Anterior and Posterior Syndesmotic Augmentation Using Nonabsorbable Suture Tape for Acute Syndesmotic Instability: A Technical Note
Abstract
1. Introduction
2. Preoperative Assessment and Imaging
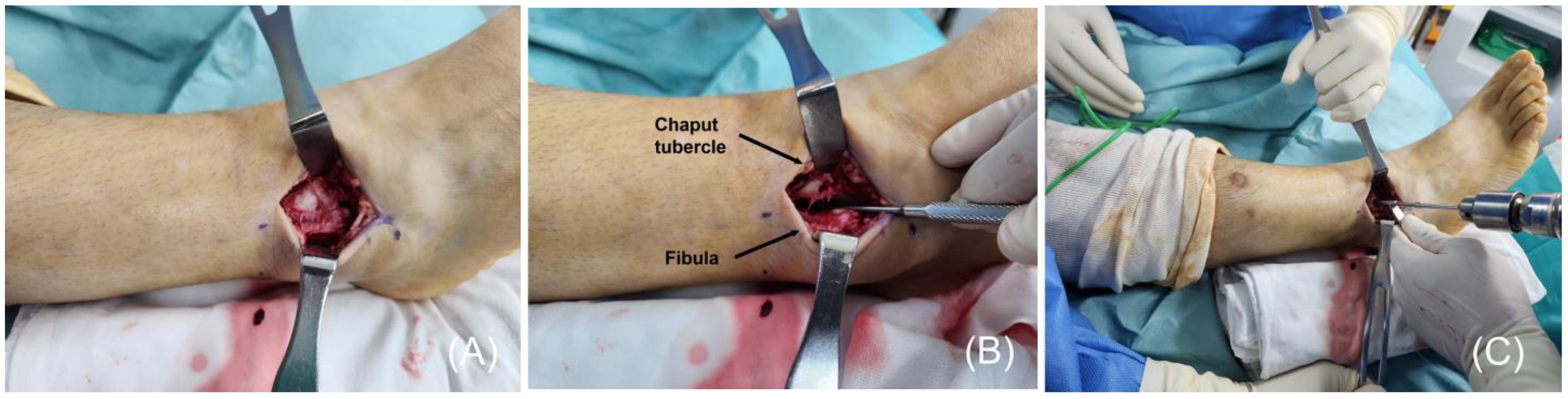
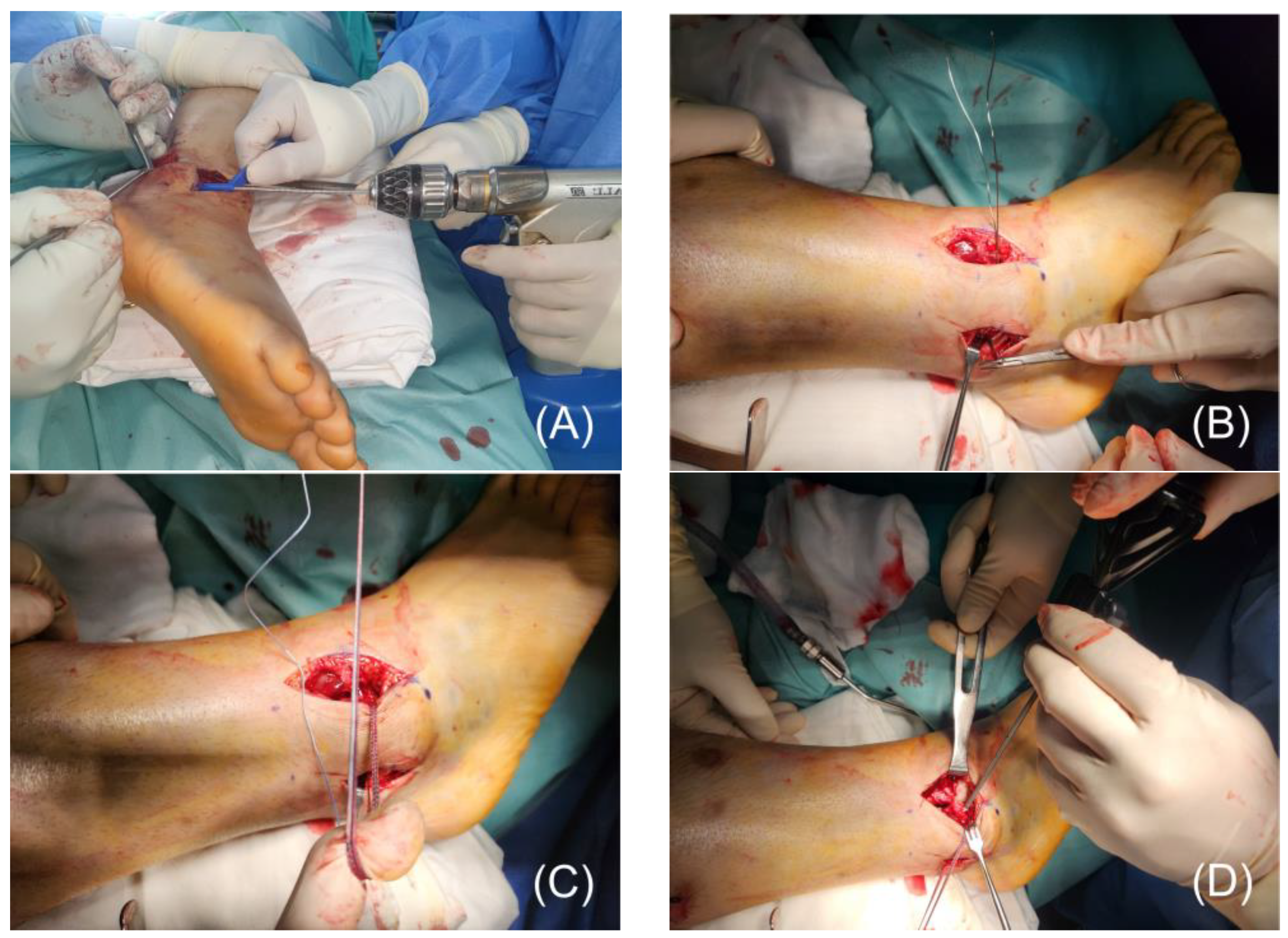
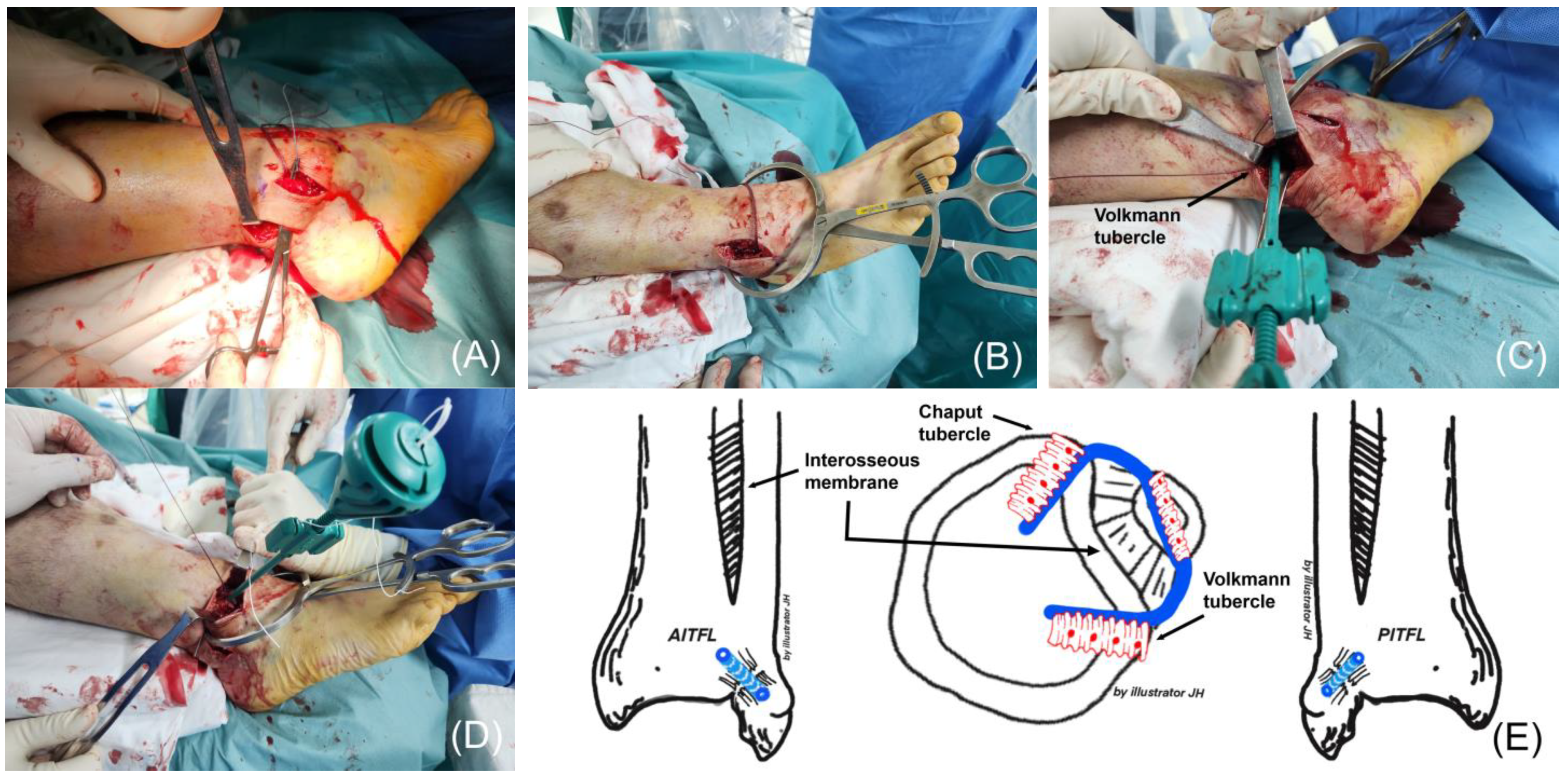
3. Surgical Technique
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AITFL | anterior inferior tibiofibular ligament |
| PITFL | posterior inferior tibiofibular ligament |
| MRI | magnetic resonance imaging |
| CT | computed tomography |
| ROM | ankle range of motion |
| OMAS | Olerud–Molander ankle score |
| VAS | visual analog scale |
References
- Wang, Q.; Liu, S.; Wang, Z.; Li, A.; Ding, J. Meta-analysis of elastic versus rigid fixation in the treatment of acute tibiofibular syndesmosis injury. Syst. Rev. 2024, 13, 51. [Google Scholar] [PubMed]
- Bejarano-Pineda, L.; Guss, D.; Waryasz, G.; DiGiovanni, C.W.; Kwon, J.Y. The Syndesmosis, Part I: Anatomy, Injury Mechanism, Classification, and Diagnosis. Orthop. Clin. N. Am. 2021, 52, 403–415. [Google Scholar] [PubMed]
- Gomes, T.M.; Oliva, X.M.; Viridiana Sanchez, E.; Soares, S.; Diaz, T. Anatomy of the Ankle and Subtalar Joint Ligaments: What We Do Not Know About It? Foot Ankle Clin. 2023, 28, 201–216. [Google Scholar] [PubMed]
- Wake, J.; Martin, K.D. Syndesmosis Injury From Diagnosis to Repair: Physical Examination, Diagnosis, and Arthroscopic-assisted Reduction. J. Am. Acad. Orthop. Surg. 2020, 28, 517–527. [Google Scholar]
- Shibuya, N.; Davis, M.L.; Jupiter, D.C. Epidemiology of foot and ankle fractures in the United States: An analysis of the National Trauma Data Bank (2007 to 2011). J. Foot Ankle Surg. 2014, 53, 606–608. [Google Scholar]
- Jones, C.B.; Gilde, A.; Sietsema, D.L. Treatment of Syndesmotic Injuries of the Ankle: A Critical Analysis Review. JBJS Rev. 2015, 3, e1. [Google Scholar]
- Black, A.T.; Tran, S.; Haffner, Z.K.; Spoer, D.L.; Rahnama-Vaghef, A.; Stowers, J.M. Radiographic outcomes of flexible and rigid fixation techniques of syndesmotic injuries across various body mass indices: A retrospective analysis. J. Foot Ankle Surg. 2024. ahead of print. [Google Scholar]
- Lehtola, R.; Leskelä, H.V.; Flinkkilä, T.; Pakarinen, H.; Niinimäki, J.; Savola, O.; Ohtonen, P.; Kortekangas, T. Suture button versus syndesmosis screw fixation in pronation-external rotation ankle fractures: A minimum 6-year follow-up of a randomised controlled trial. Injury 2021, 52, 3143–3149. [Google Scholar]
- Miller, A.N.; Barei, D.P.; Iaquinto, J.M.; Ledoux, W.R.; Beingessner, D.M. Iatrogenic syndesmosis malreduction via clamp and screw placement. J. Orthop. Trauma 2013, 27, 100–106. [Google Scholar]
- Gardner, M.J.; Demetrakopoulos, D.; Briggs, S.M.; Helfet, D.L.; Lorich, D.G. Malreduction of the tibiofibular syndesmosis in ankle fractures. Foot Ankle Int. 2006, 27, 788–792. [Google Scholar]
- Elghazy, M.A.; Hagemeijer, N.C.; Guss, D.; El-Hawary, A.; Johnson, A.H.; El-Mowafi, H.; DiGiovanni, C.W. Screw versus suture button in treatment of syndesmosis instability: Comparison using weightbearing CT scan. Foot Ankle Surg. 2021, 27, 285–290. [Google Scholar] [PubMed]
- Shimozono, Y.; Hurley, E.T.; Myerson, C.L.; Murawski, C.D.; Kennedy, J.G. Suture Button Versus Syndesmotic Screw for Syndesmosis Injuries: A Meta-analysis of Randomized Controlled Trials. Am. J. Sports Med. 2019, 47, 2764–2771. [Google Scholar] [PubMed]
- Obey, M.R.; Schafer, K.; Matheny, L.M.; McAndrew, C.M.; Gardner, M.J.; Ricci, W.M.; Clanton, T.O.; Backus, J.D. Syndesmotic Suture Button Fixation Results in Higher Tegner Activity Scale Scores When Compared to Screw Fixation: A Multicenter Investigation. Foot Ankle Spec. 2024, 17, 270–276. [Google Scholar] [PubMed]
- Ræder, B.W.; Figved, W.; Madsen, J.E.; Frihagen, F.; Jacobsen, S.B.; Andersen, M.R. Better outcome for suture button compared with single syndesmotic screw for syndesmosis injury: Five-year results of a randomized controlled trial. Bone Jt. J. 2020, 102-b, 212–219. [Google Scholar]
- Clanton, T.O.; Whitlow, S.R.; Williams, B.T.; Liechti, D.J.; Backus, J.D.; Dornan, G.J.; Saroki, A.J.; Turnbull, T.L.; LaPrade, R.F. Biomechanical Comparison of 3 Current Ankle Syndesmosis Repair Techniques. Foot Ankle Int. 2017, 38, 200–207. [Google Scholar]
- Schermann, H.; Ogawa, T.; Lubberts, B.; Taylor, W.R.; Waryasz, G.R.; Khoury, A.; DiGiovanni, C.W.; Guss, D. Comparison of Several Combinations of Suture Tape Reinforcement and Suture Button Constructs for Fixation of Unstable Syndesmosis. J. Am. Acad. Orthop. Surg. 2022, 30, e769–e778. [Google Scholar]
- Teramoto, A.; Shoji, H.; Sakakibara, Y.; Suzuki, T.; Watanabe, K.; Yamashita, T. Suture-Button Fixation and Mini-Open Anterior Inferior Tibiofibular Ligament Augmentation Using Suture Tape for Tibiofibular Syndesmosis Injuries. J. Foot Ankle Surg. 2018, 57, 159–161. [Google Scholar]
- Shoji, H.; Teramoto, A.; Suzuki, D.; Okada, Y.; Sakakibara, Y.; Matsumura, T.; Suzuki, T.; Watanabe, K.; Yamashita, T. Suture-button fixation and anterior inferior tibiofibular ligament augmentation with suture-tape for syndesmosis injury: A biomechanical cadaveric study. Clin. Biomech. 2018, 60, 121–126. [Google Scholar]
- Szabelski, J.; Karpiński, R. Short-Term Hydrolytic Degradation of Mechanical Properties of Absorbable Surgical Sutures: A Comparative Study. J. Funct. Biomater. 2024, 15, 273. [Google Scholar] [CrossRef]
- Karpiński, R.; Szabelski, J.; Maksymiuk, J. Effect of Ringer’s solution on tensile strength of non-absorbable, medium-and long-term absorbable sutures. Advances in Science and Technology. Res. J. 2017, 11, 11–20. [Google Scholar]
- Yoon, S.J.; Jung, K.J.; Hong, Y.C.; Yeo, E.D.; Lee, H.S.; Won, S.H.; Lee, B.R.; Ji, J.Y.; Lee, D.W.; Kim, W.J. Anatomical Augmentation Using Suture Tape for Acute Syndesmotic Injury in Maisonneuve Fracture: A Case Report. Medicina 2023, 59, 652. [Google Scholar] [CrossRef] [PubMed]
- Jamieson, M.D.; Stake, I.K.; Brady, A.W.; Brown, J.; Tanghe, K.K.; Douglass, B.W.; Clanton, T.O. Anterior Inferior Tibiofibular Ligament Suture Tape Augmentation for Isolated Syndesmotic Injuries. Foot Ankle Int. 2022, 43, 994–1003. [Google Scholar] [PubMed]
- Lee, H.S.; Kim, W.J.; Young, K.W.; Jeong, G.M.; Yeo, E.D.; Lee, Y.K. Comparison of Open Anterior Syndesmotic Repair Augmented With Suture-Tape and Trans-syndesmotic Screw Fixation: A Biomechanical Study. J. Foot Ankle Surg. 2021, 60, 339–344. [Google Scholar] [PubMed]
- Harris, N.J.; Nicholson, G.; Pountos, I. Anatomical reconstruction of the anterior inferior tibiofibular ligament in elite athletes using InternalBrace suture tape. Bone Jt. J. 2022, 104-b, 68–75. [Google Scholar]
- Kwon, J.Y.; Stenquist, D.; Ye, M.; Williams, C.; Giza, E.; Kadakia, A.R.; Kreulen, C. Anterior Syndesmotic Augmentation Technique Using Nonabsorbable Suture-Tape for Acute and Chronic Syndesmotic Instability. Foot Ankle Int. 2020, 41, 1307–1315. [Google Scholar]
- Regauer, M.; Mackay, G.; Lange, M.; Kammerlander, C.; Böcker, W. Syndesmotic InternalBrace(TM) for anatomic distal tibiofibular ligament augmentation. World J. Orthop. 2017, 8, 301–309. [Google Scholar]
- Regauer, M.; Mackay, G.; Nelson, O.; Böcker, W.; Ehrnthaller, C. Evidence-Based Surgical Treatment Algorithm for Unstable Syndesmotic Injuries. J. Clin. Med. 2022, 11, 331. [Google Scholar] [CrossRef]
- Cha, S.D.; Kwak, J.Y.; Gwak, H.C.; Ha, D.J.; Kim, J.Y.; Kim, U.C.; Jang, Y.C. Arthroscopic Assessment of Intra-Articular Lesion after Surgery for Rotational Ankle Fracture. Clin. Orthop. Surg. 2015, 7, 490–496. [Google Scholar]
- Yoon, S.J.; Yeo, E.D.; Jung, K.J.; Hong, Y.C.; Hong, C.H.; Won, S.H.; Lee, K.J.; Ji, J.Y.; Byeon, J.Y.; Lee, D.W.; et al. Evaluating the Efficacy of Tension Band Wiring Fixation for Chaput Tubercle Fractures. J. Clin. Med. 2023, 12, 5490. [Google Scholar] [CrossRef]
- Lee, B.R.; Jung, K.J.; Yeo, E.D.; Won, S.H.; Hong, Y.C.; Hong, C.H.; Kim, C.H.; Kim, H.S.; Ji, J.Y.; Byeon, J.Y.; et al. The Outcomes of Mini-Plate Fixation for Unstable Wagstaffe Tubercle Fracture, an Indirect Syndesmosis Injury in Rotational Ankle Fracture. J. Clin. Med. 2024, 13, 1605. [Google Scholar] [CrossRef]
- Golanó, P.; Vega, J.; de Leeuw, P.A.; Malagelada, F.; Manzanares, M.C.; Götzens, V.; van Dijk, C.N. Anatomy of the ankle ligaments: A pictorial essay. Knee Surg. Sports Traumatol. Arthrosc. 2010, 18, 557–569. [Google Scholar] [PubMed]
- Feller, R.; Borenstein, T.; Fantry, A.J.; Kellum, R.B.; Machan, J.T.; Nickisch, F.; Blankenhorn, B. Arthroscopic Quantification of Syndesmotic Instability in a Cadaveric Model. Arthroscopy 2017, 33, 436–444. [Google Scholar] [PubMed]
- Ogilvie-Harris, D.J.; Reed, S.C.; Hedman, T.P. Disruption of the ankle syndesmosis: Biomechanical study of the ligamentous restraints. Arthroscopy 1994, 10, 558–560. [Google Scholar] [PubMed]
- van Dijk, C.N.; Longo, U.G.; Loppini, M.; Florio, P.; Maltese, L.; Ciuffreda, M.; Denaro, V. Classification and diagnosis of acute isolated syndesmotic injuries: ESSKA-AFAS consensus and guidelines. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 1200–1216. [Google Scholar]
- Switaj, P.J.; Mendoza, M.; Kadakia, A.R. Acute and Chronic Injuries to the Syndesmosis. Clin. Sports Med. 2015, 34, 643–677. [Google Scholar]
- Hunt, K.J.; Phisitkul, P.; Pirolo, J.; Amendola, A. High Ankle Sprains and Syndesmotic Injuries in Athletes. J. Am. Acad. Orthop. Surg. 2015, 23, 661–673. [Google Scholar]
- Mackay, G.M.; Blyth, M.J.; Anthony, I.; Hopper, G.P.; Ribbans, W.J. A review of ligament augmentation with the InternalBrace™: The surgical principle is described for the lateral ankle ligament and ACL repair in particular, and a comprehensive review of other surgical applications and techniques is presented. Surg. Technol. Int. 2015, 26, 239–255. [Google Scholar]
- Lubowitz, J.H.; MacKay, G.; Gilmer, B. Knee medial collateral ligament and posteromedial corner anatomic repair with internal bracing. Arthrosc. Tech. 2014, 3, e505–e508. [Google Scholar]
- Schottel, P.C.; Baxter, J.; Gilbert, S.; Garner, M.R.; Lorich, D.G. Anatomic Ligament Repair Restores Ankle and Syndesmotic Rotational Stability as Much as Syndesmotic Screw Fixation. J. Orthop. Trauma 2016, 30, e36–e40. [Google Scholar]
- Nelson, O.A. Examination and repair of the AITFL in transmalleolar fractures. J. Orthop. Trauma 2006, 20, 637–643. [Google Scholar]
- Lee, S.H.; Kim, E.S.; Lee, Y.K.; Yeo, E.D.; Oh, S.R. Arthroscopic syndesmotic repair: Technical tip. Foot Ankle Int. 2015, 36, 229–231. [Google Scholar] [CrossRef]
| Feature | Suture Tape Augmentation | Suture Button Fixation |
|---|---|---|
| Stability | Provides strong initial stabilization and support for ligament healing. | Offers dynamic stabilization with controlled micromotion, allowing for some physiological movement. |
| Biomechanical Strength | Reinforces ligament structures and helps restore anatomical alignment. | More flexible than screws and maintains stability without excessive stiffness. |
| Risk of Implant Failure | Lower risk of breakage compared to screws, but potential loosening over time. | Higher risk of button migration or malreduction if improperly placed. |
| Flexibility in Load Transfer | Distributes forces evenly across the repaired ligament structures. | Allows for partial mobility, which may help prevent stress-shielding effects. |
| Postoperative Rehabilitation | Earlier weight-bearing compared to screws; reduced need for implant removal. | Allows for early mobilization but may require additional stabilization if used alone. |
| Clinical Outcomes | Generally good functional outcomes, especially in high-activity individuals. | Some studies suggest better outcomes in preserving syndesmotic motion. |
| Complications | Risk of ligament stretching over time, requiring careful postoperative monitoring. | Potential for button prominence and irritation. |
| Pt. No. | Age | Sex | Cause | Lauge–Hansen Classification | Injured Side | Follow-Up (mo) | OMAS | VAS Score | Complications | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | Pre | Post | ||||||||
| 1 | 23 | M | S | SER IV | Left | 9 | 10 | 80 | 8 | 1 | None |
| 2 | 46 | M | S | PER IV | Right | 8 | 0 | 85 | 7 | 0 | None |
| 3 | 36 | M | S | PER IV | Right | 16 | 0 | 90 | 8 | 0 | None |
| 4 | 37 | F | S | PER IV | Left | 12 | 0 | 95 | 8 | 0 | None |
| 5 | 46 | M | S | SER IV | Left | 9 | 0 | 80 | 9 | 1 | None |
| 6 | 39 | M | TA | PER IV | Right | 12 | 0 | 90 | 8 | 0 | None |
| 7 | 19 | F | S | SER IV | Left | 9 | 0 | 85 | 9 | 0 | None |
| Mean | 35.14 | NA | NA | NA | NA | 10.71 | 1.43 | 85.71 | 8.00 | 0.29 | NA |
| SD | 10.51 | NA | NA | NA | NA | 2.81 | 3.78 | 5.35 | 0.82 | 0.49 | NA |
| p value | <0.001 | <0.001 | |||||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, S.-W.; Yoon, S.-J.; Jung, K.-J.; Yeo, E.-D.; Won, S.-H.; Hong, C.-H.; Wang, S.-D.; Cho, Y.-C.; Ji, J.-Y.; Byeon, J.-Y.; et al. Anterior and Posterior Syndesmotic Augmentation Using Nonabsorbable Suture Tape for Acute Syndesmotic Instability: A Technical Note. J. Clin. Med. 2025, 14, 2207. https://doi.org/10.3390/jcm14072207
Lee S-W, Yoon S-J, Jung K-J, Yeo E-D, Won S-H, Hong C-H, Wang S-D, Cho Y-C, Ji J-Y, Byeon J-Y, et al. Anterior and Posterior Syndesmotic Augmentation Using Nonabsorbable Suture Tape for Acute Syndesmotic Instability: A Technical Note. Journal of Clinical Medicine. 2025; 14(7):2207. https://doi.org/10.3390/jcm14072207
Chicago/Turabian StyleLee, Si-Wook, Sung-Joon Yoon, Ki-Jin Jung, Eui-Dong Yeo, Sung-Hun Won, Chang-Hwa Hong, Soon-Do Wang, Yong-Chan Cho, Jae-Young Ji, Je-Yeon Byeon, and et al. 2025. "Anterior and Posterior Syndesmotic Augmentation Using Nonabsorbable Suture Tape for Acute Syndesmotic Instability: A Technical Note" Journal of Clinical Medicine 14, no. 7: 2207. https://doi.org/10.3390/jcm14072207
APA StyleLee, S.-W., Yoon, S.-J., Jung, K.-J., Yeo, E.-D., Won, S.-H., Hong, C.-H., Wang, S.-D., Cho, Y.-C., Ji, J.-Y., Byeon, J.-Y., Lee, D.-W., & Kim, W.-J. (2025). Anterior and Posterior Syndesmotic Augmentation Using Nonabsorbable Suture Tape for Acute Syndesmotic Instability: A Technical Note. Journal of Clinical Medicine, 14(7), 2207. https://doi.org/10.3390/jcm14072207







