Surgical Treatment of Calcaneal Fractures by Minimally Invasive Technique Using a 2-Point Distractor Versus ORIF and Conservative Therapy—A Retrospective Multicenter Study
Abstract
1. Introduction
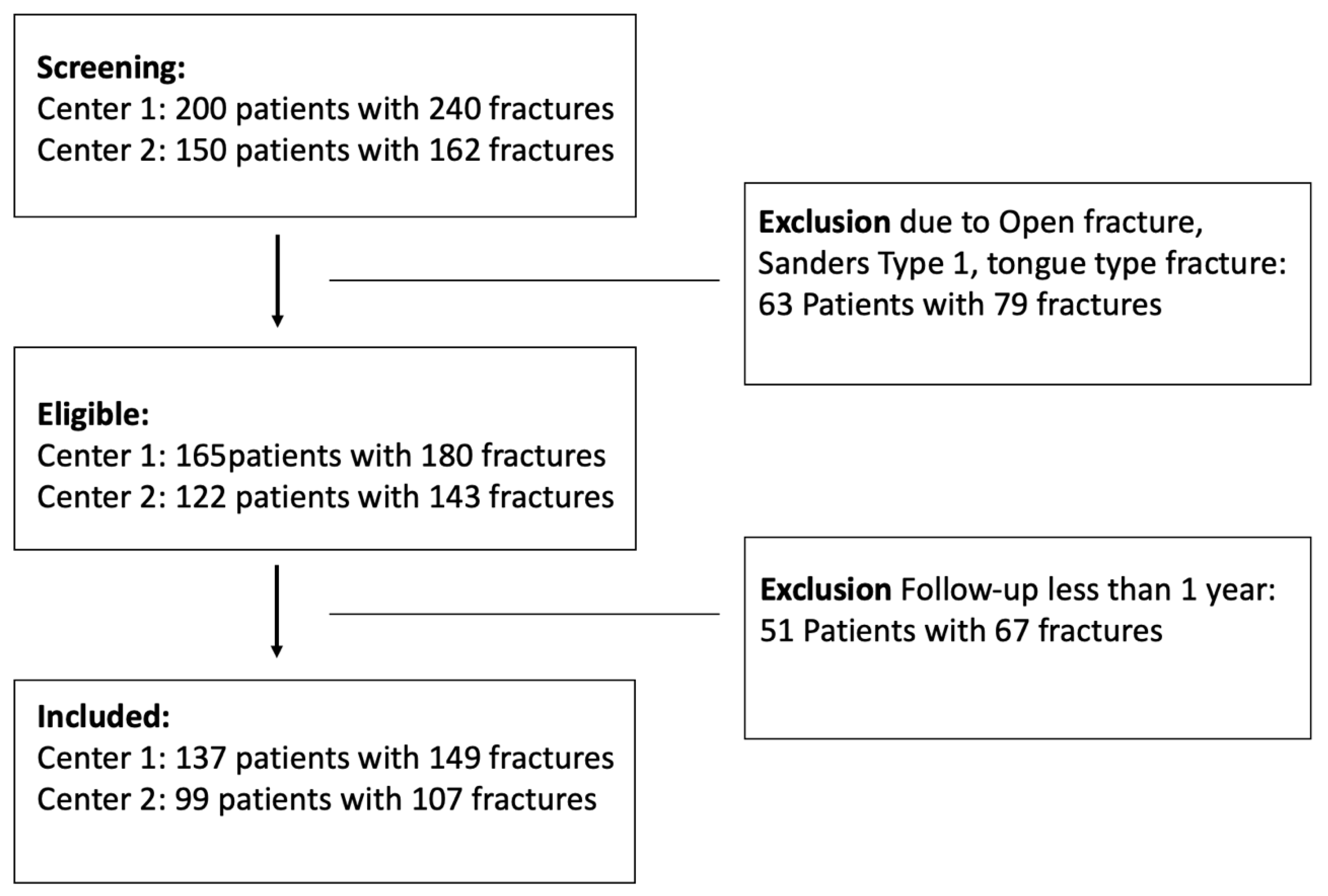
2. Materials and Methods
2.1. Inclusion and Exclusion Criteria
2.2. Treatment Methods
2.3. Evaluation
3. Results
3.1. Complications
3.2. Evaluation of the Scores
4. Discussion
4.1. Quality of Anatomical Reductions
4.2. Complications Within the Three Cohorts
4.3. Functional Outcome
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Worsham, J.R.; Elliott, M.R.; Harris, A.M. Open Calcaneus Fractures and Associated Injuries. J. Foot Ankle Surg. 2016, 55, 8–71. [Google Scholar] [CrossRef] [PubMed]
- Tantavisut, S.; Phisitkul, P.; Westerlind, B.O.; Gao, Y.; Karam, M.D.; Marsh, J.L. Percutaneous Reduction and Screw Fixation of Displaced Intra-articular Fractures of the Calcaneus. Foot Ankle Int. 2017, 38, 367–374. [Google Scholar] [CrossRef]
- Griffin, D.; Parsons, N.; Shaw, E.; Kulikov, Y.; Hutchinson, C.; Thorogood, M. Operative versus non-operative treatment for closed, displaced, intra-articular fractures of the calcaneus: Randomised controlled trial. BMJ 2014, 349, g4483. [Google Scholar] [CrossRef] [PubMed]
- Sanders, R. Intra-articular fractures of the calcaneus: Present state of the art. J. Orthop. Trauma 1992, 6, 252–265. [Google Scholar] [CrossRef] [PubMed]
- Rammelt, S.; Zwipp, H. Calcaneus fractures: Facts, controversies and recent developments. Injury 2004, 35, 443–461. [Google Scholar] [CrossRef]
- Kline, A.J.; Anderson, R.B.; Davis, W.H.; Jones, C.P.; Cohen, B.E. Minimally invasive technique versus an extensile lateral approach for intra-articular calcaneal fractures. Foot Ankle Int. 2013, 34, 773–780. [Google Scholar] [CrossRef]
- Rammelt, S.; Amlang, M.; Barthel, S.; Gavlik, J.M.; Zwipp, H. Percutaneous treatment of less severe intraarticular calcaneal fractures. Clin. Orthop. Relat. Res. 2010, 468, 983–990. [Google Scholar] [CrossRef]
- Randle, J.A.; Kreder, H.J.; Stephen, D.; Williams, J.; Jaglal, S.; Hu, R. Should calcaneal fractures be treated surgically? A meta-analysis. Clin. Orthop. Relat. Res. 2000, 377, 217–227. [Google Scholar] [CrossRef]
- Ibrahim, T.; Rowsell, M.; Rennie, W.; Brown, A.R.; Taylor, G.J.S.; Gregg, P.J. Displaced intra-articular calcaneal fractures: 15-Year follow-up of a randomised controlled trial of conservative versus operative treatment. Injury 2007, 38, 848–855. [Google Scholar] [CrossRef]
- Agren, P.H.; Wretenberg, P.; Sayed-Noor, A.S. Operative versus nonoperative treatment of displaced intra-articular calcaneal fractures: A prospective, randomized, controlled multicenter trial. J. Bone Jt. Surg. 2013, 95, 1351–1357. [Google Scholar] [CrossRef]
- Fröhlich, P.; Zakupszky, Z.; Csomor, L. Erfahrungen mit der gedeckten verschraubung intraartikularer fersenbeinbruche: Operationstechnik und klinische ergebnisse. Unfallchirurg. 1999, 102, 359–364. [Google Scholar] [CrossRef] [PubMed]
- Paul, M.; Peter, R.; Hoffmeyer, P. Fractures of the calcaneum. A review of 70 patients. J. Bone Jt. Surg. Br. 2004, 86, 1142–1145. [Google Scholar] [CrossRef]
- Makki, D.; Alnajjar, H.M.; Walkay, S.; Ramkumar, U.; Watson, A.J.; Allen, P.W. Osteosynthesis of displaced intra-articular fractures of the calcaneum: A long-term review of 47 cases. J. Bone Jt. Surg. Br. 2010, 92, 693–700. [Google Scholar] [CrossRef] [PubMed]
- Pradana, A.S.; Mustamsir, E.; Breilyan, S.; Putra, D.P.; Phatama, K.Y.; Hidayat, M. Plating technique outcome evaluation in calcaneal fracture based on American orthopaedics foot and ankle score and Bohler-Gissane angle: A case series. Int. J. Surg. Case Rep. 2022, 94, 107131. [Google Scholar] [CrossRef]
- Wei, N.; Yuwen, P.; Liu, W.; Zhu, Y.; Chang, W.; Feng, C. Operative versus nonoperative treatment of displaced intra-articular calcaneal fractures: A meta-analysis of current evidence base. Medicine 2017, 96, e9027. [Google Scholar] [CrossRef]
- Bruce, J.; Sutherland, A. Surgical versus conservative interventions for displaced intra-articular calcaneal fractures. Cochrane Database Syst. Rev. 2013, 1, CD008628. [Google Scholar] [CrossRef]
- Fan, B.; Zhou, X.; Wei, Z.; Ren, Y.; Lin, W.; Hao, Y. Cannulated screw fixation and plate fixation for displaced intra-articular calcaneus fracture: A meta-analysis of randomized controlled trials. Int. J. Surg. 2016, 34, 64–72. [Google Scholar] [CrossRef] [PubMed]
- Rastegar, S.; Ravanbod, H.; Moradi, M.; Moradi, N. Extensile approach versus minimally invasive technique in management of calcaneus fractures. Int. J. Burn. Trauma. 2021, 11, 27–33. [Google Scholar]
- Biz, C.; Barison, E.; Ruggieri, P.; Iacobellis, C. Radiographic and functional outcomes after displaced intra-articular calcaneal fractures: A comparative cohort study among the traditional open technique (ORIF) and percutaneous surgical procedures. J. Orthop. Surg. Res. 2016, 11, 92. [Google Scholar] [CrossRef]
- De Boer, A.S.; Van Lieshout, E.M.; Hartog, D.D.; Weerts, B.; Verhofstad, M.H.; Schepers, T. Functional outcome and patient satisfaction after displaced intra-articular calcaneal fractures: A comparison among open, percutaneous, and nonoperative treatment. J. Foot Ankle Surg. 2015, 54, 298–305. [Google Scholar] [CrossRef]
- Ding, L.; He, Z.; Xiao, H.; Chai, L.; Xue, F. Risk factors for postoperative wound complications of calcaneal fractures following plate fixation. Foot Ankle Int. 2013, 34, 1238–1244. [Google Scholar] [CrossRef] [PubMed]
- Khurana, A.; Dhillon, M.S.; Prabhakar, S.; John, R. Outcome evaluation of minimally invasive surgery versus extensile lateral approach in management of displaced intra- articular calcaneal fractures: A randomised control trial. Foot 2017, 31, 23–30. [Google Scholar] [CrossRef] [PubMed]
- Reddy, S.V.; Gavi Raj, R. Functional outcome of intraarticular calcaneal fracture managed by open reduction and internal fixation. Int. J. Life Sci. Biotechnol. Pharma Res. 2023, 12, 449–453. [Google Scholar]



| ORIF | MIT | CT | p | |
|---|---|---|---|---|
| Number of patients | 60 | 70 | 106 | 0.02 |
| Age (mean ± standard deviation) | 45.1 ± 13.1 | 48.8 ± 13.1 | 44.8 ± 18.5 | 0.04 |
| Gender | ||||
| Male | 53 | 157 | 67 | 0.2 |
| Female | 14 | 43 | 28 | |
| Fracture side | 0.4 | |||
| Unilateral | 50 | 40 | 70 | |
| Bilateral | 5 | 15 | 28 | |
| Cause of accident | 0.008 | |||
| Fall | 47 | 51 | 86 | |
| Road accident | 12 | 15 | 10 | |
| Other causes | 1 | 4 | 10 | |
| Sanders Classification | 0.3 | |||
| 2 | 1 | 10 | 19 | |
| 3 | 22 | 21 | 41 | |
| 4 | 37 | 39 | 66 | |
| Surgery time (minutes) | ||||
| (mean ± standard deviation) | 119.1 ± 39.3 | 51.3 ± 29.2 | n/a | p < 0.001 |
| Length of stay (days) | ||||
| (mean ± standard deviation) | 15.7 ± 12.8 | 10.5 ± 14.1 | 13.5 ± 19.5 | p < 0.001 |
| Böhler’s Angle | ORIF | MIT | CT | p |
|---|---|---|---|---|
| preoperative | ||||
| Sanders 2 | 26.6 ± 8.3 | 25.4 ± 5.6 | 30.8 ± 6.9 | 0.1 |
| Sanders 3 | 19.3 ± 7.1 | 23.3 ± 4.9 | 25.4 ± 8.7 | 0.1 |
| Sanders 4 | 20.8 ± 7.5 | 20.6 ± 6.0 | 23.9 ± 7.0 | 0.4 |
| postoperative | ||||
| Sanders 2 | 28.6 ± 7.1 | 29.4 ± 5.1 | n/a | 0.4 |
| Sanders 3 | 27.7 ± 4.9 | 29.8 ± 5.7 | n/a | p < 0.001 |
| Sanders 4 | 27.9 ± 5.0 | 28.6 ± 5.9 | n/a | p < 0.001 |
| follow-up | ||||
| Sanders 2 | 27.5 ± 4.5 | 28.3 ± 4.4 | 26.4 ± 7.8 | 0.5 |
| Sanders 3 | 26.5 ± 4.8 | 28.8 ± 5.9 | 20.9 ± 8.8 | p < 0.001 |
| Sanders 4 | 25.6 ± 4.9 | 26.2 ± 5.8 | 18.5 ± 10.9 | p < 0.001 |
| Gissane’s Angles | ORIF | MIT | CT | p |
|---|---|---|---|---|
| preoperative | ||||
| Sanders 2 | 111.7 ± 25.9 | 110.4 ± 12.3 | 100.4 ± 20.5 | 0.9 |
| Sanders 3 | 111.4 ± 11.5 | 111.6 ± 11.4 | 122.6 ± 10.5 | 0.8 |
| Sanders 4 | 107.9 ± 19.8 | 106.1 ± 15.7 | 109.4 ± 16.9 | 0.9 |
| postoperative | ||||
| Sanders 2 | 120.7 ±15.4 | 122.4 ± 9.5 | n/a | 0.5 |
| Sanders 3 | 113.7 ± 9.1 | 118.6 ± 6.5 | n/a | p < 0.001 |
| Sanders 4 | 118.6 ± 8.9 | 115.9 ± 11.3 | n/a | p < 0.001 |
| follow-up | ||||
| Sanders 2 | 119.9 ± 14.3 | 120.7 ± 7.8 | 98.5 ± 17.8 | 0.8 |
| Sanders 3 | 111.9 ± 18.1 | 116.8 ± 4.9 | 110.2 ± 11.2 | p < 0.001 |
| Sanders 4 | 116.0 ± 8.1 | 111.5 ± 11.9 | 104.8 ± 10.5 | p < 0.001 |
| Complications | ORIF | % | MIT | % | CT | % | p |
|---|---|---|---|---|---|---|---|
| n = 60 | n = 70 | n = 126 | |||||
| Wound healing disorders | 10 | 16.7 | 5 | 7.1 | 1 | 0.8 | 0.7 |
| Deep Infection | 7 | 11.7 | 2 | 2.9 | 1 | 0.8 | p < 0.001 |
| Revision | 3 | 5.0 | 1 | 1.4 | 0 | 1 | |
| Stiffness | 15 | 25.0 | 18 | 25.7 | 22 | 17.5 | 0.07 |
| Gait abnormality | 7 | 11.7 | 5 | 7.1 | 34 | 27.0 | 0.07 |
| Osteoarthritis Grade 3 | 5 | 8.3 | 3 | 4.3 | 37 | 29.4 | 0.09 |
| OR | 95% CI | p | ||
|---|---|---|---|---|
| Days until surgery | 1.033 | 0.969 | 1.101 | 0.32 |
| Surgery time | 0.86 | 0.472 | 1.579 | 0.63 |
| Sanders fracture | 1.391 | 1.259 | 1.536 | p < 0.001 |
| Surgical Therapy | 0.607 | 0.457 | 0.807 | p < 0.001 |
| Conservative Therapy | 0.513 | 0.535 | 0.787 | p < 0.001 |
| Score (Mean ± SD) | ORIF | MIT | CT | p |
|---|---|---|---|---|
| MFS | 72.2 ± 10.4 | 76.3 ± 9.8 | 55.4 ± 6.5 | p < 0.001 |
| AOFAS | 79.0 ± 10.6 | 81.7 ± 9.5 | 71.8 ± 13.2 | p = 0.04 |
| VAS | 3.6 ± 0.6 | 3.3 ± 0.9 | 4.3 ± 1.7 | p < 0.001 |
| PMS | 8.7 ± 0.5 | 8.4 ± 1.0 | 7.4 ± 1.7 | p = 0.004 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nia, A.; Hajdu, S.; Sarahrudi, K.; Widhalm, H.K.; Popp, D.; Schmoelz, L.; Doering, K.; Tiefenboeck, T. Surgical Treatment of Calcaneal Fractures by Minimally Invasive Technique Using a 2-Point Distractor Versus ORIF and Conservative Therapy—A Retrospective Multicenter Study. J. Clin. Med. 2025, 14, 2015. https://doi.org/10.3390/jcm14062015
Nia A, Hajdu S, Sarahrudi K, Widhalm HK, Popp D, Schmoelz L, Doering K, Tiefenboeck T. Surgical Treatment of Calcaneal Fractures by Minimally Invasive Technique Using a 2-Point Distractor Versus ORIF and Conservative Therapy—A Retrospective Multicenter Study. Journal of Clinical Medicine. 2025; 14(6):2015. https://doi.org/10.3390/jcm14062015
Chicago/Turabian StyleNia, Arastoo, Stefan Hajdu, Kambiz Sarahrudi, Harald Kurt Widhalm, Domenik Popp, Lukas Schmoelz, Kevin Doering, and Thomas Tiefenboeck. 2025. "Surgical Treatment of Calcaneal Fractures by Minimally Invasive Technique Using a 2-Point Distractor Versus ORIF and Conservative Therapy—A Retrospective Multicenter Study" Journal of Clinical Medicine 14, no. 6: 2015. https://doi.org/10.3390/jcm14062015
APA StyleNia, A., Hajdu, S., Sarahrudi, K., Widhalm, H. K., Popp, D., Schmoelz, L., Doering, K., & Tiefenboeck, T. (2025). Surgical Treatment of Calcaneal Fractures by Minimally Invasive Technique Using a 2-Point Distractor Versus ORIF and Conservative Therapy—A Retrospective Multicenter Study. Journal of Clinical Medicine, 14(6), 2015. https://doi.org/10.3390/jcm14062015







