Refractive Error and Ocular Pathology of Children Examined in an Ophthalmological Practice in Moldova
Abstract
1. Background
2. Methods
2.1. Study Population and Recruitment
2.2. Data Collection
2.3. Data Analysis
2.4. Ethics
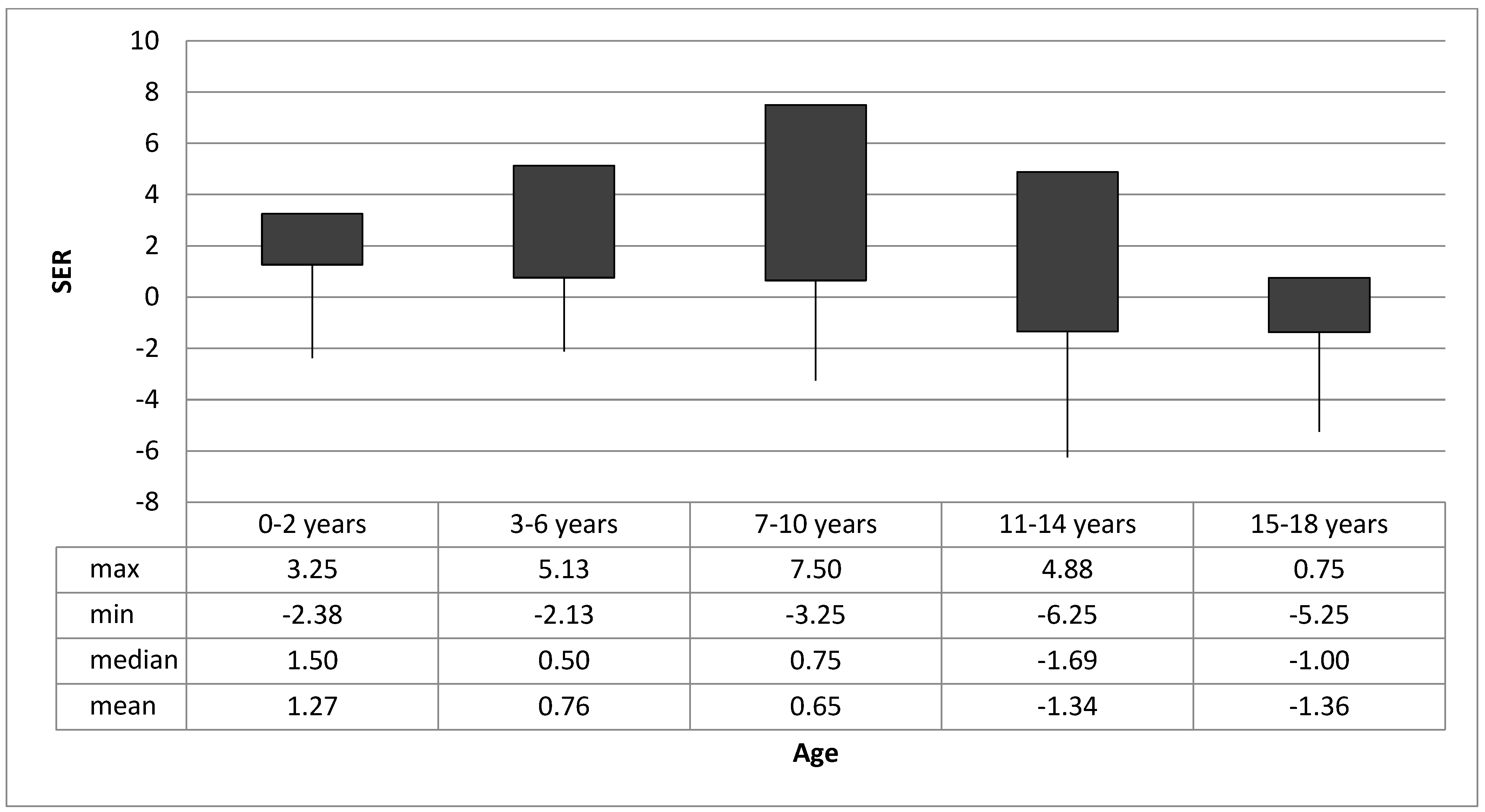
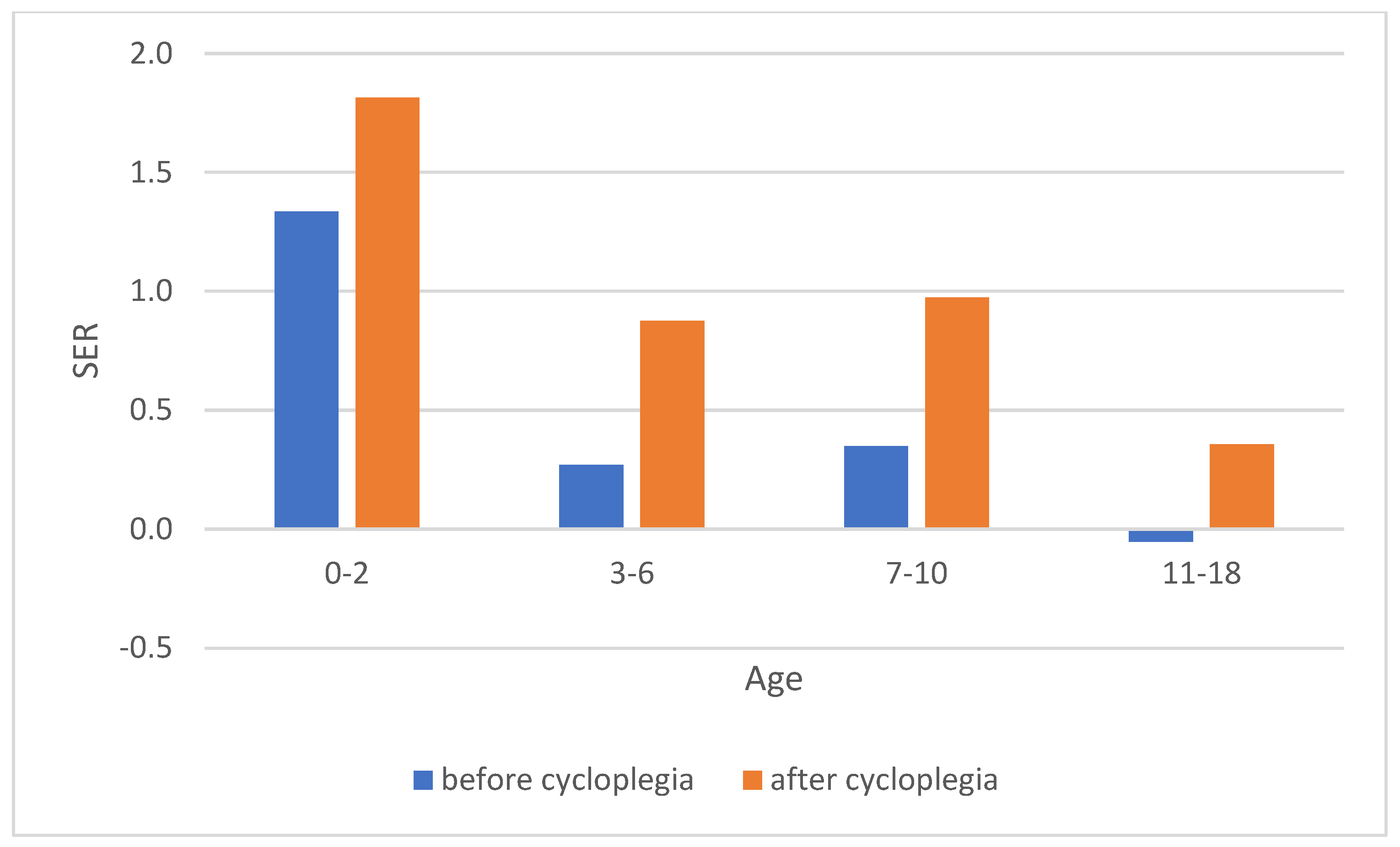
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dandona, R.; Dandona, L. Refractive error blindness. Bull. World Health Organ. 2001, 79, 237–243. [Google Scholar] [PubMed]
- Bourne, R.R.A.; Dineen, B.P.; Huq, D.M.N.; Ali, S.M.; Johnson, G.J. Correction of Refractive Error in the Adult Population of Bangladesh: Meeting the Unmet Need. Investig. Ophthalmol. Vis. Sci. 2004, 45, 410–417. [Google Scholar] [CrossRef] [PubMed]
- Skarzyński, H.; Piotrowska, A. Prevention of communication disorders-screening pre-school and school-age children for problems with hearing, vision and speech: European consensus statement. Med. Sci. Monit. 2012, 18, SR17–SR21. [Google Scholar] [CrossRef] [PubMed]
- Harrington, S.; Davison, P.A.; O’Dwyer, V. School performance and undetected and untreated visual problems in schoolchildren in Ireland; a population-based cross-sectional study. Ir. Educ. Stud. 2022, 41, 367–388. [Google Scholar] [CrossRef]
- Quaid, P.; Simpson, T. Association between reading speed, cycloplegic refractive error, and oculomotor function in reading disabled children versus controls. Graefe’s Arch. Clin. Exp. Ophthalmol. 2013, 251, 169–187. [Google Scholar] [CrossRef]
- Hagen, L.; Gilson, S.J.; Baraas, R.C. Vision status and reading test results in Norwegian adolescents. Scand. J. Optom. Vis. Sci. 2020, 13, 2–7. [Google Scholar] [CrossRef]
- Sankaridurg, P.; Tahhan, N.; Kandel, H.; Naduvilath, T.; Zou, H.; Frick, K.D.; Marmamula, S.; Friedman, D.S.; Lamoureux, E.; Keeffe, J.; et al. IMI Impact of Myopia. Investig. Ophthalmol. Vis. Sci. 2021, 62, 2. [Google Scholar] [CrossRef]
- Tideman, J.W.L.; Snabel, M.C.C.; Tedja, M.S.; van Rijn, G.A.; Wong, K.T.; Kuijpers, R.W.A.M.; Vingerling, J.R.; Hofman, A.; Buitendijk, G.H.S.; Keunen, J.E.E.; et al. Association of Axial Length With Risk of Uncorrectable Visual Impairment for Europeans With Myopia. JAMA Ophthalmol. 2016, 134, 1355–1363. [Google Scholar] [CrossRef]
- Colburn, J.D.; Morrison, D.G.; Estes, R.L.; Li, C.; Lu, P.; Donahue, S.P. Longitudinal follow-up of hypermetropic children identified during preschool vision screening. J. Am. Assoc. Pediatr. Ophthalmol. Strabismus 2010, 14, 211–215. [Google Scholar] [CrossRef]
- World Health Organization. Global Data on Visual Impairment; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- Vitale, S.; Ellwein, L.; Cotch, M.F.; Ferris, F.L., 3rd; Sperduto, R. Prevalence of refractive error in the United States, 1999–2004. Arch. Ophthalmol. 2008, 126, 1111–1119. [Google Scholar] [CrossRef]
- Fotedar, R.; Rochtchina, E.; Morgan, I.; Wang, J.J.; Mitchell, P.; Rose, K.A. Necessity of Cycloplegia for Assessing Refractive Error in 12-Year-Old Children: A Population-Based Study. Am. J. Ophthalmol. 2007, 144, 307–309. [Google Scholar] [CrossRef] [PubMed]
- Zadnik, K.; Manny, R.E.; Yu, J.A.; Mitchell, G.L.; Cotter, S.A.; Quiralte, J.C.; Shipp, M.D.; Friedman, N.E.; Kleinstein, R.N.; Walker, T.W.; et al. Ocular component data in schoolchildren as a function of age and gender. Optom. Vis. Sci. 2003, 80, 226–236. [Google Scholar] [CrossRef] [PubMed]
- Pan, C.W.; Dirani, M.; Cheng, C.Y.; Wong, T.Y.; Saw, S.M. The age-specific prevalence of myopia in Asia: A meta-analysis. Optom. Vis. Sci. 2015, 92, 258–266. [Google Scholar] [CrossRef] [PubMed]
- Hagen, L.; Gjelle, J.V.B.; Arnegard, S.; Pedersen, H.; Gilson, S.; Baraas, R. Prevalence and Possible Factors of Myopia in Norwegian Adolescents. Sci. Rep. 2018, 8, 13479. [Google Scholar] [CrossRef]
- Demir, P.; Baskaran, K.; Theagarayan, B.; Gierow, P.; Sankaridurg, P.; Macedo, A.F. Refractive error, axial length, environmental and hereditary factors associated with myopia in Swedish children. Clin. Exp. Optom. 2021, 104, 595–601. [Google Scholar] [CrossRef]
- Teikari, J.M.; O’Donnell, J.; Kaprio, J.; Koskenvuo, M. Impact of Heredity in Myopia. Hum. Hered. 1991, 41, 151–156. [Google Scholar] [CrossRef]
- Hammond, C.J.; Snieder, H.; Gilbert, C.E.; Spector, T.D. Genes and environment in refractive error: The twin eye study. Investig. Ophthalmol. Vis. Sci. 2001, 42, 1232–1236. [Google Scholar]
- Morgan, I.G.; Wu, P.-C.; Ostrin, L.A.; Tideman, J.W.L.; Yam, J.C.; Lan, W.; Baraas, R.C.; He, X.; Sankaridurg, P.; Saw, S.-M.; et al. IMI Risk Factors for Myopia. Investig. Ophthalmol. Vis. Sci. 2021, 62, 3. [Google Scholar] [CrossRef]
- Dirani, M.; Crowston, J.G.; Wong, T.Y. From reading books to increased smart device screen time. Br. J. Ophthalmol. 2019, 103, 1–2. [Google Scholar] [CrossRef]
- Németh, J.; Tapasztó, B.; Aclimandos, W.A.; Kestelyn, P.; Jonas, J.B.; De Faber, J.-T.H.N.; Januleviciene, I.; Grzybowski, A.; Nagy, Z.Z.; Pärssinen, O.; et al. Update and guidance on management of myopia. European Society of Ophthalmology in cooperation with International Myopia Institute. Eur. J. Ophthalmol. 2021, 31, 853–883. [Google Scholar] [CrossRef]
- Fan, Q.; Verhoeven, V.J.M.; Wojciechowski, R.; Barathi, V.A.; Hysi, P.G.; Guggenheim, J.A.; Höhn, R.; Vitart, V.; Khawaja, A.P.; Yamashiro, K.; et al. Meta-analysis of gene–environment-wide association scans accounting for education level identifies additional loci for refractive error. Nat. Commun. 2016, 7, 11008. [Google Scholar] [CrossRef] [PubMed]
- Harb, E.N.; Wildsoet, C.F. Origins of Refractive Errors: Environmental and Genetic Factors. Annu. Rev. Vis. Sci. 2019, 5, 47–72. [Google Scholar] [CrossRef] [PubMed]
- Bourne, R.R.A.; Flaxman, S.R.; Braithwaite, T.; Cicinelli, M.V.; Das, A.; Jonas, J.B.; Keeffe, J.; Kempen, J.H.; Kempen, J.; Kempen, H.; et al. Magnitude, temporal trends, and projections of the global prevalence of blindness and distance and near vision impairment: A systematic review and meta-analysis. Lancet Global Health 2017, 5, e888–e897. [Google Scholar] [CrossRef]
- Zatic, T.; Bendelic, E.; Paduca, A.; Rabiu, M.; Corduneanu, A.; Garaba, A.; Novac, V.; Curca, C.; Sorbala, I.; Chiaburu, A.; et al. Rapid assessment of avoidable blindness and diabetic retinopathy in Republic of Moldova. Br. J. Ophthalmol. 2015, 99, 832–836. [Google Scholar] [CrossRef]
- Ministry of Health. Retinopatia Prematurului 2017. Available online: https://ms.gov.md/wp-content/uploads/2020/07/15498-PCN-22620Retinopatia20prematurului.pdf (accessed on 17 February 2025).
- Ministry of Health. Cataracta la Copil 2017. Available online: https://ms.gov.md/wp-content/uploads/2020/07/15496-PCN-5220Cataracta20la20copil.pdf (accessed on 17 February 2025).
- Ministry of Health. Strabismul la Copil 2017. Available online: https://ms.gov.md/wp-content/uploads/2020/07/15493-PCN-4320Strabismul20la20copil.pdf (accessed on 17 February 2025).
- Leat, S.J. To prescribe or not to prescribe? Guidelines for spectacle prescribing in infants and children. Clin. Exp. Optom. 2011, 94, 514–527. [Google Scholar] [CrossRef]
- Morgan, I.G.; Rose, K.A.; Ellwein, L.B.; Refractive Error Study in Children Survey Group. Is emmetropia the natural endpoint for human refractive development? An analysis of population-based data from the refractive error study in children (RESC). Acta Ophthalmol. 2010, 88, 877–884. [Google Scholar] [CrossRef]
- Armstrong, R.A. Statistical guidelines for the analysis of data obtained from one or both eyes. Ophthalmic Physiol. Opt. 2013, 33, 7–14. [Google Scholar] [CrossRef]
- World Health Organization. ICD-10: International Statistical Classification of Diseases and Related Health Problems: Tenth Revision, 2nd ed.; World Health Organization: Geneva, Switzerland, 2004. [Google Scholar]
- Grzybowski, A.; Kanclerz, P.; Tsubota, K.; Lanca, C.; Saw, S.-M. A review on the epidemiology of myopia in school children worldwide. BMC Ophthalmol. 2020, 20, 27. [Google Scholar] [CrossRef]
- Matsumura, S.; Ching-Yu, C.; Saw, S.-M. Global Epidemiology of Myopia. In Updates on Myopia: A Clinical Perspective; Ang, M., Wong, T.Y., Eds.; Springer: Singapore, 2020; pp. 27–51. [Google Scholar]
- Tedja, M.S.; Haarman, A.E.G.; Meester-Smoor, M.A.; Kaprio, J.; Mackey, D.A.; Guggenheim, J.A.; Hammond, C.J.; Verhoeven, V.J.M.; Klaver, C.C.W.; the CREAM Consortium. IMI-Myopia Genetics Report. Investig. Ophthalmol. Vis. Sci. 2019, 60, M89–M105. [Google Scholar] [CrossRef]
- Czepita, M.; Czepita, D.; Safranow, K. Role of Gender in the Prevalence of Myopia among Polish Schoolchildren. J. Ophthalmol. 2019, 2019, 9748576. [Google Scholar] [CrossRef]
- Hagen, L.A.; Arnegard, S.; Kuchenbecker, J.A.; Gilson, S.J.; Neitz, M.; Neitz, J.; Baraas, R.C. The association between L:M cone ratio, cone opsin genes and myopia susceptibility. Vis. Res. 2019, 162, 20–28. [Google Scholar] [CrossRef] [PubMed]
- Wu, L.J.; You, Q.S.; Duan, J.L.; Luo, Y.X.; Liu, L.J.; Li, X.; Gao, Q.; Zhu, H.P.; He, Y.; Xu, L.; et al. Prevalence and associated factors of myopia in high-school students in Beijing. PLoS ONE 2015, 10, e0120764. [Google Scholar] [CrossRef] [PubMed]
- Hashemi, H.; Rezvan, F.; Beiranvand, A.; Papi, O.-A.; Hoseini-Yazdi, H.; Ostadimoghaddam, H.; Yekta, A.A.; Norouzirad, R.; Khabazkhoob, M. Prevalence of Refractive Errors among High School Students in Western Iran. J. Ophthalmic Vis. Res. 2014, 9, 232–239. [Google Scholar]
- Rose, K.A.; Morgan, I.G.; Smith, W.; Burlutsky, G.; Mitchell, P.; Saw, S.M. Myopia, lifestyle, and schooling in students of Chinese ethnicity in Singapore and Sydney. Arch. Ophthalmol. 2008, 126, 527–530. [Google Scholar] [CrossRef]
- Rudnicka, A.R.; Kapetanakis, V.V.; Wathern, A.K.; Logan, N.S.; Gilmartin, B.; Whincup, P.H.; Cook, D.G.; Owen, C.G. Global variations and time trends in the prevalence of childhood myopia, a systematic review and quantitative meta-analysis: Implications for aetiology and early prevention. Br. J. Ophthalmol. 2016, 100, 882–890. [Google Scholar] [CrossRef]
- Resnikoff, S.; Jonas, J.B.; Friedman, D.; He, M.; Jong, M.; Nichols, J.J.; Ohno-Matsui, K.; Smith, E.L., III; Wildsoet, C.F.; Taylor, H.R.; et al. Myopia—A 21st Century Public Health Issue. Investig. Ophthalmol. Vis. Sci. 2019, 60, Mi–Mii. [Google Scholar] [CrossRef]
- Rao, G.N.; Sabnam, S.; Pal, S.; Rizwan, H.; Thakur, B.; Pal, A. Prevalence of ocular morbidity among children aged 17 years or younger in the eastern India. Clin. Ophthalmol. 2018, 12, 1645–1652. [Google Scholar] [CrossRef]
- Totuk, O.; Kabadayı, K.; Ekizoğlu, N.; Arici, T. Prevalence of Childhood Eye Diseases. Turk. Klin. Pediatri. 2018, 27, 111–117. [Google Scholar]
- Yazdani, N.; Sadeghi, R.; Momeni-Moghaddam, H.; Zarifmahmoudi, L.; Ehsaei, A. Comparison of cyclopentolate versus tropicamide cycloplegia: A systematic review and meta-analysis. J. Optom. 2018, 11, 135–143. [Google Scholar] [CrossRef]
- Buckingham, T. Visual Problems in Childhood; Butterworth-Heinemann: Oxford, UK; Boston, MA, USA, 1993. [Google Scholar]
- Pei, R.; Liu, Z.; Rong, H.; Zhao, L.; Du, B.; Jin, N.; Zhang, H.; Wang, B.; Pang, Y.; Wei, R. A randomized clinical trial using cyclopentolate and tropicamide to compare cycloplegic refraction in Chinese young adults with dark irises. BMC Ophthalmol. 2021, 21, 256. [Google Scholar] [CrossRef]
- Morgan, I.G.; Iribarren, R.; Fotouhi, A.; Grzybowski, A. Cycloplegic refraction is the gold standard for epidemiological studies. Acta Ophthalmol. 2015, 93, 581–585. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.-Y.; Wei, S.-F.; Li, S.-M.; Hu, J.-P.; Yang, X.-H.; Cao, K.; Lin, C.-X.; Du, J.-L.; Guo, J.-Y.; Li, H.; et al. Cycloplegic refraction by 1% cyclopentolate in young adults: Is it the gold standard? The Anyang University Students Eye Study (AUSES). Br. J. Ophthalmol. 2019, 103, 654–658. [Google Scholar] [CrossRef] [PubMed]
| N | SER ≤ −0.5 | −0.50 D < SER < +0.50 D | +0.50 D ≤ SER < +3.00 D | SER ≥ +3.0 | |
|---|---|---|---|---|---|
| All | 177 | 42 (24%) [0.18–0.31] | 21 (12%) [0.08–0.18] | 107 (60%) [0.53–0.68] | 7 (4%) [0.02–0.08] |
| 0–2 years | 47 | 4 (9%) [0.02–0.20] | 8 (17%) [0.08–0.31] | 34 (72%) [0.57–0.84] | 1 (2%) [0.00–0.11] |
| 3–6 years | 64 | 5 (8%) [0.03–0.17] | 11 (17%) [0.09–0.29] | 46 (72%) [0.59–0.82] | 2 (3%) [0.00–0.11] |
| 7–18 years | 66 | 33 (50%) [0.37–0.63] | 2 (3%) [0.00–0.11] | 27 (41%) [0.29–0.54] | 4 (6%) [0.02–0.15] |
| 7–10 years | 40 | 12 (30%) [0.17–0.47] | 2 (5%) [0.01–0.17] | 23 (58%) [0.41–0.73] | 3 (7%) [0.02–0.20] |
| 11–14ars | 16 | 13 (81%) [0.54–0.96] | 0 | 2 (13%) [0.02–0.38] | 1 (6%) [0.00–0.30] |
| 15–18 years | 10 | 8 (80%) [0.44–0.97] | 0 | 2 (20%) [0.03–0.57] | 0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ziziuchin, V.; Horgen, G.; Sundling, V. Refractive Error and Ocular Pathology of Children Examined in an Ophthalmological Practice in Moldova. J. Clin. Med. 2025, 14, 1554. https://doi.org/10.3390/jcm14051554
Ziziuchin V, Horgen G, Sundling V. Refractive Error and Ocular Pathology of Children Examined in an Ophthalmological Practice in Moldova. Journal of Clinical Medicine. 2025; 14(5):1554. https://doi.org/10.3390/jcm14051554
Chicago/Turabian StyleZiziuchin, Veronica, Gro Horgen, and Vibeke Sundling. 2025. "Refractive Error and Ocular Pathology of Children Examined in an Ophthalmological Practice in Moldova" Journal of Clinical Medicine 14, no. 5: 1554. https://doi.org/10.3390/jcm14051554
APA StyleZiziuchin, V., Horgen, G., & Sundling, V. (2025). Refractive Error and Ocular Pathology of Children Examined in an Ophthalmological Practice in Moldova. Journal of Clinical Medicine, 14(5), 1554. https://doi.org/10.3390/jcm14051554






