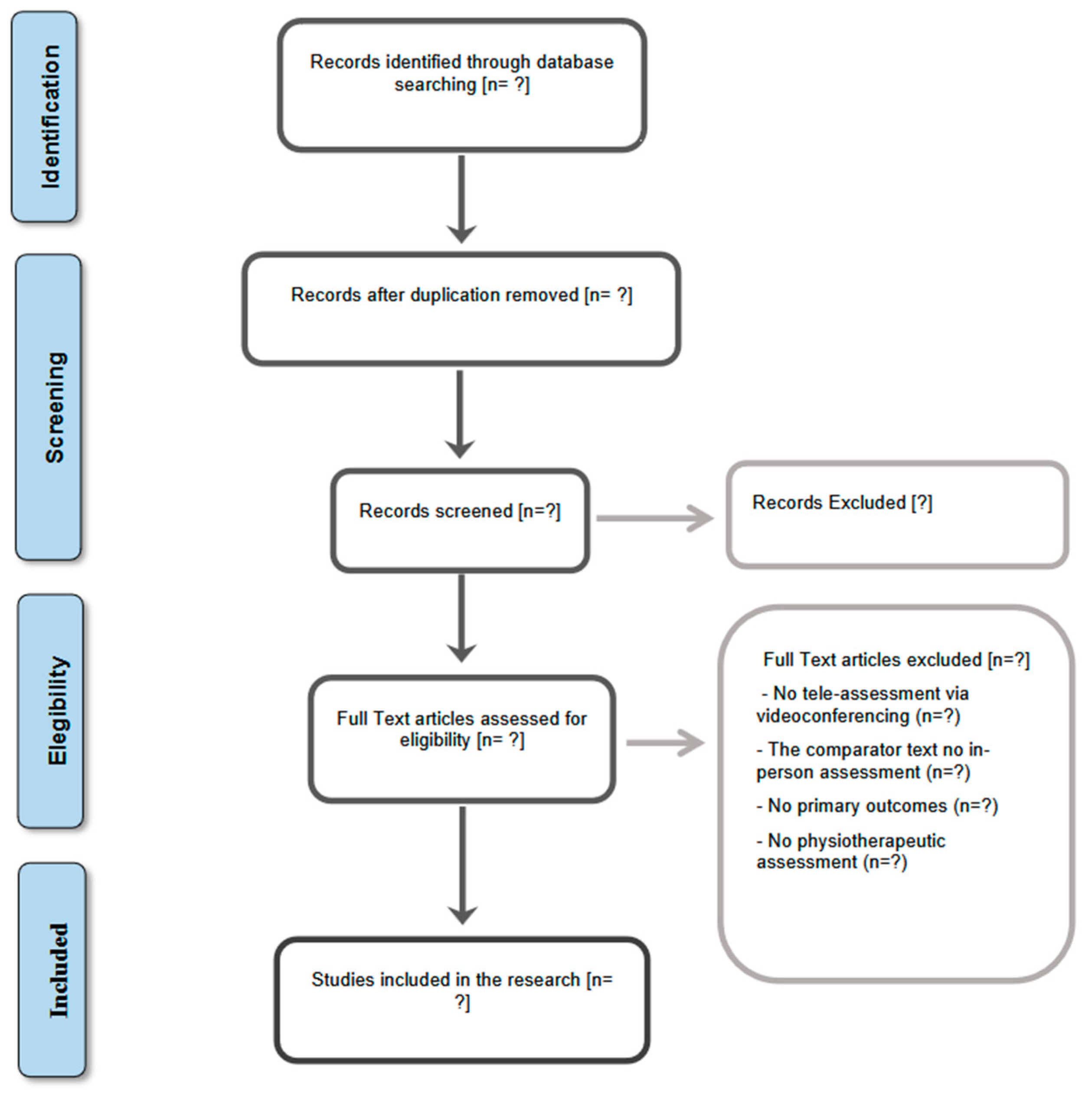
4. Selection Process
5. Data Extraction
- Research characteristics: Title, first author, publication year, study setting, study design, sample size, and diagnostic criteria for stroke.
- Population characteristics: Age range, gender/sex, comorbidity, cognition, and mobility.
- Intervention characteristics: Intervention type, delivery devices, types of platforms, mode of delivery (synchronous/asynchronous), location, duration, and results.
- Comparator intervention: usual face-to-face assessment process, location, duration, and results.
- Outcome characteristics: Validity, inter-rater and intra-rater reliability, accuracy, minimal detectable change score, and measurement error study for physiotherapy assessment components. As secondary outcomes: sensorimotor impairment, balance, mobility, functional capacity, gait, motor function, grasp, grip, pinch, gross, and any other outcomes that the authors do not consider as primary clinical variables.
- Analysis method: Statistical methods used, quantitative synthesis, risk of bias, and quality assessment.
6. Methodological Quality Check
7. Statistical Analysis
8. Certainty of Evidence
9. Ethics and Dissemination
10. Discussion
11. Conclusions, Strengths, and Limitations
- ⇒
- This research will be the first systematic review on the use of digital physiotherapy assessment compared to face-to-face assessment in adults with stroke.
- ⇒
- This review seeks to determine the scientific evidence on the use of a digital assessment in a study of populations with a high prevalence.
- ⇒
- The results may provide answers to questions and paradoxes that currently remain unresolved.
- ⇒
- This review will adhere to the Preferred Reporting Items for Systematic Review and Meta-Analyses in order to reduce bias.
- ⇒
- There may be high heterogeneity in the selected studies due to different diagnostic criteria, types of devices used, and characteristics of adults with stroke.
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- ACV el Concepto ESUS—OPS/OMS|Organización Panamericana de la Salud. Available online: https://www.paho.org/es/relacsis-0/foro-dr-roberto-becker/acv-concepto-esus (accessed on 13 November 2024).
- Cardiovascular Diseases (CVDs). Available online: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) (accessed on 14 November 2024).
- Stroke—Causes and Risk Factors|NHLBI, NIH. Available online: https://www.nhlbi.nih.gov/health/stroke/causes (accessed on 28 January 2025).
- Feigin, V.L.; Stark, B.A.; Johnson, C.O.; Roth, G.A.; Bisignano, C.; Abady, G.G.; Abbasifard, M.; Abbasi-Kangevari, M.; Abd-Allah, F.; Abedi, V.; et al. Global, regional, and national burden of stroke and its risk factors, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet. Neurol. 2021, 20, 795–820. [Google Scholar] [CrossRef]
- Siuly, S.; Zhang, Y. Medical Big Data: Neurological Diseases Diagnosis Through Medical Data Analysis. Data Sci. Eng. 2016, 1, 54–64. [Google Scholar] [CrossRef]
- Guidelines for Assessment and Intervention with Persons with Disabilities. Available online: https://www.apa.org/pi/disability/resources/assessment-disabilities (accessed on 13 November 2024).
- Gebreheat, G.; Goman, A.; Porter-Armstrong, A. The use of home-based digital technology to support post-stroke upper limb rehabilitation: A scoping review. Clin. Rehabil. 2023, 38, 60. [Google Scholar] [CrossRef] [PubMed]
- Nikolaev, V.A.; Nikolaev, A.A. Perspectives of Decision Support System TeleRehab in the Management of Post-Stroke Telerehabilitation. Life 2024, 14, 1059. [Google Scholar] [CrossRef]
- Virtual Practice. Available online: https://www.collegept.org/registrants/virtual-practice-in-physiotherapy (accessed on 13 November 2024).
- Tchero, H.; Teguo, M.T.; Lannuzel, A.; Rusch, E. Telerehabilitation for Stroke Survivors: Systematic Review and Meta-Analysis. J. Med. Internet Res. 2018, 20, e10867. [Google Scholar] [CrossRef]
- Peretti, A.; Amenta, F.; Tayebati, S.K.; Nittari, G.; Mahdi, S.S. Telerehabilitation: Review of the state-of-the-art and areas of application. JMIR Rehabil. Assist. Technol. 2017, 4, e7511. [Google Scholar] [CrossRef]
- Chen, J.; Jin, W.; Dong, W.S.; Jin, Y.; Qiao, F.L.; Zhou, Y.F.; Ren, C.C. Effects of Home-based Telesupervising Rehabilitation on Physical Function for Stroke Survivors with Hemiplegia: A Randomized Controlled Trial. Am. J. Phys. Med. Rehabil. 2017, 96, 152–160. [Google Scholar] [CrossRef]
- Chen, J.; Sun, D.; Zhang, S.; Shi, Y.; Qiao, F.; Zhou, Y.; Liu, J.; Ren, C. Effects of home-based telerehabilitation in patients with stroke: A randomized controlled trial. Neurology 2020, 95, E2318–E2330. [Google Scholar] [CrossRef]
- Mulligan, C.A.; Ayoub, J.L. Remote Assessment: Origins, Benefits, and Concerns. J. Intell. 2023, 11, 114. [Google Scholar] [CrossRef]
- Lai, B.; Wadsworth, D.; Spring, K.; Jones, C.S.; Mintz, M.; Malone, L.A.; Kim, Y.; Wilroy, J.; Lee, H. Validity and Reliability of a Telehealth Physical Fitness and Functional Assessment Battery for Ambulatory Youth With and Without Mobility Disabilities: Observational Measurement Study. JMIR Rehabil. Assist. Technol. 2024, 11, e50582. [Google Scholar] [CrossRef]
- Silva, T.G.d.; da Costa, A.B.; da Costa, N.M.; Michaelsen, S.M. Adaptation and development of the instruction manual for a videoconference-based Motor Assessment Scale: Validity, reliability and measurement error of Tele-MAS. Disabil. Rehabil. 2024, 1–8. [Google Scholar] [CrossRef]
- Retos. Available online: https://recyt.fecyt.es/index.php/retos (accessed on 29 January 2025).
- Lee, A.C.; Deutsch, J.E.; Holdsworth, L.; Kaplan, S.L.; Kosakowski, H.; Latz, R.; McNeary, L.L.; O’Neil, J.; Ronzio, O.; Sanders, K.; et al. Telerehabilitation in Physical Therapist Practice: A Clinical Practice Guideline From the American Physical Therapy Association. Phys. Ther. 2024, 104, pzae045. [Google Scholar] [CrossRef] [PubMed]
- Bearne, L.M.; Gregory, W.J.; Hurley, M.V. Remotely delivered physiotherapy: Can we capture the benefits beyond COVID-19? Rheumatology 2021, 60, keab104. [Google Scholar] [CrossRef] [PubMed]
- Mani, S.; Sharma, S.; Omar, B.; Paungmali, A.; Joseph, L. Validity and reliability of Internet-based physiotherapy assessment for musculoskeletal disorders: A systematic review. J. Telemed. Telecare 2017, 23, 379–391. [Google Scholar] [CrossRef]
- Saporito, S.; Brodie, M.A.; Delbaere, K.; Hoogland, J.; Nijboer, H.; Rispens, S.M.; Spina, G.; Stevens, M.; Annegarn, J. Remote timed up and go evaluation from activities of daily living reveals changing mobility after surgery. Physiol. Meas. 2019, 40, 035004. [Google Scholar] [CrossRef] [PubMed]
- Cabana, F.; Boissy, P.; Tousignant, M.; Moffet, H.; Corriveau, H.; Dumais, R. Interrater agreement between telerehabilitation and face-to-face clinical outcome measurements for total knee arthroplasty. Telemed. J. e-Health 2010, 16, 293–298. [Google Scholar] [CrossRef]
- Peterson, S.; Kuntz, C.; Roush, J. Use of a modified treatment-based classification system for subgrouping patients with low back pain: Agreement between telerehabilitation and face-to-face assessments. Physiother. Theory Pract. 2019, 35, 1078–1086. [Google Scholar] [CrossRef]
- Lade, H.; McKenzie, S.; Steele, L.; Russell, T.G. Validity and reliability of the assessment and diagnosis of musculoskeletal elbow disorders using telerehabilitation. Telemed. J. e-Health 2012, 18, 413–418. [Google Scholar] [CrossRef]
- Russell, T.; Truter, P.; Blumke, R.; Richardson, B. The Diagnostic Accuracy of Telerehabilitation for Nonarticular Lower-Limb Musculoskeletal Disorders. Telemed. J. e-Health 2010, 16, 585–594. [Google Scholar] [CrossRef]
- Wagner, J.; Zurlo, A.; Rusconi, E. Individual differences in visual search: A systematic review of the link between visual search performance and traits or abilities. Cortex 2024, 178, 51–90. [Google Scholar] [CrossRef]
- Moher, D.; Stewart, L.; Shekelle, P. Implementing PRISMA-P: Recommendations for prospective authors. Syst. Rev. 2016, 5, 1–2. [Google Scholar] [CrossRef]
- Rogante, M.; Kairy, D.; Giacomozzi, C.; Grigioni, M. A quality assessment of systematic reviews on telerehabilitation: What does the evidence tell us? Ann. Ist. Super. Sanita 2015, 51, 11–18. [Google Scholar] [CrossRef] [PubMed]
- Yepes-Nuñez, J.J.; Urrútia, G.; Romero-García, M.; Alonso-Fernández, S. Declaración PRISMA 2020: Una guía actualizada para la publicación de revisiones sistemáticas. Rev. Española Cardiol. 2021, 74, 790–799. [Google Scholar] [CrossRef]
- Cumpston, M.; Li, T.; Page, M.J.; Chandler, J.; Welch, V.A.; Higgins, J.P.; Thomas, J. Updated guidance for trusted systematic reviews: A new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst. Rev. 2019, 10, ED000142. [Google Scholar] [CrossRef]
- De España, G.; Internacional, C. MINISTERIO DE SANIDAD, SERVICIOS SOCIALES E IGUALDAD MINISTERIO DE LA PRESIDENCIA Y PARA LAS ADMINISTRACIONES TERRITORIALES BOLETÍN OFICIAL DEL ESTADO CIE • 10 • ES MINISTERIO DE SANIDAD, SERVICIOS SOCIALES E IGUALDAD MINISTERIO DE LA PRESIDENCIA Y PARA LAS ADMINISTRACIONES TERRITORIALES-BOLETÍN OFICIAL DEL ESTADO. 2018. Available online: https://www.sanidad.gob.es/estadEstudios/estadisticas/normalizacion/CIE10/CIE10ES_2018_diag_pdf_20180202.pdf (accessed on 28 January 2025).
- Recommendations|Stroke Rehabilitation in Adults|Guidance|NICE. Available online: https://www.nice.org.uk/ (accessed on 29 November 2024).
- Jordan, H.T.; Stinear, C.M. Accuracy and Reliability of Remote Categorization of Upper Limb Outcome After Stroke. Neurorehabil. Neural Repair 2024, 38, 167–175. [Google Scholar] [CrossRef]
- Listas Guía de Comprobación de Estudios Sobre Pruebas Diagnósticas Incluidos en las Revisiones Sistemáticas: Declaración QUADAS—Evidencias en Pediatría. Available online: https://evidenciasenpediatria.es/articulo/5969/listas-guia-de-comprobacion-de-estudios-sobre-pruebas-diagnosticas-incluidos-en-las-revisiones-sistematicas-declaracion-quadas (accessed on 29 November 2024).
- Lucas, N.; Macaskill, P.; Irwig, L.; Moran, R.; Rickards, L.; Turner, R.; Bogduk, N. The reliability of a quality appraisal tool for studies of diagnostic reliability (QAREL). BMC Med. Res. Methodol. 2013, 13, 111. [Google Scholar] [CrossRef]
- Whiting, P.; Rutjes, A.W.S.; Reitsma, J.B.; Bossuyt, P.M.M.; Kleijnen, J. The development of QUADAS: A tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC Med. Res. Methodol. 2003, 3, 25. [Google Scholar] [CrossRef]
- Whiting, P.; Rutjes, A.W.S.; Dinnes, J.; Reitsma, J.B.; Bossuyt, P.M.M.; Kleijnen, J. Development and validation of methods for assessing the quality of diagnostic accuracy studies. Health Technol. Assess. 2004, 8, 1–234. [Google Scholar] [CrossRef]
- Wang, Z.; He, K.; Sui, X.; Yi, J.; Yang, Z.; Wang, K.; Gao, Y.; Bian, L.; Jiang, J.; Zhao, L. The Effect of Web-Based Telerehabilitation Programs on Children and Adolescents With Brain Injury: Systematic Review and Meta-Analysis. J. Med. Internet Res. 2023, 25, e46957. [Google Scholar] [CrossRef]
- Harbord, R.M.; Egger, M.; Sterne, J.A.C. A modified test for small-study effects in meta-analyses of controlled trials with binary endpoints. Stat. Med. 2006, 25, 3443–3457. [Google Scholar] [CrossRef]
- Prasad, M. Introduction to the GRADE tool for rating certainty in evidence and recommendations. Clin. Epidemiol. Glob. Health 2024, 25, 101484. [Google Scholar] [CrossRef]
- Wiercioch, W.; Nieuwlaat, R.; Zhang, Y.; Alonso-Coello, P.; Dahm, P.; Iorio, A.; Manja, V.; Mustafa, R.A.; Neumann, I.; Ortel, T.L.; et al. New methods facilitated the process of prioritizing questions and health outcomes in guideline development What is new? J. Clin. Epidemiol. 2022, 143, 91–104. [Google Scholar] [CrossRef] [PubMed]
- Tejada Meza, H.; Artal Roy, J.; Pérez Lázaro, C.; Bestué Cardiel, M.; Alberti González, O.; Tejero Juste, C.; Hernando Quintana, N.; Jarauta Lahoz, L.; Giménez Muñoz, A.; Campello Morer, I.; et al. Epidemiology and characteristics of ischaemic stroke in young adults in Aragon. Neurologia 2022, 37, 434–440. [Google Scholar] [CrossRef] [PubMed]
- Fryer, C.E.; Luker, J.A.; Mcdonnell, M.N.; Hillier, S.L. Self management programmes for quality of life in people with stroke. Cochrane Database Syst. Rev. 2016, 2016, CD010442. [Google Scholar] [CrossRef]
- World Health Organization. Global Strategy on Digital Health 2020–2025; World Health Organization: Geneva, Switzerland, 2021; Available online: http://apps.who.int/bookorders (accessed on 2 August 2023).
- Shamseer, L.; Moher, D.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: Elaboration and explanation. BMJ 2015, 349, g7647. [Google Scholar]
| Data to Be Extracted | Item |
|---|---|
| Publication ID | Title, first author, and publication characteristics (year, setting, etc.) |
| Participants’ Characteristics | Sex, age, disabilities |
| Tele-Assessment Characteristics | Tele-test or tele-scale, delivery device types, synchronous and/or asynchronous, location, duration, results |
| Comparator Test Characteristics | Test or scale, location, duration, results |
| Primary Outcomes | Validity, inter-rater, intra-rater reliability, accuracy studies, minimal detectable change score, and measurement error study |
| Secondary Outcomes Measure | Other outcomes that the authors do not consider as primary clinical variables |
| Certainty of Evidence | Methods used |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Estebanez-Pérez, M.-J.; Pastora-Estebanez, P.; Romero-García, I.; Vinolo-Gil, M.J.; Fernández-Navarro, R.; Pastora-Bernal, J.-M. Physiotherapist Online Assessment in Patients with Stroke: Protocol for a Systematic Review and Meta-Analysis. J. Clin. Med. 2025, 14, 2311. https://doi.org/10.3390/jcm14072311
Estebanez-Pérez M-J, Pastora-Estebanez P, Romero-García I, Vinolo-Gil MJ, Fernández-Navarro R, Pastora-Bernal J-M. Physiotherapist Online Assessment in Patients with Stroke: Protocol for a Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2025; 14(7):2311. https://doi.org/10.3390/jcm14072311
Chicago/Turabian StyleEstebanez-Pérez, María-José, Pablo Pastora-Estebanez, Ismael Romero-García, Maria Jesus Vinolo-Gil, Rocío Fernández-Navarro, and José-Manuel Pastora-Bernal. 2025. "Physiotherapist Online Assessment in Patients with Stroke: Protocol for a Systematic Review and Meta-Analysis" Journal of Clinical Medicine 14, no. 7: 2311. https://doi.org/10.3390/jcm14072311
APA StyleEstebanez-Pérez, M.-J., Pastora-Estebanez, P., Romero-García, I., Vinolo-Gil, M. J., Fernández-Navarro, R., & Pastora-Bernal, J.-M. (2025). Physiotherapist Online Assessment in Patients with Stroke: Protocol for a Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 14(7), 2311. https://doi.org/10.3390/jcm14072311






