Simultaneous Vascularized Lymph Node Transfer and Breast Reconstruction: A Systematic Review
Abstract
1. Introduction
2. Methods
2.1. Search Strategy and Study Selection
2.2. Data Extraction and Statistical Analysis
3. Results
3.1. Search Results
3.2. Patient Characteristics
3.3. Comorbidities
3.4. Breast and Lymphatic Reconstruction
3.5. Simultaneous VLNT and Breast Reconstruction Outcomes
3.6. Complications
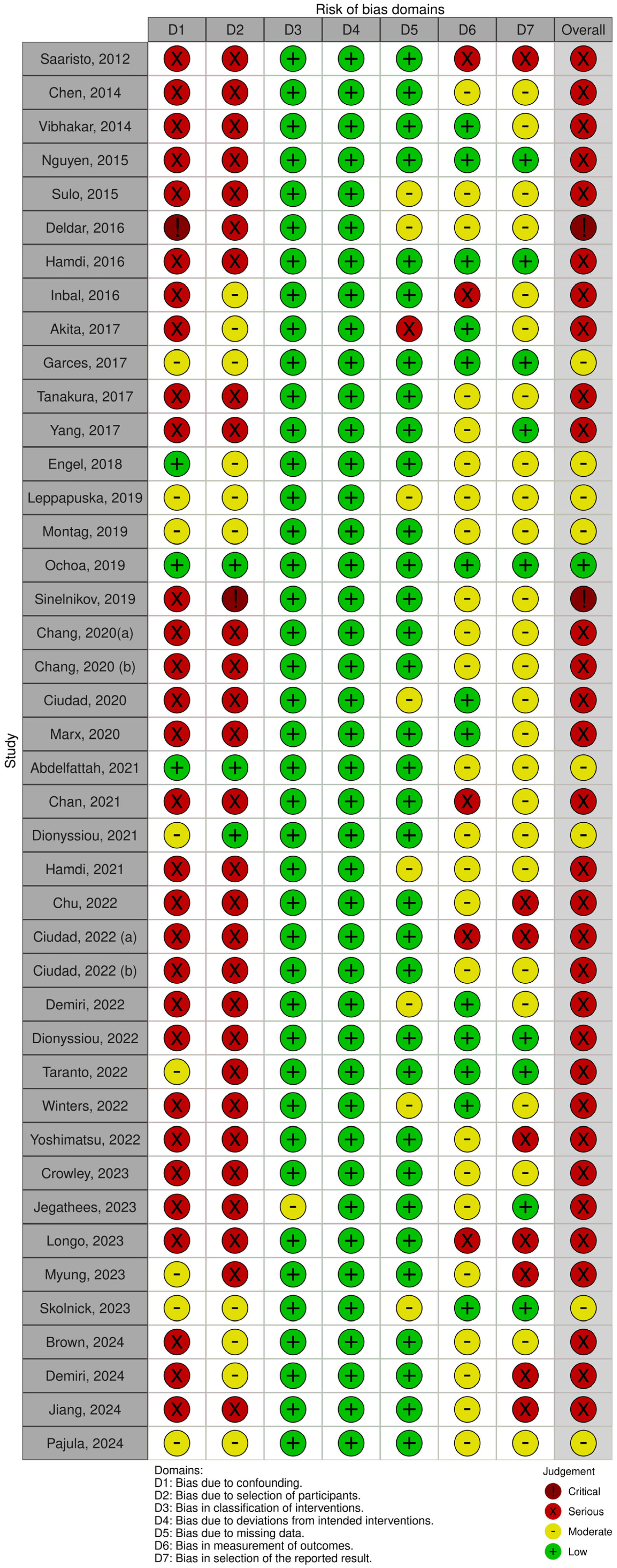
3.7. Risk of Bias
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- DiSipio, T.; Rye, S.; Newman, B.; Hayes, S. Incidence of Unilateral Arm Lymphoedema after Breast Cancer: A Systematic Review and Meta-Analysis. Lancet Oncol. 2013, 14, 500–515. [Google Scholar] [CrossRef] [PubMed]
- Shamoun, S.; Ahmad, M. Complete Decongestive Therapy Effect on Breast Cancer Related to Lymphedema: A Systemic Review and Meta-Analysis of Randomized Controlled Trials. Asian Pac. J. Cancer Prev. 2023, 24, 2225–2238. [Google Scholar] [CrossRef] [PubMed]
- Ciudad, P.; Bolletta, A.; Kaciulyte, J.; Losco, L.; Manrique, O.J.; Cigna, E.; Mayer, H.F.; Escandón, J.M. The Breast Cancer-related Lymphedema Multidisciplinary Approach: Algorithm for Conservative and Multimodal Surgical Treatment. Microsurgery 2023, 43, 427–436. [Google Scholar] [CrossRef] [PubMed]
- Brahma, B.; Yamamoto, T. Breast Cancer Treatment-Related Lymphedema (BCRL): An Overview of the Literature and Updates in Microsurgery Reconstructions. Eur. J. Surg. Oncol. 2019, 45, 1138–1145. [Google Scholar] [CrossRef]
- Clodius, L.; Smith, P.J.; Bruna, J.; Serafin, D. The Lymphatics of the Groin Flap. Ann. Plast. Surg. 1982, 9, 447–458. [Google Scholar] [CrossRef]
- Schaverien, M.; Badash, I.; Patel, K.; Selber, J.; Cheng, M.-H. Vascularized Lymph Node Transfer for Lymphedema. Semin. Plast. Surg. 2018, 32, 028–035. [Google Scholar] [CrossRef]
- Chang, E.I.; Masià, J.; Smith, M.L. Combining Autologous Breast Reconstruction and Vascularized Lymph Node Transfer. Semin. Plast. Surg. 2018, 32, 36–41. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Viitanen, T.P.; Mäki, M.T.; Seppänen, M.P.; Suominen, E.A.; Saaristo, A.M. Donor-Site Lymphatic Function after Microvascular Lymph Node Transfer: Plast. Reconstr. Surg. 2012, 130, 1246–1253. [Google Scholar] [CrossRef]
- Chen, R.; Mu, L.; Zhang, H.; Xin, M.; Luan, J.; Mu, D.; Liu, C.; Ji, K.; Hu, J.; Sun, J.; et al. Simultaneous Breast Reconstruction and Treatment of Breast Cancer–Related Upper Arm Lymphedema with Lymphatic Lower Abdominal Flap. Ann. Plast. Surg. 2014, 73, S12–S17. [Google Scholar] [CrossRef]
- Vibhakar, D.; Reddy, S.; Morgan-Hazelwood, W.; Chang, E.I. Chimeric Pedicled Latissimus Dorsi Flap with Lateral Thoracic Lymph Nodes for Breast Reconstruction and Lymphedema Treatment in a Hypercoagulable Patient. Plast. Reconstr. Surg. 2014, 134, 494e–495e. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, A.T.; Chang, E.I.; Suami, H.; Chang, D.W. An Algorithmic Approach to Simultaneous Vascularized Lymph Node Transfer with Microvascular Breast Reconstruction. Ann. Surg. Oncol. 2015, 22, 2919–2924. [Google Scholar] [CrossRef] [PubMed]
- Sulo, E.; Hartiala, P.; Viitanen, T.; Mäki, M.; Seppänen, M.; Saarikko, A. Risk of Donor-Site Lymphatic Vessel Dysfunction after Microvascular Lymph Node Transfer. J. Plast. Reconstr. Aesthet. Surg. 2015, 68, 551–558. [Google Scholar] [CrossRef] [PubMed]
- Deldar, R.; Duquette, S.; Ceppa, E.P.; Lester, M.; Sood, R.; Socas, J. An Alternative Approach to Combined Autologous Breast Reconstruction with Vascularized Lymph Node Transfer. Microsurgery 2017, 37, 463–464. [Google Scholar] [CrossRef]
- De Brucker, B.; Zeltzer, A.; Seidenstuecker, K.; Hendrickx, B.; Adriaenssens, N.; Hamdi, M. Breast Cancer–Related Lymphedema: Quality of Life after Lymph Node Transfer. Plast. Reconstr. Surg. 2016, 137, 1673–1680. [Google Scholar] [CrossRef]
- Inbal, A.; Teven, C.M.; Chang, D.W. Latissimus Dorsi Flap with Vascularized Lymph Node Transfer for Lymphedema Treatment: Technique, Outcomes, Indications and Review of Literature. J. Surg. Oncol. 2017, 115, 72–77. [Google Scholar] [CrossRef]
- Akita, S.; Tokumoto, H.; Yamaji, Y.; Sasahara, Y.; Kubota, Y.; Kubo, M.; Kuriyama, M.; Mitsukawa, N. Contribution of Simultaneous Breast Reconstruction by Deep Inferior Epigastric Artery Perforator Flap to the Efficacy of Vascularized Lymph Node Transfer in Patients with Breast Cancer-Related Lymphedema. J. Reconstr. Microsurg. 2017, 33, 571–578. [Google Scholar] [CrossRef]
- Miranda Garcés, M.; Pons, G.; Mirapeix, R.; Masià, J. Intratissue Lymphovenous Communications in the Mechanism of Action of Vascularized Lymph Node Transfer. J. Surg. Oncol. 2017, 115, 27–31. [Google Scholar] [CrossRef]
- Tanakura, K.; Matsumoto, A.; Kuramoto, Y.; Sawaizumi, M. The Number of Lymph Nodes That Can Be Added to an Abdominal Flap for Breast Reconstruction: Review of Enhanced MDCT Images. Int. Microsurg. J. 2017, 1, 1. [Google Scholar] [CrossRef]
- Yang, Z.; Huang, S.; Wang, J.; Xi, Y.; Yang, X.; Tang, Q.; Du, J.; Nie, J.; Zou, T.; Zhou, S.; et al. A Retrospective Study of Lymphatic Transverse Rectus Abdominis Myocutaneous/Deep Inferior Epigastric Perforator Flaps for Breast Cancer Treatment-Induced Upper-Limb Lymphoedema. Sci. Rep. 2017, 7, 80. [Google Scholar] [CrossRef]
- Engel, H.; Lin, C.-Y.; Huang, J.-J.; Cheng, M.-H. Outcomes of Lymphedema Microsurgery for Breast Cancer-Related Lymphedema with or Without Microvascular Breast Reconstruction. Ann. Surg. 2018, 268, 1076–1083. [Google Scholar] [CrossRef] [PubMed]
- Leppäpuska, I.-M.; Suominen, E.; Viitanen, T.; Rannikko, E.; Visuri, M.; Mäki, M.; Saarikko, A.; Hartiala, P. Combined Surgical Treatment for Chronic Upper Extremity Lymphedema Patients: Simultaneous Lymph Node Transfer and Liposuction. Ann. Plast. Surg. 2019, 83, 308–317. [Google Scholar] [CrossRef] [PubMed]
- Montag, E.; Okada, A.Y.; Arruda, E.G.P.; Fonseca, A.S.; Bromley, M.; Munhoz, A.M.; Busnardo, F.F.; Gemperli, R. Influência Do Posicionamento Do Retalho Linfonodal Vascularizado Na Resposta Ao Tratamento Cirúrgico Do Linfedema Secundário Ao Câncer de Mama. Rev. Colégio Bras. Cir. 2019, 46, e2156. [Google Scholar] [CrossRef] [PubMed]
- Ochoa, O.; Metzner, M.; Theoharis, C.; Chrysopoulo, M.; Pisano, S.; Nastala, C.; Ledoux, P.; Arishita, G.; Garza, R.; Snider, T. Deep Inferior Epigastric Lymph Node Basin: Analysis of Novel Donor Site for Vascularized Lymph Node Transfer among 10 Consecutive Patients. Microsurgery 2019, 39, 215–220. [Google Scholar] [CrossRef]
- Sinelnikov, M.Y.; Chen, K.; Sukorceva, N.S.; Lan, M.; Bikov, I.I.; Zakirova, A.A.; Reshetov, I.V. A Clinical Case of Breast Reconstruction with Greater Omentum Flap for Treatment of Upper Extremity Lymphedema. Plast. Reconstr. Surg. Glob. Open 2019, 7, e2402. [Google Scholar] [CrossRef]
- Chang, E.I.; Schaverien, M.V.; Hanson, S.E.; Chu, C.K.; Hanasono, M.M. Evolution in Surgical Management of Breast Cancer-Related Lymphedema: The MD Anderson Cancer Center Experience. Plast. Reconstr. Surg. Glob. Open 2020, 8, e2674. [Google Scholar] [CrossRef]
- Chang, E.I.; Ibrahim, A.; Liu, J.; Robe, C.; Suami, H.; Hanasono, M.M.; Nguyen, A.T. Optimizing Quality of Life for Patients with Breast Cancer–Related Lymphedema: A Prospective Study Combining DIEP Flap Breast Reconstruction and Lymphedema Surgery. Plast. Reconstr. Surg. 2020, 145, 676e–685e. [Google Scholar] [CrossRef]
- Ciudad, P.; Manrique, O.J.; Bustos, S.S.; Vargas, M.I.; Reynaga, C.; Agko, M.; Huang, T.C.T.; Benites, E.F.; Mayer, H.F.; Forte, A.J. Combined Microvascular Breast and Lymphatic Reconstruction with Deep Inferior Epigastric Perforator Flap and Gastroepiploic Vascularized Lymph Node Transfer for Postmastectomy Lymphedema Patients. Gland Surg. 2020, 9, 512–520. [Google Scholar] [CrossRef]
- Marx, M.; Geßner, M.; Florek, A.; Morgenstern, S.; Passin, S.; Brucker, S.Y.; Wallwiener, D.; Hahn, M. Re-augmentation of the Axilla Using a Turn-Over Flap—A New Approach for the Surgical Treatment of Secondary Lymphedema After Breast Cancer. Geburtshilfe Frauenheilkd. 2020, 80, 526–531. [Google Scholar] [CrossRef]
- Abdelfattah, U.; Hamza, F.; Elbanoby, T.; Ayad, W.; Hong, J. Evaluation of Free Vascularized Groin Lymph Nodes Transfer for Treatment of Secondary Upper Limb Lymphedema. Al-Azhar Int. Med. J. 2021, 2, 31–38. [Google Scholar] [CrossRef]
- Chan, S.L.S.; Gogna, A.; Chui, C.H.K.; Wong, M. Complete Lymphatic Restoration by Simultaneous Vascularized Lymph Node and Lymphatic Vessel Transplantation. Eur. J. Plast. Surg. 2021, 44, 687–697. [Google Scholar] [CrossRef]
- Dionyssiou, D.; Sarafis, A.; Tsimponis, A.; Kalaitzoglou, A.; Arsos, G.; Demiri, E. Long-Term Outcomes of Lymph Node Transfer in Secondary Lymphedema and Its Correlation with Flap Characteristics. Cancers 2021, 13, 6198. [Google Scholar] [CrossRef]
- Hamdi, M.; Ramaut, L.; De Baerdemaeker, R.; Zeltzer, A. Decreasing Donor Site Morbidity after Groin Vascularized Lymph Node Transfer with Lessons Learned from a 12-Year Experience and Review of the Literature. J. Plast. Reconstr. Aesthet. Surg. 2021, 74, 540–548. [Google Scholar] [CrossRef] [PubMed]
- Pons, G.; Abdelfattah, U.; Sarria, J.; Duch, J.; Masia, J. Reverse Lymph Node Mapping Using Indocyanine Green Lymphography: A Step Forward in Minimizing Donor-Site Morbidity in Vascularized Lymph Node Transfer. Plast. Reconstr. Surg. 2021, 147, 207e–212e. [Google Scholar] [CrossRef] [PubMed]
- Chang, E.I.; Chu, C.K.; Hanson, S.E.; Selber, J.C.; Hanasono, M.M.; Schaverien, M.V. Comprehensive Overview of Available Donor Sites for Vascularized Lymph Node Transfer. Plast. Reconstr. Surg. Glob. Open 2020, 8, e2675. [Google Scholar] [CrossRef]
- Demiri, E.; Dionyssiou, D. Combined Autologous Breast and Lymphedema Reconstruction with a Predesigned DIEP and Lymph-Node Flap. In Clinical Scenarios in Reconstructive Microsurgery; Gravvanis, A., Kakagia, D.D., Ramakrishnan, V., Eds.; Springer International Publishing: Cham, Switzerland, 2022; pp. 665–672. ISBN 978-3-030-23705-9. [Google Scholar]
- Dionyssiou, D.; Demiri, E. A Comprehensive Treatment Algorithm for Patients Requiring Simultaneous Breast and Lymphedema Reconstruction Based on Lymph Node Transfer. Ann. Breast Surg. 2022, 6, 33. [Google Scholar] [CrossRef]
- Di Taranto, G.; Coleman, G.J.; Hardwicke, J.; Wallis, K.L.; Skillman, J. A Comparative Study between Deep Inferior Epigastric Artery Perforator Flap Breast Reconstruction and DIEP Flap Breast Reconstruction Coupled with Vascularized Lymph Node Transfer: Improving the Quality of Life of Patients with Breast Cancer Related Lymphedema without Affecting Donor Site Outcomes. Microsurgery 2023, 43, 213–221. [Google Scholar] [CrossRef]
- Winters, H.; Tielemans, H.J.P.; Hummelink, S.; Slater, N.J.; Ulrich, D.J.O. DIEP Flap Breast Reconstruction Combined with Vascularized Lymph Node Transfer for Patients with Breast Cancer-Related Lymphedema. Eur. J. Surg. Oncol. 2022, 48, 1718–1722. [Google Scholar] [CrossRef]
- Yoshimatsu, H.; Karakawa, R.; Fuse, Y.; Yano, T. Simultaneous Lymphatic Superficial Circumflex Iliac Artery Perforator Flap Transfer from the Zone 4 Region in Autologous Breast Reconstruction Using the Deep Inferior Epigastric Artery Perforator Flap: A Proof-of-Concept Study. J. Clin. Med. 2022, 11, 534. [Google Scholar] [CrossRef]
- Crowley, J.S.; Liu, F.C.; Rizk, N.M.; Nguyen, D. Concurrent Management of Lymphedema and Breast Reconstruction with Single-stage Omental Vascularized Lymph Node Transfer and Autologous Breast Reconstruction: A Case Series. Microsurgery 2024, 44, e31017. [Google Scholar] [CrossRef]
- Jegathees, T.; Mackie, H.; Ngo, Q.; Lam, T. Breast Reconstruction for Treatment of Upper Limb Lymphoedema: A Case Report. Australas. J. Plast. Surg. 2023, 6, 1–5. [Google Scholar] [CrossRef]
- Longo, B.; Pistoia, A.; D’Orsi, G.; Gagliano, E.; Vannucchi, L.; Cervelli, V. Lympho-diep flap transfer perfused by reverse-flow thoracodorsal artery: A case report. Plast. Reconstr. Regen. Surg. 2023, 2, 20–24. [Google Scholar] [CrossRef]
- Myung, Y.; Park, J.K.; Beom, J.; Lim, J.-Y.; Park, Y.S.; Ahn, S.-H.; Kang, E.; Shin, H.-C.; Kim, E.-K.; Nam, S.-Y.; et al. Outcome Analysis of Combined Surgical Approaches in Advanced-Stage Upper Extremity Breast Cancer-Related Lymphedema. Plast. Reconstr. Surg. Glob. Open 2023, 11, e5237. [Google Scholar] [CrossRef] [PubMed]
- Chiang, S.; Skolnick, G.; Sacks, J.M.; Christensen, J.M. Complication Profile of Combined Microvascular Breast Reconstruction Combined with Vascularised Lymph Node Transplant. Available online: https://woundsinternational.com/journal-articles/complication-profile-of-combined-microvascular-breast-reconstruction-combined-with-vascularised-lymph-node-transplant/ (accessed on 16 October 2024).
- Brown, S.; Kokosis, G.; Graziano, F.D.; Haran, O.; Smith-Montes, E.; Zivanovic, O.; Ariyan, C.E.; Coit, D.G.; Coriddi, M.; Mehrara, B.J.; et al. Immediate Lymphatic Reconstruction with Vascularized Omentum Lymph Node Transplant: Reducing the Risk of Both Painful Contracture and Lymphedema. Plast. Reconstr. Surg. Glob. Open 2024, 12, e5747. [Google Scholar] [CrossRef]
- Demiri, E.; Dionyssiou, D.; Kyriazidis, I.; Drougou, A.; Tsimponis, A. Predesigned Chimeric Deep Inferior Epigastric Perforator and Inguinal Lymph Node Flap for Combined Breast and Lymphedema Reconstruction: A Comprehensive Algorithmic Approach. JPRAS Open 2024, 40, 1–18. [Google Scholar] [CrossRef]
- Jiang, Z.; Yu, Z.; Li, S. Vascularized Lymph Node Transfer Using Axilla as Recipient Site Restores Lymphatic Flow in Upper Limb Lymphedema: Evidence from Magnetic Resonance Lymphangiography. Chin. J. Plast. Reconstr. Surg. 2024, 6, 1–7. [Google Scholar] [CrossRef]
- Pajula, S.; Saarikko, A.; Suominen, S.; Kaartinen, I.; Kiiski, J.; Mani, M.; Halle, M.; Hartiala, P. Donor-Site Safety in Microvascular Lymph Node Transfer for Breast Cancer-Related Lymphedema Using Reverse Lymphatic Mapping—A Prospective Study. J. Plast. Reconstr. Aesthet. Surg. 2024, 98, 20–31. [Google Scholar] [CrossRef]
- Ciudad, P.; Escandón, J.M.; Manrique, O.J.; Gutierrez-Arana, J.; Mayer, H.F. Lymphedema Prevention and Immediate Breast Reconstruction with Simultaneous Gastroepiploic Vascularized Lymph Node Transfer and Deep Inferior Epigastric Perforator Flap: A Case Report. Microsurgery 2022, 42, 617–621. [Google Scholar] [CrossRef]
- Saaristo, A.M.; Niemi, T.S.; Viitanen, T.P.; Tervala, T.V.; Hartiala, P.; Suominen, E.A. Microvascular Breast Reconstruction and Lymph Node Transfer for Postmastectomy Lymphedema Patients. Ann. Surg. 2012, 255, 468–473. [Google Scholar] [CrossRef]
- Chu, C.K.; Hanasono, M.M.; Chang, E.I. Treatment of Multiple Limb Lymphedema with Combined Supermicrosurgical Techniques. Microsurgery 2023, 43, 13–19. [Google Scholar] [CrossRef]
- World Cancer Research Fund. Worldwide Cancer Data 2024. Available online: https://www.wcrf.org/preventing-cancer/cancer-statistics/worldwide-cancer-data/#global-cancer-incidence-in-women (accessed on 19 December 2024).
- Matar, D.Y.; Wu, M.; Haug, V.; Orgill, D.P.; Panayi, A.C. Surgical Complications in Immediate and Delayed Breast Reconstruction: A Systematic Review and Meta-Analysis. J. Plast. Reconstr. Aesthet. Surg. 2022, 75, 4085–4095. [Google Scholar] [CrossRef] [PubMed]
- Scaglioni, M.F.; Arvanitakis, M.; Chen, Y.; Giovanoli, P.; Chia-Shen Yang, J.; Chang, E.I. Comprehensive Review of Vascularized Lymph Node Transfers for Lymphedema: Outcomes and Complications. Microsurgery 2018, 38, 222–229. [Google Scholar] [CrossRef] [PubMed]
- Demiri, E.; Dionyssiou, D.; Tsimponis, A.; Goula, O.C.; Mιlothridis, P.; Pavlidis, L.; Spyropoulou, G.A.; Foroglou, P. Donor-Site Lymphedema Following Lymph Node Transfer for Breast Cancer-Related Lymphedema: A Systematic Review of the Literature. Lymphat. Res. Biol. 2018, 16, 2–8. [Google Scholar] [CrossRef] [PubMed]
- Dayan, J.H.; Dayan, E.; Smith, M.L. Reverse Lymphatic Mapping: A New Technique for Maximizing Safety in Vascularized Lymph Node Transfer. Plast. Reconstr. Surg. 2015, 135, 277–285. [Google Scholar] [CrossRef]
- Gerety, P.A.; Pannucci, C.J.; Basta, M.N.; Wang, A.R.; Zhang, P.; Mies, C.; Kanchwala, S.K. Lymph Node Content of Supraclavicular and Thoracodorsal-Based Axillary Flaps for Vascularized Lymph Node Transfer. J. Vasc. Surg. Venous Lymphat. Disord. 2016, 4, 80–87. [Google Scholar] [CrossRef]
- Raju, A.; Chang, D.W. Vascularized Lymph Node Transfer for Treatment of Lymphedema: A Comprehensive Literature Review. Ann. Surg. 2015, 261, 1013–1023. [Google Scholar] [CrossRef]
- Howell, A.C.; Gould, D.J.; Mayfield, C.; Samakar, K.; Hassani, C.; Patel, K.M. Anatomical Basis of the Gastroepiploic Vascularized Lymph Node Transfer: A Radiographic Evaluation Using Computed Tomographic Angiography. Plast. Reconstr. Surg. 2018, 142, 1046–1052. [Google Scholar] [CrossRef]
- Masià, J.; Pons, G.; Rodríguez-Bauzà, E. Barcelona Lymphedema Algorithm for Surgical Treatment in Breast Cancer–Related Lymphedema. J. Reconstr. Microsurg. 2016, 32, 329–335. [Google Scholar] [CrossRef]
- Cho, M.-J.; Flores Garcia, J.; Myung, Y.; Cha, H.G.; Hayashi, A.; Hong, J.P.; Skoracki, R. Evolving Role of Lymphedema Surgery on Breast Reconstruction: A Systematic Review and Multi-Institutional Algorithmic Approach. J. Clin. Med. 2024, 13, 6518. [Google Scholar] [CrossRef]
- Brazio, P.S.; Nguyen, D.H. Combined Liposuction and Physiologic Treatment Achieves Durable Limb Volume Normalization in Class II–III Lymphedema: A Treatment Algorithm to Optimize Outcomes. Ann. Plast. Surg. 2021, 86, S384–S389. [Google Scholar] [CrossRef]

| Authors | Year | Indication for VLNT | Type of Breast Reconstruction | Donor Site | N | Follow-Up (Months) | Outcome |
|---|---|---|---|---|---|---|---|
| Saaristo et al. [9] | 2012 | Treatment | TRAM, DIEP | SCIA | 9 | 24 | Simultaneous BR and VLNT is an optimal option for BRCL. |
| Chen et al. [10] | 2014 | Treatment | TRAM, DIEP | SCIA | 10 | 12 | BR with simultaneous VLNT and adjuvant lymphedema therapy is effective in restoring function of the breasts |
| Vibhakar et al. [11] | 2014 | Treatment | LD | Lateral Thoracic | 1 | 2.5 | Simultaneous LD flap and VLNT is an excellent solution for BR and lymphedema treatment. |
| Nguyen et al [12] | 2015 | Treatment | TRAM, DIEP | SIEA | 29 | 11 | The algorithm discussed in this paper shows promising results for simultaneous abdominal BR and VLNT. |
| Sulo et al. [13] | 2015 | Treatment | DIEP, TRAM | SCIA | 21 | 34.8 | Care must be taken when harvesting donor lymph nodes, although no clinical donor lymphedema was found in the study population. |
| Deldar et al. [14] | 2016 | Treatment | DIEP | Omentum | 5 | NA | Gastroepiploic lymph nodes for use of simultaneous BR and VLNT allows for less risk compared to the groin. |
| Hamdi et al. [15] | 2016 | Treatment | DIEP | SCIA | 22 | 29.9 | VLNT significantly improves the quality of life in BRCL patients. |
| Inbal et al. [16] | 2016 | Treatment | LD | Lateral Thoracic | 11 | 6.7 | LD for BR with VLNT is a viable option for treatment of BRCL. |
| Akita et al. [17] | 2017 | Treatment | DIEP | SCIA | 13 | 13.9 | The DIEP flap is a strong option for simultaneous breast reconstruction when using the SCIA as a donor site for VLNT. |
| Garces et al. [18] | 2017 | Not specified | DIEP, SGAP | NA | 23 | 23.8 | ICG is an appropriate method to determine functional lymphovenous communications following BR with VLNT. |
| Tanakura et al. [19] | 2017 | Treatment | DIEP | SIEA | 1 | NA | On average, 3.67 nodes exist superior to the saphenofemoral junction using multidetector CT images. |
| Yang et al. [20] | 2017 | Treatment | TRAM, DIEP | SCIA | 10 | 12 | TRAM/DIEP VLNT and BR is a safe and effective treatment for patients with post-mastectomy lymphedema. |
| Engel et al. [21] | 2018 | Treatment | DIEP | SCIA | 11 | 15.4 | BR alone does not improve BRCL, but VLNT, with or without BR significantly improved BRCL. |
| Leppapuska et al. [22] | 2019 | Treatment | TRAM, DIEP | SCIA | 10 | SCIA | Simultaneous operations including BR, VLT, and liposuction are better than any procedure alone. |
| Montag et al. [23] | 2019 | Treatment | DIEP | SCIA | 9 | 18 | Simultaneous BR and VLNT positively impacts patients with BRCL with no difference in relation to the position of the flap. |
| Ochoa et al. [24] | 2019 | Not specified | DIEP | DIEP | 10 | NA | DIEP is an appropriate lymphatic donor site for BR and VLNT. |
| Sinelnikov et al. [25] | 2019 | Treatment | Greater Omental Flap | Omentum | 1 | 6 | BR using the greater omental flap, with its high lymphatic capability, allows for correction of disrupted fluid drainage in the upper extremities. |
| Chang et al. [26] | 2020 | Treatment | DIEP | SCIA, SIEA | 54 | 12 | DIEP flap with VLNT and lymphovenous bypass may be superior to BR and VLNT alone. |
| Chang et al. [27] | 2020 | Treatment | DIEP | SCIA | 38 | 19.1 | Simultaneous BR with VLNT, with or without lymphovenous bypass, is a promising treatment for BRCL. |
| Ciudad et al. [28] | 2020 | Treatment | DIEP | Omental | 6 | 12.8 | Combined DIEP and Omental VLNT is a safe, reliable, single-staged operation for BRCL. |
| Marx et al. [29] | 2020 | Treatment | DIEP | Thoracodorsal | 5 | 6 | BR and VLNT allow for reductions in lymphedema and pain and improved quality of life. |
| Abdelfattah et al. [30] | 2021 | Treatment | DIEP | SCIA | 6 | 30 | BR with simultaneous VLNT to the axilla or forearm is effective and reliable for treatment of BRCL. |
| Chan et al. [31] | 2021 | Treatment | DIEP | SIEA | 2 | 23 | VLNT, BR, and lymphatic anastomosis together seems to be better than VLNT and BR alone. |
| Dionyssiou et al. [32] | 2021 | Treatment | DIEP, LD | SIEA, SCIA | 24 | 36 | Larger flaps consisting of a higher number of LNs were associated with improved outcomes following simultaneous BR and VLNT. |
| Hamdi et al. [33] | 2021 | Treatment | DIEP | SIEA | 65 | 62.4 | Seroma is the most likely complication of simultaneous VLNT and BR. |
| Chu et al. [34] | 2022 | Treatment | DIEP | SIEA | 3 | NA | Patients suffering from BRCL can be safely treated with simultaneous BR and VLNT, with or without lymphovenous bypass. |
| Ciudad et al. [3] | 2022 | Preventative | DIEP | Omentum | 1 | 36 | Simultaneous VLNT and BR allows for the possibility of the prevention of lymphedema without the risk of iatrogenic lymphedema. |
| Ciudad et al. [35] | 2022 | Treatment | DIEP | Omentum | 10 | NA | For advanced stages of BRCL, a combination of procedures along with BR-VLNT is needed. |
| Demiri et al. [36] | 2022 | Treatment | DIEP | SCIA | 1 | 28 | Patient reported high level of satisfaction with breast and lymphedema reconstructions. |
| Dionyssiou et al. [37] | 2022 | Treatment | TDAP, DIEP, LD, 2 Stage TE | Lateral Thoracic, Groin | 69 | 56 | VLNT with BR allows for a single surgical procedure to provide the best outcome in post-mastectomy lymphedema patients. |
| Taranto et al. [38] | 2022 | Treatment | DIEP | SIEA | 32 | 42.5 | Simultaneous DIEP and VLNT improves the quality of life of lymphedema patients and use with abdominal flap at no increased risk. |
| Winters et al. [39] | 2022 | Treatment | DIEP | DIEP | 45 | 51.1 | Simultaneous VLNT and DIEP flap breast reconstruction can cause significant improvement in BRCL patient quality of life, with or without a change in volume difference. |
| Yoshimatsu et al. [40] | 2022 | Preventative | DIEP | SCIA, SCIP | 4 | 33.9 | Use of SCIP flap from Zone 4 region in DIEP flap breast reconstruction can improve and/or prevent lymphedema without need of another donor site. |
| Crowley et al. [41] | 2023 | Treatment | TRAM, DIEP | Omentum | 7 | 14.6 | The omentum is a versatile and safe door site for simultaneous VLNT and BR. |
| Jegathees et al. [42] | 2023 | Treatment | TRAM | SCIA | 1 | 49 | Simultaneous BR and VLNT allows for a functional solution for BR with disrupted lymphatic systems. |
| Longo et al. [43] | 2023 | Treatment | DIEP | SIEA | 1 | 3 | Retrograde flow from the thoracodorsal artery is a viable option as a recipient vessel and enhances the success of DIEP flap BR VLNT. |
| Myung et al. [44] | 2023 | Treatment | TRAM, DIEP | Omentum | 49 | 27.05 | All surgical methods in the study, including VLNT with BR using the omental flap resulted in reduction in edema and improved patient satisfaction. |
| Skolnick et al. [45] | 2023 | Not specified | NA | NA | 75 | 1 | VLNT with BR for BRCL does not significantly change the risk from BR alone. |
| Brown et al. [46] | 2024 | Preventative | DIEP | Omentum | 13 | 15.1 | VLNT is a promising procedure to minimize lymphedema and contracture following extensive lymph node dissection and radiotherapy |
| Demiri et al. [47] | 2024 | Treatment | DIEP | SCIA | 34 | 35 | The algorithm proposed for DIEP and VLNT allows for “highly satisfactory” breast and lymphedema reconstruction. |
| Jiang et al. [48] | 2024 | Treatment | DIEP | SCIA | 2 | 12 | VLNT is an effective treatment for BRLC, with or without BR. |
| Pajula et al. [49] | 2024 | Treatment | DIEP | SCIA | 26 | 12 | VLNT with reverse lymphatic mapping is safe and does not increase risk of donor site lymphedema with or without BR. |
| Outcome | |
|---|---|
| Significantly Improved Symptoms | 332 patients |
| Reported in | 22 (52.4%) articles |
| Improved Limb Volume | |
| Mean Excess Volume Reduction | 39.5% |
| Reported in | 21 (50%) articles |
| Mean Excess Circumference reduction | 33.5% |
| Reported in | 9 (21.4%) articles |
| No Change in Limb Volume | |
| No Change in Excess Volume | 57 Patients |
| Reported in | 3 (7.1%) articles |
| No Change in Excess Circumference | 2 Patients |
| Reported in | 2 (4.8%) articles |
| Complication | Number (%) |
|---|---|
| Total Complications | 168 (21.8%) |
| Donor Site Seroma | 46 (6%) |
| Abdominal Wound Dehiscence/Delayed Wound Healing | 42 (5.4%) |
| Skin Infections | 15 (1.9%) |
| Donor Site Pain/Numbness | 14 (1.8%) |
| Recipient Site Delayed Wound Healing | 10 (1.3%) |
| Non-specified Infections | 8 (1%) |
| Recipient Site Infection | 6 (0.8%) |
| Donor Site Lymphedema | 4 (0.5%) |
| Breast Flap Donor Site Hernia | 4 (0.5%) |
| Venous Thrombosis | 4 (0.5%) |
| Fat Necrosis | 4 (0.5%) |
| VLNT + BR Partial Flap Failure | 3 (0.4%) |
| Total Flap Failure | 3 (0.4%) |
| Flap Congestion | 2 (0.3%) |
| Skin Necrosis | 2 (0.3%) |
| Partial Breast Flap Failure | 1 (0.2%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Almadani, H.; Lu, J.; Bokhari, S.; How-Volkman, C.; Brazio, P.S. Simultaneous Vascularized Lymph Node Transfer and Breast Reconstruction: A Systematic Review. J. Clin. Med. 2025, 14, 1694. https://doi.org/10.3390/jcm14051694
Almadani H, Lu J, Bokhari S, How-Volkman C, Brazio PS. Simultaneous Vascularized Lymph Node Transfer and Breast Reconstruction: A Systematic Review. Journal of Clinical Medicine. 2025; 14(5):1694. https://doi.org/10.3390/jcm14051694
Chicago/Turabian StyleAlmadani, Hamzah, Jocelyn Lu, Sara Bokhari, Christiane How-Volkman, and Philip S. Brazio. 2025. "Simultaneous Vascularized Lymph Node Transfer and Breast Reconstruction: A Systematic Review" Journal of Clinical Medicine 14, no. 5: 1694. https://doi.org/10.3390/jcm14051694
APA StyleAlmadani, H., Lu, J., Bokhari, S., How-Volkman, C., & Brazio, P. S. (2025). Simultaneous Vascularized Lymph Node Transfer and Breast Reconstruction: A Systematic Review. Journal of Clinical Medicine, 14(5), 1694. https://doi.org/10.3390/jcm14051694






