Low Back Pain Among Health Sciences Undergraduates: Results Obtained from a Machine-Learning Analysis
Abstract
1. Introduction
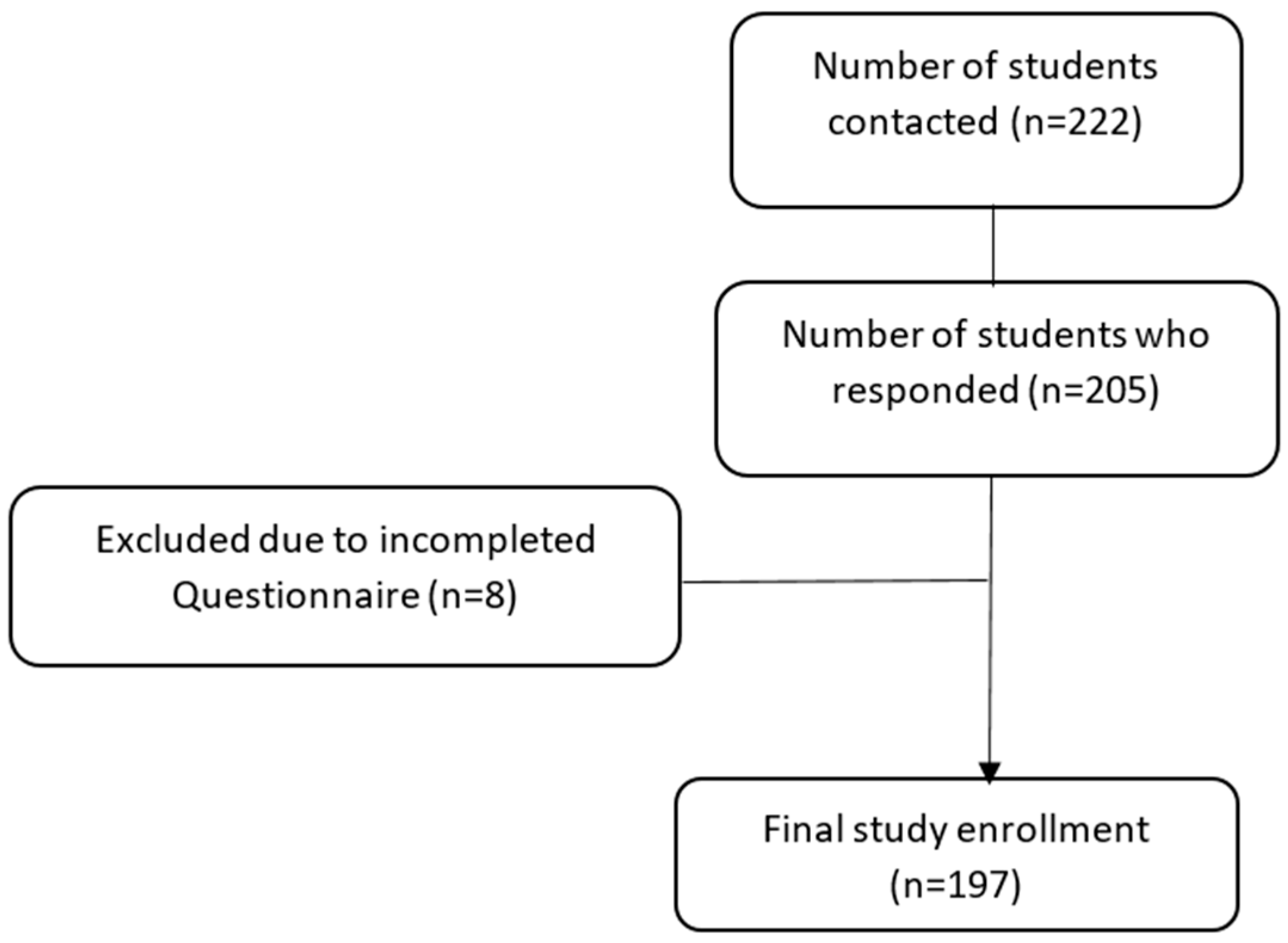
2. Materials and Methods
2.1. Instruments and Measures
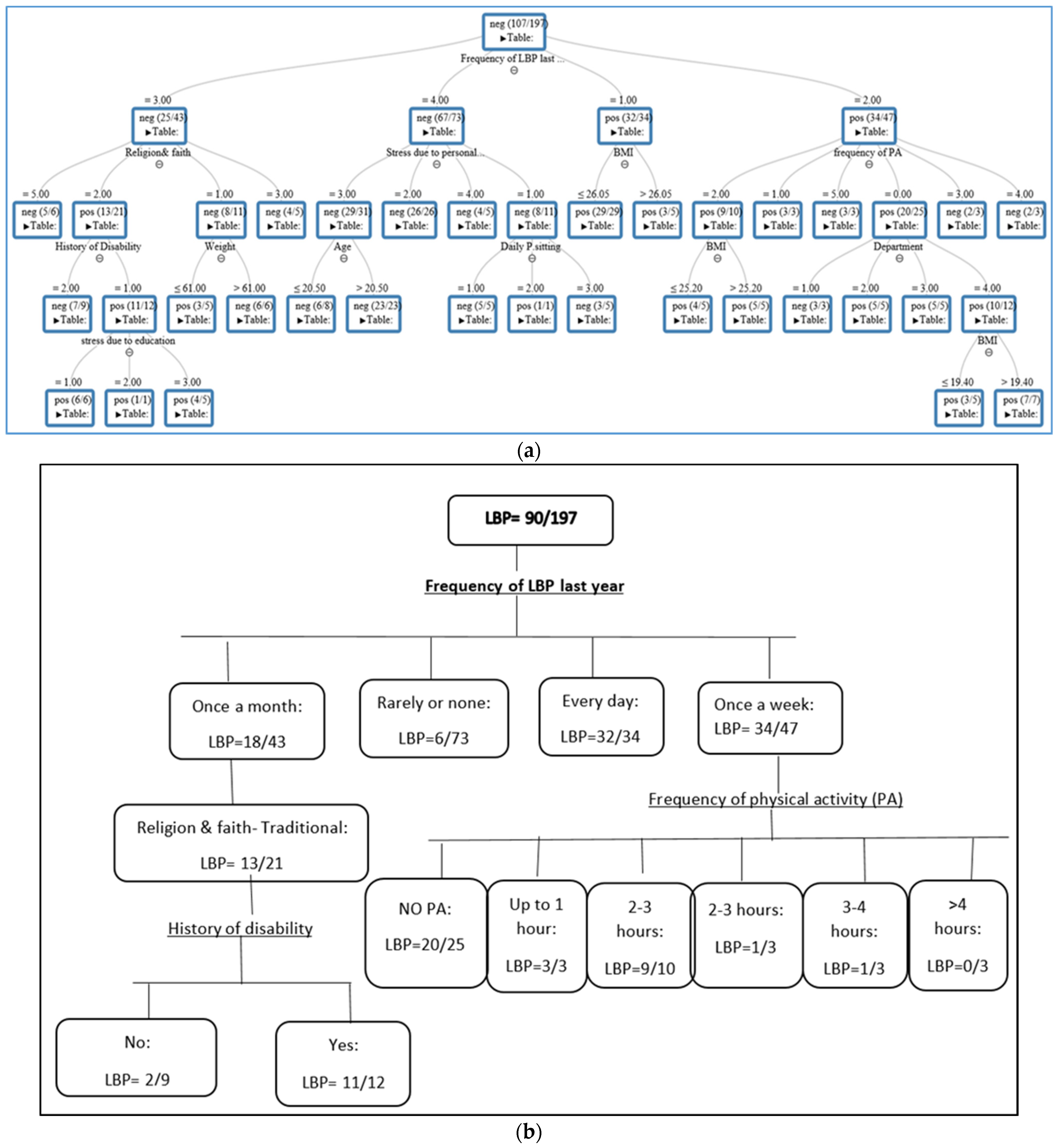
2.2. Statistical and Supervised Machine-Learning Analyses
3. Results
3.1. Student Characteristics
3.2. Low Back Pain
4. Discussion
5. Limitations of the Study
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Itz, C.J.; Geurts, J.W.; van Kleef, M.; Nelemans, P. Clinical course of non-specific low back pain: A systematic review of prospective cohort studies set in primary care. Eur. J. Pain 2013, 17, 5–15. [Google Scholar] [CrossRef] [PubMed]
- Gaonkar, A.P.; Kulkarni, R.; Caytiles, R.D.; Iyengar, N. Classification of Lower Back Pain Disorder Using Multiple Machine Learning Techniques and Identifying Degree of Importance of Each Parameter. Int. J. Adv. Sci. Technol. 2017, 105, 11–24. [Google Scholar] [CrossRef]
- Lall, M.P.; Restrepo, E. The biopsychosocial model of low back pain and patient-centered outcomes following lumbar fusion. Orthop. Nurs. 2017, 36, 213–221. [Google Scholar] [CrossRef] [PubMed]
- Crawford, R.J.; Volken, T.; René Schaffert, R.; Bucher, T. Higher low back and neck pain in final year Swiss health professions’ students: Worrying susceptibilities identified in a multi-centre comparison to the national population. BMC Public Health 2018, 8, 1188. [Google Scholar] [CrossRef]
- Cakmak, A.; Yücel, B.; Ozyalçn, S.N. The frequency and associated factors of low back pain among a younger population in Turkey. Spine 2004, 29, 1567–1572. [Google Scholar] [CrossRef]
- Wong, A.Y.L.; Chan, L.L.Y.; Lo, C.W.T.; Chan, W.W.Y.; Lam, K.C.K.; Bao, J.C.H.; Ferreira, M.L.; Armijo-Olivo, S. Prevalence/Incidence of Low Back Pain and Associated Risk Factors Among Nursing and Medical Students: A Systematic Review and Meta-Analysis. PM&R 2021, 13, 1266–1280. [Google Scholar]
- Nyland, L.J.; Grimmer, K.A. Is undergraduate physiotherapy student a risk factor for low back pain? A prevalence study of low back pain in physiotherapy students. BMC Musculoskelet. Disord. 2003, 4, 22. [Google Scholar] [CrossRef]
- Falavigna, A.; Teles, A.R.; Mazzocchin, T.; de Braga, G.L.; Kleber, F.D.; Barreto, F.; Santin, J.T.; Barazzetti, D.; Lazzaretti, L.; Steiner, B.; et al. Increased prevalence of low back pain among physiotherapy students compared to medical students. Eur. Spine J. 2011, 20, 500–505. [Google Scholar] [CrossRef]
- Algarni, A.D.; Al-Saran, Y.; Al-Moawi, A.; Bin Dous, A.; Al-Ahaideb, A.; Kachanathu, S.J. The prevalence of and factors associated with neck, shoulder, and low-back pains among medical students at university hospitals in Central Saudi Arabia. Pain Res. Treat. 2017, 1, 1235706. [Google Scholar] [CrossRef]
- Feyer, A.M.; Herbison, P.; Williamson, A.M. The role of physical and psychological factors in occupational low back pain: A prospective cohort study. Occup. Environ. Med. 2000, 57, 116–120. [Google Scholar] [CrossRef]
- Mitchell, T.; O’Sullivan, P.B.; Burnett, A. Identification of modifiable personal factors that predict new-onset low back pain: A prospective study of female nursing students. Clin. J. Pain 2010, 26, 275–283. [Google Scholar] [CrossRef]
- Amelot, A.; Mathon, B.; Haddad, R.; Renault, M.C.; Duguet, A.; Steichen, O. Low Back Pain among Medical Students: A Burden and an Impact to Consider! Spine 2019, 44, 1390–1395. [Google Scholar] [CrossRef]
- AlShayhan, F.A.; Saadeddin, M. Prevalence of low back pain among health sciences students. Eur. J. Orthop. Surg. Traumatol. 2018, 28, 165–170. [Google Scholar] [CrossRef]
- Khan, O.; Badhiwala, J.H.; Wilson, J.R.F.; Jiang, F.; Martin, A.R.; Fehlings, M.G. Predictive modeling of outcomes after traumatic and nontraumatic spinal cord injury using machine learning: Review of current progress and future directions. Neurospine 2019, 16, 678–685. [Google Scholar] [CrossRef]
- Senders, J.T.; Staples, P.C.; Karhade, A.V.; Zaki, M.M.; Gormley, W.B.; Broekman, M.L.; Smith, T.R.; Arnaout, O. Machine learning and neurosurgical outcome prediction: A systematic review. World Neurosurg. 2018, 109, 476–486.e1. [Google Scholar]
- LeCun, Y.; Bengio, Y.; Hinton, G. Deep learning. Nature 2015, 521, 436–444. [Google Scholar] [CrossRef]
- Ren, G.; Yu, K.; Xie, Z.; Wang, P.; Zhang, W.; Huang, Y.; Wang, Y.; Wu, X. Current Applications of Machine Learning in Spine: From Clinical View. Glob. Spine J. 2021, 28, 521, 436–444. [Google Scholar] [CrossRef]
- Galbusera, F.; Casaroli, G.; Bassani, T. Artificial intelligence and machine learning in spine research. JOR Spine 2019, 2, e1044. [Google Scholar] [CrossRef]
- Azimi, P.; Yazdanian, T.; Benzel, E.C.; Aghaei, H.N.; Azhari, S.; Sadeghi, S.; Montazeri, A. A Review on the Use of Artificial Intelligence in Spinal Diseases. Asian Spine J. 2020, 14, 543–571. (In English) [Google Scholar]
- Tagliaferri, S.D.; Angelova, M.; Zhao, X.; Owenet, P.J.; Miller, C.T.; Wilkin, T.; Belavy, D.L. Artificial intelligence to improve back pain outcomes and lessons learnt from clinical classification approaches: Three systematic reviews. NPJ Digit. Med. 2020, 3, 93. [Google Scholar]
- Kuorinka, I.; Jonsson, B.; Kilbom, A. Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl. Ergon. 1987, 18, 233–237. [Google Scholar] [CrossRef]
- Jessor, R.; Turbin, M.S.; Costa, M.F. Survey of Personal and Social Development at CU; Institute of Behavioral Sciences, University of Colorado: Boulder, CO, USA, 2003; Volume 19, p. 2016. Available online: http://www.colorado.edu/ibs/jessor/questionnaires/questionnaire_spsd2.pdf (accessed on 15 December 2021).
- Thompson, W.R.; Gordon, N.F.; Pescatello, L.S. American College of Sport Medicine. In ACSM’s Guidelines for Exercise Testing and Prescription, 9th ed.; Lippincott Williams and Wilkins: Philadelphia, PA, USA, 2014. [Google Scholar]
- Fairbank, J.C.; Pynsent, P.B. The Oswestry Disability Index. Spine 2000, 25, 2940–2952. [Google Scholar] [CrossRef]
- Dionne, C.E.; Dunn, K.M.; Croft, P.R. A consensus approach toward the standardization of back pain definitions for use in prevalence studies. Spine 2008, 33, 95–103. [Google Scholar] [CrossRef]
- Breiman, L. Random forests. Mach. Learn. 2001, 45, 5–32. [Google Scholar] [CrossRef]
- Biau, G.; Scornet, E. A random forest guided tour. Test 2016, 25, 197–227. [Google Scholar] [CrossRef]
- Picard, R.R.; Cook, R.D. Cross-validation of regression models. J. Am. Stat. Assoc. 1984, 79, 575–583. [Google Scholar] [CrossRef]
- Feng, Y.; Wang, Z.; Cui, R.; Xiao, M.; Gao, H.; Bai, H.; Delvoux, B.; Dekker, A.; Romano, A.; Wang, S.; et al. Clinical analysis and artificial intelligence survival prediction of serous ovarian cancer based on preoperative circulating leukocytes. J. Ovarian Res. 2022, 15, 64. [Google Scholar] [CrossRef]
- Muhaimil, A.; Pendem, S.; Sampathilla, N.; Priya, P.S.; Nayak, K.; Chadaga, K.; Goswami, A.; Chandran, O.M.; Shirlal, A. Role of Artificial intelligence model in prediction of low back pain using T2 weighted MRI of Lumbar spine. F1000Research 2024, 13, 1035. [Google Scholar] [CrossRef]
- Dasgupta, P.; Kuhn, L.M.; Sekeroglu, K.; Prasai, A. A mathematical modelling approach for analysing the risk of low back pain in college students using student desks. Int. J. Hum. Factors Ergon. 2023, 10, 85–112. [Google Scholar] [CrossRef]
- Shim, J.G.; Ryu, K.H.; Cho, E.A.; Ahn, J.H.; Kim, H.K.; Lee, Y.-J.; Lee, S.H. Machine learning approaches to predict chronic lower back pain in people aged over 50 years. Medicina 2021, 57, 1230. [Google Scholar] [CrossRef]
- Mitchell, T.; O’Sullivan, P.B.; Burnett, A.F. Low back pain characteristics from undergraduate student to working nurse in Australia: A cross-sectional survey. Int. J. Nurs. Stud. 2008, 45, 1636–1644. [Google Scholar] [CrossRef]
- Nordin, N.; Singh, D.; Kanglun, L. Low back pain and associated risk factors among health science undergraduates. Sains Malays. 2014, 43, 423–428. [Google Scholar]
- Hafeez, K.; Memon, A.A.; Jawaid, M. Back pain-are health care undergraduates at risk? Iran. J. Public Health 2013, 42, 819–825. [Google Scholar] [PubMed]
- Yucel, H.; Torun, P. Incidence and Risk Factors of Low Back Pain in Students Studying at a Health University. Bezmialem Sci. 2016, 4, 12–18. [Google Scholar] [CrossRef]
- Anggiat, L.; Hon, W.H.C.; Baait, W.S.N. The incidence of Low back pain among university students. J. Pro-Life 2018, 5, 677–687. [Google Scholar]
- Smedley, J.; Trevelyan, F.; Inskip, H. Impact of ergonomic intervention on back pain among nurses. Scand. J. Work. Environ. Health 2003, 29, 117–123. [Google Scholar] [CrossRef]
- Maul, I.; Läubli, T.; Klipstein, A.; Krueger, H. Course of low back pain among nurses: A longitudinal study across eight years. Occup. Environ. Med. 2003, 60, 497–503. [Google Scholar] [CrossRef]
- Da-Silva, T.; Mills, K.; Brown, B.T. Risk of Recurrence of Low Back Pain: A Systematic Review. J. Orthop. Sports Phys. Ther. 2017, 47, 305–313. [Google Scholar] [CrossRef]
- Machado, G.C.; Maher, C.G.; Ferreira, P.H.; Latimer, J.; Koes, B.W.; Steffens, D.; Ferreira, M.L. Can recurrence after an acute episode of low back pain be predicted? Phys. Ther. 2017, 97, 889–895. [Google Scholar] [CrossRef]
- Alshagga, M.A.; Nimer, A.R.; Yan, L.P.; Ibrahim, I.A.A.; Al-Ghamdi, S.S.; Al-Dubai, S.A.R. Prevalence and factors associated with neck, shoulder and low back pains among medical students in a Malaysian Medical College. BMC Res. Notes 2013, 6, 244. [Google Scholar] [CrossRef]
- Citko, A.; Górski, S.; Marcinowicz, L.; Górska, A. Sedentary Lifestyle and nonspecific low back pain in medical personnel in North-East Poland. BioMed Res. Int. 2018, 2018, 1965807. [Google Scholar] [CrossRef] [PubMed]
- van den Heuvel, S.G.; Ariëns, G.A.; Boshuizen, H.C.; Hoogendoorn, W.E.; Bongers, P.M. Prognostic factors related to recurrent low-back pain and sickness absence. Scand. J. Work. Environ. Health 2004, 1, 459–467. [Google Scholar] [CrossRef] [PubMed]
- Estlander, A.M.; Takala, E.P.; Viikari-Juntura, E. Do psychological factors predict changes in musculoskeletal pain? J. Occup. Environ. Med. 1998, 5, 445–453. [Google Scholar] [CrossRef]
- Mitchell, T.; O’Sullivan, P.B.; Smith, A. Biopsychosocial factors are associated with low back pain in female nursing students: A cross-sectional study. Int. J. Nurs. Stud. 2009, 46, 678–688. [Google Scholar] [CrossRef]
- Skoffer, B.; Foldspang, A. Physical activity and low-back pain in schoolchildren. Eur. Spine J. 2008, 17, 373–379. [Google Scholar] [CrossRef]
- Felemban, R.A.; Sofi, R.A.; Alhebshi, S.A.; Alharbi, S.G.; Farsi, N.J.; Abduljabbar, F.H.; Farsi, J.M. Prevalence and predictors of musculoskeletal pain among undergraduate students at a dental school in Saudi Arabia. Clin. Cosmet. Investig. Dent. 2021, 17, 39–46. [Google Scholar] [CrossRef]
- Warburton, D.E.; Nicol, C.W.; Bredin, S.S. Health benefits of physical activity: The evidence. Can. Med. Assoc. J. 2006, 174, 801–809. [Google Scholar] [CrossRef]
- O’Donovan, G.; Lee, I.M.; Hamer, M.; Stamatakis, E. Association of “Weekend Warrior” and Other Leisure Time Physical Activity Patterns with Risks for All-Cause, Cardiovascular Disease, and Cancer Mortality. JAMA Intern. Med. 2017, 177, 335–342. [Google Scholar] [CrossRef]
- Sadarangani, K.P.; Hamer, M.; Mindell, J.S.; Coombs, N.A.; Stamatakis, E. Physical activity and risk of all-cause and cardiovascular disease mortality in diabetic adults from Great Britain: Pooled analysis of 10 population-based cohorts. Diabetes Care 2014, 37, 1016–1023. [Google Scholar] [CrossRef]
- National Institute for Health and Clinical Excellence. Physical Activity: Exercise Referral Schemes; National Institute for Health and Clinical Excellence: London, UK, 2014. [Google Scholar]
- Iwamoto, J.; Abe, H.; Tsukimura, Y.; Wakano, K. Relationship between radiographic abnormalities of lumbar spine and incidence of low back pain in high school and college football players: A prospective study. Am. J. Sports Med. 2004, 32, 781–786. [Google Scholar] [CrossRef]
- Lundin, O.; Hellstrom, M.; Nilsson, I.; Sward, L. Back pain and radiological changes in the thoracolumbar spine of athletes: A long term follow-up. Scand. J. Med. Sci. Sports 2001, 11, 103–109. [Google Scholar] [CrossRef]
- Heneweer, H.; Staes, F.; Aufdemkampe, G.; van Rijn, M.; Vanhees, L. Physical activity and low back pain: A systematic review of recent literature. Eur. Spine J. 2001, 20, 826–845. [Google Scholar] [CrossRef] [PubMed]
- Alzahrani, H.; Martin Mackey, M.; Stamatakis, E.; Zadro, J.R.; Shirley, D. The association between Physical activity and low back pain: A systematic review and meta-analysis of observation studies. Sci. Rep. 2019, 9, 8244. [Google Scholar] [CrossRef] [PubMed]
- Keating, X.D.; Guan, J.; Piñero, J.C.; Bridges, D.M. A meta-analysis of college students’ physical activity behaviors. J. Am. Coll. Health 2005, 54, 116–126. [Google Scholar] [CrossRef] [PubMed]
- Jakubiec, D.; Kornafel, D.; Cygan, A.; Gorska-Klek, L.; Chromik, K. Lifestyle of students from different universities in Wroclaw, Poland. Rocz. Państwowego Zakładu Hig. 2015, 66, 337–344. [Google Scholar]
- Almutairi, K.M.; Alonazi, W.B.; Vinluan, J.M.; Almigbal, T.H.; Batais, M.A.; Al Odhayani, A.; Alsadhan, N.; Tumala, R.B.; Moussa, M.; Aboshaiqah, A.E.; et al. Health promoting lifestyle of university students in Saudi Arabia: A cross-sectional assessment. BMC Public Health 2018, 8, 1093. [Google Scholar] [CrossRef]
- Sigmundová, D.; ChmelÍk, F.; Sigmund, E.; Feltlová, D.; Frömel, K. Physical activity in the lifestyle of Czech university students: Meeting health recommendations. Eur. J. Sport Sci. 2013, 13, 744–750. [Google Scholar] [CrossRef]
- Deliens, T.; Deforche, B.; De Bourdeaudhuij, I.; Clarys, P. Determinants of physical activity and sedentary behaviour in university students: A qualitative study using focus group discussions. BMC Public Health 2015, 15, 201. [Google Scholar] [CrossRef]
- Descatha, A.; Roquelaure, Y.; Chastang, J.F.; Evanoff, B.; Melchior, M.; Mariot, C.; Ha, C.; Imbernon, E.; Goldberg, M.; Leclerc, A. Validity of Nordic-style questionnaires in the surveillance of upper-limb work-related musculoskeletal disorders. Scand. J. Work. Environ. Health 2007, 33, 58–65. [Google Scholar] [CrossRef]
- Baron, S.; Hales, T.; Hurrell, J. Evaluation of symptom surveys for occupational musculoskeletal disorders. Am. J. Ind. Med. 1996, 29, 609–617. [Google Scholar] [CrossRef]
- Crawford, J.O. The Nordic Musculoskeletal Questionnaire. Occup. Med. 2007, 57, 300–301. [Google Scholar] [CrossRef]
- Palmer, K.; Smith, G.; Kellingray, S.; Cooper, C. Repeatability and validity of an upper limb and neck discomfort questionnaire: The utility of the standardized Nordic questionnaire. Occup. Med. 1999, 49, 171–175. [Google Scholar] [CrossRef]
- Moons, K.G.; Kengne, A.P.; Woodward, M.; Royston, P.; Vergouwe, Y.; Altman, D.G.; Grobbee, D.E. Risk prediction models: I. Development, internal validation, and assessing the incremental value of a new (bio) marker. Heart 2012, 98, 683–690. [Google Scholar] [CrossRef]
- Wolff, R.F.; Moons, K.G.; Riley, R.D.; Whiting, P.F.; Westwood, M.; Collins, G.S.; Reitsma, J.B.; Kleijnen, J.; Mallett, S.; PROBAST Group. PROBAST: A tool to assess the risk of bias in prediction model studies. Ann. Intern. Med. 2019, 170, 51–58. [Google Scholar] [CrossRef]
- Hancock, M.J.; Maher, C.G.; Latimer, J.; Herbert, R.D.; McAuley, J.H. Can predictors of response to NSAIDs be identified in patients with acute low back pain? Clin. J. Pain 2011, 27, 535–540. [Google Scholar] [CrossRef]
- Cuenca-Zaldívar, J.N.; Fernández-Carnero, J.; Sánchez-Romero, E.A.; Álvarez-Gonzalo, V.; Conde-Rodríguez, R.; Rodríguez-Sanz, D.; Calvo-Lobo, C. Effects of a Therapeutic Exercise Protocol for Patients with Chronic Non-Specific Back Pain in Primary Health Care: A Single-Group Retrospective Cohort Study. J. Clin. Med. 2023, 12, 6478. [Google Scholar] [CrossRef]
| % (n)/or Mean ± SD | |
|---|---|
| 89 (197) | Response rate |
| 25 (49) | Male |
| 75 (148) | Female |
| Department: | |
| 45 (89) | Nursing |
| 21 (41) | Physical Therapy |
| 19 (37) | Medical Lab |
| 15(30) | Emergency Medical Services |
| 23 ± 3.8 | Mean age (year) |
| 23 ± 3.5 | Mean BMI (kg/m2) |
| 91 (179) | Dominant right hand |
| Marital status: | |
| 93 (184) | Single |
| 7 (13) | Other |
| 15 (30) | Smoking |
| Religion & faith: | |
| 30 (60) | Secular |
| 43 (84) | Traditional |
| 13 (26) | Religious/orthodox |
| 14 (27) | Other |
| 55 (108) | Those with physical activity (wk): |
| 7 (14) | 20 min to 1 h |
| 19 (37) | 1–2 h |
| 10 (20) | 2–3 h |
| 9 (18) | 3–4 h |
| 10 (19) | >4 h |
| Prolonged daily sitting: | |
| 40 (78) | Up to 3 h |
| 23 (45) | 3–5 h |
| 37 (74) | 5 h> |
| Total daily sitting: | |
| 32 (63) | Up to 6 h |
| 30 (60) | 6–8 h |
| 38 (74) | >8 h |
| * Study-related stress: | |
| 85 (167) | Very high–quite high |
| 15 (30) | Little–none |
| N (%) | |
|---|---|
| 146 (74) | Those who experienced LBP at some point in their life |
| 8 (4) | Those who had been hospitalized due to LBP |
| LBP in the last year: | |
| 1. Frequency of LBP: | |
| 34 (17) |
|
| 47 (24) |
|
| 43 (22) |
|
| 73 (37) |
|
| 65 (33) | 2. Disability |
| 39 (20) | 3. Seeking care |
| 39 (20) | 4. Medication consumption |
| 90 (46) | 1-month LBP |
| Accuracy | Recall | Specificity | Precision | F1 | Area Under Curve | |
|---|---|---|---|---|---|---|
| Mean | 0.84 | 0.93 | 0.76 | 0.79 | 0.84 | 0.88 |
| SD | 0.09 | 0.09 | 0.18 | 0.13 | 0.07 | 0.07 |
| Variable | Score |
|---|---|
| Frequency of LBP | 1 |
| History of Disability | 0.34 |
| Frequency of physical activity (PA) | 0.21 |
| Weight | 0.18 |
| Religion and faith | 0.13 |
| Department | 0.12 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abbas, J.; Yousef, M.; Hamoud, K.; Joubran, K. Low Back Pain Among Health Sciences Undergraduates: Results Obtained from a Machine-Learning Analysis. J. Clin. Med. 2025, 14, 2046. https://doi.org/10.3390/jcm14062046
Abbas J, Yousef M, Hamoud K, Joubran K. Low Back Pain Among Health Sciences Undergraduates: Results Obtained from a Machine-Learning Analysis. Journal of Clinical Medicine. 2025; 14(6):2046. https://doi.org/10.3390/jcm14062046
Chicago/Turabian StyleAbbas, Janan, Malik Yousef, Kamal Hamoud, and Katherin Joubran. 2025. "Low Back Pain Among Health Sciences Undergraduates: Results Obtained from a Machine-Learning Analysis" Journal of Clinical Medicine 14, no. 6: 2046. https://doi.org/10.3390/jcm14062046
APA StyleAbbas, J., Yousef, M., Hamoud, K., & Joubran, K. (2025). Low Back Pain Among Health Sciences Undergraduates: Results Obtained from a Machine-Learning Analysis. Journal of Clinical Medicine, 14(6), 2046. https://doi.org/10.3390/jcm14062046








