Does Corpus Luteum Doppler Have a Role in Prognostic Prediction for Outcome with Threatened Abortion?
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Participants
2.3. Ultrasonography and Doppler Study Protocol
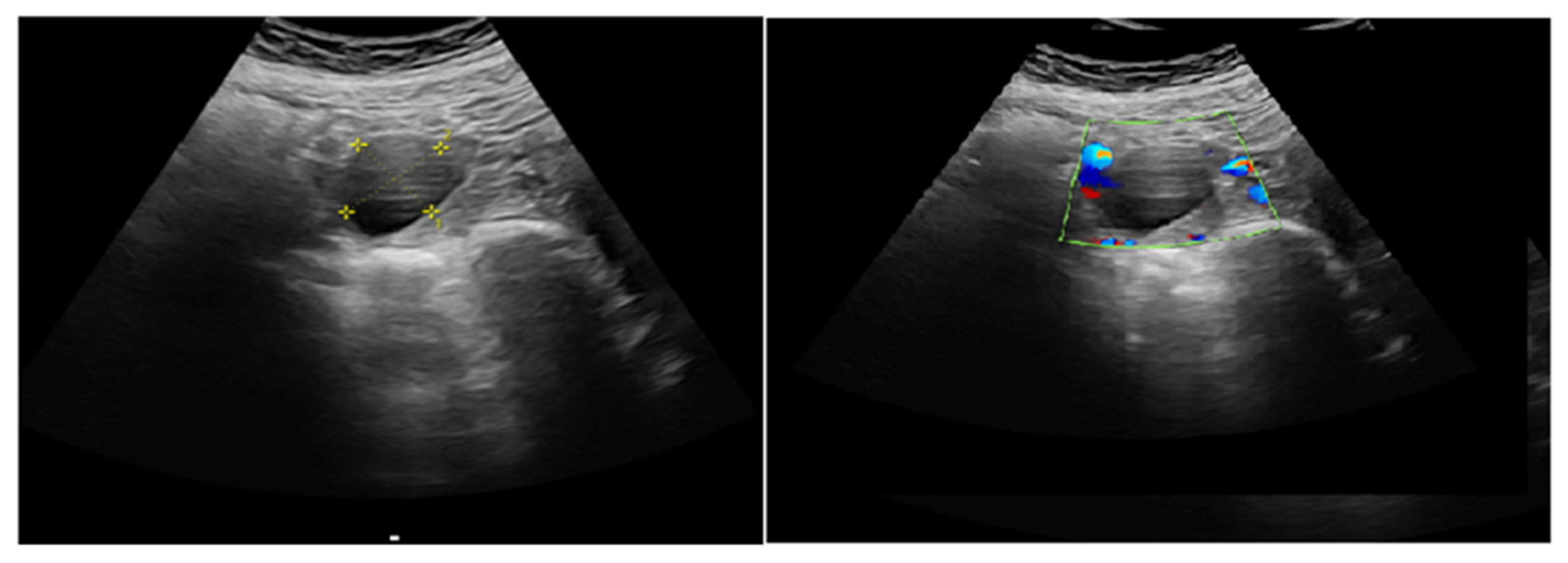
2.3.1. Corpus Luteum (CL) Localization and Identification
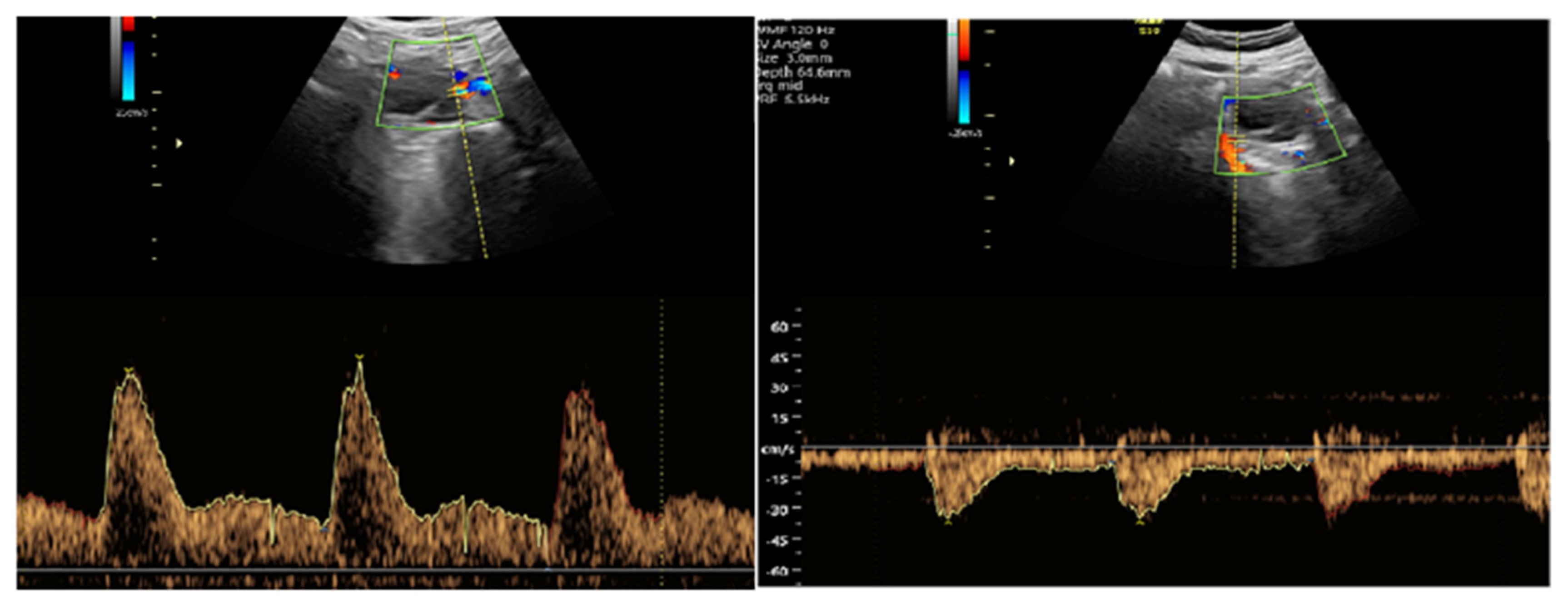
2.3.2. Doppler Measurement Procedure
- S/D ratio (Systolic/Diastolic ratio)
- RI (Resistance Index)
- PI (Pulsatility Index)
2.3.3. Measurement Standards and Bias Reduction Strategies
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AUC | Area Under Curve |
| BMI | Body Mass Index |
| CL | Corpus Luteum |
| CRL | Crown-Rump Length |
| hCG | Human Chorionic Gonadotropin |
| PI | Pulsatility Index |
| RI | Resistance Index |
| ROC | Receiver Operating Characteristics |
| S/D | Systole/Diastole Ratio |
References
- Bloom, S.L.; Corton, M.M.; Spong, C.Y.; Dashe, J.S.; Leveno, K.J. Williams Obstetrics 24/E; McGraw-Hill Education: New York, NY, USA, 2014. [Google Scholar]
- Hanita, O.; Roslina, O.; Azlin, M.I.N. Maternal level of pregnancy-associated plasma protein A as a predictor of pregnancy failure in threatened abortion. Malays. J. Pathol. 2012, 34, 145–151. [Google Scholar] [PubMed]
- Wijesiriwardana, A.; Bhattacharya, S.; Shetty, A.; Smith, N.; Bhattacharya, S. Obstetric outcome in women with threatened miscarriage in the first trimester. Obstet. Gynecol. 2006, 107, 557–562. [Google Scholar] [CrossRef]
- Oates, J.; Casikar, I.; Campain, A.; Müller, S.; Yang, J.; Reid, S.; Condous, G. A prediction model for viability at the end of the first trimester after a single early pregnancy evaluation. Aust. N. Z. J. Obstet. Gynaecol. 2013, 53, 51–57. [Google Scholar] [CrossRef]
- Pearlstone, M.; Baxi, L. Subchorionic hematoma: A review. Obstet. Gynecol. Surv. 1993, 48, 65–68. [Google Scholar] [CrossRef]
- Maso, G.; D’Ottavio, G.; De Seta, F.; Sartore, A.; Piccoli, M.; Mandruzzato, G. First-trimester intrauterine hematoma and outcome of pregnancy. Obstet. Gynecol. 2005, 105, 339–344. [Google Scholar] [CrossRef]
- Børlum, K.G.; Thomsen, A.; Clausen, I.; Eriksen, G. Long-term prognosis of pregnancies in women with intrauterine hematomas. Obstet. Gynecol. 1989, 74, 231–233. [Google Scholar] [PubMed]
- Tuuli, M.G.; Norman, S.M.; Odibo, A.O.; Macones, G.A.; Cahill, A.G. Perinatal outcomes in women with subchorionic hematoma: A systematic review and meta-analysis. Obstet. Gynecol. 2011, 117, 1205–1212. [Google Scholar] [CrossRef] [PubMed]
- Aboelwan, Y.; Abd Elsalam, W.A.A.; Hamed, B.M.; Mohamed, Z. Doppler Ultrasound Assessment in Women with Threatened Abortion. Zagazig Univ. Med. J. 2022, 28, 145–151. [Google Scholar] [CrossRef]
- Balıkoğlu, M.; Bayraktar, B.; Yurtkul, A.A.; Özeren, M. The Effect of Vaginal Bleeding in Early Pregnancy on First Trimester Screening Test, Uterine Artery Doppler Indices and Perinatal Outcomes. Med. Rec. 2023, 5, 393–399. [Google Scholar] [CrossRef]
- Jaffe, R.; Dorgan, A.; Abramowicz, J.S. Color Doppler imaging of the uteroplacental circulation in the first trimester: Value in predicting pregnancy failure or complication. AJR Am. J. Roentgenol. 1995, 164, 1255–1258. [Google Scholar] [CrossRef][Green Version]
- Pellizzari, P.; Pozzan, C.; Marchiori, S.; Zen, T.; Gangemi, M. Assessment of uterine artery blood flow in normal first-trimester pregnancies and in those complicated by uterine bleeding. Ultrasound Obstet. Gynecol. 2002, 19, 366–370. [Google Scholar] [CrossRef] [PubMed]
- Durfee, S.M.; Frates, M.C. Sonographic spectrum of the corpus luteum in early pregnancy: Gray-scale, color, and pulsed Doppler appearance. J. Clin. Ultrasound 1999, 27, 55–59. [Google Scholar] [CrossRef]
- Takasaki, A.; Tamura, H.; Taniguchi, K.; Asada, H.; Taketani, T.; Matsuoka, A.; Yamagata, Y.; Shimamura, K.; Morioka, H.; Sugino, N. Luteal blood flow and luteal function. J. Ovarian Res. 2009, 2, 1. [Google Scholar] [CrossRef]
- Tamanini, C.; De Ambrogi, M. Angiogenesis in developing follicle and corpus luteum. Reprod. Domest. Anim. 2004, 39, 206–216. [Google Scholar] [CrossRef] [PubMed]
- Pillai, R.N.; Konje, J.C.; Tincello, D.G.; Potdar, N. Role of serum biomarkers in the prediction of outcome in women with threatened miscarriage: A systematic review and diagnostic accuracy meta-analysis. Hum. Reprod. Update 2016, 22, 228–239. [Google Scholar] [CrossRef]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coef-ficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Baba, S.; Noda, H.; Nakayama, M.; Waguri, M.; Mitsuda, N.; Iso, H. Risk factors of early spontaneous abortions among Japanese: A matched case-control study. Hum. Reprod. 2011, 26, 466–472. [Google Scholar] [CrossRef]
- Shah, D.; Nagarajan, N. Luteal insufficiency in first trimester. Indian. J. Endocrinol. Metab. 2013, 17, 44–49. [Google Scholar] [CrossRef]
- Dinelli, L.; Courbière, B.; Achard, V.; Jouve, E.; Deveze, C.; Gnisci, A.; Grillo, J.M.; Paulmyer-Lacroix, O. Prognosis factors of pregnancy after intrauterine insemination with the husband’s sperm: Conclusions of an analysis of 2,019 cycles. Fertil. Steril. 2014, 101, 994–1000. [Google Scholar] [CrossRef]
- Şükür, Y.E.; Göç, G.; Köse, O.; Açmaz, G.; Özmen, B.; Atabekoğlu, C.S.; Koç, A.; Söylemez, F. The effects of subchorionic hematoma on pregnancy outcome in patients with threatened abortion. J. Turk. Ger. Gynecol. Assoc. 2014, 15, 239–242. [Google Scholar] [CrossRef]
- Ball, R.H.; Ade, C.M.; Schoenborn, J.A.; Crane, J.P. The clinical significance of ultransonographically detected subchorionic hemorrhages. Am. J. Obstet. Gynecol. 1996, 174, 996–1002. [Google Scholar] [CrossRef] [PubMed]
- Nagy, S.; Bush, M.; Stone, J.; Lapinski, R.H.; Gardó, S. Clinical significance of subchorionic and retroplacental hematomas detected in the first trimester of pregnancy. Obstet. Gynecol. 2003, 102, 94–100. [Google Scholar] [CrossRef]
- Alcázar, J.L.; Laparte, C.; López-Garcia, G. Corpus luteum blood flow in abnormal early pregnancy. J. Ultrasound Med. 1996, 15, 645–649. [Google Scholar] [CrossRef] [PubMed]
- Mäkikallio, K.; Tekay, A.; Jouppila, P. Effects of bleeding on uteroplacental, umbilicoplacental and yolk-sac hemodynamics in early pregnancy. Ultrasound Obstet. Gynecol. 2001, 18, 352–356. [Google Scholar] [CrossRef] [PubMed]
- Alcázar, J.L.; Ruiz-Perez, M.L. Uteroplacental circulation in patients with first-trimester threatened abortion. Fertil. Steril. 2000, 73, 130–135. [Google Scholar] [CrossRef]
- Jauniaux, E.; Johns, J.; Burton, G.J. The role of ultrasound imaging in diagnosing and investigating early pregnancy failure. Ultrasound Obstet. Gynecol. 2005, 25, 613–624. [Google Scholar] [CrossRef]
- El-mashad, A.I.; Mohamed, M.A.; Farag, M.A.E.; Ahmad, M.K.; Ismail, Y. Role of uterine artery Doppler velocimetry indices and plasma adrenomedullin level in women with unexplained recurrent pregnancy loss. J. Obstet. Gynaecol. Res. 2011, 37, 51–57. [Google Scholar] [CrossRef]
- Mansour, G.M.; Hussein, S.H.; Abd El Hady, R.M.; Mohammed, H.F.; Abd El Gawad, M.M.; Abou Gabal, A.I.; Al-Awadhy, R.M.; El Saied, M. Uterine artery flow velocity waveform (FVW) type and subednometrial vascularity in recurrent pregnancy loss. J. Matern.-Fetal Neonatal Med. 2020, 33, 527–532. [Google Scholar] [CrossRef]
- Kang, X.; Wang, T.; He, L.; Xu, H.; Liu, Z.; Zhao, A. Effect of Low-Dose Aspirin on Midluteal Phase Uterine Artery Blood Flow in Patients with Recurrent Pregnancy Loss. J. Ultrasound Med. 2016, 35, 2583–2587. [Google Scholar] [CrossRef]
- Zhong, Y.; Wang, N.; Lu, S.; Lu, Y.; Pan, X.; Zhou, Y. Doppler Evaluation of Uterine Blood Flow in Patients with Unexplained Recurrent Pregnancy Loss. Int. J. Womens Health 2024, 16, 1803–1814. [Google Scholar] [CrossRef]
- Shehata, N.A.A.; Ali, H.A.A.; Hassan, A.E.G.M.A.; Katta, M.A.; Ali, A.S.F. Doppler and biochemical assessment for the prediction of early pregnancy outcome in patients experiencing threatened spontaneous abortion. Int. J. Gynaecol. Obstet. 2018, 143, 150–155. [Google Scholar] [CrossRef] [PubMed]
- Applebaum, M. Corpus luteum blood flow in normal and abnormal early pregnancy: Evaluation with transvaginal color and pulsed Doppler sonography. J. Ultrasound Med. 1995, 14, 756. [Google Scholar] [CrossRef]
- Kalogirou, D.; Antoniou, G.; Botsis, D.; Kontoravdis, A.; Vitoratos, N.; Giannikos, L. Transvaginal Doppler ultrasound with color flow imaging in the diagnosis of luteal phase defect (LPD). Clin. Exp. Obstet. Gynecol. 1997, 24, 95–97. [Google Scholar]
- Han, H.; Mo, X.; Ma, Y.; Zhou, Y.; Zhang, B. The Role of Blood Flow in Corpus Luteum Measured by Transvaginal Two-Dimensional and Three-Dimensional Ultrasound in the Prediction of Early Intrauterine Pregnancy Outcomes. Front. Pharmacol. 2019, 10, 767. [Google Scholar] [CrossRef]
- Blavier, F.; Faron, G.; Cools, W.; Blockeel, C.; Santos-Ribeiro, S.; Done, E.; Ranisavljevic, N.; Rayssiguier, R.; Fuchs, F.; Gucciardo, L. Corpus luteum score, a simple Doppler examination to prognose early pregnancies. Eur. J. Obstet. Gynecol. Reprod. Biol. 2021, 258, 324–331. [Google Scholar] [CrossRef]
- Tamura, H.; Takasaki, A.; Taniguchi, K.; Matsuoka, A.; Shimamura, K.; Sugino, N. Changes in blood-flow impedance of the human corpus luteum throughout the luteal phase and during early pregnancy. Fertil. Steril. 2008, 90, 2334–2339. [Google Scholar] [CrossRef]
- Lek, S.M.; Ku, C.W.; Allen, J.C.; Malhotra, R.; Tan, N.S.; Østbye, T.; Tan, T.C. Validation of serum progesterone <35nmol/L as a predictor of miscarriage among women with threatened miscarriage. BMC Pregnancy Childbirth 2017, 17, 78. [Google Scholar] [CrossRef]
- Johns, J.; Muttukrishna, S.; Lygnos, M.; Groome, N.; Jauniaux, E. Maternal serum hormone concentrations for prediction of adverse outcome in threatened miscarriage. Reprod. Biomed. Online 2007, 15, 413–421. [Google Scholar] [CrossRef]
- Ku, C.W.; Allen, J.C.; Lek, S.M.; Chia, M.L.; Tan, N.S.; Tan, T.C. Serum progesterone distribution in normal pregnancies compared to pregnancies complicated by threatened miscarriage from 5 to 13 weeks gestation: A prospective cohort study. BMC Pregnancy Childbirth 2018, 18, 360. [Google Scholar] [CrossRef]

| Variables | Abortus Imminens Without Subchorionic Bleeding Area n = 120 | Abortus Imminens with Subchorionic Bleeding Area n = 60 | p |
|---|---|---|---|
| Age median (q1–q3) | 27 (24–29) | 26 (23–31) | 0.803 Φ |
| BMI (kg/m2) median (q1–q3) | 27.8 (23.5–31.3) | 27.1 (24.5–30.0) | 0.468 Φ |
| Gravida median (q1–q3) | 2 (1–3) | 2 (1–3) | 0.165 Φ |
| Parity median (q1–q3) | 0 (0–1) | 1 (0–1) | 0.388 Φ |
| Gestational week (according to ultrasound) median (q1–q3) | 8 (6–10) | 8 (7–9) | 0.731 Φ |
| Ectopic pregnancy history median (q1–q3) | 0 (0–0) | 0 (0–0) | 0.086 Φ |
| TSH median (q1–q3) | 1.40 (1.10–2.78) | 1.59 (1.16–1.96) | 0.818 Φ |
| Variables | Pregnant Women Who Have Abortıon in the First Trımester n = 44 | Those Who Contınue Theır Pregnancy in the Second Trımester n = 136 | p |
|---|---|---|---|
| Age median (q1–q3) | 26 (24–30) | 27 (24–30) | 0.989 Φ |
| BMI (kg/m2) median (q1–q3) | 26.8 (23.3–28.8) | 28.0 (24.2–31.2) | 0.076 Φ |
| Gravida median (q1–q3) | 2 (1–4) | 2 (1–3) | 0.465 Φ |
| Parity median (q1–q3) | 1 (0–1) | 0 (0–1) | 0.087 Φ |
| Gestational week (according to ultrasound) median (q1–q3) | 7 (6–9) | 9 (7–10) | 0.061 Φ |
| Ectopic pregnancy history median (q1–q3) | 0 (0–0) | 0 (0–0) | 0.158 Φ |
| TSH median (q1–q3) | 1.50 (1.23–1.70) | 1.48 (1.08–2.78) | 0.799 Φ |
| Variables | Pregnant Women Who Have an Abortıon in the First Trımester n = 44 | Those Who Contınue Their Pregnancy in the Second Trımester n = 136 | p |
|---|---|---|---|
| CL S/D ratio | 3.64 (2.92–4.23) | 2.21 (1.98–2.93) | <0.001 Φ |
| CL PI | 1.28 (1.10–1.52) | 0.82 (0.73–0.98) | <0.001 Φ |
| CL RI | 0.75 (0.65–0.92) | 0.54 (0.47–0.64) | <0.001 Φ |
| Variables | Abortus imminens without subchorionic bleeding area n = 120 | Abortus imminens with subchorionic bleeding area n = 60 | p |
| CL S/D ratio | 2.13 (1.92–2.82) | 3.07 (2.82–3.92) | <0.001 Φ |
| CL PI | 0.80 (0.68–1.08) | 1.11 (0.87–1.32) | <0.001 Φ |
| CL RI | 0.53 (0.43–0.67) | 0.68 (0.56–0.78) | <0.001 Φ |
| Variables | Pregnant Women with Subchorionic Bleeding Areas and Who Abort in the First Trimester n = 18 | Continuing Pregnancy into the 2nd Trimester with a Subchorionic Bleeding Area n = 42 | p |
|---|---|---|---|
| CL S/D ratio | 3.98 (3.70–4.28) | 2.97 (2.61–3.20) | <0.001 Φ |
| CL PI | 1.32 (1.13–1.52) | 0.98 (0.82–1.23) | 0.001 Φ |
| CL RI | 0.75 (0.67–0.86) | 0.60 (0.52–0.71) | 0.001 Φ |
| Variables | Pregnant women who have no subchorionic bleeding area and who abort in the first trimester n = 26 | Continuing pregnancy into the 2nd trimester without a subchorionic bleeding area n = 94 | p |
| CL S/D ratio | 3.01 (2.55–4.12) | 2.12 (1.92–2.36) | <0.001 Φ |
| CL PI | 1.26 (0.94–1.48) | 0.76 (0.67–0.87) | <0.001 Φ |
| CL RI | 0.74 (0.47–0.98) | 0.53 (0.42–0.61) | <0.001 Φ |
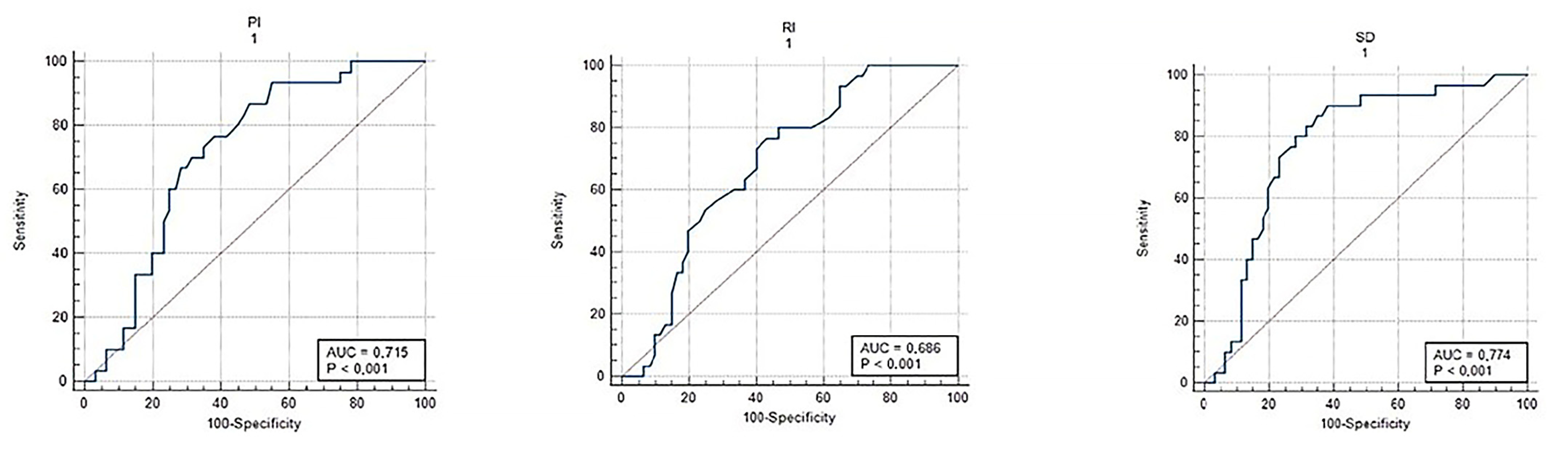
| Variables | AUC | 95% CI | Cut-Off | p | Sensitivite | Spesifite |
|---|---|---|---|---|---|---|
| Abortus imminens with subchorionic bleeding area | ||||||
| S/D | 0.774 | 0.705–0.833 | >2.27 | <0.001 | 90 | 62 |
| PI | 0.715 | 0.643–0.780 | >0.76 | <0.001 | 93 | 45 |
| RI | 0.686 | 0.613–0.753 | >0.53 | <0.001 | 80 | 53 |
| Pregnant women who have abortıon ın the First trımester | ||||||
| S/D | 0.767 | 0.698–0.826 | >2.87 | <0.001 | 77 | 75 |
| PI | 0.761 | 0.692–0.822 | >0.93 | <0.001 | 86 | 74 |
| RI | 0.768 | 0.699–0.827 | >0.62 | <0.001 | 77 | 75 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aktemur, G.; Tokgöz Çakır, B.; Sucu, S.; Karabay, G.; Şeyhanlı, Z.; Vanlı Tonyalı, N.; Diktaş, E.G.; Ünsal, M.; Erkaya, S. Does Corpus Luteum Doppler Have a Role in Prognostic Prediction for Outcome with Threatened Abortion? J. Clin. Med. 2025, 14, 1419. https://doi.org/10.3390/jcm14051419
Aktemur G, Tokgöz Çakır B, Sucu S, Karabay G, Şeyhanlı Z, Vanlı Tonyalı N, Diktaş EG, Ünsal M, Erkaya S. Does Corpus Luteum Doppler Have a Role in Prognostic Prediction for Outcome with Threatened Abortion? Journal of Clinical Medicine. 2025; 14(5):1419. https://doi.org/10.3390/jcm14051419
Chicago/Turabian StyleAktemur, Gizem, Betül Tokgöz Çakır, Sadun Sucu, Gülşan Karabay, Zeynep Şeyhanlı, Nazan Vanlı Tonyalı, Elif Gülşah Diktaş, Mehmet Ünsal, and Salim Erkaya. 2025. "Does Corpus Luteum Doppler Have a Role in Prognostic Prediction for Outcome with Threatened Abortion?" Journal of Clinical Medicine 14, no. 5: 1419. https://doi.org/10.3390/jcm14051419
APA StyleAktemur, G., Tokgöz Çakır, B., Sucu, S., Karabay, G., Şeyhanlı, Z., Vanlı Tonyalı, N., Diktaş, E. G., Ünsal, M., & Erkaya, S. (2025). Does Corpus Luteum Doppler Have a Role in Prognostic Prediction for Outcome with Threatened Abortion? Journal of Clinical Medicine, 14(5), 1419. https://doi.org/10.3390/jcm14051419





