Management of Severe Hypothermia: Challenges and Advanced Strategies
Abstract
1. Introduction
2. Case Report
- (a)
- Bradycardia: 38 bpm;
- (b)
- Blood pressure: 160/74 mmHg;
- (c)
- SpO2: 84% (corrected to 93% with oxygen administration via nasal cannula at 3 L/min);
- (d)
- Normal, sluggishly reactive pupils;
- (e)
- Glasgow Coma Scale (GCS) score of 11—altered level of consciousness.
- ➢
- Pathological blood exam results are as follows:
- ○
- pH: 7.31 (mild acidosis);
- ○
- pH: 7.31 (mild acidosis);
- ○
- Lactate: 5.8 mmol/L (hyperlactatemia);
- ○
- Sodium (Na): 131 mmol/L (mild hyponatremia);
- ○
- Potassium (K): 3.0 mmol/L (mild hypokalemia);
- ○
- Glucose: 232 mg/dL (mild hyperglycemia).
- ➢
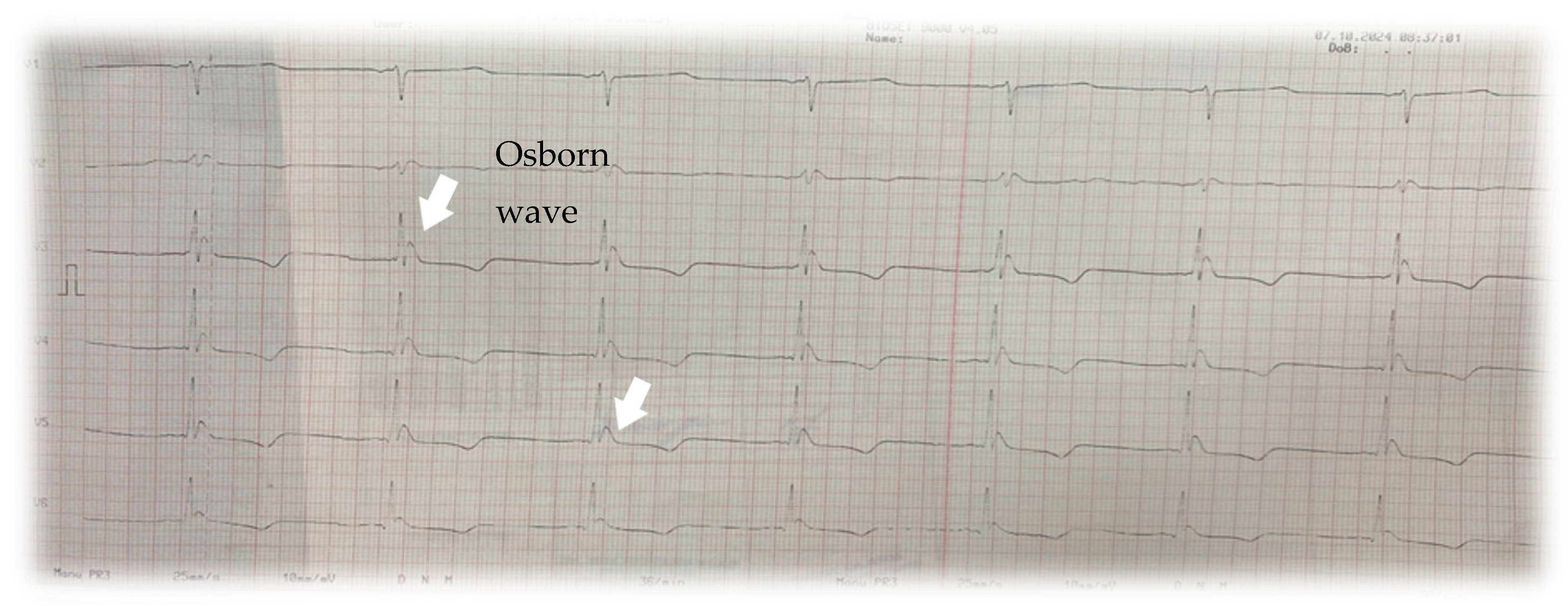
- Electrocardiogram (ECG): Sinus bradycardia at 38 bpm and the presence of an Osborn wave (J wave) was revealed, a hallmark finding in hypothermia(Figure 1).
- ➢
- Chest X-ray: No acute parenchymal pulmonary lesions were visible. Left-sided cardiac silhouette opacification and enlarged heart were observed.
- ○
- Passive Rewarming: The use of thermal blankets and placement of the patient in a warm environment.
- ○
- Active Rewarming:
- (a)
- Administration of heated intravenous (IV) fluids: Intravenous saline solutions were warmed to a safe temperature of 41 °C using a temperature-controlled convection device. These fluids contributed to the gradual elevation of the patient’s core temperature and stabilization of vital signs.
- (b)
- Controlled intravascular temperature management (IVTM):
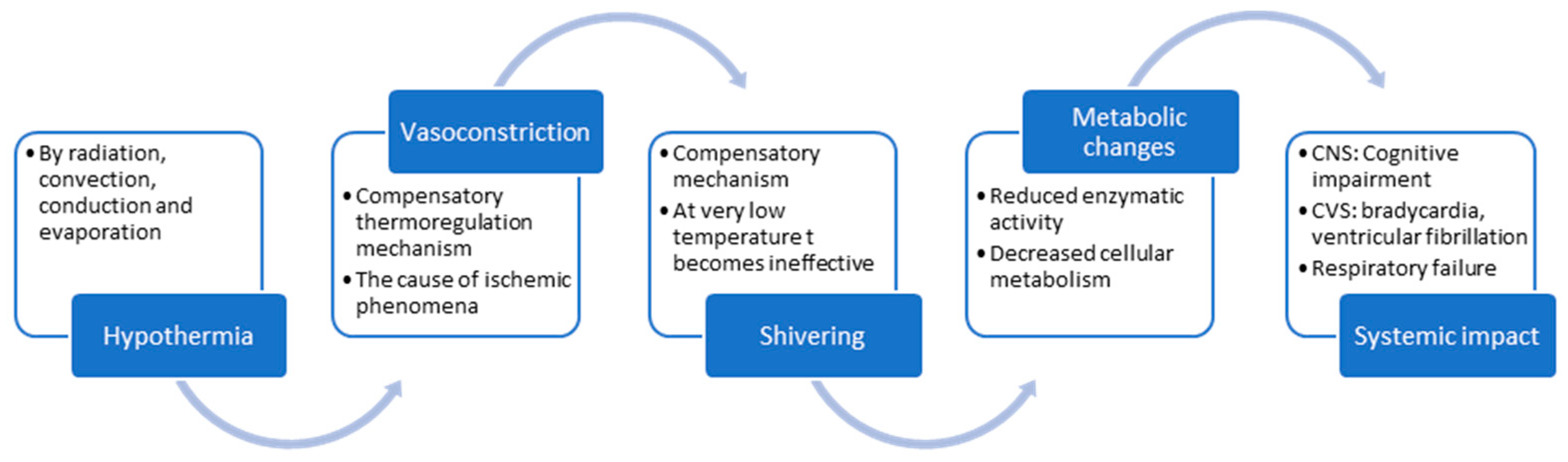
3. Discussion
- Stage 1: Core temperature between 35–32 °C—clear consciousness with shivering
- Stage 2: Core temperature between 32–28 °C—impaired consciousness without shivering
- Stage 3: Core temperature between 28–24 °C—unconsciousness
- Stage 4: Core temperature between 24–14 °C—apparent death
- Stage 5: Core temperature bellow 14 °C—death.
- Mild Hypothermia (32–35 °C), with symptoms like shivering, mild confusion, and weakness.
- Moderate Hypothermia (28–32 °C), with symptoms including severe bradycardia, profound confusion, and impaired coordination.
- Controlled intravascular active warming method (used in this case):This is an advanced temperature management system designed to precisely and rapidly regulate the patient’s core temperature. It utilizes a specialized intravascular catheter with multiple heat-exchange balloons, through which cooled or warmed saline circulates within a closed circuit, without infusing fluid into the patient. As venous blood passes over the balloons, its temperature is adjusted, allowing for the efficient cooling or warming of the patient.The system comprises a console and a heat-exchange catheter with multiple balloons. Saline circulates through the catheter within the closed circuit, cooling or warming the patient as venous blood flows past the balloons, without the additional fluid infused in the circulatory system. The target temperature and rate of temperature adjustment are set, and the system modifies the saline temperature accordingly. Patient and system data are displayed on the system screen or can be synchronized with hospital monitors.The working principle of this method [7] involves temperature regulation via a specialized circuit that maintains a constant body temperature or gradually increases the core temperature in a controlled manner, based on the patient’s clinical needs. This temperature management system is typically used in critical cases, such as cardiac arrest, stroke, or traumatic brain injury [8], where precise control of body temperature can be vital for improving clinical outcomes [9]. The key features of this procedures are the following:
- (a)
- Precise temperature control: The system enables the precise regulation of the patient’s temperature, whether cooling or warming is required. This capability is essential in therapeutic hypothermia or targeted temperature management (TTM).
- (b)
- Rapid temperature adjustment: The system can quickly adjust a patient’s temperature, which is critical in emergency situations where time is a decisive factor.
- (c)
- Closed-circuit system: It operates using a closed-loop system with catheters circulating thermally controlled saline, ensuring efficient heat exchange without relying on intravenous fluid administration.
- (d)
- Unlike other methods, this system does not require extracorporeal circulation.
- ECMO treatment (Extracorporeal Membrane Oxygenation) in hypothermiaECMO is a life-support technique used in cases of severe hypothermia, particularly when conventional rewarming methods fail or when the patient experiences cardiac or respiratory failure.ECMO is indicated in severe hypothermia (core temperature typically <28 °C) associated with cardiac or respiratory failure, especially in patients in cardiac arrest or those with refractory hypothermia (unresponsive to conventional rewarming methods such as external rewarming or internal methods like heated fluids).The ECMO circuit is initiated by inserting large cannulas (tubes) into major blood vessels. In veno-arterial (VA) ECMO, blood is drained from a large vein (typically the femoral or jugular vein), passed through the ECMO device for oxygenation and warming, and then returned to the body through a major artery (usually the femoral or carotid artery).Blood is gradually warmed as it circulates through the ECMO circuit. This controlled rewarming allows for a steady increase in core body temperature, minimizing complications such as “afterdrop” (the return of cold blood from peripheral tissues to the body core, exacerbating hypothermia) and, despite the complications [10] like bleeding, infection, or mechanical failure, with the following benefits:
- (a)
- Controlled rewarming: ECMO allows for a gradual and precise increase in core body temperature, reducing the risk of thermal shock or complications like arrhythmias, which are common during rapid rewarming.
- (b)
- Cardiopulmonary support: Since cardiac function is impaired in hypothermia, ECMO provides critical circulatory support.
- (c)
- Preservation of organ function: By maintaining circulation and oxygenation, ECMO ensures vital organ function is sustained during the rewarming process.
4. Challenges Encountered in Case Management
- Initial slow response to rewarming in a bradycardic and hypertensive patient with risks of fluid overload: Severe hypothermia presents significant challenges in elevating core body temperature through conventional methods such as thermal blankets and the administration of warm intravenous fluids. In this case, initial rewarming during the first two hours achieved only a 0.5 °C/hour increase in core temperature. Given the patient’s systolic blood pressure exceeding 160 mmHg, continued intravascular fluid administration posed risks of volume overload, necessitating the adoption of advanced rewarming techniques.
- Invasiveness of central venous catheter placement for IVTM: The invasive nature of inserting a specialized central venous catheter, typically via a femoral approach, poses additional challenges. The complications of the procedure are operator-dependent and similar to those associated with the insertion of a temporary dialysis catheter via femoral access.
- Cost [13] of advanced rewarming techniques: Advanced methods for managing severe hypothermia are significantly more expensive [14] compared to conventional active rewarming therapies. However, when comparing the IVTM technique used in this patient to extracorporeal membrane oxygenation (ECMO), there are notable cost differences. These differences may justify the selective use of IVTM, particularly in patients with contraindications to intravascular volume administration.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Savioli, G.; Ceresa, I.F.; Bavestrello Piccini, G.; Gri, N.; Nardone, A.; La Russa, R.; Saviano, A.; Piccioni, A.; Ricevuti, G.; Esposito, C. Hypothermia: Beyond the Narrative Review—The point of view of emergency physicians and medico-legal considerations. J. Pers. Med. 2023, 13, 1690. [Google Scholar] [CrossRef] [PubMed]
- Mattu, A.; Brady, W.J.; Perron, A.D.; Tabas, J.A. Electrocardiographic manifestations of hypothermia. Am. J. Emerg. Med. 2002, 20, 314–326. [Google Scholar] [CrossRef] [PubMed]
- Bartlett, E.S.; Valenzuela, T.; Idris, A.; Deye, N.; Glover, G.; Gillies, M.A.; Taccone, F.S.; Sunde, K.; Flint, A.C.; Thiele, H.; et al. Systematic review and meta-analysis of intravascular temperature management vs. surface cooling in comatose patients resuscitated from cardiac arrest. Resuscitation 2019, 146, 82–95. [Google Scholar] [CrossRef] [PubMed]
- Musi, M.E.; Sheets, A.; Zafren, K.; Brugger, H.; Paal, P.; Hölzl, N.; Pasquier, M. Clinical staging of accidental hypothermia: The Revised Swiss System. Resuscitation 2021, 162, 182–187. [Google Scholar] [CrossRef] [PubMed]
- Wiberg, S.; Mortensen, A.F.; Kjaergaard, J.; Hassager, C.; Wanscher, M. Accidental hypothermia in Denmark: A nationwide cohort study of incidence and outcome. BMJ Open 2021, 11, e046806. [Google Scholar] [CrossRef] [PubMed]
- PMC. Management of Hypothermia in Emergency Medicine. Available online: https://pmc.ncbi.nlm.nih.gov/articles/PMC10745126/ (accessed on 18 November 2024).
- HMP Global Learning Network. Intravascular Temperature Management (IVTM) Techniques for Therapeutic Hypothermia. Available online: https://www.hmpgloballearningnetwork.com/site/eplab/articles/intravascular-temperature-management-ivtm-techniques-therapeutic-hypothermia (accessed on 18 November 2024).
- Taylor, E.E.; Carroll, J.P.; Lovitt, M.A.; Petrey, L.B.; Gray, P.E.; Mastropieri, C.J.; Foreman, M.L. Active intravascular rewarming for hypothermia associated with traumatic injury: Early experience with a new technique. Bayl. Univ. Med. Cent. Proc. 2008, 21, 120–126. [Google Scholar] [CrossRef] [PubMed]
- ZOLL Medical Corporation. Thermogard XP. Available online: https://pdf.medicalexpo.com/pdf/zoll-medical-corporation/thermogard-xp/70628-158966.html (accessed on 18 November 2024).
- Sørensen, M.K.; Holmberg, M.; Thomsen, J.H.; et al. Intravascular temperature management techniques for therapeutic hypothermia in emergency settings. Scand. J. Trauma Resusc. Emerg. Med. 2020, 28, 42. [Google Scholar]
- Mayo Clinic Staff. Hypothermia. Mayo Clinic. Available online: https://www.mayoclinic.org/diseases-conditions/hypothermia/symptoms-causes/syc-20352682 (accessed on 1 December 2024).
- Zhang, X.; et al. Recent advances in clinical hypothermia applications. J. Clin. Med. 2023, 13, 4221. [Google Scholar]
- Oude Lansink-Hartgring, A.; van Minnen, O.; Vermeulen, K.M.; van den Bergh, W.M.; Dutch Extracorporeal Life Support Study Group. Hospital Costs of Extracorporeal Membrane Oxygenation in Adults: A systematic Review. Pharmacoecon. Open 2021, 5, 613–623. [Google Scholar] [CrossRef] [PubMed]
- NICE. Thermogard XP for Therapeutic Hypothermia After Cardiac Arrest. Available online: https://www.nice.org.uk/advice/mib37/resources/thermogard-xp-for-therapeutic-hypothermia-after-cardiac-arrest-63499110633925 (accessed on 1 December 2024).
- AAFP. Treatment and management of hypothermia in family medicine. Am. Fam. Physician 2019, 100, 680–685. [Google Scholar]

| Criteria | Intravascular Temperature Management (IVTM) | Extracorporeal Membrane Oxygenation (ECMO) |
|---|---|---|
| Main purpose | Intravascular temperature control for gradual rewarming | Extracorporeal life support and rewarming |
| Mechanism | Catheter inserted intravascularly to regulate temperature via fluid pefusion or heat exchange | Extracorporeal circuit that oxygenates and warms the blood |
| Indications | Severe hypothermia without cardiac arrest Hemodynamically stable patients | Severe hypothermia with cardiac arrest Multi-organ dysfunction |
| Contraindications | Absolute Severe systemic infections Severe thrombocytopenia or clotting disorders Allergy or intolerance to catheter materials Relative Severe hemodynamic instability Vascular obstuctions Extreme hypothermia with cardiac arrest | Absolute Irreversible terminal disease Severe clotting disorders Patients with severe contraindications for aticoagulation Relative Elderly patients Severe chronic conditions Uncontrolled active infections Extreme obesity |
| Limitations | Catheter-related issues (infection, thrombosis) Limited availability in some hospitals Limited effectiveness in cardiac arrest | Very high costs Requires advanced infrastructure Increased risk of complications (bleeding, infection) |
| Complications | Insertion site infections Thrombophlebitis Risk of vascular perforation | Systemic infection Severe bleeding Thrombosis in the circuit Mechanical device complications |
| Ideal cases of application | Isolated hypothermia without cardiac arrest Patients at risk of fluid overload | Hypothermia with cardiac arrest Severe organ dysfunction or urgent oxygenation needs |
| Availability | More commonly available in general hospitals | Available only in specialized centers and large hospitals |
| Costs | Significantly lower than ECMO | Extremely high, including equipment, personnel, consumables |
| Associated survival rates | Insufficient data to confirm | Associated with higher survival rates in severe cases |
| Nr. Crt. | Immediate Complications | Delayed Complications |
|---|---|---|
| Intravascular Temperature Management (IVTM) | Cardiac arrhythmias (ventricular fibrillation, ventricular tachycardia, bradycardia) Rewarming shock with severe hypotension Myocardial ischemia Rewarming syndrome: metabolic acidosis, hyperkalimia, hypoglycemia Cerebral edema Seizures Pulmonary edema: non-cardiogenic induced by rewarming; or cardiogenic secondary to heart failure Hypoventilation Acute renal failure associated with severe hypotension or rhabdomuolysis Coagulopathy-DIC Thrombembolism | Recurence of hypothermia Paradoxical hyperthermia—in aggresive rewarming Secondary infections/Nosocomial infections Multiple Organ Dysfunction Syndrome—due to reperfusion injury Persistent neurological symptoms Residual metabolic disorders: hypokalemia, hypomagnesemia, metabolic acidosis Post-hypothermia syndrome—chronic fatigue, confusion, anxiety, depression |
| Extracorporeal Membrane Oxygenation (ECMO) | Cardiac arrhythmias (ventricular fibrillation, ventricular tachycardia, bradycardia) Myocardial ischemia Arterial hypotension Pulmonary edema Atelectasis Cerebral edema Seizures Persistent coma Bleeding Thrombocytopenia Metabolic complications: hyperkalemia, metabolic acidosis Arterial or venous dissection Air embolism or thrombosis | Recurence of hypothermia Pneumonia Pulmonary fibrosis—prolonged inflammation or aggresive mechanical ventilation Catheter infection DIC Hemolytic anemia—due to cellular trauma related to blood passage through the ECMO Cognitive or motor deficits Stroke Chronic renal failure Post-intensive care syndrome Delayed rehabilitation |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oprita, B.; Olaru, I.; Botezatu, L.; Diaconu, A.E.; Oprita, R. Management of Severe Hypothermia: Challenges and Advanced Strategies. J. Clin. Med. 2025, 14, 1584. https://doi.org/10.3390/jcm14051584
Oprita B, Olaru I, Botezatu L, Diaconu AE, Oprita R. Management of Severe Hypothermia: Challenges and Advanced Strategies. Journal of Clinical Medicine. 2025; 14(5):1584. https://doi.org/10.3390/jcm14051584
Chicago/Turabian StyleOprita, Bogdan, Ionut Olaru, Liviu Botezatu, Alice Elena Diaconu, and Ruxandra Oprita. 2025. "Management of Severe Hypothermia: Challenges and Advanced Strategies" Journal of Clinical Medicine 14, no. 5: 1584. https://doi.org/10.3390/jcm14051584
APA StyleOprita, B., Olaru, I., Botezatu, L., Diaconu, A. E., & Oprita, R. (2025). Management of Severe Hypothermia: Challenges and Advanced Strategies. Journal of Clinical Medicine, 14(5), 1584. https://doi.org/10.3390/jcm14051584






