Postoperative Patient-Reported Pain and Opioid Consumption After Total Hip Arthroplasty: A Propensity Score-Matched Comparison of the Direct Superior and Posterior Approaches
Abstract
1. Introduction
2. Method
2.1. Patient Demographics
2.2. Cohort Matching
2.3. Surgical Approaches
2.4. Direct Superior Approach
2.5. Pain Management Protocol
2.6. Patient-Reported Pain and Opioid Consumption
2.7. Postoperative Outcomes
2.8. Statistical Analysis
3. Results
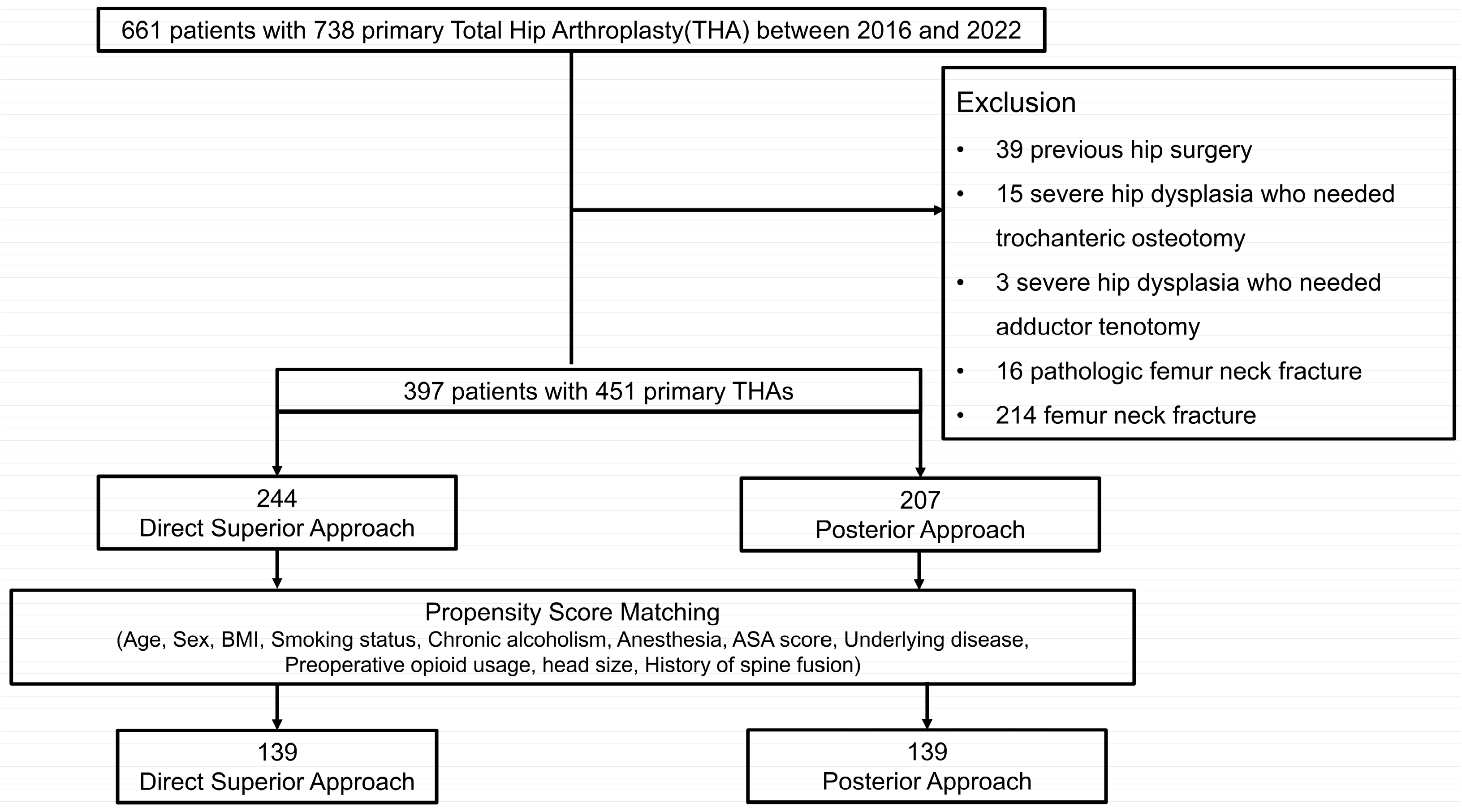
3.1. Patient Selection
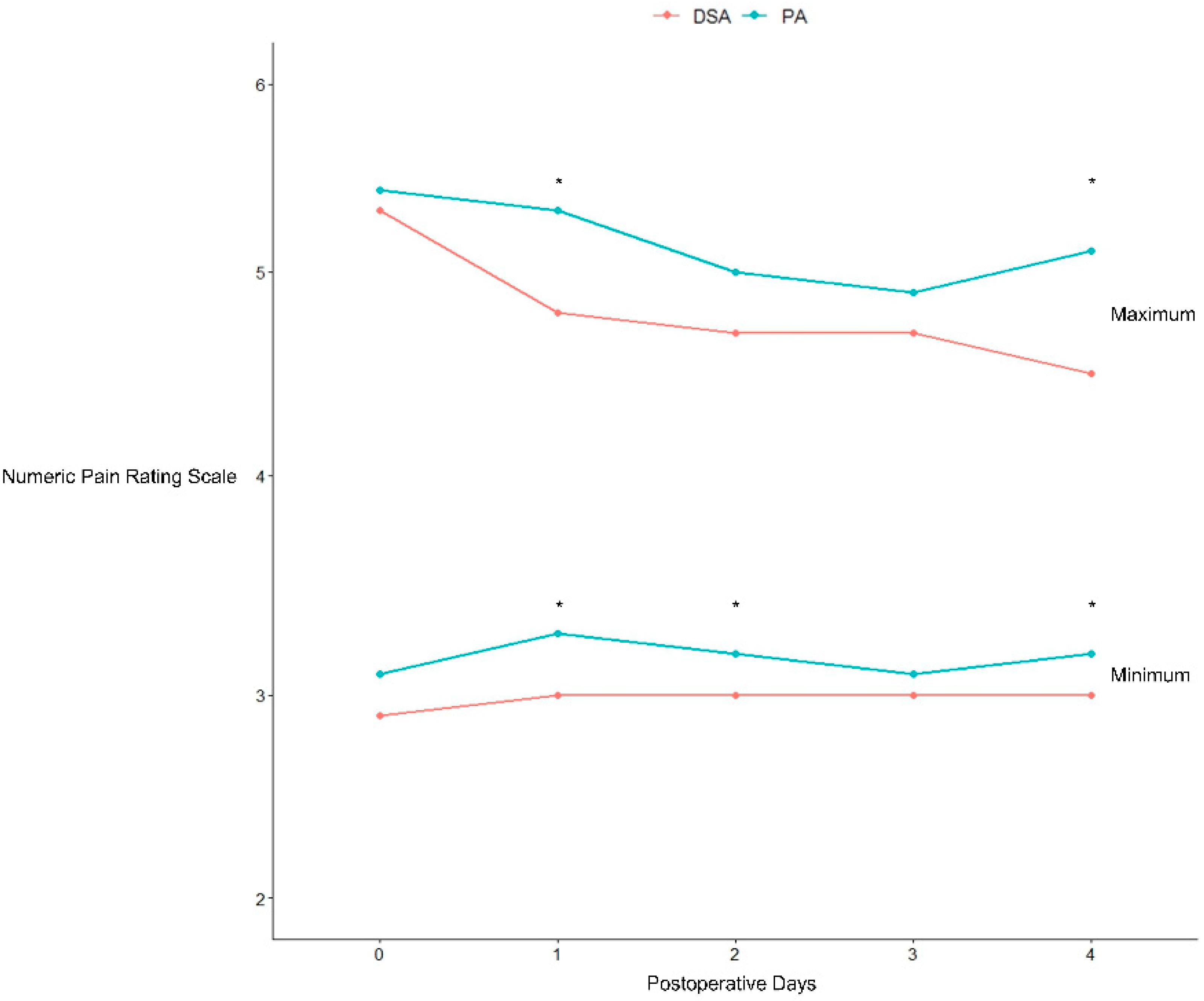
3.2. Patient-Reported Pain and Inpatient Opioid Consumption
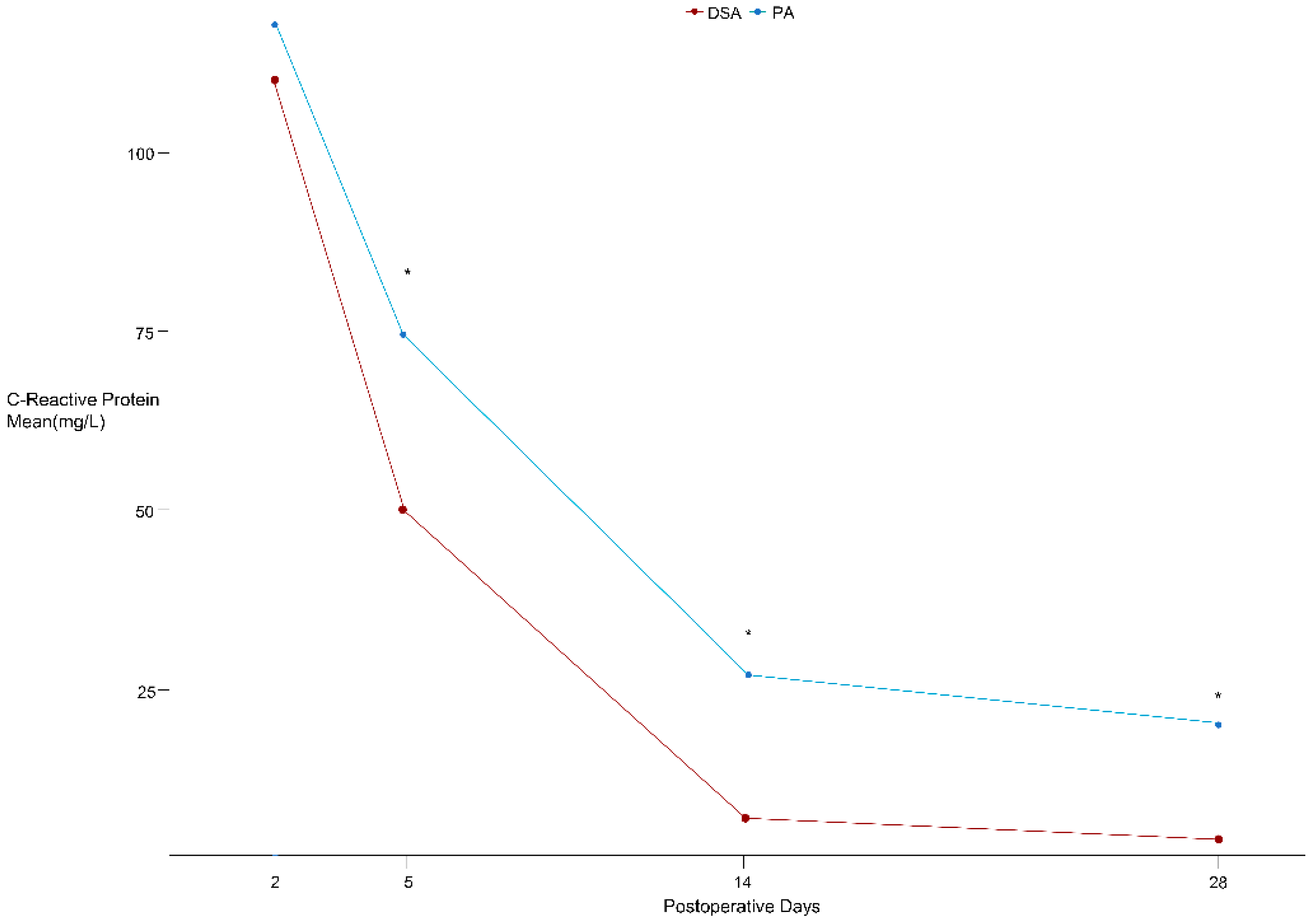
3.3. Postoperative Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Penenberg, B.L.; Bolling, W.S.; Riley, M. Percutaneously assisted total hip arthroplasty (PATH): A preliminary report. J. Bone Jt. Surg. 2008, 90, 209–220. [Google Scholar] [CrossRef] [PubMed]
- Parvizi, J.; Porat, M.; Gandhi, K.; Viscusi, E.R.; Rothman, R.H. Postoperative pain management techniques in hip and knee arthroplasty. Instr. Course Lect. 2009, 58, 769–779. [Google Scholar] [PubMed]
- Parvizi, J.; Miller, A.G.; Gandhi, K. Multimodal pain management after total joint arthroplasty. J. Bone Jt. Surg. 2011, 93, 1075–1084. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, A.C.; Hung, C.W.; Ghanta, R.B.; Harrington, M.A.; Halawi, M.J. Spinal anesthesia is a grossly underutilized gold standard in primary total joint arthroplasty: Propensity-matched analysis of a national surgical quality database. Arthroplasty 2023, 5, 7. [Google Scholar] [CrossRef]
- Roger, D.J.; Hill, D. Minimally invasive total hip arthroplasty using a transpiriformis approach: A preliminary report. Clinical Orthopaedics and Related. Research® 2012, 470, 2227–2234. [Google Scholar]
- Seah, S.; Quinn, M.; Tirosh, O.; Tran, P. Postoperative opioid consumption after total hip arthroplasty: A comparison of three surgical approaches. J. Arthroplast. 2019, 34, 2676–2680. [Google Scholar] [CrossRef]
- Kayani, B.; Konan, S.; Chandramohan, R.; Haddad, F.S. The direct superior approach in total hip arthroplasty. Br. J. Hosp. Med. 2019, 80, 320–324. [Google Scholar] [CrossRef]
- Leonard, H.J.; Ohly, N.E. Direct superior approach for total hip arthroplasty. Bone Jt. J. 2021, 103, 500–506. [Google Scholar] [CrossRef]
- Duijnisveld, B.J.; van den Hout, J.A.; Wagenmakers, R.; Koenraadt, K.L.; Bolder, S.B. No learning curve of the direct superior approach in total hip arthroplasty. Orthop. Surg. 2020, 12, 852–860. [Google Scholar] [CrossRef]
- Ezzibdeh, R.M.; Barrett, A.A.; Arora, P.; Amanatullah, D.F. Learning curve for the direct superior approach to total hip arthroplasty. Orthopedics 2020, 43, e237–e243. [Google Scholar] [CrossRef]
- Rennick, A.; Atkinson, T.; Cimino, N.M.; Strassels, S.A.; McPherson, M.L.; Fudin, J. Variability in opioid equivalence calculations. Pain Med. 2016, 17, 892–898. [Google Scholar] [CrossRef] [PubMed]
- Barrett, A.A.; Ezzibdeh, R.M.; Horst, P.K.; Roger, D.J.; Amanatullah, D.F. Direct superior approach to the hip for total hip arthroplasty. JBJS Essent. Surg. Tech. 2019, 9, e17. [Google Scholar] [CrossRef] [PubMed]
- Kenanidis, E.; Paparoidamis, G.; Pegios, V.F.; Anagnostis, P.; Potoupnis, M.; Tsiridis, E. Earlier functional recovery and discharge from hospital for THA patients operated on via direct superior compared to standard posterior approach: A retrospective frequency-matched case-control study. Hip Int. 2023, 33, 620–627. [Google Scholar] [CrossRef] [PubMed]
- Bono, O.J.; Damsgaard, C.; Robbins, C.; Aghazadeh, M.; Talmo, C.T.; Bono, J.V. Influence of Soft Tissue Preservation in Total Hip Arthroplasty: A 16-Year Experience. Surg. Technol. Int. 2018, 33, 301–307. [Google Scholar]
- Rohe, S.; Röhner, E.; Windisch, C.; Matziolis, G.; Brodt, S.; Böhle, S. Sex differences in serum C-reactive protein course after total hip arthroplasty. Clin. Orthop. Surg. 2022, 14, 48. [Google Scholar] [CrossRef]
- Zhang, Z.; Zhang, F.; Yang, X.; Fan, H.; Cheng, Q.; Guo, H. The efficacy and safety of direct superior approach (DSA) for total hip arthroplasty: A systematic review and meta-analysis. J. Orthop. Surg. Res. 2023, 18, 1–12. [Google Scholar] [CrossRef]
- Schlosser, M.J.; Korwek, K.M.; Dunn, R.; Poland, R.E. Reduced post-operative opioid use decreases length of stay and readmission rates in patients undergoing hip and knee joint arthroplasty. J. Orthop. 2020, 21, 88–93. [Google Scholar] [CrossRef]
- Hills, J.M.; Carlile, C.R.; Archer, K.R.; Wick, J.B.; Butler, M.; Daryoush, J.; Khan, I.; Call, R.; Devin, C.J.; Pennings, J.S. Duration and dosage of opioids after spine surgery: Implications on outcomes at 1 year. Spine 2020, 45, 1081–1088. [Google Scholar] [CrossRef]
- Messina, A.; La Via, L.; Milani, A.; Savi, M.; Calabrò, L.; Sanfilippo, F.; Negri, K.; Castellani, G.; Cammarota, G.; Robba, C.; et al. Spinal anesthesia and hypotensive events in hip fracture surgical repair in elderly patients: A meta-analysis. J. Anesth. Analg. Crit. Care 2022, 2, 19. [Google Scholar] [CrossRef]
- Atwood, K.; Shackleford, T.; Lemons, W.; Eicher, J.L.; Lindsey, B.A.; Klein, A.E. Postdischarge opioid use after total hip and total knee arthroplasty. Arthroplast. Today 2021, 7, 126–129. [Google Scholar] [CrossRef]
- Bovonratwet, P.; Chen, A.Z.; Shen, T.S.; Ondeck, N.T.; Kunze, K.N.; Su, E.P. Postoperative patient-reported pain and opioid consumption after total hip arthroplasty: A comparison of the direct anterior and posterior approaches. JAAOS-J. Am. Acad. Orthop. Surg. 2022, 30, e108–e117. [Google Scholar] [CrossRef] [PubMed]
- Delaney, L.D.; Gunaseelan, V.; Rieck, H.; Dupree IV, J.M.; Hallstrom, B.R.; Waljee, J.F. High-risk prescribing increases rates of new persistent opioid use in total hip arthroplasty patients. J. Arthroplast. 2020, 35, 2472–2479.e2472. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.; Shin, W.C.; Lee, S.M.; Choi, M.J.; Moon, N.H. Efficacy of Pericapsular Nerve Group Block for Pain Reduction and Opioid Consumption after Total Hip Arthroplasty: A Meta-Analysis of Randomized Controlled Trials. Hip Pelvis 2023, 35, 63. [Google Scholar] [CrossRef] [PubMed]
- Gentry, W.; Stambough, J.B.; Porter III, A.; Barnes, C.L.; Stronach, B.M.; Mears, S.C. Surgical Approach Does Not Affect Chronic Opioid Usage After Total Hip Arthroplasty. J. Arthroplast. 2023, 38, 1812–1816. [Google Scholar] [CrossRef] [PubMed]
- Siljander, M.P.; Whaley, J.D.; Koueiter, D.M.; Alsaleh, M.; Karadsheh, M.S. Length of stay, discharge disposition, and 90-day complications and revisions following primary total hip arthroplasty: A comparison of the direct anterior, posterolateral, and direct superior approaches. J. Arthroplast. 2020, 35, 1658–1661. [Google Scholar] [CrossRef]
- Tsiridis, E.; Kenanidis, E.; Potoupnis, M.; Sayegh, F.E. Direct superior approach with standard instrumentation for total hip arthroplasty: Safety and efficacy in a prospective 200-case series. Hip Int. 2020, 30, 552–558. [Google Scholar] [CrossRef]
| Characteristic | DSA 1, n = 244 | PA 2, n = 207 | p-Value |
|---|---|---|---|
| Age, mean ± SD | 60 ± 14 | 59 ± 14 | 0.3 |
| Sex, n (%) | 0.15 | ||
| Female | 131 (54%) | 96 (46%) | |
| Male | 113 (46%) | 111 (54%) | |
| Direction, n (%) | 0.74 | ||
| Left | 113 (46%) | 100 (48%) | |
| Right | 131 (54%) | 107 (52%) | |
| BMI, mean ± SD | 24.2 ± 3.6 | 24.6 ± 3.7 | 0.25 |
| Anesthesia, n (%) | 0.00 | ||
| General | 139 (57%) | 153 (74%) | |
| Spinal | 105 (43%) | 54 (26%) | |
| Diagnosis, n (%) | 0.4 | ||
| Avascular necrosis | 139 (57%) | 134 (65%) | |
| Osteoarthritis | 39 (22%) | 39 (19%) | |
| Secondary osteoarthritis | 34 (21%) | 34 (16%) | |
| History of lumbar spine fusion, n(%) | 20 (8.2%) | 10 (4.8%) | 0.21 |
| Femoral head size | 0.00 | ||
| 28 mm | 0 (0%) | 2 (1.0%) | |
| 32 mm | 50 (20.5%) | 48 (23.2%) | |
| 36 mm | 122 (50.0%) | 147 (71.0%) | |
| Dual mobility construct | 72 (29.5%) | 10 (4.8%) | |
| Opioid naïve patients, n (%) | 240 (98%) | 205 (99%) | 0.7 |
| Alcohol abuse, n (%) | 23 (9.5%) | 33 (15.9%) | 0.07 |
| ASA 3 score | 0.00 | ||
| 1 | 5 (2.0%) | 19 (9.2%) | |
| 2 | 179 (73.4%) | 159 (76.8%) | |
| 3 | 58 (23.8%) | 29 (14.0%) | |
| 4 | 2 (0.8%) | 0 (0.0%) | |
| Underlying disease, n (%) | |||
| HTN | 100 (41%) | 94 (45%) | 0.4 |
| Angina | 18 (7.4%) | 15 (7.2%) | 0.99 |
| DM | 50 (20.5%) | 25 (12.1%) | 0.02 |
| Stroke | 13 (5.3%) | 11 (5.3%) | 0.99 |
| Parkinson | 3 (1.2%) | 2 (1.0%) | 0.99 |
| Dementia | 4 (1.6%) | 5 (2.4%) | 0.99 |
| Smoking status, n (%) | 0.2 | ||
| Non-smoker | 149 (61%) | 128 (62%) | |
| Ex-smoker | 39 (16%) | 21 (10%) | |
| Current smoker | 56 (23%) | 58 (28%) |
| Characteristic | DSA 1, n = 139 | PA 2, n = 139 | Abs.SMD 3 |
|---|---|---|---|
| Age, mean ± SD | 58 ± 13 | 58 ± 14 | 0.03 |
| Sex, n (%) | 0.11 | ||
| Female | 67 (48%) | 61 (44%) | |
| Male | 72 (52%) | 78 (56%) | |
| Direction, n (%) | 0.04 | ||
| Left | 64 (45.8%) | 67 (48.1%) | |
| Right | 75 (54.2%) | 72 (51.9%) | |
| BMI, mean ± SD | 24.5 ± 3.9 | 24.5 ± 3.3 | 0.00 |
| Anesthesia, n (%) | 0.15 | ||
| General | 86 (61.8%) | 96 (80.1%) | |
| Spinal | 53 (38.2%) | 43 (30.9%) | |
| Diagnosis, n (%) | 0.02 | ||
| Osteonecrosis of femoral head | 89 (64.1%) | 85 (61.1%) | |
| Osteoarthritis | 26 (18.3%) | 32 (23.0%) | |
| Secondary osteoarthritis | 24 (17.6%) | 22 (15.9%) | |
| History of lumbar spine fusion, n (%) | 7 (5.0%) | 6 (4.3%) | 0.02 |
| Femoral head size | 0.01 | ||
| 28 mm | 0 (0.0%) | 1 (7.2%) | |
| 32 mm | 29 (20.8%) | 34 (24.4%) | |
| 36 mm | 96 (64.7%) | 94 (67.6%) | |
| Dual mobility construct | 14 (10.0%) | 10 (7.2%) | |
| Alcohol abuse | 16 (11.5%) | 17 (12.2%) | 0.03 |
| ASA score | −0.06 | ||
| 1 | 8 (6.1%) | 5 (3.8%) | |
| 2 | 103 (74.0%) | 114 (81.7%) | |
| 3 | 28 (19.8%) | 20 (14.5%) | |
| Opioid naïve patients, n (%) | 137 (98%) | 137 (98%) | 0.000 |
| Underlying disease, n (%) | |||
| HTN | 54 (38.8%) | 56 (40.3%) | 0.03 |
| Angina | 10 (7.2%) | 8 (5.8%) | −0.05 |
| DM | 19 (13.7%) | 20 (14.4%) | 0.02 |
| Stroke | 7 (5.0%) | 6 (4.3%) | 0.00 |
| Parkinson | 2 (1.4%) | 4 (2.9%) | 0.03 |
| Dementia | 3 (2.2%) | 3 (2.2%) | 0.00 |
| Smoking status, n (%) | 0.10 | ||
| Non-smoker | 93 (67%) | 89 (64%) | |
| Ex-smoker | 18 (13%) | 13 (9.4%) | |
| Current smoker | 28 (20%) | 37 (26%) |
| Characteristic | DSA 1, n = 139 | PA 2, n = 139 | p-Value 3 |
|---|---|---|---|
| Maximum NRS 4 | |||
| POD 5 #0 | 5.3 ± 1.4 | 5.4 ± 1.4 | 0.684 |
| POD 5 #1 | 4.8 ± 1.1 | 5.3 ± 1.5 | 0.006 |
| POD 5 #2 | 4.7 ± 1.1 | 5.0 ± 1.3 | 0.112 |
| POD 5 #3 | 4.7 ± 1.1 | 4.9 ± 1.2 | 0.20 |
| POD 5 #4 | 4.5 ± 0.8 | 5.1 ± 1.4 | 0.000 |
| Minimum NRS 4 | |||
| POD 5 #0 | 2.9 ± 0.5 | 3.1 ± 0.7 | 0.1 |
| POD 5 #1 | 3.0 ± 0.6 | 3.3 ± 0.9 | 0.04 |
| POD 5 #2 | 3.0 ± 0.5 | 3.2 ± 0.8 | 0.02 |
| POD 5 #3 | 3.0 ± 0.5 | 3.1 ± 0.7 | 0.09 |
| POD 5 #4 | 3.0 ± 0.6 | 3.2 ± 0.7 | 0.01 |
| OME 6, mean ± SD | 108 ± 127 | 194 ± 117 | 0.002 |
| Opioid refill > 90 days, n (%) | 2 (1.4%) | 1 (0.7%) | >0.9 |
| Opioid refill > 180 days, n (%) | 1 (0.7%) | 0 (0%) | >0.9 |
| Characteristic | DSA 1, n = 139 | PA 2, n = 139 | p-Value 3 |
|---|---|---|---|
| CRP 4, Mean ± SD | |||
| POD 5 #2 | 120 ± 50 | 113 ± 60 | 0.5 |
| POD 5 #5 | 53 ± 33 | 74 ± 43 | <0.001 |
| POD 5 #14 | 9 ± 16 | 28 ± 43 | <0.001 |
| POD 5 #28 | 7 ± 13 | 23 ± 39 | <0.001 |
| ESR 6, Mean ± SD | |||
| POD 5 #2 | 48 ± 29 | 34 ± 23 | 0.008 |
| POD 5 #5 | 43 ± 30 | 42 ± 24 | 0.6 |
| POD 5 #14 | 41 ± 30 | 39 ± 24 | >0.9 |
| POD 5 #28 | 39 ± 29 | 38 ± 23 | 0.8 |
| Characteristic | DSA 1, n = 139 | PA 2, n = 139 | p-Value 1 |
|---|---|---|---|
| Intraoperative Fracture, n (%) | 1 (0.7%) | 1 (0.7%) | >0.9 |
| Revision, n (%) | 1 (0.7%) | 1 (0.7%) | >0.9 |
| Periprosthetic Fracture, n (%) | 1 (0.7%) | 1 (0.7%) | >0.9 |
| Periprosthetic Infection, n (%) | 0 (0%) | 0 (0%) | >0.9 |
| Revision Due to Component Malposition, n (%) | 0 (0%) | 0 (0%) | >0.9 |
| Acute Dislocation, n (%) | 3 (2.2%) | 8 (5.6%) | 0.15 |
| Length of Stay, Mean ± SD | 5.4 ± 3.1 | 8.4 ± 8.3 | <0.001 |
| HHS 3, 6 months post-operation | 88.1 ± 11.1 | 87.3 ± 8.7 | 0.5 |
| WOMAC 4, 6 months post-operation | 15.2 ± 11.3 | 18.9 ± 17.6 | 0.13 |
| HHS 3, 12 months post-operation | 93.6. ± 7.9 | 93.6 ± 3.8 | >0.9 |
| WOMAC 4, 12 months post-operation | 10.2 ± 7.8 | 9.9 ± 3.8 | >0.9 |
| 90-Day Readmission, n (%) | 2 (1.4%) | 7 (5%) | 0.1 |
| Postoperative Complications, n (%) | |||
| Delirium | 5 (3.6%) | 13 (9.4%) | 0.05 |
| Urinary Tract Infection | 0 (0%) | 0 (0%) | >0.9 |
| Acute Kidney Injury | 0 (0%) | 0 (0%) | >0.9 |
| Pneumonia | 0 (0%) | 0 (0%) | >0.9 |
| Stroke | 0 (0%) | 0 (0%) | >0.9 |
| Sepsis | 0 (0%) | 0 (0%) | >0.9 |
| Death | 0 (0%) | 0 (0%) | >0.9 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hong, S.H.; Yu, K.H.; Han, S.B. Postoperative Patient-Reported Pain and Opioid Consumption After Total Hip Arthroplasty: A Propensity Score-Matched Comparison of the Direct Superior and Posterior Approaches. J. Clin. Med. 2025, 14, 1400. https://doi.org/10.3390/jcm14051400
Hong SH, Yu KH, Han SB. Postoperative Patient-Reported Pain and Opioid Consumption After Total Hip Arthroplasty: A Propensity Score-Matched Comparison of the Direct Superior and Posterior Approaches. Journal of Clinical Medicine. 2025; 14(5):1400. https://doi.org/10.3390/jcm14051400
Chicago/Turabian StyleHong, Seok Ha, Kang Hun Yu, and Seung Beom Han. 2025. "Postoperative Patient-Reported Pain and Opioid Consumption After Total Hip Arthroplasty: A Propensity Score-Matched Comparison of the Direct Superior and Posterior Approaches" Journal of Clinical Medicine 14, no. 5: 1400. https://doi.org/10.3390/jcm14051400
APA StyleHong, S. H., Yu, K. H., & Han, S. B. (2025). Postoperative Patient-Reported Pain and Opioid Consumption After Total Hip Arthroplasty: A Propensity Score-Matched Comparison of the Direct Superior and Posterior Approaches. Journal of Clinical Medicine, 14(5), 1400. https://doi.org/10.3390/jcm14051400







