Gait Characteristics of People with Hallux and Forefoot Amputations—A Case Series
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Instrumentation and Experimental Protocol
2.3. Data Analysis
3. Results
3.1. Time–Distance Parameter
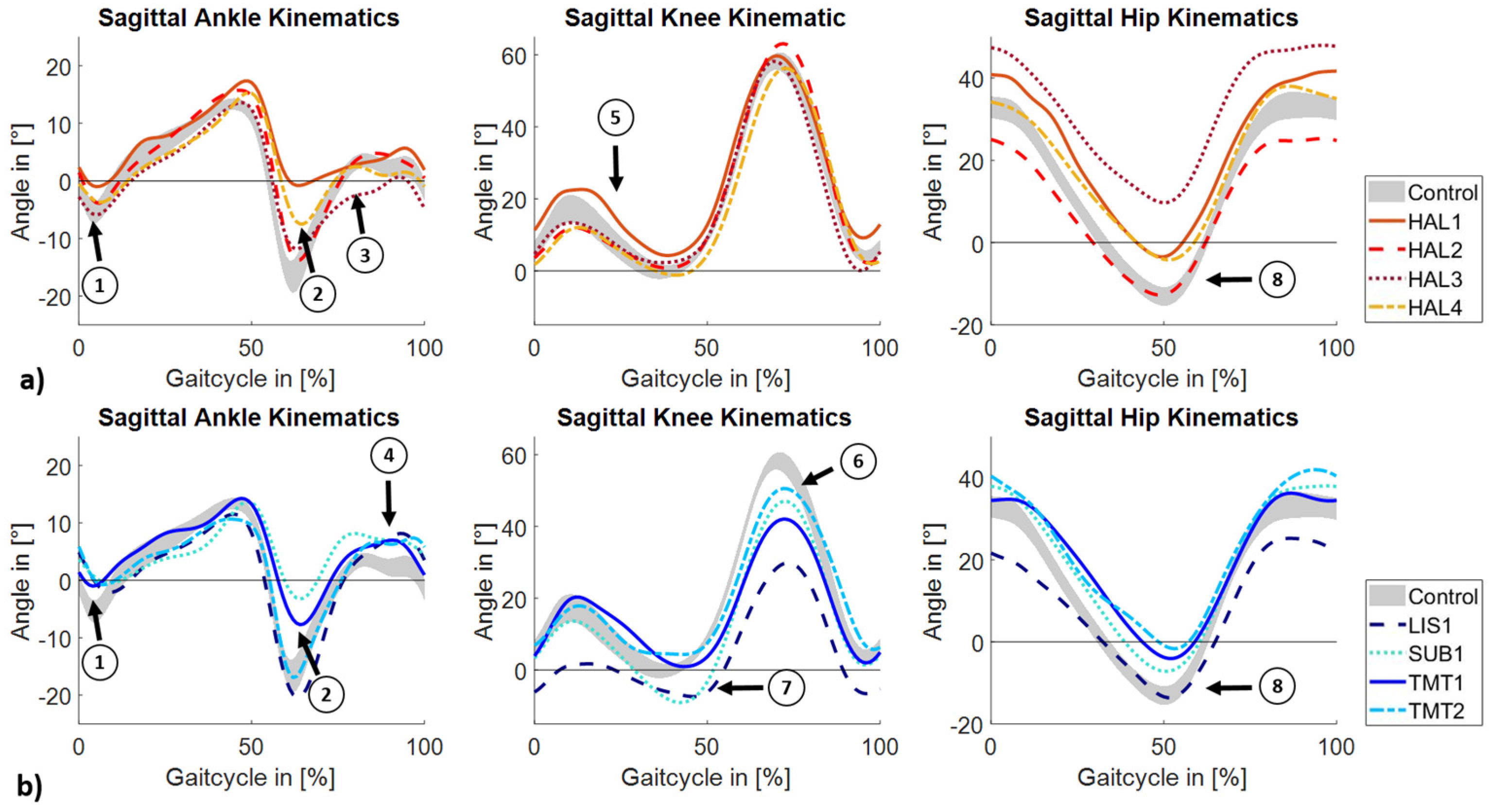
3.2. Kinematic Data
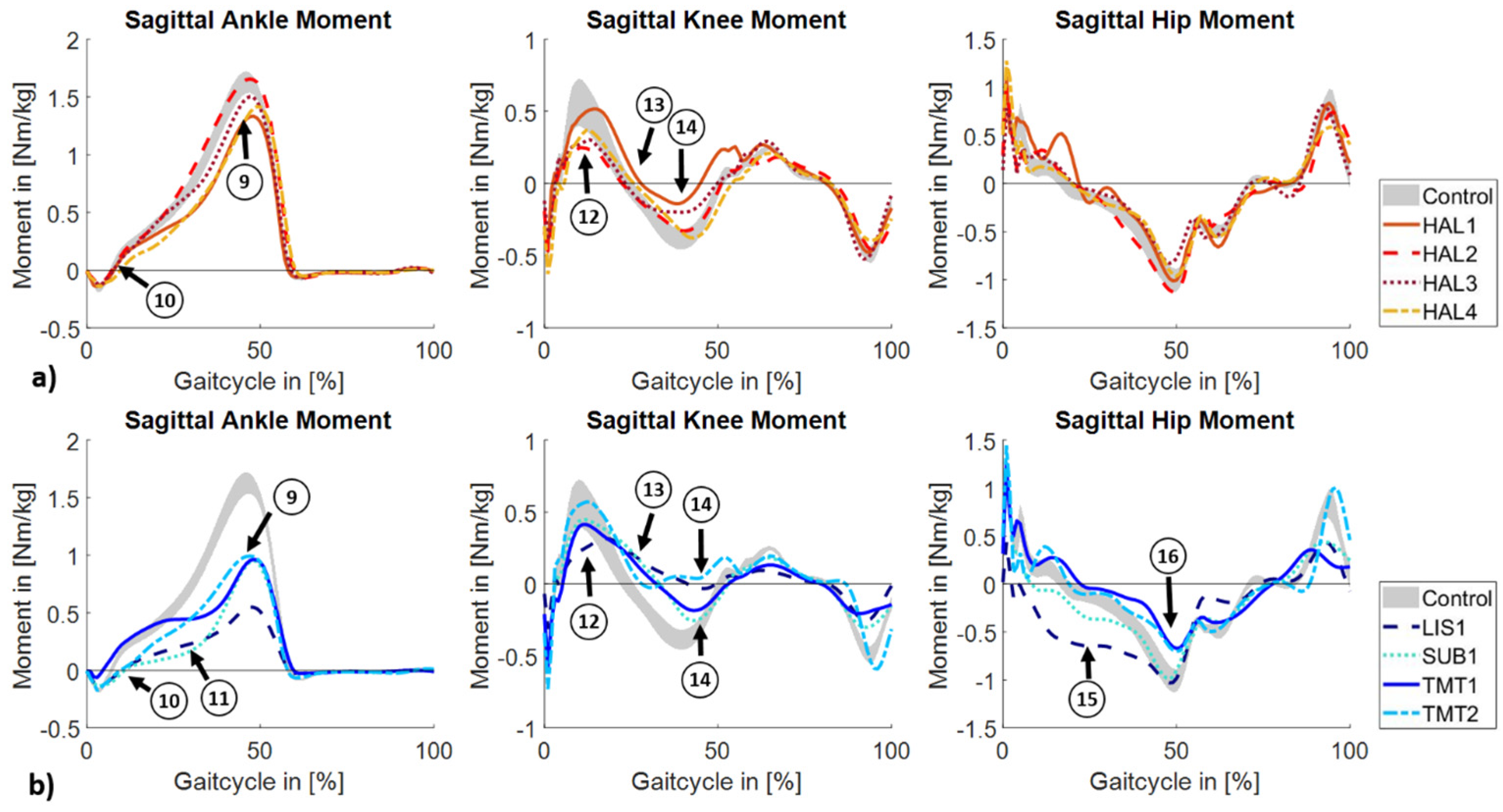
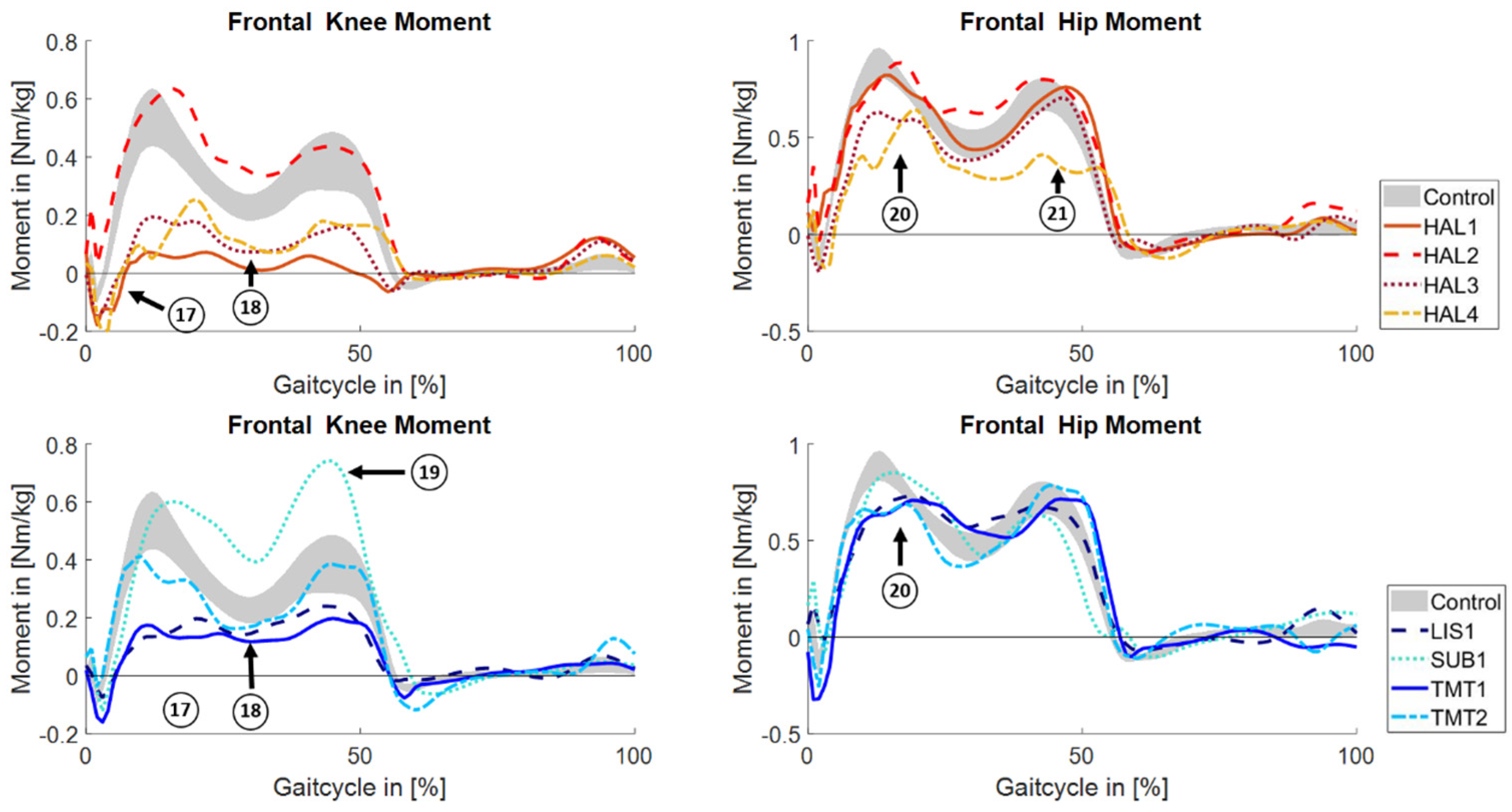
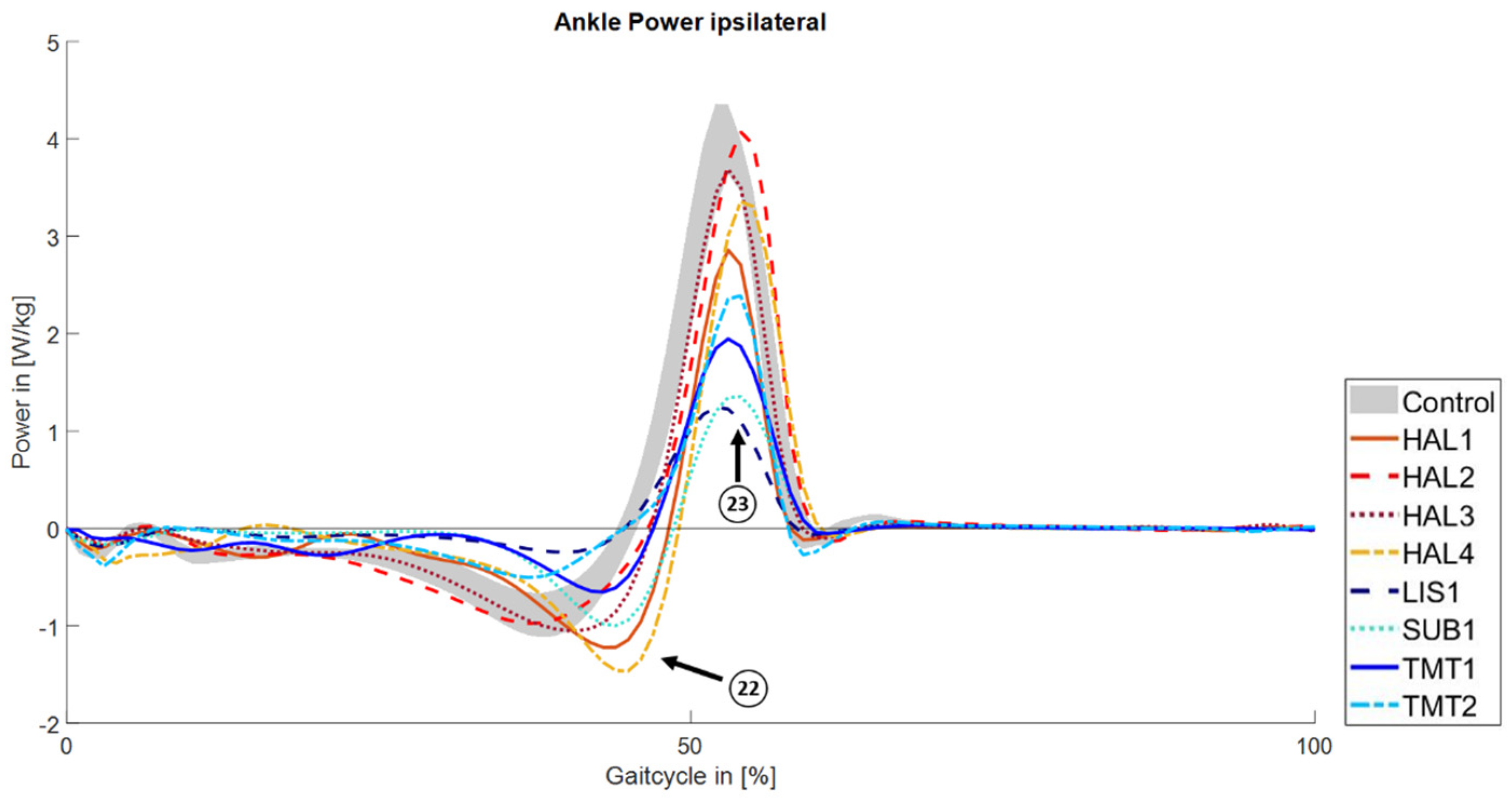
3.3. Kinetic Data
4. Discussion
4.1. Time-Distance Parameter
4.2. Methodological Challenges
4.3. Sagittal Plane Biomechanics
4.4. Frontal Plane Biomechanics
4.5. Implications for Novel Device Concepts
4.6. Limitations and Future Perspectives
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| RoM | range of motion |
| MTP | metatarsophalangeal |
| TMT | transmetatarsal |
| GRF | ground reaction force |
| CI | confidence interval |
| GVS | Gait Variable Score |
| mGPS | modified Gait Profile Score |
References
- Spoden, M.; Nimptsch, U.; Mansky, T. Amputation Rates of the Lower Limb by Amputation Level—Observational Study Using German National Hospital Discharge Data from 2005 to 2015. BMC Health Serv. Res. 2019, 19, 8. [Google Scholar] [CrossRef]
- Walter, N.; Alt, V.; Rupp, M. Lower Limb Amputation Rates in Germany. Medicina 2022, 58, 101. [Google Scholar] [CrossRef] [PubMed]
- Goodney, P.P.; Tarulli, M.; Faerber, A.E.; Schanzer, A.; Zwolak, R.M. Fifteen-Year Trends in Lower Limb Amputation, Revascularization, and Preventive Measures Among Medicare Patients. JAMA Surg. 2015, 150, 84. [Google Scholar] [CrossRef] [PubMed]
- De Oliveira, F.C.L.; Williamson, S.; Ardern, C.L.; Fagher, K.; Heron, N.; Janse Van Rensburg, D.C.; Jansen, M.G.T.; Kolman, N.; O’Connor, S.R.; Saueressig, T.; et al. Association between the Level of Partial Foot Amputation and Gait: A Scoping Review with Implications for the Minimum Impairment Criteria for Wheelchair Tennis. Br. J. Sports Med. 2023, 57, 237–248. [Google Scholar] [CrossRef]
- Aprile, I.; Galli, M.; Pitocco, D.; Di Sipio, E.; Simbolotti, C.; Germanotta, M.; Bordieri, C.; Padua, L.; Ferrarin, M. Does First Ray Amputation in Diabetic Patients Influence Gait and Quality of Life? J. Foot Ankle Surg. 2018, 57, 44–51. [Google Scholar] [CrossRef]
- Forczek-Karkosz, W.; Taylor, S.; Kicka, A.; Cappellini, G.; Dewolf, A.H.; Ivanenko, Y. Adjustments in the Range of Angular Motion during Walking after Amputation of the Toes: A Case Report. Symmetry 2021, 13, 2065. [Google Scholar] [CrossRef]
- Tang, S.F.T.; Chen, C.P.C.; Chen, M.J.L.; Chen, W.-P.; Leong, C.-P.; Chu, N.-K. Transmetatarsal Amputation Prosthesis with Carbon-Fiber Plate: Enhanced Gait Function. Am. J. Phys. Med. Rehabil. 2004, 83, 124–130. [Google Scholar] [CrossRef]
- Elabd, O.M.; El Nahass, B.G.; Ibrahim, M.M. Pathological Gait in Partial Foot Amputation versus Peripheral Neuropathy. Gait Posture 2023, 100, 41–48. [Google Scholar] [CrossRef]
- Mann, R.A.; Poppen, N.K.; O’Konski, M. Amputation of the Great Toe. A Clinical and Biomechanical Study. Clin. Orthop. Relat. Res. 1988, 226, 192–205. [Google Scholar] [CrossRef]
- Doi, N.; Pataky, T.; Tateuchi, H.; Nagai-Tanima, M.; Aoyama, T. Biomechanical Gait Analysis and Rehabilitation in a Traumatic Hallux Deficit Patient: A Case Report. J. Med. Case Rep. 2024, 18, 105. [Google Scholar] [CrossRef]
- Philbin, T.M.; Leyes, M.; Sferra, J.J.; Donley, B.G. Orthotic and Prosthetic Devices in Partial Foot Amputations. Foot Ankle Clin. 2001, 6, 215–228. [Google Scholar] [CrossRef] [PubMed]
- Janisse, D.J.; Janisse, E.J. Shoes, Orthoses, and Prostheses for Partial Foot Amputation and Diabetic Foot Infection. Foot Ankle Clin. 2010, 15, 509–523. [Google Scholar] [CrossRef] [PubMed]
- Mueller, M.J.; Salsich, G.B.; Bastian, A.J. Differences in the Gait Characteristics of People with Diabetes and Transmetatarsal Amputation Compared with Age-Matched Controls. Gait Posture 1998, 7, 200–206. [Google Scholar] [CrossRef] [PubMed]
- Dillon, M.P.; Fatone, S.; Hansen, A.H. Effect of Prosthetic Design on Center of Pressure Excursion in Partial Foot Prostheses. JRRD 2011, 48, 161. [Google Scholar] [CrossRef]
- Dillon, M.P.; Barker, T.M. Comparison of Gait of Persons with Partial Foot Amputation Wearing Prosthesis to Matched Control Group: Observational Study. J. Rehabil. Res. Dev. 2008, 45, 1317–1334. [Google Scholar]
- Dillon, M.P.; Barker, T.M. Can Partial Foot Prostheses Effectively Restore Foot Length? Prosthet. Orthot. Int. 2006, 30, 17–23. [Google Scholar] [CrossRef]
- Dillon, M.P.; Barker, T.M. Preservation of Residual Foot Length in Partial Foot Amputation: A Biomechanical Analysis. Foot Ankle Int. 2006, 27, 110–116. [Google Scholar] [CrossRef]
- Kaib, T.; Block, J.; Heitzmann, D.W.W.; Putz, C.; Alimusaj, M.; Wolf, S.I. Prosthetic Restoration of the Forefoot Lever after Chopart Amputation and Its Consequences onto the Limb during Gait. Gait Posture 2019, 73, 1–7. [Google Scholar] [CrossRef]
- Behling, A.; Rainbow, M.J.; Welte, L.; Kelly, L. Chasing Footprints in Time—Reframing Our Understanding of Human Foot Function in the Context of Current Evidence and Emerging Insights. Biol. Rev. 2023, 98, 2136–2151. [Google Scholar] [CrossRef]
- Doerks, F.; Riedel, L.; Einfeldt, A.-K.; Windhagen, H.; Hurschler, C.; Jakubowitz, E. Contribution of Various Forefoot Areas to Push-off Peak at Different Speeds and Slopes during Walking. Gait Posture 2024, 108, 264–269. [Google Scholar] [CrossRef]
- Kadaba, M.P.; Ramakrishnan, H.K.; Wootten, M.E. Measurement of Lower Extremity Kinematics during Level Walking. J. Orthop. Res. 1990, 8, 383–392. [Google Scholar] [CrossRef] [PubMed]
- Baker, R.; McGinley, J.L.; Schwartz, M.H.; Beynon, S.; Rozumalski, A.; Graham, H.K.; Tirosh, O. The Gait Profile Score and Movement Analysis Profile. Gait Posture 2009, 30, 265–269. [Google Scholar] [CrossRef] [PubMed]
- Pau, M.; Capodaglio, P.; Leban, B.; Porta, M.; Galli, M.; Cimolin, V. Kinematics Adaptation and Inter-Limb Symmetry during Gait in Obese Adults. Sensors 2021, 21, 5980. [Google Scholar] [CrossRef] [PubMed]
- Monfrini, R.; Rossetto, G.; Scalona, E.; Galli, M.; Cimolin, V.; Lopomo, N.F. Technological Solutions for Human Movement Analysis in Obese Subjects: A Systematic Review. Sensors 2023, 23, 3175. [Google Scholar] [CrossRef]
- Perry, J. Gait Analysis: Normal and Pathological Function. JAMA 1992, 268, 3257. [Google Scholar] [CrossRef]
- Bowker, J.H. Partial Foot Amputations and Disarticulations: Surgical Aspects. JPO J. Prosthet. Orthot. 2007, 19, 62–76. [Google Scholar] [CrossRef]
- Henson, D.P.; Edgar, C.; Ding, Z.; Sivapuratharasu, B.; Le Feuvre, P.; Finnegan, M.E.; Quest, R.; McGregor, A.H.; Bull, A.M.J. Understanding Lower Limb Muscle Volume Adaptations to Amputation. J. Biomech. 2021, 125, 110599. [Google Scholar] [CrossRef]
- Burger, H.; Erzar, D.; Maver, T.; Olenšek, A.; Cikajlo, I.; Matjačić, Z. Biomechanics of Walking with Silicone Prosthesis after Midtarsal (Chopart) Disarticulation. Clin. Biomech. 2009, 24, 510–516. [Google Scholar] [CrossRef]
- Haim, A.; Rozen, N.; Dekel, S.; Halperin, N.; Wolf, A. Control of Knee Coronal Plane Moment via Modulation of Center of Pressure: A Prospective Gait Analysis Study. J. Biomech. 2008, 41, 3010–3016. [Google Scholar] [CrossRef]
- D’Souza, N.; Charlton, J.; Grayson, J.; Kobayashi, S.; Hutchison, L.; Hunt, M.; Simic, M. Are Biomechanics during Gait Associated with the Structural Disease Onset and Progression of Lower Limb Osteoarthritis? A Systematic Review and Meta-Analysis. Osteoarthr. Cartil. 2022, 30, 381–394. [Google Scholar] [CrossRef]
- Kark, L.; Vickers, D.; McIntosh, A.; Simmons, A. Use of Gait Summary Measures with Lower Limb Amputees. Gait Posture 2012, 35, 238–243. [Google Scholar] [CrossRef] [PubMed]
- Fukuchi, C.A.; Fukuchi, R.K.; Duarte, M. Effects of Walking Speed on Gait Biomechanics in Healthy Participants: A Systematic Review and Meta-Analysis. Syst. Rev. 2019, 8, 153. [Google Scholar] [CrossRef]
- Chung, M.-J.; Wang, M.-J.J. The Change of Gait Parameters during Walking at Different Percentage of Preferred Walking Speed for Healthy Adults Aged 20–60 Years. Gait Posture 2010, 31, 131–135. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Lockhart, T.E. Comparison of 3D Joint Moments Using Local and Global Inverse Dynamics Approaches among Three Different Age Groups. Gait Posture 2006, 23, 480–485. [Google Scholar] [CrossRef] [PubMed]
- Zelik, K.E.; Honert, E.C. Ankle and Foot Power in Gait Analysis: Implications for Science, Technology and Clinical Assessment. J. Biomech. 2018, 75, 1–12. [Google Scholar] [CrossRef]
| Subject | Level of Amputation | Sex | Age (y) | Weight (kg) | Height (m) | Residual Length (% Contralateral Foot Length) | Cause of Amputation | Time since Amputation (y) |
|---|---|---|---|---|---|---|---|---|
| HAL1 | Hallux | F | 52 | 66.8 | 1.57 | 95.1 | Diabetes Type II | 6 |
| HAL2 | Hallux | M | 59 | 70.4 | 1.80 | 87.7 | Diabetes Type I | <1 |
| HAL3 | Hallux | F | 41 | 83.7 | 1.72 | 95.0 | Diabetes Type I | <1 |
| HAL4 | Hallux | F | 31 | 58.9 | 1.71 | 91.7 | Deformity | - |
| LIS1 | Lisfranc | F | 47 | 110.7 | 1.74 | 58.8 | Embolisms | 6 |
| SUB1 | Subtotal TMT * | F | 22 | 75.8 | 1.59 | 75.0 | Trauma | 19 |
| TMT1 | TMT | F | 56 | 54.1 | 1.59 | 62.2 | Trauma | 35 |
| TMT2 | TMT | M | 29 | 73.3 | 1.70 | 73.7 | Trauma | 4 |
| Subject | Walking Speed [m/s] | Stride Length Ipsilateral [m] | Stride Length Contralateral [m] | Foot Off Ipsilateral [%] | Foot Off Contralateral [%] |
|---|---|---|---|---|---|
| Controls | 1.41 ± 0.1 | 1.44 ± 0.1 | 58.93 ± 1.18 | ||
| HAL1 | 1.23 ± 0.05 | 1.15 ± 0.03 | 1.12 ± 0.01 | 58.32 ± 0.66 | 60.50 ± 0.27 |
| HAL2 | 1.23 ± 0.03 | 1.30 ± 0.03 | 1.32 ± 0.03 | 60.75 ± 0.55 | 60.85 ± 0.69 |
| HAL3 | 1.19 ± 0.03 | 1.20 ± 0.01 | 1.17 ± 0.01 | 59.58 ± 0.79 | 61.00 ± 0.80 |
| HAL4 | 1.26 ± 0.01 | 1.29 ± 0.01 | 1.27 ± 0.01 | 59.57 ± 0.92 | 59.51 ± 0.81 |
| LIS1 | 0.84 ± 0.04 | 1.09 ± 0.04 | 1.07 ± 0.03 | 58.18 ± 1.33 | 66.10 ± 1.00 |
| SUB1 | 1.15 ± 0.03 | 1.17 ± 0.03 | 1.17 ± 0.02 | 59.38 ± 0.60 | 64.11 ± 0.93 |
| TMT1 | 1.03 ± 0.03 | 1.07 ± 0.01 | 1.06 ± 0.01 | 59.09 ± 0.66 | 61.52 ± 0.57 |
| TMT2 | 1.39 ± 0.03 | 1.29 ± 0.02 | 1.30 ± 0.02 | 57.75 ± 0.59 | 61.03 ± 0.63 |
| Subject | GVSAnkle | GVSKnee | GVSHip | mGPS |
|---|---|---|---|---|
| HAL1 | 5.8° | 5.0° | 8.7° | 6.7° |
| HAL2 | 2.3° | 3.2° | 5.6° | 4.0° |
| HAL3 | 3.0° | 3.2° | 18.6° | 11.0° |
| HAL4 | 4.1° | 3.9° | 5.8° | 4.7° |
| LIS1 | 3.6° | 16.9° | 7.0° | 10.8° |
| SUB1 | 6.0° | 8.0° | 4.9° | 6.4° |
| TMT1 | 3.9° | 8.1° | 7.1° | 6.6° |
| TMT2 | 2.9° | 4.6° | 8.5° | 5.8° |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Doerks, F.; Gempfer, C.; Reulbach, M.; Jakubowitz, E. Gait Characteristics of People with Hallux and Forefoot Amputations—A Case Series. J. Clin. Med. 2025, 14, 2140. https://doi.org/10.3390/jcm14072140
Doerks F, Gempfer C, Reulbach M, Jakubowitz E. Gait Characteristics of People with Hallux and Forefoot Amputations—A Case Series. Journal of Clinical Medicine. 2025; 14(7):2140. https://doi.org/10.3390/jcm14072140
Chicago/Turabian StyleDoerks, Frithjof, Carina Gempfer, Magnus Reulbach, and Eike Jakubowitz. 2025. "Gait Characteristics of People with Hallux and Forefoot Amputations—A Case Series" Journal of Clinical Medicine 14, no. 7: 2140. https://doi.org/10.3390/jcm14072140
APA StyleDoerks, F., Gempfer, C., Reulbach, M., & Jakubowitz, E. (2025). Gait Characteristics of People with Hallux and Forefoot Amputations—A Case Series. Journal of Clinical Medicine, 14(7), 2140. https://doi.org/10.3390/jcm14072140







