Functional Mobility Studies in Younger Adults: Instrumented Timed Up and Go (iTUG) Test Using Inertial Devices
Abstract
1. Introduction
2. Materials and Methods
2.1. Setting and Ethical Considerations
2.2. Participants
2.3. Procedure
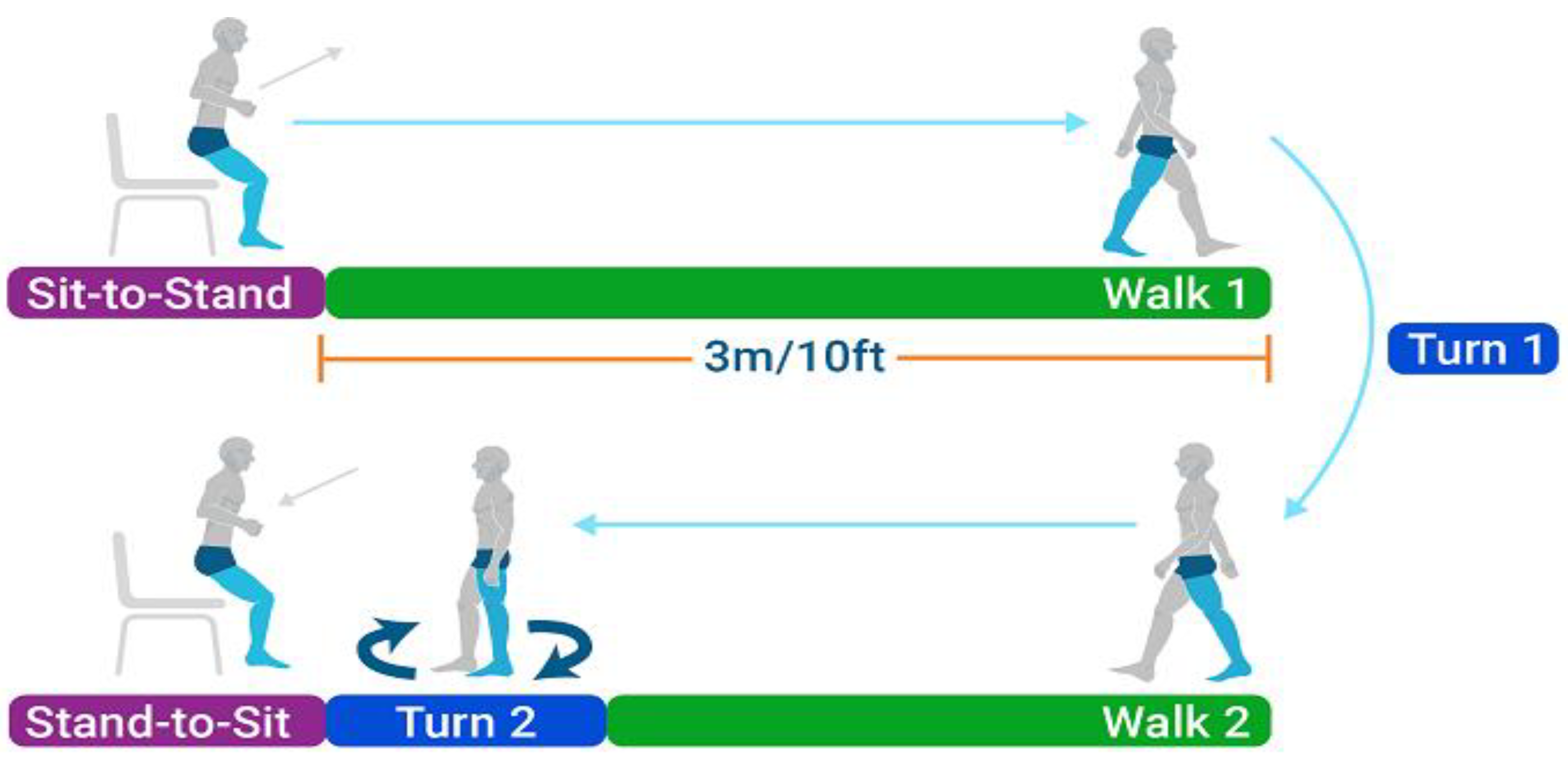
- Participants were seated in a standard chair with armrests, with their feet resting flat on the floor.
- They were instructed to stand up upon a verbal command (‘Go’), walk a distance of 3 m (measured and marked on the floor), turn around at the designated marker, and return to the chair to sit down.
- Measurements were taken one participant at a time to minimise distractions and ensure accurate motion capture.
- Participants performed the test at their self-selected normal walking speed. They were instructed not to run but to perform the task as quickly and safely as possible.
2.4. Data Analysis
2.5. Motion Analysis
2.6. Statistical Calculations
3. Results
3.1. iTUG Time Parameters
3.2. Parameters of Walk 1 and Walk 2 Phases
3.3. Turn 1 and Turn 2 Phase Parameters
3.4. Parameters of the Sitting Phase (Transition from Standing to Sitting)
4. Discussion
Study Limitation
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Low, D.; Walsh, G. The minimal important change for measures of balance and postural control in older adults: A systematic review. Age Ageing 2022, 51, afac284. [Google Scholar] [CrossRef] [PubMed]
- Ockerman, J.; Velghe, S.; Van Bladel, A.; Auvinet, E.; Saldien, J.; Klingels, K.; Bar-on, L.; Verbecque, E. Checks and balances: A meta-analysis on the known-groups validity of functional postural control tests in children. Eur. J. Phys. Rehabil. Med. 2024, 60, 656–670. [Google Scholar] [CrossRef] [PubMed]
- Long, J.; Cai, T.; Huang, X.; Zhou, Y.; Kuang, J.; Wu, L. Reference value for the TUGT in healthy older people: A systematic review and meta-analysis. Geriatr. Nurs. 2020, 41, 325–330. [Google Scholar] [CrossRef] [PubMed]
- Nordin, E.; Rosendahl, E.; Lundin-Olsson, L. Timed ”Up & Go” Test: Reliability in older people dependent in activities of daily living—Focus on cognitive state. Phys. Ther. 2006, 86, 646–655. [Google Scholar]
- Zahedian-Nasab, N.; Jaberi, A.; Shirazi, F.; Kavousipor, S. Effect of virtual reality exercises on balance and fall in elderly people with fall risk: A randomized controlled trial. BMC Geriatr. 2021, 21, 509. [Google Scholar] [CrossRef]
- Stanmore, E.; Mavroeidi, A.; de Jong, L.; Skelton, D.; Sutton, C.; Benedetto, V.; Munford, L.; Meekes, W.; Bell, V.; Todd, C. The effectiveness and cost-effectiveness of strength and balance Exergames to reduce falls risk for people aged 55 years and older in UK assisted living facilities: A multi-centre, cluster randomised controlled trial. BMC Med. 2019, 17, 49. [Google Scholar] [CrossRef]
- Junata, M.; Cheng, K.; Man, H.; Lai, C.; Soo, Y.; Tong, R. Kinect-based rapid movement training to improve balance recovery for stroke fall prevention: A randomized controlled trial. J. Neuroeng. Rehabil. 2021, 18, 150. [Google Scholar] [CrossRef]
- Shih, M.; Wang, R.; Cheng, S.; Yang, Y. Effects of a balance-based exergaming intervention using the Kinect sensor on posture stability in individuals with Parkinson’s disease: A single-blinded randomized controlled trial. J. Neuroeng. Rehabil. 2016, 13, 78. [Google Scholar] [CrossRef]
- Montano, V.; Lopriore, P.; Gruosso, F.; Carelli, V.; Comi, G.; Filosto, M.; Lamperti, C.; Mongini, T.; Musumeci, O.; Servidei, S.; et al. Primary mitochondrial myopathy: 12-month follow-up results of an Italian cohort. J. Neurol. 2022, 269, 6555–6565. [Google Scholar] [CrossRef]
- Fu, S.; Duan, T.; Hou, M.; Yang, F.; Chai, Y.; Chen, Y.; Liu, B.; Ma, Y.; Liu, A.; Wang, X.; et al. Postural Balance in Individuals With Knee Osteoarthritis During Stand-to-Sit Task. Front. Hum. Neurosci. 2021, 15, 760960. [Google Scholar] [CrossRef]
- Gaino, J.; Bértolo, M.; Nunes, C.; Barbosa, C.; Landim, S.; Sachetto, Z.; Magalhaes, E. The effect of foot orthoses on balance, foot function, and mobility in rheumatoid arthritis: A randomized controlled clinical trial. Clin. Rehabil. 2021, 35, 1011–1020. [Google Scholar] [CrossRef] [PubMed]
- Krolikowska, A.; Komar, N.; Oleksy, L.; Prill, R.; Janczak, D.; Reichert, P. A randomized, double-blind placebo control pilot trial on the effect of a blood flow restriction on the knee joint position sense in healthy recreational athletes. J. Clin. Med. 2023, 39, 217–218. [Google Scholar] [CrossRef]
- Samuelsson, K.; Egenvall, M.; Klarin, I.; Lökk, J.; Gunnarsson, U. Preoperative geriatric assessment and follow-up of patients older than 75 years undergoing elective surgery for suspected colorectal cancer. J. Geriatr. Oncol. 2019, 10, 709–715. [Google Scholar] [CrossRef] [PubMed]
- Mao, Q.; Zhang, J.; Yu, L.; Zhao, Y.; Luximon, Y.; Wang, H. Effectiveness of sensor-based interventions in improving gait and balance performance in older adults: Systematic review and meta-analysis of randomized controlled trials. J. Neuroeng. Rehabil. 2024, 21, 85. [Google Scholar] [CrossRef]
- Bao, T.; Carender, W.; Kinnaird, C.; Barone, V.; Peethambaran, G.; Whitney, S.; Kabeto, M.; Seidler, R.; Sienko, K. Effects of long-term balance training with vibrotactile sensory augmentation among community-dwelling healthy older adults: A randomized preliminary study. J. Neuroeng. Rehabil. 2018, 15, 5. [Google Scholar] [CrossRef]
- Yoon, S.; Son, H. Effects of Full Immersion Virtual Reality Training on Balance and Knee Function in Total Knee Replacement Patients: A Randomized Controlled Study. J. Mech. Med. Biol. 2020, 20, 697–709. [Google Scholar] [CrossRef]
- Hagedorn, D.; Holm, E. Effects of traditional physical training and visual computer feedback training in frail elderly patients: A randomized intervention study. Eur. J. Phys. Rehabil. Med. 2010, 46, 159–168. [Google Scholar]
- Gschwind, Y.; Schoene, D.; Lord, S.; Ejupi, A.; Valenzuela, T.; Aal, K.; Woodbury, A.; Delbaere, K. The effect of sensor-based exercise at home on functional performance associated with fall risk in older people—A comparison of two exergame interventions. Eur. Rev. Aging Phys. Act. 2015, 12, 11. [Google Scholar] [CrossRef]
- Schwenk, M.; Grewal, G.; Honarvar, B.; Schwenk, S.; Mohler, J.; Khalsa, D.; Najafi, B. Interactive balance training integrating sensor-based visual feedback of movement performance: A pilot study in older adults. J. Neuroeng. Rehabil. 2014, 11, 164. [Google Scholar] [CrossRef]
- Capodaglio, P.; Capodaglio, E.; Ferri, A.; Scaglioni, G.; Marchi, A.; Saibene, F. Muscle function and functional ability improves more in community-dwelling older women with a mixed-strength training programme. Age Ageing 2005, 34, 141–147. [Google Scholar] [CrossRef][Green Version]
- Sadeghi, H.; Jehu, D.; Daneshjoo, A.; Shakoor, E.; Razeghi, M.; Amani, A.; Hakim, M.; Yusof, A. Effects of 8 Weeks of Balance Training, Virtual Reality Training, and Combined Exercise on Lower Limb Muscle Strength, Balance, and Functional Mobility Among Older Men: A Randomized Controlled Trial. Sports Health: A Multidiscip. Approach 2021, 13, 606–612. [Google Scholar] [CrossRef] [PubMed]
- Htut, T.; Hiengkaew, V.; Jalayondeja, C.; Vongsirinavarat, M. Effects of physical, virtual reality-based, and brain exercise on physical, cognition, and preference in older persons: A randomized controlled trial. Eur. Rev. Aging Phys. Act. 2018, 15, 10. [Google Scholar] [CrossRef] [PubMed]
- Chow, D.; Mann, S. Effect of Cyber-Golfing on Balance Amongst the Elderly in Hong Kong: A Pilot Randomised Trial. Hong Kong J. Occup. Ther. 2015, 26, 9–13. [Google Scholar] [CrossRef]
- Kobsar, D.; Charlton, J.; Tse, C.; Esculier, J.; Graffos, A.; Krowchuk, N.; Thatcher, D.; Hunt, M. Validity and reliability of wearable inertial sensors in healthy adult walking: A systematic review and meta-analysis. J. Neuroeng. Rehabil. 2020, 17, 62. [Google Scholar] [CrossRef]
- Ortega-Bastidas, P.; Gómez, B.; Aqueveque, P.; Luarte-Martínez, S.; Cano-de-la-Cuerda, R. Instrumented Timed Up and Go Test (iTUG)-More Than Assessing Time to Predict Falls: A Systematic Review. Sensors 2023, 23, 3426. [Google Scholar] [CrossRef]
- Nguyen, H.; Ayachi, F.; Lavigne-Pelletier, C.; Blamoutier, M.; Rahimi, F.; Boissy, P.; Jog, M.; Duval, C. Auto detection and segmentation of physical activities during a Timed-Up-and-Go (TUG) task in healthy older adults using multiple inertial sensors. J. Neuroeng. Rehabil. 2015, 12, 36. [Google Scholar] [CrossRef]
- Spina, S.; Facciorusso, S.; D’ascanio, M.; Morone, G.; Baricich, A.; Fiore, P.; Santamato, A. Sensor based assessment of turning during instrumented Timed Up and Go Test for quantifying mobility in chronic stroke patients. Eur. J. Phys. Rehabil. Med. 2023, 59, 6–13. [Google Scholar] [CrossRef]
- van Lummel, R.; Walgaard, S.; Hobert, M.; Maetzler, W.; van Dieën, J.; Galindo-Garre, F.; Terwee, C. Intra-Rater, Inter-Rater and Test-Retest Reliability of an Instrumented Timed Up and Go (iTUG) Test in Patients with Parkinson’s Disease. PLoS ONE 2016, 11, e0151881. [Google Scholar] [CrossRef]
- Valle, M.; Casabona, A.; Sapienza, I.; Laudani, L.; Vagnini, A.; Lanza, S.; Cioni, M. Use of a Single Wearable Sensor to Evaluate the Effects of Gait and Pelvis Asymmetries on the Components of the Timed Up and Go Test, in Persons with Unilateral Lower Limb Amputation. Sensors 2022, 22, 95. [Google Scholar] [CrossRef]
- Van Uem, J.; Walgaard, S.; Ainsworth, E.; Hasmann, S.; Heger, T.; Nussbaum, S.; Hobert, M.; Micó-Amigo, E.; Van Lummel, R.; Berg, D.; et al. Quantitative Timed-Up-and-Go Parameters in Relation to Cognitive Parameters and Health-Related Quality of Life in Mild-to-Moderate Parkinson’s Disease. PLoS ONE 2016, 11, e0151997. [Google Scholar] [CrossRef]
- Zarzeczny, R.; Nawrat-Szoltysik, A.; Polak, A.; Maliszewski, J.; Kieltyka, A.; Matyja, B.; Dudek, M.; Zborowska, J.; Wajdman, A. Aging effect on the instrumented Timed-Up-and-Go test variables in nursing home women aged 80–93 years. Biogerontology 2017, 18, 651–663. [Google Scholar] [CrossRef] [PubMed]
- Gasparutto, X.; Gueugnon, M.; Laroche, D.; Martz, P.; Hannouche, D.; Armand, S. Which functional tasks present the largest deficits for patients with total hip arthroplasty before and six months after surgery? A study of the timed up-and-go test phases. PLoS ONE 2021, 16, e0255037. [Google Scholar] [CrossRef] [PubMed]
- Hassani, A.; Kubicki, A.; Brost, V.; Mourey, F.; Yang, F. Kinematic analysis of motor strategies in frail aged adults during the Timed Up and Go: How to spot the motor frailty? Clin. Interv. Aging 2015, 10, 505–513. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Królikowska, A.; Reichert, P.; Karlsson, J.; Mouton, C.; Becker, R.; Prill, R. Improving the reliability of measurements in orthopaedics and sports medicine. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 5277–5285. [Google Scholar] [CrossRef]
- Prill, R.; Walter, M.; Królikowska, A.; Becker, R. A Systematic Review of Diagnostic Accuracy and Clinical Applications of Wearable Movement Sensors for Knee Joint Rehabilitation. Sensors 2021, 21, 8221. [Google Scholar] [CrossRef]

| Region | Inertial Unit Positions |
|---|---|
| Sternum | At the level of the sternum or breastbone |
| Mid-spine | At the mid-point of the spine, around the level of the thoracic vertebrae |
| Lower spine | At the lumbar region of the spine |
| Left and Right shoulder | On each shoulder on the acromion—the bony prominence at the top of the shoulder |
| Left/Right upper arm | On the lateral side of each upper arm, midway between the shoulder and the elbow |
| Left/Right forearm | On the lateral side of each forearm, typically halfway between the elbow and the wrist |
| Left/Right hand | On the dorsum (back) of each hand, near the wrist |
| Left/Right thigh | On each thigh, midway between the hip and knee, on the lateral side |
| Left/Right shank | On the lateral side of each shank, midway between the knee and the ankle |
| Parameter | Unit | Definition | Interpretation and Clinical Significance |
|---|---|---|---|
| Stand Phase (transition from sitting to standing) | |||
| Stand Duration | s | Time taken to transition from sitting to standing | Duration indicates the efficiency and control in transitioning to a standing position |
| Stand Flexion Duration | s | Duration of trunk flexion during the stand | Longer durations may indicate difficulty in initiating or maintaining flexion |
| Stand Extension Duration | s | Duration of trunk extension during the stand | Duration reflects control over trunk extension during standing |
| Trunk Flexion ROM | deg | Range of motion of the trunk in flexion | Greater ROM indicates greater flexibility and mobility |
| Trunk Lateral ROM | deg | Lateral range of motion of the trunk | Greater lateral ROM may reflect trunk stability |
| Trunk Rotation ROM | deg | Rotational range of motion of the trunk | Greater rotational ROM may reflect rotational mobility |
| Trunk Flexion Speed Avg | deg/s | Average speed of trunk flexion | Higher speeds suggest greater control and dynamics of trunk flexion |
| Trunk Flexion Speed Max | deg/s | Maximum speed of trunk flexion | Higher peak speed reflects better control and strength in trunk flexion |
| Trunk Extension Speed Avg | deg/s | Average speed of trunk extension | Higher speeds suggest greater control and dynamics of trunk extension |
| Trunk Extension Speed Max | deg/s | Maximum speed of trunk extension | Higher peak speed reflects better control and strength in trunk extension |
| Walk 1 and Walk 2 Phases | |||
| Walk Duration | s | Time taken to walk the 3-metre distance | A shorter duration indicates faster and potentially more efficient walking |
| Walk Cadence | steps/min | Number of steps per minute | Higher cadence reflects a faster pace |
| Walk Step Count | steps | Total number of steps taken | A lower step count may indicate efficient gait with adequate stride length, stability, and confidence in walking ability |
| Walk Stride Time | s | Time taken for one complete gait cycle | Shorter stride times indicate quicker gait cycles |
| Walk Stance | % | Percentage of the gait cycle spent in stance phase, recorded separately for left and right legs | Reduced stance phase percentage can reflect a quicker gait or increased confidence in single-leg support |
| Walk Swing | % | Percentage of the gait cycle spent in swing phase, recorded separately for left and right legs | Higher swing phase percentage may indicate a faster gait with shorter stance duration |
| Walk Single Support | % | Percentage of the gait cycle spent on single-leg support, recorded separately for left and right legs | Higher percentage reflects balance in single-leg stance |
| Walk 1st Double Support | % | Percentage of the gait cycle spent on double-leg support | Higher double support indicates stability during the weight acceptance phase |
| Walk Foot Pitch at Contact | deg | Angle of the foot at initial ground contact, recorded separately for left and right feet | Foot angle reflects gait and balance during contact |
| Walk Stance Ratio | % | Ratio of stance times between the right and left legs | Closer to 100% indicates equal stance times; a measure of asymmetry |
| Walk Double Support Ratio | % | The ratio of double support times between the right and left legs | Closer to 100% indicates equal double support time, a measure of asymmetry |
| Walk Foot Pitch at Foot Off | deg | Angle of the foot at the moment it leaves the ground, recorded separately for left and right feet | Reflects foot dynamics at foot-off or efficiency of push-off |
| Walk Foot Pitch Speed Max | deg/s | Maximum speed of foot pitch during walking, recorded separately for left and right feet | Higher values indicate greater control in foot movement |
| Turn 1 and Turn 2 Phases | |||
| Turn 1 Duration | s | Time taken to complete the first turn | A shorter time indicates efficient turning |
| Turn 1 Step Count | steps | Number of steps taken during the first turn | A higher count indicates more steps needed for turning |
| Turn 1 Stride Time | s | Time taken for one stride during the turn | Shorter stride time indicates quicker movement |
| Turn 1 Stance | % | Percentage of the turn spent in stance phase, recorded separately for left and right legs | A higher stance percentage suggests stability during the turn |
| Turn 1 Swing | % | Percentage of the turn spent in swing phase, recorded separately for left and right legs | A higher swing percentage indicates a more dynamic turn |
| Turn 1 Single Support | % | Percentage of the turn spent on single-leg support, recorded separately for left and right legs | A higher support percentage indicates balance on one leg |
| Turn 1 1st Double Support | % | Percentage of the turn spent on double-leg support | Higher values indicate balanced turning support |
| Turn 1 Trunk Rotation Speed Max | deg/s | Maximum speed of trunk rotation during the first turn | Higher values suggest rapid trunk rotation control |
| Turn 2 Duration | s | Time taken to complete the second turn | A shorter duration indicates an efficient final turn |
| Turn 2 Trunk Rotation Speed Max | deg/s | Maximum speed of trunk rotation during the second turn | Higher speed suggests agility in trunk rotation |
| Sit Phase (transition from standing to sitting) | |||
| Sit Duration | s | Time taken to transition from standing to sitting | A shorter time suggests control and efficiency in sitting |
| Sit Trunk Flexion Duration | s | Duration of trunk flexion during the sit | Longer flexion duration may indicate difficulty or cautious movement |
| Sit Trunk Extension Duration | s | Duration of trunk extension during the sit | Reflects control during trunk extension in sitting |
| Sit Trunk Flexion ROM | deg | Range of motion of the trunk in flexion during the sit | Greater ROM indicates flexibility and mobility |
| Sit Trunk Lateral ROM | deg | Lateral range of motion of the trunk during the sit | Higher lateral ROM may reflect trunk stability |
| Sit Trunk Rotation ROM | deg | Rotational range of motion of the trunk during the sit | Reflects rotational mobility |
| Sit Trunk Flexion Speed Avg | deg/s | Average speed of trunk flexion during the sit | Higher speeds suggest better trunk control |
| Sit Trunk Flexion Speed Max | deg/s | Maximum speed of trunk flexion during the sit | Higher peak speed reflects agility in trunk flexion |
| Sit Trunk Extension Speed Avg | deg/s | Average speed of trunk extension during the sit | Higher speeds suggest controlled extension |
| Sit Trunk Extension Speed Max | deg/s | Maximum speed of trunk extension during the sit | Higher peak speed reflects controlled trunk extension during sitting |
| Variable | Mean | Median | SD | Minimum | Maximum | Lower Quartile | Upper Quartile | Quartile Range | Coef.Var. |
|---|---|---|---|---|---|---|---|---|---|
| Total time [s] | 13.1 | 12.7 | 1.9 | 9.9 | 17.7 | 11.6 | 14.6 | 3.0 | 14.8 |
| Stand phase [s] | 1.1 | 1.1 | 0.3 | 0.6 | 2.9 | 0.9 | 1.2 | 0.3 | 29.2 |
| Walk 1 phase [s] | 4.1 | 4.2 | 0.9 | 2.4 | 6.7 | 3.4 | 4.7 | 1.4 | 22.4 |
| Turn 1 phase [s] | 2.0 | 2.0 | 0.4 | 1.0 | 3.1 | 1.7 | 2.2 | 0.6 | 19.5 |
| Walk 2 phase [s] | 3.2 | 3.1 | 0.7 | 1.7 | 5.0 | 2.7 | 3.7 | 1.0 | 20.5 |
| Turn 2 phase [s] | 1.1 | 1.1 | 0.3 | 0.7 | 2.2 | 0.9 | 1.3 | 0.4 | 24.1 |
| Sit phase [s] | 1.6 | 1.5 | 0.4 | 0.9 | 2.7 | 1.3 | 1.8 | 0.5 | 23.2 |
| Stand Duration [s] | 1.1 | 1.1 | 0.3 | 0.6 | 2.9 | 0.9 | 1.2 | 0.3 | 29.2 |
| Stand Flex. Duration [s] | 0.6 | 0.6 | 0.2 | 0.2 | 1.7 | 0.5 | 0.7 | 0.2 | 31.3 |
| Stand Ext. Duration [s] | 0.5 | 0.4 | 0.2 | 0.2 | 1.2 | 0.4 | 0.6 | 0.2 | 39.1 |
| Variable | Mean | Median | SD | Minimum | Maximum | Lower Quartile | Upper Quartile | Quartile Range | Coef.Var. |
|---|---|---|---|---|---|---|---|---|---|
| Walk Duration [s] | 7.3 | 7.3 | 1.4 | 4.8 | 10.6 | 6.0 | 8.5 | 2.5 | 19.8 |
| Walk Cadence [steps/min] | 107.6 | 108.1 | 8.3 | 91.3 | 122.4 | 101.3 | 113.9 | 12.5 | 7.7 |
| Walk Step Count [steps] | 11.3 | 11.0 | 2.3 | 8.0 | 16.0 | 10.0 | 13.0 | 3.0 | 20.2 |
| Walk Stride Time [s] | 1.1 | 1.1 | 0.1 | 1.0 | 1.3 | 1.0 | 1.2 | 0.1 | 7.7 |
| Walk Stance left [%] | 60.3 | 60.4 | 2.0 | 55.3 | 64.9 | 58.9 | 61.9 | 3.0 | 3.3 |
| Walk Stance right [%] | 59.6 | 59.6 | 2.3 | 52.2 | 63.6 | 58.1 | 61.2 | 3.1 | 3.9 |
| Walk Swing left [%] | 39.7 | 39.6 | 2.0 | 35.1 | 44.7 | 38.1 | 41.1 | 3.0 | 5.0 |
| Walk Swing right [%] | 40.5 | 40.4 | 2.3 | 36.4 | 47.8 | 38.8 | 41.9 | 3.1 | 5.7 |
| Walk Single Support left [%] | 39.1 | 40.7 | 8.6 | 0.0 | 48.0 | 38.4 | 42.7 | 4.3 | 22.1 |
| Walk Single Support right [%] | 39.3 | 39.2 | 3.0 | 27.5 | 45.8 | 38.0 | 41.1 | 3.1 | 7.6 |
| Walk 1st Double Support left [%] | 9.7 | 9.5 | 2.0 | 4.8 | 14.2 | 8.7 | 11.0 | 2.4 | 20.3 |
| Walk 1st Double Support right [%] | 10.6 | 10.5 | 2.4 | 5.7 | 19.5 | 9.0 | 12.0 | 3.0 | 22.8 |
| Walk Stance Ratio (R − L)/(R + L) [%] | −0.7 | −0.5 | 2.1 | −10.9 | 3.1 | −1.7 | 0.6 | 2.3 | −313.0 |
| Walk Double Support Ratio (R − L)/(R + L) [%] | 4.1 | 3.3 | 11.0 | −23.6 | 46.8 | −2.5 | 9.6 | 12.1 | 271.5 |
| Walk Foot Pitch At Contact left [deg] | −19.1 | −17.3 | 5.3 | −35.6 | −11.2 | −21.4 | −15.2 | 6.3 | −28.0 |
| Walk Foot Pitch At Contact right [deg] | −17.8 | −18.1 | 4.3 | −26.8 | −10.5 | −21.1 | −14.2 | 6.9 | −24.3 |
| Walk Foot Pitch At Foot Off left [deg] | 56.6 | 56.7 | 8.0 | 34.6 | 71.7 | 51.6 | 62.7 | 11.1 | 14.1 |
| Walk Foot Pitch At Foot Off right [deg] | 55.4 | 55.2 | 7.5 | 35.8 | 73.3 | 50.6 | 59.2 | 8.6 | 13.6 |
| Walk Foot Pitch Speed Max left [deg] | 40.2 | 39.6 | 6.4 | 22.8 | 52.0 | 35.9 | 45.7 | 9.8 | 15.8 |
| Walk Foot Pitch Speed Max right [deg] | 40.6 | 40.5 | 5.3 | 29.5 | 50.6 | 36.8 | 44.7 | 7.9 | 13.1 |
| Variable | Mean | Median | SD | Minimum | Maximum | Lower Quartile | Upper Quartile | Quartile Range | Coef.Var. |
|---|---|---|---|---|---|---|---|---|---|
| Turn 1 Duration [s] | 2.0 | 2.0 | 0.4 | 1.0 | 3.1 | 1.7 | 2.2 | 0.6 | 19.5 |
| Turn 1 Step Count [steps] | 1.9 | 2.0 | 0.9 | 0.0 | 5.0 | 1.0 | 2.0 | 1.0 | 45.2 |
| Turn 1 Stride Time [s] | 1.2 | 1.2 | 0.1 | 0.7 | 1.4 | 1.1 | 1.3 | 0.2 | 11.4 |
| Turn 1 Stance left [%] | 59.1 | 59.1 | 5.0 | 47.5 | 68.6 | 56.0 | 62.4 | 6.4 | 8.4 |
| Turn 1 Stance right [%] | 58.8 | 58.3 | 4.2 | 50.5 | 67.9 | 55.8 | 61.7 | 5.9 | 7.1 |
| Turn 1 Swing left [%] | 40.9 | 40.9 | 5.0 | 31.4 | 52.5 | 37.6 | 44.0 | 6.4 | 12.2 |
| Turn 1 Swing right [%] | 41.2 | 41.7 | 4.2 | 32.1 | 49.5 | 38.3 | 44.2 | 5.9 | 10.2 |
| Turn 1 Single Support left [%] | 36.7 | 37.9 | 7.4 | 0.0 | 44.9 | 34.0 | 40.5 | 6.6 | 20.2 |
| Turn 1 Single Support right [%] | 37.5 | 37.3 | 3.7 | 31.3 | 46.9 | 34.9 | 39.5 | 4.5 | 9.8 |
| Turn 1 1st Double Support left [%] | 11.5 | 11.2 | 4.9 | 4.5 | 36.0 | 9.4 | 12.3 | 2.9 | 42.9 |
| Turn 1 1st Double Support right [%] | 10.9 | 11.0 | 2.9 | 5.1 | 15.5 | 8.5 | 13.4 | 4.9 | 26.9 |
| Turn 1 Trunk Rotation Speed Max [deg/s] | 67.0 | 66.0 | 22.8 | 31.9 | 144.7 | 50.4 | 77.3 | 26.9 | 34.0 |
| Turn 2 Duration [s] | 1.1 | 1.1 | 0.3 | 0.7 | 2.2 | 0.9 | 1.3 | 0.4 | 24.1 |
| Turn 2 Trunk Rotation Speed Max [deg/s] | 67.0 | 66.0 | 22.8 | 31.9 | 144.7 | 50.4 | 77.3 | 26.9 | 34.0 |
| Variable | Mean | Median | SD | Minimum | Maximum | Lower Quartile | Upper Quartile | Quartile Range | Coef.Var. |
|---|---|---|---|---|---|---|---|---|---|
| Sit Duration [s] | 1.6 | 1.5 | 0.4 | 0.9 | 2.7 | 1.3 | 1.8 | 0.5 | 23.2 |
| Sit Trunk Flex. Duration [s] | 0.6 | 0.6 | 0.2 | 0.2 | 1.2 | 0.4 | 0.7 | 0.3 | 40.0 |
| Sit Trunk Ext. Duration [s] | 1.0 | 1.0 | 0.2 | 0.5 | 1.6 | 0.9 | 1.1 | 0.2 | 21.0 |
| Sit Trunk Flex. ROM [deg] | 51.7 | 48.5 | 20.1 | 20.9 | 132.5 | 37.1 | 64.2 | 27.1 | 38.9 |
| Sit Trunk Lat. ROM [deg] | 45.9 | 43.2 | 20.9 | 15.1 | 113.6 | 29.8 | 55.4 | 25.6 | 45.6 |
| Sit Trunk Rot. ROM [deg] | 163.5 | 151.2 | 70.4 | 30.5 | 359.7 | 118.3 | 183.4 | 65.2 | 43.1 |
| Sit Trunk Flex. Speed Avg [deg/s] | 36.3 | 41.6 | 44.3 | −71.4 | 151.0 | 16.8 | 65.1 | 48.3 | 122.1 |
| Sit Trunk Flex. Speed Max [deg/s] | 152.7 | 111.2 | 160.1 | −27.6 | 1101.6 | 79.2 | 166.9 | 87.7 | 104.9 |
| Sit Trunk Ext. Speed Avg [deg/s] | 8.5 | 19.3 | 31.7 | −58.7 | 54.0 | −13.0 | 33.6 | 46.6 | 373.6 |
| Sit Trunk Ext. Speed Max [deg/s] | 92.9 | 66.1 | 175.9 | 10.2 | 1520.0 | 53.4 | 81.2 | 27.8 | 189.4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kowal, M.; Winiarski, S.; Morgiel, E.; Madej, M.; Proc, K.; Madziarski, M.; Wedel, N.; Sebastian, A. Functional Mobility Studies in Younger Adults: Instrumented Timed Up and Go (iTUG) Test Using Inertial Devices. J. Clin. Med. 2025, 14, 1944. https://doi.org/10.3390/jcm14061944
Kowal M, Winiarski S, Morgiel E, Madej M, Proc K, Madziarski M, Wedel N, Sebastian A. Functional Mobility Studies in Younger Adults: Instrumented Timed Up and Go (iTUG) Test Using Inertial Devices. Journal of Clinical Medicine. 2025; 14(6):1944. https://doi.org/10.3390/jcm14061944
Chicago/Turabian StyleKowal, Mateusz, Sławomir Winiarski, Ewa Morgiel, Marta Madej, Krzysztof Proc, Marcin Madziarski, Nicole Wedel, and Agata Sebastian. 2025. "Functional Mobility Studies in Younger Adults: Instrumented Timed Up and Go (iTUG) Test Using Inertial Devices" Journal of Clinical Medicine 14, no. 6: 1944. https://doi.org/10.3390/jcm14061944
APA StyleKowal, M., Winiarski, S., Morgiel, E., Madej, M., Proc, K., Madziarski, M., Wedel, N., & Sebastian, A. (2025). Functional Mobility Studies in Younger Adults: Instrumented Timed Up and Go (iTUG) Test Using Inertial Devices. Journal of Clinical Medicine, 14(6), 1944. https://doi.org/10.3390/jcm14061944







