Prognostic Markers of Adverse Outcomes in Acute Heart Failure: Use of Machine Learning and Network Analysis with Real Clinical Data
Abstract
1. Introduction
2. Materials and Methods
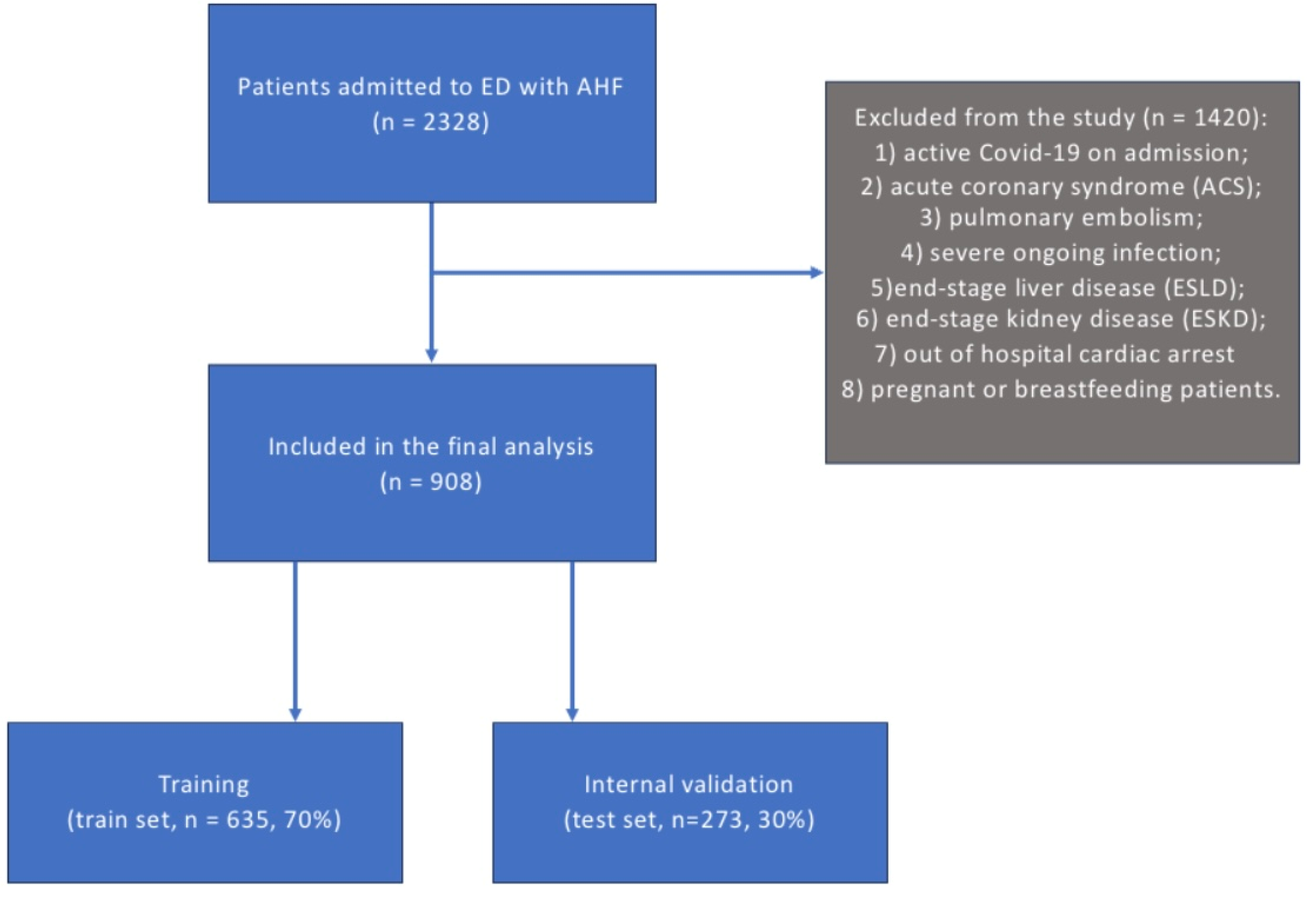
2.1. Study Cohort and Sample
2.2. Outcomes and Variable Definitions
2.3. Statistical Analysis
3. Results
3.1. Cohort Characteristics
3.2. Risk of In-Hospital Outcomes According to Model Predictions
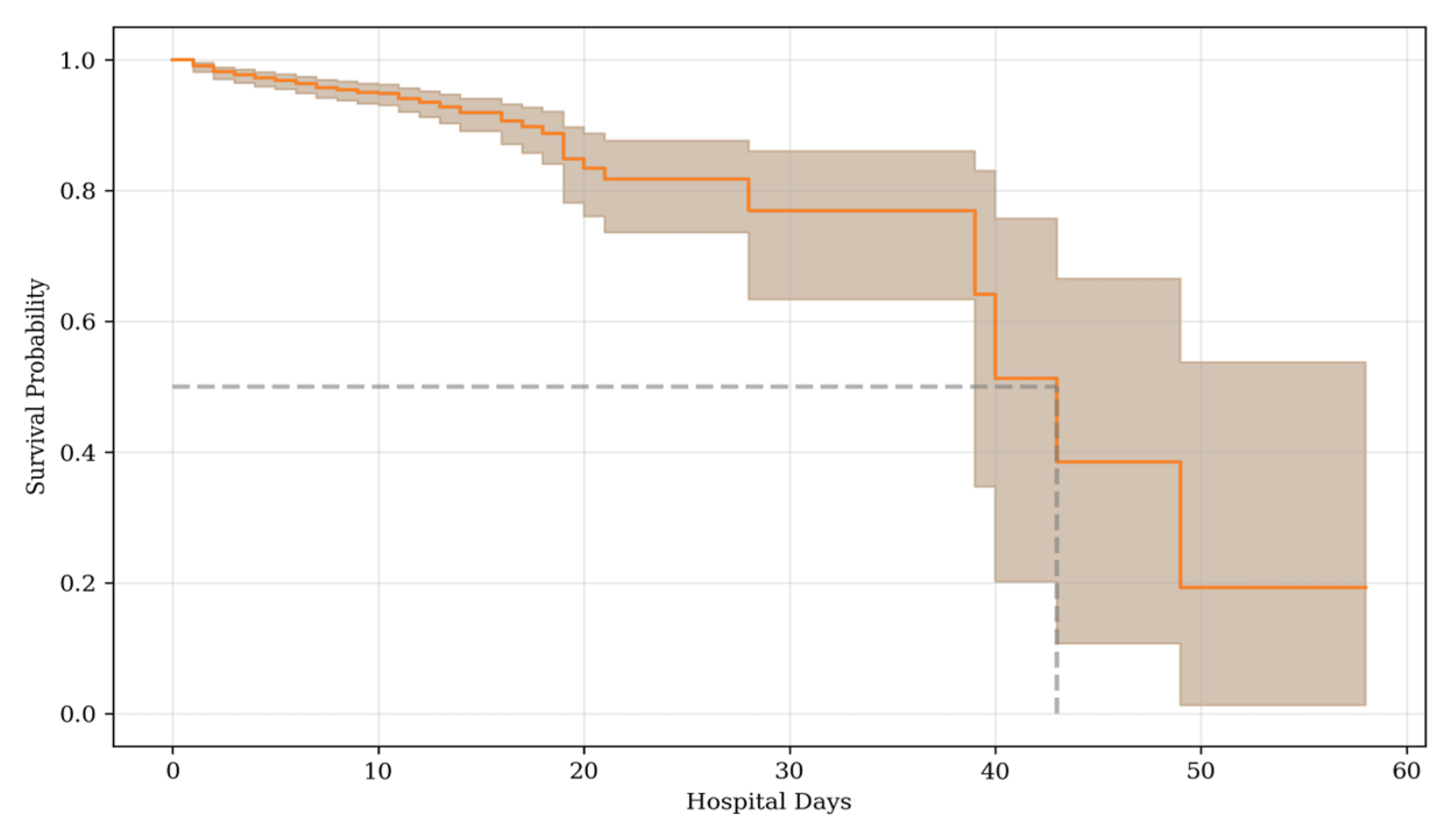
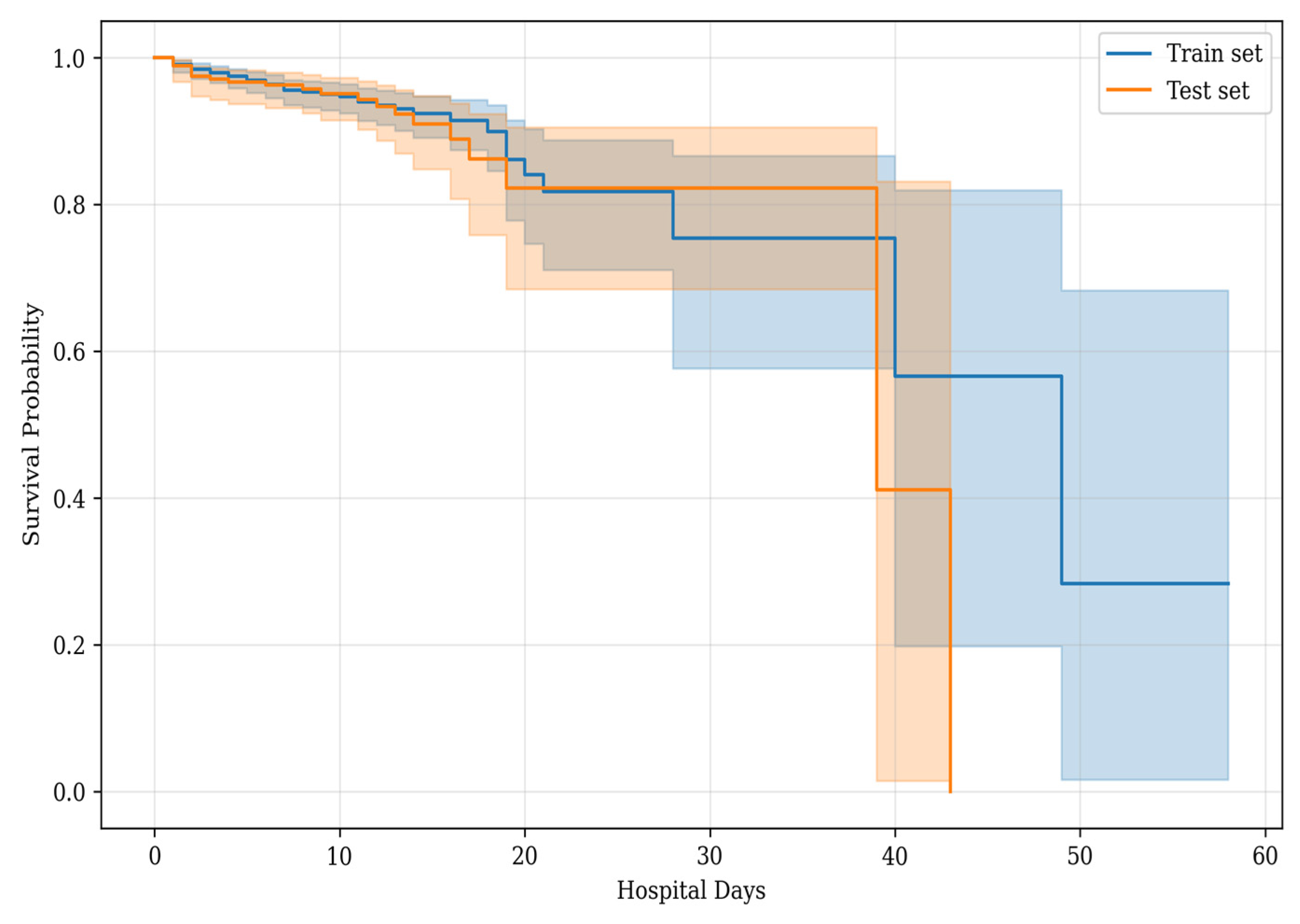
3.2.1. Main Outcome
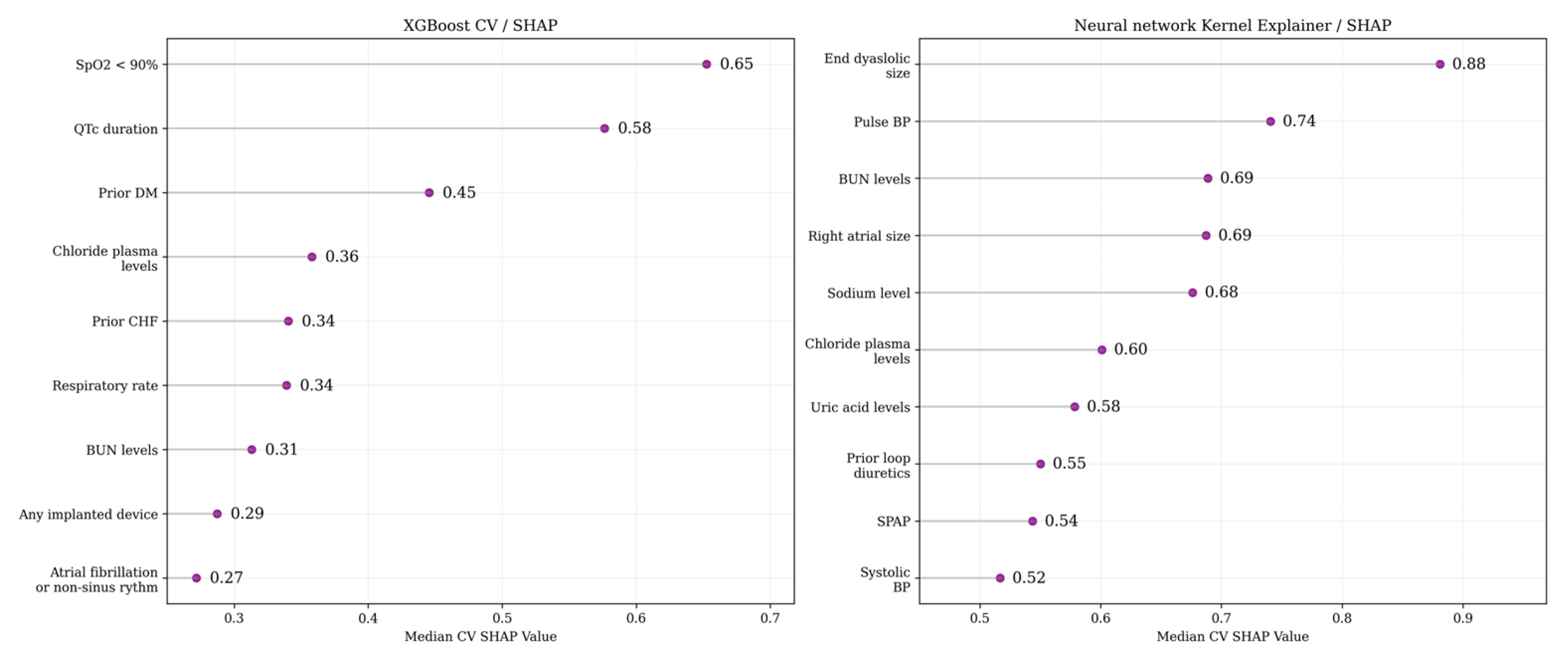
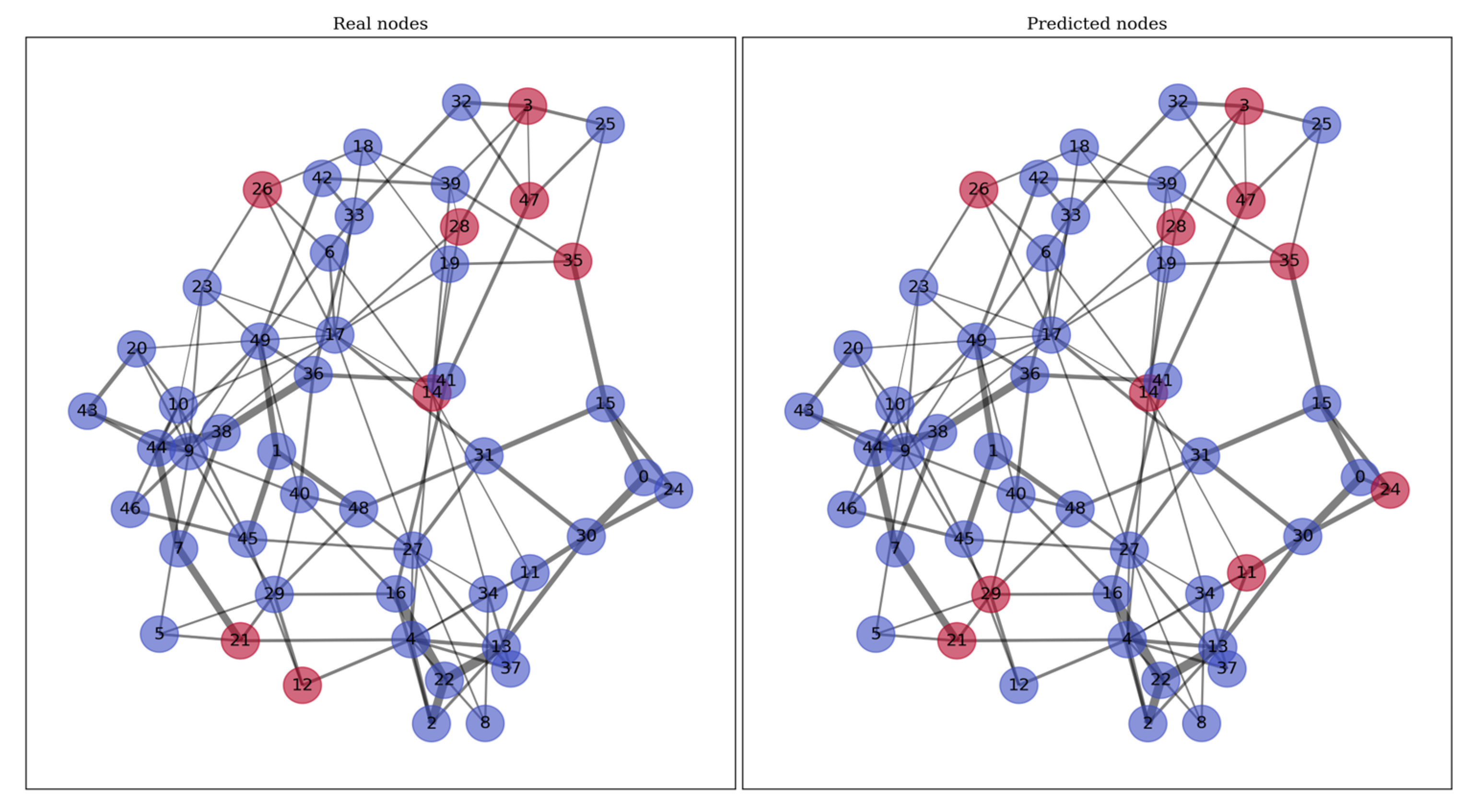
3.2.2. Feature Selection and Modeling Results
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chioncel, O.; Mebazaa, A.; Harjola, V.P.; Coats, A.J.; Piepoli, M.F.; Crespo-Leiro, M.G.; Laroche, C.; Seferovic, P.M.; Anker, S.D.; Ferrari, R.; et al. Clinical phenotypes and outcome of patients hospitalized for acute heart failure: The 8 Heart Failure Long-Term Registry. Eur. J. Heart Fail. 2017, 19, 1242–1254. [Google Scholar] [CrossRef] [PubMed]
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M.; Burri, H.; Butler, J.; Čelutkienė, J.; Chioncel, O.; et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 2021, 42, 3599–3726, Erratum in: Eur. Heart J. 2021, 42, 4901. [Google Scholar] [CrossRef]
- van Diepen, S.; Bakal, J.A.; Lin, M.; Kaul, P.; McAlister, F.A.; Ezekowitz, J.A. Variation in critical care unit admission rates and outcomes for patients with acute coronary syndromes or heart failure among high- and low-volume cardiac hospitals. J. Am. Heart Assoc. 2015, 4, e001708. [Google Scholar] [CrossRef]
- Wunsch, H.; Angus, D.C.; Harrison, D.A.; Collange, O.; Fowler, R.; Hoste, E.A.J.; de Keizer, N.F.; Kersten, A.; Linde-Zwirble, W.T.; Sandiumenge, A.; et al. Variation in critical care services across North America and Western Europe. Crit. Care Med. 2008, 36, 2787.e8. [Google Scholar] [CrossRef] [PubMed]
- Shiraishi, Y.; Kohsaka, S.; Abe, T.; Nagai, T.; Goda, A.; Nishihata, Y.; Nagatomo, Y.; Saji, M.; Toyosaki, Y.; Takei, M.; et al. Derivation and validation of clinical prediction models for rapid risk stratification for time-sensitive management for acute heart failure. J. Clin. Med. 2020, 9, 3394. [Google Scholar] [CrossRef]
- Sepehrvand, N.; Youngson, E.; Bakal, J.A.; McAlister, F.A.; Rowe, B.H.; Ezekowitz, J.A. External Validation and Refinement of Emergency Heart Failure Mortality Risk Grade Risk Model in Patients With Heart Failure in the Emergency Department. CJC Open 2019, 1, 123–130. [Google Scholar] [CrossRef]
- Peterson, P.N.; Rumsfeld, J.S.; Liang, L.; Albert, N.M.; Hernandez, A.F.; Peterson, E.D.; Fonarow, G.C.; Masoudi, F.A. A validated risk score for in-hospital mortality in patients with heart failure from the American Heart Association get with the guidelines program. Circ. Cardiovasc. Qual. Outcomes 2010, 3, 25–32. [Google Scholar] [CrossRef] [PubMed]
- Auble, T.E.; Hsieh, M.; Gardner, W.; Cooper, G.F.; Stone, R.A.; McCausland, J.B.; Yealy, D.M. A prediction rule to identify low-risk patients with heart failure. Acad. Emerg. Med. 2005, 12, 514–521. [Google Scholar] [CrossRef] [PubMed]
- Royston, P.; Altman, D.G. Risk stratification for in-hospital mortality in acutely decompensated heart failure. JAMA 2005, 293, 2467–2468. [Google Scholar] [CrossRef]
- Chaddad, A.; Peng, J.; Xu, J.; Bouridane, A. Survey of Explainable AI Techniques in Healthcare. Sensors 2023, 5, 634. [Google Scholar] [CrossRef]
- McCallum, W.; Sarnak, M.J. Cardiorenal Syndrome in the Hospital. Clin. J. Am. Soc. Nephrol. 2023, 18, 933–945. [Google Scholar] [CrossRef]
- Wussler, D.; Michou, E.; Belkin, M.; Kozhuharov, N.; Diebold, M.; Gualandro, D.M.; Breidthardt, T.; Mueller, C. Mortality prediction in acute heart failure: Scores or biomarkers? Swiss. Med. Wkly. 2020, 150, w20320. [Google Scholar] [CrossRef] [PubMed]
- Miró, Ò.; Rossello, X.; Gil, V.; Martín-Sánchez, F.J.; Llorens, P.; Herrero-Puente, P.; Jacob, J.; Bueno, H.; Pocock, S.J.; on behalf of the ICA-SEMES Research Group. Predicting 30-Day Mortality for Patients with Acute Heart Failure in the Emergency Department: A Cohort Study. Ann. Intern. Med. 2017, 167, 698–705. [Google Scholar] [CrossRef]
- Collins, G.S.; Reitsma, J.B.; Altman, D.G.; Moons, K.G. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): The TRIPOD statement. BMJ 2015, 350, g7594. [Google Scholar] [CrossRef] [PubMed]
- Lundberg, S.M.; Lee, S.-I. A Unified Approach to Interpreting Model Predictions. arXiv 2017. [Google Scholar] [CrossRef]
- Fey, M.; Lenssen, J.E. Fast Graph Representation Learning with PyTorch Geometric. arXiv 2017. [Google Scholar] [CrossRef]
- Sax, D.R.; Mark, D.G.; Rana, J.S.; Reed, M.E.; Lindenfeld, J.; Stevenson, L.W.; Storrow, A.B.; Butler, J.; Pang, P.S.; Collins, S.P. Current Emergency Department Disposition of Patients With Acute Heart Failure: An Opportunity for Improvement. J. Card. Fail. 2022, 28, 1545–1559. [Google Scholar] [CrossRef]
- Long, B.; Koyfman, A.; Gottlieb, M. Diagnosis of Acute Heart Failure in the Emergency Department: An Evidence-Based Review. West. J. Emerg. Med. 2019, 20, 875–884. [Google Scholar] [CrossRef]
- Miró, Ò.; Aguiló, O.; Trullàs, J.C.; Gil, V.; Espinosa, B.; Jacob, J.; Herrero-Puente, P.; Tost, J.; Comas, P.; Bibiano, C.; et al. QT interval and short-term outcome in acute heart failure. Clin. Res. Cardiol. 2023, 112, 1754–1765. [Google Scholar] [CrossRef]
- Brooksby, P.; Batin, P.D.; Nolan, S.J.; Lindsay, S.J.; Andrews, R.; Mullen, M.; Baig, W.; Flapan, A.D.; Prescott, R.J.; Neilson, J.M.; et al. The relationship between QT intervals and mortality in ambulant patients with chronic heart failure. The United Kingdom heart failure evaluation and assessment of risk trial (UKHEART). Eur. Heart 1999, 20, 1335–1341. [Google Scholar] [CrossRef]
- Vrtovec, B.; Delgado, R.; Zewail, A.; Thomas, C.D.; Richartz, B.M.; Radovancevic, B. Prolonged QTc interval and high B-type natriuretic peptide levels together predict mortality in patients with advanced heart failure. Circulation 2003, 107, 1764–1769. [Google Scholar] [CrossRef] [PubMed]
- Hong, J.A.; Kim, M.-S.; Park, H.; Lee, S.E.; Lee, H.-Y.; Cho, H.-J.; Choi, J.O.; Jeon, E.-S.; Hwang, K.-K.; Chae, S.C.; et al. Prognostic Value of QRS Duration Among Patients with Cardiogenic Shock Complicating Acute Heart Failure: Data from the Korean Acute Heart Failure (KorAHF) Registry. Int. J. Heart Fail. 2020, 2, 121–130. [Google Scholar] [CrossRef] [PubMed]
- Ponikowski, P.; Voors, A.A.; Anker, S.D.; Bueno, H.; Cleland, J.G.F.; Coats, A.J.S.; Falk, V.; González-Juanatey, J.R.; Harjola, V.-P.; Jankowska, E.A.; et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016, 37, 2129–2200, Correction: Eur. Heart J. 2018, 39, 860. [Google Scholar] [CrossRef] [PubMed]
- Long, B.; Koyfman, A.; Gottlieb, M. Management of Heart Failure in the Emergency Department Setting: An Evidence-Based Review of the Literature. J. Emerg. Med. 2018, 55, 635–646. [Google Scholar] [CrossRef] [PubMed]
- Petrie, C.J.; Voors, A.A.; Robertson, M.; van Veldhuisen, D.J.; Dargie, H.J. A low pulse pressure predicts mortality in subjects with heart failure after an acute myocardial infarction: A post-hoc analysis of the CAPRICORN study. Clin. Res. Cardiol. 2012, 101, 29–35. [Google Scholar] [CrossRef]
- Regnault, V.; Lagrange, J.; Pizard, A.; Safar, M.E.; Fay, R.; Pitt, B.; Challande, P.; Rossignol, P.; Zannad, F.; Lacolley, P. Opposite predictive value of pulse pressure and aortic pulse wave velocity on heart failure with reduced left ventricular ejection fraction: Insights from an Eplerenone Post-Acute Myocardial Infarction Heart Failure Efficacy and Survival Study (EPHESUS) substudy. Hypertension 2014, 63, 105–111. [Google Scholar] [CrossRef]
- Gheorghiade, M.; Vaduganathan, M.; Ambrosy, A.; Böhm, M.; Campia, U.; Cleland, J.G.F.; Fedele, F.; Fonarow, G.C.; Maggioni, A.P.; Mebazaa, A.; et al. Current management and future directions for the treatment of patients hospitalized for heart failure with low blood pressure. Heart Fail. Rev. 2013, 18, 107–122. [Google Scholar] [CrossRef]
- Masip, J.; Peacock, W.F.; Price, S.; Cullen, L.; Martin-Sanchez, F.J.; Seferovic, P.; Maisel, A.S.; Miro, O.; Filippatos, G.; Vrints, C.; et al. Indications and practical approach to non-invasive ventilation in acute heart failure. Eur. Heart J. 2018, 39, 17–25. [Google Scholar] [CrossRef]
- Park, S.B.; Khattar, D. Tachypnea. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2024. [Google Scholar]
- Filippatos, G.; Rossi, J.; Lloyd-Jones, D.M.; Stough, W.G.; Ouyang, J.; Shin, D.D.; O’Connor, C.; Adams, K.F.; Orlandi, C.; Gheorghiade, M. Prognostic value of blood urea nitrogen in patients hospitalized with worsening heart failure: Insights from the Acute and Chronic Therapeutic Impact of a Vasopressin Antagonist in Chronic Heart Failure (ACTIV in CHF) study. J. Card. Fail. 2007, 13, 360–364. [Google Scholar] [CrossRef]
- Zhou, H.-B.; Xu, T.-Y.; Liu, S.-R.; Bai, Y.-J.; Huang, X.-F.; Zhan, Q.; Zeng, Q.-C.; Xu, D.-L. Association of serum uric acid change with mortality, renal function and diuretic dose administered in treatment of acute heart failure. Nutr. Metab. Cardiovasc. Dis. 2019, 29, 351–359. [Google Scholar] [CrossRef]
- Huang, G.; Qin, J.; Deng, X.; Luo, G.; Yu, D.; Zhang, M.; Zhou, S.; Wang, L. Prognostic value of serum uric acid in patients with acute heart failure: A meta-analysis. Medicine 2019, 98, e14525. [Google Scholar] [CrossRef]
- Madan, V.D.; Novak, E.; Rich, M.W. Impact of change in serum sodium concentration on mortality in patients hospitalized with heart failure and hyponatremia. Circ. Heart Fail. 2011, 4, 637–643. [Google Scholar] [CrossRef]
- Klein, L.; O’connor, C.M.; Leimberger, J.D.; Gattis-Stough, W.; Piña, I.L.; Felker, G.M.; Adams, K.F., Jr.; Califf, R.M.; Gheorghiade, M.; OPTIME-CHF Investigators. Lower serum sodium is associated with increased short-term mortality in hospitalized patients with worsening heart failure: Results from the Outcomes of a Prospective Trial of Intravenous Milrinone for Exacerbations of Chronic Heart Failure (OPTIME-CHF) study. Circulation 2005, 111, 2454–2460. [Google Scholar] [CrossRef] [PubMed]
- Kajimoto, K.; Minami, Y.; Sato, N.; Takano, T. Investigators of the Acute Decompensated Heart Failure Syndromes (ATTEND) registry. Serum sodium concentration, blood urea nitrogen, and outcomes in patients hospitalized for acute decompensated heart failure. Int. J. Cardiol. 2016, 222, 195–201. [Google Scholar] [CrossRef] [PubMed]
- Marchenko, R.; Sigal, A.; Wasser, T.E.; Reyer, J.; Green, J.; Mercogliano, C.; Khan, M.S.; Donato, A.A. Hypochloraemia and 30 day readmission rate in patients with acute decompensated heart failure. ESC Heart Fail. 2020, 7, 903–907. [Google Scholar] [CrossRef]
- Radulović, B.; Potočnjak, I.; Terešak, S.D.; Trbušić, M.; Vrkić, N.; Malogorski, D.; Starčević, N.; Milošević, M.; Frank, S.; Degoricija, V. Hypochloraemia as a predictor of developing hyponatraemia and poor outcome in acute heart failure patients. Int. J. Cardiol. 2016, 212, 237–241. [Google Scholar] [CrossRef]
- Wan, S.-H.; Slusser, J.P.; Hodge, D.O.; Chen, H.H. Outcomes of Patients with Diabetes Versus Patients Without Diabetes Hospitalized with Acute Heart Failure. Am. J. Cardiol. 2022, 165, 65–71. [Google Scholar] [CrossRef] [PubMed]
- Kong, M.G.; Jang, S.Y.; Jang, J.; Cho, H.-J.; Lee, S.; Lee, S.E.; Kim, K.H.; Yoo, B.-S.; Kang, S.-M.; Baek, S.H.; et al. Impact of diabetes mellitus on mortality in patients with acute heart failure: A prospective cohort study. Cardiovasc. Diabetol. 2020, 19, 49. [Google Scholar] [CrossRef]
- Kocabaş, U.; Sinan, Ü.Y.; Aruğaslan, E.; Kurşun, M.; Çoner, A.; Özcan Çelebi, Ö.; Öztürk, C.; Dalgıç, O.; Türkoğlu, E.I.; Kemal, H.S.; et al. Clinical characteristics and in-hospital outcomes of acute decompensated heart failure patients with and without atrial fibrillation. Anatol. J. Cardiol. 2020, 23, 260–267. [Google Scholar] [CrossRef]
- Velliou, M.; Sanidas, E.; Diakantonis, A.; Ventoulis, I.; Parissis, J.; Polyzogopoulou, E. The Optimal Management of Patients with Atrial Fibrillation and Acute Heart Failure in the Emergency Department. Medicina 2023, 59, 2113. [Google Scholar] [CrossRef]
- Ito, K.; Li, S.; Homma, S.; Thompson, J.L.P.; Buchsbaum, R.; Matsumoto, K.; Anker, S.D.; Qian, M.; Di Tullio, M.R.; WARCEF Investigators. Left ventricular dimensions and cardiovascular outcomes in systolic heart failure: The WARCEF trial. ESC Heart Fail. 2021, 8, 4997–5009. [Google Scholar] [CrossRef] [PubMed]
- Almodares, Q.; Guron, C.W.; Thurin, A.; Fu, M.; Kontogeorgos, S.; Thunstrom, E.; Johansson, M.C. Larger right atrium than left atrium is associated with all-cause mortality in elderly patients with heart failure. Echocardiography 2017, 34, 662–667. [Google Scholar] [CrossRef] [PubMed]
- Merlos, P.; Núñez, J.; Sanchis, J.; Miñana, G.; Palau, P.; Bodí, V.; Husser, O.; Santas, E.; Bondanza, L.; Chorro, F.J. Echocardiographic estimation of pulmonary arterial systolic pressure in acute heart failure. Prognostic implications. Eur. J. Intern. Med. 2013, 24, 562–567. [Google Scholar] [CrossRef] [PubMed]
- Raffaello, W.M.; Henrina, J.; Huang, I.; Lim, M.A.; Suciadi, L.P.; Siswanto, B.B.; Pranata, R. Clinical Characteristics of De Novo Heart Failure and Acute Decompensated Chronic Heart Failure: Are They Distinctive Phenotypes That Contribute to Different Outcomes? Card. Fail. Rev. 2021, 7, e02. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | Study Cohort (N = 908) | Met Primary Endpoint (N = 81) | Did not Meet Primary Endpoint (N = 827) | p-Value |
|---|---|---|---|---|
| Medical history | ||||
| Age, years | 71.6 ± 13 | 74.9 ± 13.3 | 71.2 ± 13.0 | 0.003 |
| Men, N (%) | 500 (55.1) | 35 (43.2) | 465 (56.2) | 0.025 |
| De novo HF, N (%) | 748 (82.4) | 63 (77.8) | 685 (82.8) | 0.255 |
| Diabetes mellitus, N (%) | 346 (38.1) | 32 (39.5) | 314 (38) | 0.786 |
| Hypertension, N (%) | 836 (92) | 75 (92.6) | 761 (92) | 0.855 |
| Previous MI, N (%) | 563 (62) | 51 (63) | 512 (61.9) | 0.852 |
| PCI, N (%) | 340 (37.4) | 15 (18.5) | 325 (39.3) | <0.001 |
| CABG/MCBG, N (%) | 78 (8.6) | 4 (4.9) | 74 (8.9) | 0.219 |
| Valvular heart disease, N (%) | 66 (7.3) | 5 (6.2) | 61 (7.4) | 0.691 |
| Prior stroke, N (%) | 170 (18.7) | 29 (35.8) | 141 (17) | <0.001 |
| Prior PM implantation | 98 (10.8) | 15 (18.5) | 83 (10) | 0.019 |
| Prior ICD/CRT implantation, N (%) | 40 (4.4) | 3 (3.7) | 37 (4.5) | >0.999 |
| CKD, N (%) | 494 (54.4) | 63 (77.7) | 431 (52.1) | <0.001 |
| Prior dialysis, N (%) | 6 (0.7) | 5 (0.6) | 1 (1.2) | 0.430 |
| Cancer, N (%) | 46 (5.1) | 4 (4.9) | 42 (5.1) | >0.999 |
| Prior CPAP, N (%) | 16 (1.76) | 7 (0.8) | 9 (11.1) | <0.001 |
| Vital signs at presentation | ||||
| HR, bpm | 80 [70; 94] | 88.0 [72.0; 102.0] | 78.0 [70.0; 92.0] | 0.013 |
| SBP, mm Hg | 129.7 ± 24.4 | 113.6 ± 27.0 | 131.3 ± 23.5 | <0.001 |
| DBP, mm Hg | 77.2 ± 14.4 | 68.1 ± 18.0 | 78.0 ± 13.7 | <0.001 |
| Brachial pulse BP, mm Hg | 52.5 ± 17.0 | 45.5 ± 14.9 | 53.2 ± 17.1 | <0.001 |
| RR, brpm | 17 [16; 18] | 19.4 ± 4.3 | 17.5 ± 3.1 | <0.001 |
| SpO2 < 90%, N (%) | 106 (11.7) | 69 (8.3) | 37 (45.7) | <0.001 |
| Admission laboratory values | ||||
| Nt-proBNP, pg/mL | 4632 [2137; 9172] | 5133.5 [2122; 9017] | 4115 [2158; 9448] | 0.2 |
| Troponin I, ng/mL | 0.0 [0.0; 0.0] | 0.0 [0.0; 0.1] | 0.0 [0.0; 0.0] | <0.001 |
| Creatinine, mcmol/L | 123.8 ± 76.7 | 180.8 ± 125.6 | 118.3 ± 67.7 | <0.001 |
| eGFR, mL/min per 1.73 m2 | 58.1 ± 23.0 | 42.6 ± 25.6 | 59.6 ± 22.1 | <0.001 |
| Blood urea nitrogen, mg/dL | 7.8 [5.9; 11.0] | 12.3 [7.7; 21.4] | 7.5 [5.8; 10.3] | <0.001 |
| Uric acid, mcmol/L | 462.6 ± 178.4 | 589.2 ± 212.5 | 450.2 ± 169.8 | <0.001 |
| Blood sodium, mmol/l | 139.3 ± 4.9 | 137.1 ± 8.3 | 139.5 ± 4.4 | <0.001 |
| Hyponatremia, N (%) | 114 (12.6) | 28 (34.6) | 86 (10.4) | <0.001 |
| Blood chloride, mmol/l | 104.5 ± 6.3 | 104.6 ± 9.8 | 104.5 ± 5.9 | 0.402 |
| Hypochloremia, N (%) | 61 (6.7) | 8 (9.9) | 53 (6.4) | 0.234 |
| Blood potassium, mmol/l | 4.2 ± 1.1 | 4.5 ± 2.3 | 4.2 ± 0.9 | <0.001 |
| Hypokalemia, N (%) | 132 (14.5) | 18 (22.2) | 114 (13.8) | 0.040 |
| Hyperkalemia, N (%) | 26 (2.9) | 7 (8.6) | 19 (2.3) | 0.006 |
| Glucose, mmol/l | 6.55 [5.61; 8.23] | 7.05 [6.61; 8.44] | 5.48 [4.90; 6.51] | 0.07 |
| Hemoglobin, g/l | 129.4 ± 23.8 | 126.1 ± 26.4 | 129.7 ± 23.5 | 0.134 |
| Hematocrit, % | 39.8 ± 9.1 | 38.6 ± 7.4 | 39.9 ± 9.3 | 0.223 |
| Anemia, N (%) | 333 (36.7) | 296 (35.8%) | 37 (45.7%) | 0.078 |
| Platelet count, ×109/L | 214.0 ± 82.8 | 195.7 ± 90.6 | 215.8 ± 81.8 | 0.004 |
| Leukocyte count, ×109/L | 8.1 ± 4.2 | 10.7 ± 6.6 | 7.9 ± 3.8 | <0.001 |
| Lymphocyte count, ×109/L | 21.3 ± 10.2 | 14.2 ± 9.8 | 22.0 ± 10 | <0.001 |
| Bilirubin, mcmol/L | 17.3 ± 13 | 3.5 ± 1.2 | 4.2 ± 1.3 | 0.024 |
| TC, mmol/L | 4.1 ± 1.3 | 3.5 ± 1.2 | 4.2 ± 1.3 | <0.001 |
| TAG, mmol/L | 1.4 ± 0.7 | 1.4 ± 0.5 | 1.4 ± 0.7 | 0.420 |
| ALT, U/L | 29 [20; 43.6] | 31 [25; 69] | 29 [20; 43] | 0.004 |
| AST, U/L | 27 [21.5; 38] | 26.4 [21; 36.9] | 35 [24; 69] | <0.001 |
| CRP, mg/L | 9.6 [2.7; 27.1] | 27.9 [9.6; 63.9] | 8.7 [2.6; 23.5] | <0.001 |
| Procalcitonin, ng/mL | 0.2 [0.1; 0.4] | 0.1 [0.1; 0.3] | 0.3 [0.1; 0.7] | <0.001 |
| LDH, U/L | 301.5 [214.5; 408.5] | 362 [241; 611] | 293.4 [212; 405] | <0.001 |
| Lactate, mmol/L | 2.1 [1.4; 2.9] | 2.5 [1.9; 3.6] | 2.1 [1.4; 2.8] | <0.001 |
| INR | 1.3 [1.1; 1.6] | 1.5 [1.2; 1.8] | 1.2 [1.1; 1.5] | <0.001 |
| Fibrinogen, g/L | 4.2 ± 2.1 | 4.2 ± 2.2 | 4.0 ± 1.0 | 0.428 |
| ECG at admission | ||||
| Atrial fibrillation/flutter, N (%) | 325 (35.8) | 32 (39.5) | 293 (35.4) | 0.465 |
| LBBB, N (%) | 160 (17.6) | 20 (24.7) | 140 (16.9) | 0.080 |
| QRS duration, ms | 100 [100; 100] | 100 [100; 100] | 100 [100; 100] | 0.117 |
| Corrected QT interval, ms | 500 [400; 500] | 500 [400; 500] | 500 [400; 500] | 0.966 |
| ECHO at admission | ||||
| LVEF, % | 40.9 ± 12.2 | 37.1 ± 13.3 | 41.2 ± 12.0 | 0.002 |
| LVEF ≤ 40%, N (%) | 457 (50.3) | 49 (60.5) | 408 (49.3) | 0.072 |
| LVEF = 41–49%, N (%) | 180 (19.8) | 14 (17.3) | 166 (20.1) | 0.649 |
| LVEF ≥ 50%, N (%) | 271 (29.8) | 18 (22.2) | 253 (30.6) | 0.149 |
| LVEDV, mL | 139.2 ± 65.4 | 134.6 ± 63.3 | 139.7 ± 65.6 | 0.579 |
| LVEDS, mm | 5.4 ± 2.4 | 5.4 ± 2.5 | 5.3 ± 1.1 | 0.788 |
| RVD, mm | 3.5 ± 1.6 | 3.5 ± 1.7 | 3.5 ± 0.8 | 0.832 |
| LAV, mL | 94.9 ± 41.1 | 94.6 ± 41.1 | 98.2 ± 40.3 | 0.304 |
| RAD, mm | 5.0 [4.0; 17.5] | 5.2 [4.4; 19.1] | 5 [4; 17.5] | 0.297 |
| RAV, mL | 74.2 ± 39.3 | 86.5 ± 45.3 | 73.0 ± 38.5 | 0.004 |
| IVC diameter, mm | 2.1 ± 0.9 | 2.2 ± 0.5 | 2.1 ± 0.9 | 0.007 |
| IVC non-collapsable, N (%) | 512 (57.5) | 61 (75.3) | 461 (55.7) | 0.001 |
| Mitral regurgitation moderate–severe, N (%) | 435 (47.9) | 48 (59.3) | 387 (46.8) | 0.042 |
| Tricuspid regurgitation moderate–severe, N (%) | 338 (37.2) | 48 (59.3) | 290 (35.1) | <0.001 |
| PA SBP, mm Hg | 46.9 ± 17.5 | 53.5 ± 17.5 | 46.3 ± 17.3 | <0.001 |
| PH derived by ECHO, N (%) | 705 (77.6) | 635 (76.8) | 70 (86.4) | 0.047 |
| Peak aortic valve velocity, m/s | 1.8 ± 1.1 | 1.9 ± 1.2 | 1.8 ± 1.1 | 0.763 |
| Data | N, Included | Moderate Risk, Needed Pressors | High Risk, Died | Median Survival Time, Days |
|---|---|---|---|---|
| Training set | 635 | 10 (1.6%) | 43 (6%) | 43 (40, –) |
| Test set | 273 | 7 (2.6%) | 21 (7%) | 39 (39, 39) |
| XGBoost CV/SHAP | Neural Network Kernel Explainer/SHAP |
|---|---|
| SpO2 < 90% | LV EDS |
| QTc duration | PBP |
| Prior DM | BUN levels |
| Serum chloride concentration | RAS |
| Prior HF diagnosis | Serum chloride concentration |
| RR | Serum sodium concentration |
| BUN levels | Serum uric acid concentration |
| Any implanted device | Prior loop diuretics |
| AF on admission | SBP |
| SPAP |
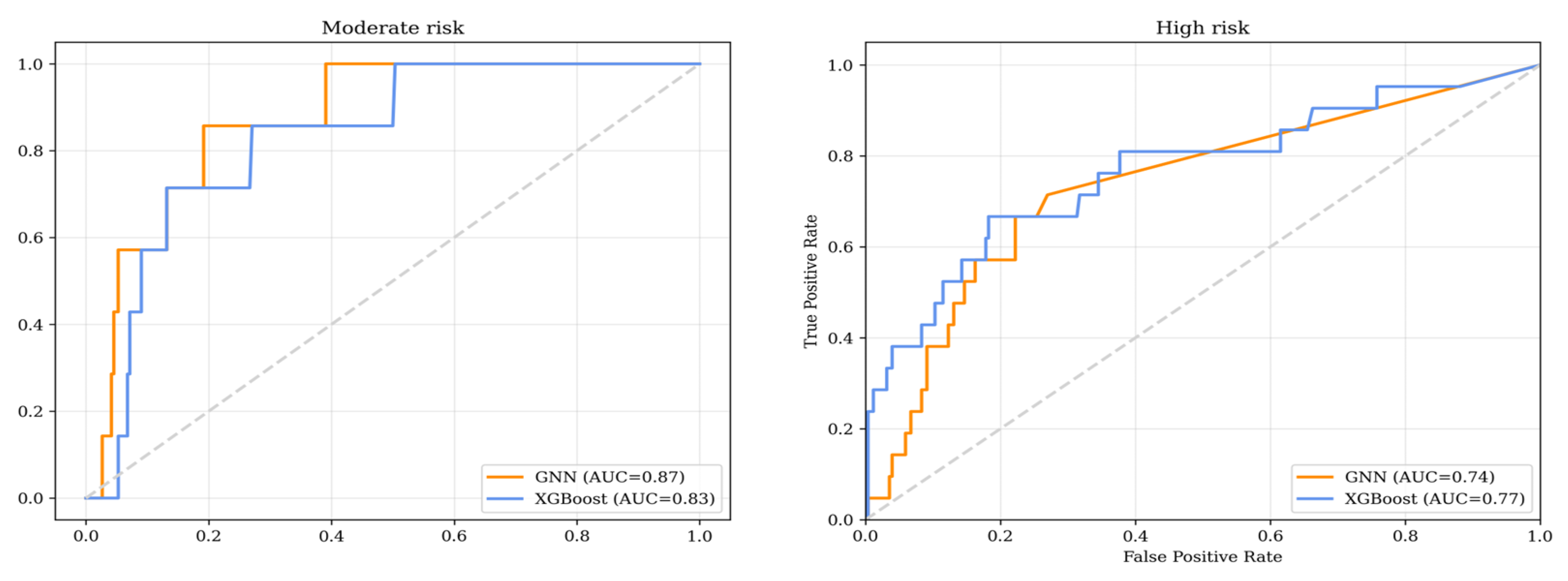
| Metric | XGBoost | GNN |
|---|---|---|
| AUC | 0.83 (0.698; 0.931) | 0.867 (0.744; 0.951) |
| Sensitivity | 0.714 (0.35; 0.789) | 0.857 (0.5; 1) |
| Specificity | 0.774 (0.722; 0.826) | 0.665 (0.606; 0.725) |
| NPV | 0.999 (0.976; 0.999) | 0.994 (0.982; 1) |
| PPV | 0.077 (0.017; 0.156) | 0.1 (0.021; 0.121) |
| Metric | XGBoost | GNN |
|---|---|---|
| AUC | 0.744 (0.636; 0.879) | 0.765 (0.634; 0.862) |
| Sensitivity | 0.238 (0.056; 0.435) | 0.429 (0.211; 0.647) |
| Specificity | 0.996 (0.988; 0.999) | 0.937 (0.905; 0.967) |
| NPV | 0.94 (0.91; 0.966) | 0.952 (0.924; 0.977) |
| PPV | 0.833 (0.4; 0.999) | 0.36 (0.172; 0.556) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shchekochikhin, D.; Charaya, K.; Shilova, A.; Nesterov, A.; Pershina, E.; Sherashov, A.; Panov, S.; Ibraimov, S.; Bogdanova, A.; Suvorov, A.; et al. Prognostic Markers of Adverse Outcomes in Acute Heart Failure: Use of Machine Learning and Network Analysis with Real Clinical Data. J. Clin. Med. 2025, 14, 1934. https://doi.org/10.3390/jcm14061934
Shchekochikhin D, Charaya K, Shilova A, Nesterov A, Pershina E, Sherashov A, Panov S, Ibraimov S, Bogdanova A, Suvorov A, et al. Prognostic Markers of Adverse Outcomes in Acute Heart Failure: Use of Machine Learning and Network Analysis with Real Clinical Data. Journal of Clinical Medicine. 2025; 14(6):1934. https://doi.org/10.3390/jcm14061934
Chicago/Turabian StyleShchekochikhin, Dmitri, Kristina Charaya, Alexandra Shilova, Alexey Nesterov, Ekaterina Pershina, Andrei Sherashov, Sergei Panov, Shevket Ibraimov, Alexandra Bogdanova, Alexander Suvorov, and et al. 2025. "Prognostic Markers of Adverse Outcomes in Acute Heart Failure: Use of Machine Learning and Network Analysis with Real Clinical Data" Journal of Clinical Medicine 14, no. 6: 1934. https://doi.org/10.3390/jcm14061934
APA StyleShchekochikhin, D., Charaya, K., Shilova, A., Nesterov, A., Pershina, E., Sherashov, A., Panov, S., Ibraimov, S., Bogdanova, A., Suvorov, A., Trushina, O., Bguasheva, Z., Rozina, N., Klimenko, A., Mareyeva, V., Voinova, N., Dukhnovskaya, A., Konchina, S., Zakaryan, E., ... Andreev, D. (2025). Prognostic Markers of Adverse Outcomes in Acute Heart Failure: Use of Machine Learning and Network Analysis with Real Clinical Data. Journal of Clinical Medicine, 14(6), 1934. https://doi.org/10.3390/jcm14061934







