Analyzing Declining Trends, Patient Demographics, and Complications in Total Elbow Arthroplasty: Nationwide Retrospective Data Analysis
Abstract
1. Introduction
2. Methods
2.1. Data Source
2.2. Cohort Definition and Selection Criteria
2.3. Statistical Analysis
2.4. Ethical Consideration
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| HCUP | Healthcare Cost and Utilization Project |
| ICD-10 | International Classification of Diseases, 10th Revision |
| TEA | Total Elbow Replacement |
| LOS | Length of Stay |
| RA | Rheumatoid Arthritis |
| NIS | Nationwide Inpatient Sample |
| SPSS | Statistical Package for the Social Sciences |
References
- Gay, D.M.; Lyman, S.; Do, H.; Hotchkiss, R.N.; Marx, R.G.; Daluiski, A. Indications and reoperation rates for total elbow arthroplasty: An analysis of trends in New York State. J. Bone Jt. Surg. Am. 2012, 94, 110–117. [Google Scholar] [CrossRef] [PubMed]
- Shi, L.L.; Zurakowski, D.; Jones, D.G.; Koris, M.J.; Thornhill, T.S. Semiconstrained primary and revision total elbow arthroplasty with use of the Coonrad-Morrey prosthesis. J. Bone Jt. Surg. Am. 2007, 89, 1467–1475. [Google Scholar] [CrossRef]
- Sørensen, B.W.; Brorson, S.; Olsen, B.S. Primary total elbow arthroplasty in complex fractures of the distal humerus. World J. Orthop. 2014, 5, 368–372. [Google Scholar] [CrossRef] [PubMed]
- Day, J.S.; Lau, E.; Ong, K.L.; Williams, G.R.; Ramsey, M.L.; Kurtz, S.M. Prevalence and projections of total shoulder and elbow arthroplasty in the United States to 2015. J. Shoulder Elb. Surg. 2010, 19, 1115–1120. [Google Scholar] [CrossRef]
- McKissack, H.; Karzon, A.R.; Hussain, Z.B.; Worden, J.A.; Heo, K.Y.; Cooke, H.L.; Ojimakinde, A.; Gottschalk, M.B.; Wagner, E.R. Is popularity of total elbow arthroplasty in the United States decreasing? An analysis of trends, demographics, and indications. JSES Rev. Rep. Tech. 2024, 4, 797–804. [Google Scholar] [CrossRef]
- Korpela, M.; Laasonen, L.; Hannonen, P.; Kautiainen, H.; Leirisalo-Repo, M.; Hakala, M.; Paimela, L.; Blåfield, H.; Puolakka, K.; Möttönen, T.; et al. Retardation of joint damage in patients with early rheumatoid arthritis by initial aggressive treatment with disease-modifying antirheumatic drugs: Five-year experience from the FIN-RACo study. Arthritis Rheum. 2004, 50, 2072–2081. [Google Scholar] [CrossRef]
- Zhou, H.; Orvets, N.D.; Merlin, G.; Shaw, J.; Dines, J.S.; Price, M.D.; Eichinger, J.K.; Li, X. Total Elbow Arthroplasty in the United States: Evaluation of Cost, Patient Demographics, and Complication Rates. Orthop. Rev. 2016, 8, 6113. [Google Scholar]
- Zhang, D.; Earp, B.E.; Blazar, P. Factors associated with 30-day complication, reoperation, readmission, and length of stay after primary total elbow arthroplasty: A database study of 555 patients. Semin. Arthroplast. JSES 2023, 33, 59–66. [Google Scholar] [CrossRef]
- Morrey, M.E.; Morrey, B.F.; Sanchez-Sotelo, J.; Barlow, J.D.; O’Driscoll, S. A review of the surgical management of distal humerus fractures and nonunions: From fixation to arthroplasty. J. Clin. Orthop. Trauma 2021, 20, 101477. [Google Scholar] [CrossRef]
- Polmear, M.M.; Scanaliato, J.P.; Rossettie, S.; Bader, J.; Nesti, L.J.; Dunn, J.C. Post-operative Immobilization in Total Elbow Arthroplasty for Rheumatoid Arthritis: A Systematic Review of Outcomes. J. Surg. Orthop. Adv. 2022, 31, 209–217. [Google Scholar]
- Kim, J.M.; Mudgal, C.S.; Konopka, J.F.; Jupiter, J.B. Complications of total elbow arthroplasty. J. Am. Acad. Orthop. Surg. 2011, 19, 328–339. [Google Scholar] [CrossRef] [PubMed]
- Voloshin, I.; Schippert, D.W.; Kakar, S.; Kaye, E.K.; Morrey, B.F. Complications of total elbow replacement: A systematic review. J. Shoulder Elb. Surg. 2011, 20, 158–168. [Google Scholar] [CrossRef] [PubMed]
- Dam, W.V.; Meijering, D.; Stevens, M.; Boerboom, A.L.; Eygendaal, D. Postoperative management of total elbow arthroplasty: Results of a European survey among orthopedic surgeons. PLoS ONE 2022, 17, e0277662. [Google Scholar] [CrossRef] [PubMed]
- Prkic, A.; Welsink, C.; The, B.; van den Bekerom, M.P.J.; Eygendaal, D. Why does total elbow arthroplasty fail today? A systematic review of recent literature. Arch. Orthop. Trauma Surg. 2017, 137, 761–769. [Google Scholar] [CrossRef]
- Jenkins, P.J.; Watts, A.C.; Norwood, T.; Duckworth, A.D.; Rymaszewski, L.A.; McEachan, J.E. Total elbow replacement: Outcome of 1,146 arthroplasties from the Scottish Arthroplasty Project. Acta Orthop. 2013, 84, 119–123. [Google Scholar] [CrossRef]
- Hamoodi, Z.; Sayers, A.; Whitehouse, M.R.; Rangan, A.; Kearsley-Fleet, L.; Sergeant, J.; Watts, A.C. Total elbow arthroplasty in England. Bone Jt. J. 2024, 106, 1312–1320. [Google Scholar] [CrossRef]
- Tarallo, L.; Celli, A.; Delvecchio, M.; Costabile, L.; Ciacca, G.; Porcellini, G.; Catani, F. Long-term outcomes and trends in elbow arthroplasty with Coonrad-Morrey prosthesis: A retrospective study in large group of patients. Int. Orthop. 2024, 48, 2689–2698. [Google Scholar] [CrossRef]
- Dehghan, N.; Furey, M.; Schemitsch, L.; Ristevski, B.; Goetz, T.; Schemitsch, E.H.; Canadian Orthopaedic Trauma Society (COTS); McKee, M. Long-term outcomes of total elbow arthroplasty for distal humeral fracture: Results from a prior randomized clinical trial. J. Shoulder Elb. Surg. 2019, 28, 2198–2204. [Google Scholar] [CrossRef]
- Viveen, J.; van den Bekerom, M.P.J.; Doornberg, J.N.; Hatton, A.; Page, R.; Koenraadt, K.L.M.; Wilson, C.; Bain, G.I.; Jaarsma, R.L.; Eygendaal, D. Use and outcome of 1,220 primary total elbow arthroplasties from the Australian Orthopaedic Association National Joint Arthroplasty Replacement Registry 2008–2018. Acta Orthop. 2019, 90, 511–516. [Google Scholar] [CrossRef]
- Zeltser, D.W.; Prentice, H.A.; Navarro, R.A.; Mirzayan, R.; Dillon, M.T.; Foroohar, A. Total Elbow Arthroplasty: A Descriptive Analysis of 170 Patients From a United States Integrated Health Care System. J. Hand Surg. Am. 2021, 46, 552–559. [Google Scholar] [CrossRef]
- Coviello, M.; Abate, A.; Ippolito, F.; Nappi, V.; Maddalena, R.; Maccagnano, G.; Noia, G.; Caiaffa, V. Continuous Cold Flow Device Following Total Knee Arthroplasty: Myths and Reality. Medicina 2022, 58, 1537. [Google Scholar] [CrossRef] [PubMed]
- Singh, J.A.; Ramachandran, R. Are there racial disparities in utilization and outcomes after total elbow arthroplasty? Rheumatol. Int. 2015, 35, 1479–1487. [Google Scholar] [CrossRef] [PubMed]
- Toor, A.S.; Jiang, J.J.; Shi, L.L.; Koh, J.L. Comparison of perioperative complications after total elbow arthroplasty in patients with and without diabetes. J. Shoulder Elb. Surg. 2014, 23, 1599–1606. [Google Scholar] [CrossRef] [PubMed]
- Lovy, A.J.; Keswani, A.; Dowdell, J.; Koehler, S.; Kim, J.; Hausman, M.R. Outcomes, complications, utilization trends, and risk factors for primary and revision total elbow replacement. J. Shoulder Elb. Surg. 2016, 25, 1020–1026. [Google Scholar] [CrossRef]
- Ramirez, M.A.; Cheung, E.V.; Murthi, A.M. Revision Total Elbow Arthroplasty. J. Am. Acad. Orthop. Surg. 2017, 25, e166–e174. [Google Scholar] [CrossRef]
- Foster, B.K.; Ayalon, O.; Hoyer, R.; Hoyen, H.A.; Grandizio, L.C. Postoperative Elbow Instability: Options for Revision Stabilization. J. Hand Surg. Am. 2024, 49, 362–371. [Google Scholar] [CrossRef]
- Jupiter, J.B.; Ring, D. Treatment of unreduced elbow dislocations with hinged external fixation. J. Bone Jt. Surg. Am. 2002, 84, 1630–1635. [Google Scholar] [CrossRef]
- Klug, A.; Gramlich, Y.; Buckup, J.; Schweigkofler, U.; Hoffmann, R.; Schmidt-Horlohé, K. Trends in total elbow arthroplasty: A nationwide analysis in Germany from 2005 to 2014. Int. Orthop. 2018, 42, 883–889. [Google Scholar] [CrossRef]
- Hodges, N.A.; Sussman, E.M.; Stegemann, J.P. Aseptic and septic prosthetic joint loosening: Impact of biomaterial wear on immune cell function, inflammation, and infection. Biomaterials 2021, 278, 121127. [Google Scholar] [CrossRef]
- Cherian, J.J.; Jauregui, J.J.; Banerjee, S.; Pierce, T.; Mont, M.A. What Host Factors Affect Aseptic Loosening After THA and TKA? Clin. Orthop. Relat. Res. 2015, 473, 2700–2709. [Google Scholar] [CrossRef]

| Characteristic | N = 4110 |
|---|---|
| Age (years) Mean (SD) | 65.99 (13.47) |
| Female | 619 (75.3%) |
| Race | |
| White | 597 (72.6%) |
| Black | 55 (6.7%) |
| Hispanic | 85 (10.3%) |
| Asian | 15 (1.8%) |
| Others | 70 (8.5%) |
| Type 2 Diabetes | 160 (19.5%) |
| Hypertension | 422 (51.3%) |
| Dyslipidemia | 306 (37.2%) |
| Sleep Apnea | 106 (12.9%) |
| Chronic Anemia | 54 (6.6%) |
| Alcohol Abuse | 8 (1%) |
| Mental Disorders | 313 (38.1%) |
| Current Smoker | 4 (0.5%) |
| Chronic kidney Disease | 67 (8.2%) |
| COPD | 95 (11.6%) |
| Hospital Size | |
| Small | 187 (22.7%) |
| Medium | 165 (20.1%) |
| Large | 470 (57.2%) |
| Geographic Region | |
| Northeast | 134 (16.3%) |
| Midwest | 203 (24.7%) |
| South | 300 (36.5%) |
| West | 185 (22.5%) |
| Hospital Teaching Status | |
| Rural | 105 (2.6) |
| Urban nonteaching | 620 (15.1) |
| Urban teaching | 3385 (82.4) |
| Primary Payer | |
| Medicare | 532 (64.7%) |
| Medicaid | 46 (5.6%) |
| Private | 191 (23.2%) |
| Other | 53 (6.4%) |
| Length of Stay (days) Median [IQR] | 2 [1–3] |
| Total Hospitalization Charges (USD) Median [IQR] | 78,473 [56,935–115,671] |
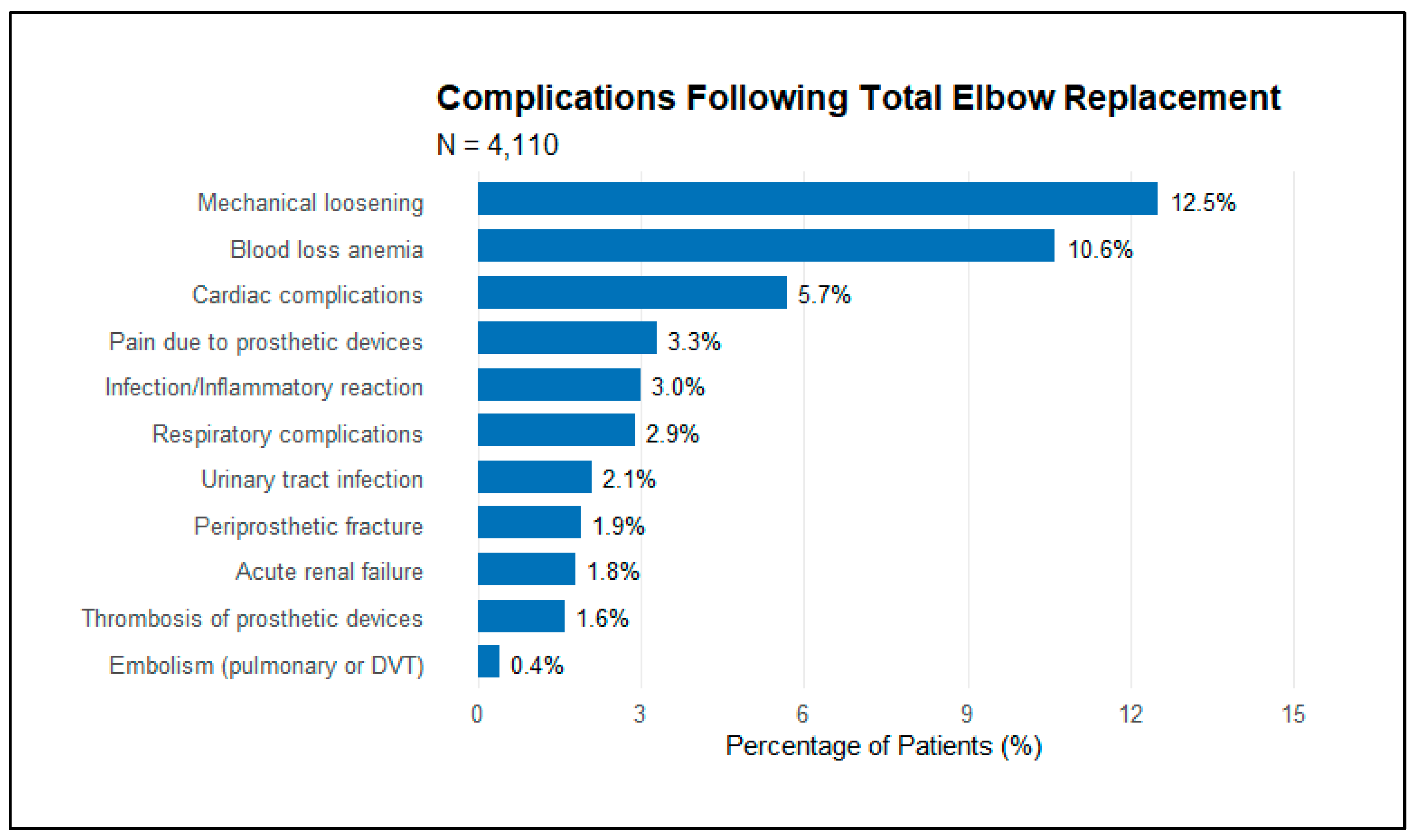
| Complication | % |
|---|---|
| Mechanical loosening | 12.5 |
| Blood loss anemia | 10.6 |
| Cardiac complications | 5.7 |
| Pain due to prosthetic devices | 3.3 |
| Infection/inflammatory reaction | 3 |
| Respiratory complications | 2.9 |
| Urinary tract infection | 2.1 |
| Periprosthetic fracture | 1.9 |
| Acute renal failure | 1.8 |
| Thrombosis of prosthetic devices | 1.6 |
| Embolism (pulmonary or DVT) | 0.4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mahamid, A.; Jayyusi, F.; Laver, L.; Haj Yahya, M.; Wolff, G.; Yassin, A.; Behrbalk, E. Analyzing Declining Trends, Patient Demographics, and Complications in Total Elbow Arthroplasty: Nationwide Retrospective Data Analysis. J. Clin. Med. 2025, 14, 1645. https://doi.org/10.3390/jcm14051645
Mahamid A, Jayyusi F, Laver L, Haj Yahya M, Wolff G, Yassin A, Behrbalk E. Analyzing Declining Trends, Patient Demographics, and Complications in Total Elbow Arthroplasty: Nationwide Retrospective Data Analysis. Journal of Clinical Medicine. 2025; 14(5):1645. https://doi.org/10.3390/jcm14051645
Chicago/Turabian StyleMahamid, Assil, Fairoz Jayyusi, Lior Laver, Mohammad Haj Yahya, Gal Wolff, Ali Yassin, and Eyal Behrbalk. 2025. "Analyzing Declining Trends, Patient Demographics, and Complications in Total Elbow Arthroplasty: Nationwide Retrospective Data Analysis" Journal of Clinical Medicine 14, no. 5: 1645. https://doi.org/10.3390/jcm14051645
APA StyleMahamid, A., Jayyusi, F., Laver, L., Haj Yahya, M., Wolff, G., Yassin, A., & Behrbalk, E. (2025). Analyzing Declining Trends, Patient Demographics, and Complications in Total Elbow Arthroplasty: Nationwide Retrospective Data Analysis. Journal of Clinical Medicine, 14(5), 1645. https://doi.org/10.3390/jcm14051645





