Trends of Pediatric Anterior Cruciate Ligament Reconstruction Surgery in Korea: Nationwide Population-Based Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source
2.2. Study Design
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rössler, R.; Donath, L.; Verhagen, E.; Junge, A.; Schweizer, T.; Faude, O. Exercise-Based Injury Prevention in Child and Adolescent Sport: A Systematic Review and Meta-Analysis. Sports Med. 2014, 44, 1733–1748. [Google Scholar] [CrossRef] [PubMed]
- Trivedi, V.; Mishra, P.; Verma, D. Pediatric ACL Injuries: A Review of Current Concepts. Open Orthop. J. 2017, 11, 378–388. [Google Scholar] [CrossRef] [PubMed]
- Millett, P.J.; Willis, A.A.; Warren, R.F. Associated Injuries in Pediatric and Adolescent Anterior Cruciate Ligament Tears: Does a Delay in Treatment Increase the Risk of Meniscal Tear? Arthrosc. J. Arthrosc. Relat. Surg. 2002, 18, 955–959. [Google Scholar] [CrossRef] [PubMed]
- Dumont, G.D.; Hogue, G.D.; Padalecki, J.R.; Okoro, N.; Wilson, P.L. Meniscal and Chondral Injuries Associated With Pediatric Anterior Cruciate Ligament Tears: Relationship of Treatment Time and Patient-Specific Factors. Am. J. Sports Med. 2012, 40, 2128–2133. [Google Scholar] [CrossRef] [PubMed]
- Vavken, P.; Murray, M.M. Treating Anterior Cruciate Ligament Tears in Skeletally Immature Patients. Arthrosc. J. Arthrosc. Relat. Surg. 2011, 27, 704–716. [Google Scholar] [CrossRef]
- Konrads, C.; Döbele, S.; Ateschrang, A.; Ahmad, S.S. Outcome of Anterior Cruciate Ligament Reconstruction in Children and Adolescents: A Retrospective Study. J. Clin. Orthop. Trauma 2021, 13, 46–49. [Google Scholar] [CrossRef]
- Patil, V.; Rajan, P.; Hayter, E.; Bartlett, J.; Symons, S. Growth Disturbances Following Paediatric Anterior Cruciate Ligament Reconstruction: A Systematic Review. Cureus 2023, 15, e40455. [Google Scholar] [CrossRef]
- Peterson, D.C.; Ayeni, O.R. Pediatric Anterior Cruciate Ligament Reconstruction Outcomes. Curr. Rev. Musculoskelet. Med. 2016, 9, 339–347. [Google Scholar] [CrossRef]
- Fabricant, P.D.; Jones, K.J.; Delos, D.; Cordasco, F.A.; Marx, R.G.; Pearle, A.D.; Warren, R.F.; Green, D.W. Reconstruction of the Anterior Cruciate Ligament in the Skeletally Immature Athlete: A Review of Current Concepts: AAOS Exhibit Selection. JBJS 2013, 95, e28. [Google Scholar] [CrossRef]
- Monk, A.P.; Davies, L.J.; Hopewell, S.; Harris, K.; Beard, D.J.; Price, A.J. Surgical versus Conservative Interventions for Treating Anterior Cruciate Ligament Injuries—Monk, AP—2016|Cochrane Library. Cochrane Database Syst. Rev. 2016, 4, CD011166. [Google Scholar]
- Matsuzaki, Y.; Chipman, D.E.; Hidalgo Perea, S.; Green, D.W. Unique Considerations for the Pediatric Athlete During Rehabilitation and Return to Sport After Anterior Cruciate Ligament Reconstruction. Arthrosc. Sports Med. Rehabil. 2022, 4, e221–e230. [Google Scholar] [CrossRef] [PubMed]
- Beck, N.A.; Lawrence, J.T.R.; Nordin, J.D.; DeFor, T.A.; Tompkins, M. ACL Tears in School-Aged Children and Adolescents Over 20 Years. Pediatrics 2017, 139, e20161877. [Google Scholar] [CrossRef]
- Buller, L.T.; Best, M.J.; Baraga, M.G.; Kaplan, L.D. Trends in Anterior Cruciate Ligament Reconstruction in the United States. Orthop. J. Sports Med. 2015, 3, 2325967114563664. [Google Scholar] [CrossRef]
- Kim, M.K.; Han, K.; Lee, S.-H. Current Trends of Big Data Research Using the Korean National Health Information Database. Diabetes Metab. J. 2022, 46, 552–563. [Google Scholar] [CrossRef]
- Bixby, E.C.; Heyworth, B.E. Management of Anterior Cruciate Ligament Tears in Skeletally Immature Patients. Curr. Rev. Musculoskelet. Med. 2024, 17, 258–272. [Google Scholar] [CrossRef]
- Frobell, R.B.; Roos, E.M.; Roos, H.P.; Ranstam, J.; Lohmander, L.S. A Randomized Trial of Treatment for Acute Anterior Cruciate Ligament Tears. N. Engl. J. Med. 2010, 363, 331–342. [Google Scholar] [CrossRef]
- Herzog, M.M.; Marshall, S.W.; Lund, J.L.; Pate, V.; Mack, C.D.; Spang, J.T. Incidence of Anterior Cruciate Ligament Reconstruction Among Adolescent Females in the United States, 2002 Through 2014. JAMA Pediatr. 2017, 171, 808–810. [Google Scholar] [CrossRef]
- Liang, J.; Luo, Y.; Yang, Y.; Xie, H.; Huang, Z.; Zhong, M.; Zhu, W. Global Overview of Anterior Cruciate Ligament Reconstruction in Children and Adolescents over the Past 20 Years: A Bibliometric Analysis. J. Orthop. Surg. 2024, 19, 350. [Google Scholar] [CrossRef]
- Bartek, B.; Jung, T.; Lackner, T.; Schatka, I.; Gwinner, C.; Walter-Rittel, T. High revision rate after transphyseal ACL reconstruction in skeletally immature patients. J. Pers. Med. 2024, 14, 1129. [Google Scholar] [CrossRef] [PubMed]
- Hosseinzadeh, S.; Kiapour, A.M. Age-related changes in ACL morphology during skeletal growth and maturation are different between females and males. J. Orthop. Res. 2021, 39, 841–849. [Google Scholar] [CrossRef]
- Longo, U.G.; Salvatore, G.; Ruzzini, L.; Risi Ambrogioni, L.; de Girolamo, L.; Viganò, M.; Facchini, F.; Cella, E.; Candela, V.; Ciccozzi, M.; et al. Trends of Anterior Cruciate Ligament Reconstruction in Children and Young Adolescents in Italy Show a Constant Increase in the Last 15 Years. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 1728–1733. [Google Scholar] [CrossRef] [PubMed]
- Paterno, M.V.; Rauh, M.J.; Schmitt, L.C.; Ford, K.R.; Hewett, T.E. Incidence of Contralateral and Ipsilateral Anterior Cruciate Ligament (ACL) Injury After Primary ACL Reconstruction and Return to Sport. Clin. J. Sport Med. 2012, 22, 116. [Google Scholar] [CrossRef] [PubMed]
- Dekker, T.J.; Godin, J.A.; Dale, K.M.; Garrett, W.E.; Taylor, D.C.; Riboh, J.C. Return to Sport After Pediatric Anterior Cruciate Ligament Reconstruction and Its Effect on Subsequent Anterior Cruciate Ligament Injury. J. Bone Jt. Surg. 2017, 99, 897. [Google Scholar] [CrossRef] [PubMed]
- Cristiani, R.; Forssblad, M.; Edman, G.; Eriksson, K.; Stålman, A. Age, Time from Injury to Surgery and Quadriceps Strength Affect the Risk of Revision Surgery after Primary ACL Reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 1795. [Google Scholar] [CrossRef]
- Garside, J.C.; Bellaire, C.P.; Schaefer, E.J.; Kim, B.S.; Panish, B.J.; Elkadi, S.H.; Kraft, D.B.; Argintar, E.H. Anterior cruciate ligament reconstruction with suture tape augmentation in the high-risk, young population. Eur. J. Orthop. Surg. Traumatol. 2024, 35, 4. [Google Scholar] [CrossRef]
- Khan, Z.A.; Kerzner, B.; Kaplan, D.J.; Riff, A.J.; Chahla, J.; Bach, B.R., Jr. A single-surgeon 35-year experience with ACL reconstruction using patellar tendon auto- and allografts with the transtibial technique. Orthop. J. Sports Med. 2024, 12, 23259671241265074. [Google Scholar] [CrossRef]
- Ardern, C.L.; Ekas, G.R.; Grindem, H.; Moksnes, H.; Anderson, A.F.; Chotel, F.; Cohen, M.; Forssblad, M.; Ganley, T.J.; Feller, J.A.; et al. 2018 International Olympic Committee consensus statement on prevention, diagnosis, and management of pediatric anterior cruciate ligament (ACL) injuries. Br. J. Sports Med. 2018, 52, 422–438. [Google Scholar] [CrossRef]
| Study Duration | 2011 to 2018 |
|---|---|
| Operated patients number (Total number, %) | 83,132 (233,478, 35.6%) |
| Age group (1:2:3:4, %) * | 224:1960:5367:75,581 (0.3:2.4:6.5:90.9) |
| Sex (Male: Female, %) | 66,157:16,975 (79.6:20.4) |
| Region (Urban: Rural, %) | 81,543:1589 (98.1:1.9) |
| Combined procedures (Number, %) | 2508 (3.02%) |
| Chondroplasty | 2009/2508, 80.1% |
| Other ligament repair | 499/2508, 19.9% |
| Male | Female | |||
|---|---|---|---|---|
| No. | % | No. | % | |
| 2011 | 7827 | 35.2 | 1850 | 18.6 |
| 2012 | 8324 | 38.4 | 2093 | 22.8 |
| 2013 | 8408 | 39.5 | 2231 | 23.7 |
| 2014 | 8553 | 41.0 | 2141 | 25.3 |
| 2015 | 8764 | 42.3 | 2106 | 25.5 |
| 2016 | 8450 | 42.0 | 2216 | 27.2 |
| 2017 | 7922 | 41.0 | 2229 | 27.8 |
| 2018 | 7909 | 43.0 | 2109 | 27.2 |
| Urban | Rural | |||
|---|---|---|---|---|
| No. | % | No. | % | |
| 2011 | 9479 | 30.8 | 198 | 14.4 |
| 2012 | 10,218 | 34.8 | 199 | 13.4 |
| 2013 | 10,433 | 35.5 | 206 | 16.1 |
| 2014 | 10,498 | 37.2 | 196 | 18.1 |
| 2015 | 10,643 | 38.2 | 227 | 21.1 |
| 2016 | 10,465 | 38.3 | 201 | 20.7 |
| 2017 | 9949 | 38.1 | 202 | 21.2 |
| 2018 | 9858 | 38.8 | 160 | 22.0 |
| ≤12 | 13–15 | 16–17 | ≥18 | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | No. | % | No. | % | |
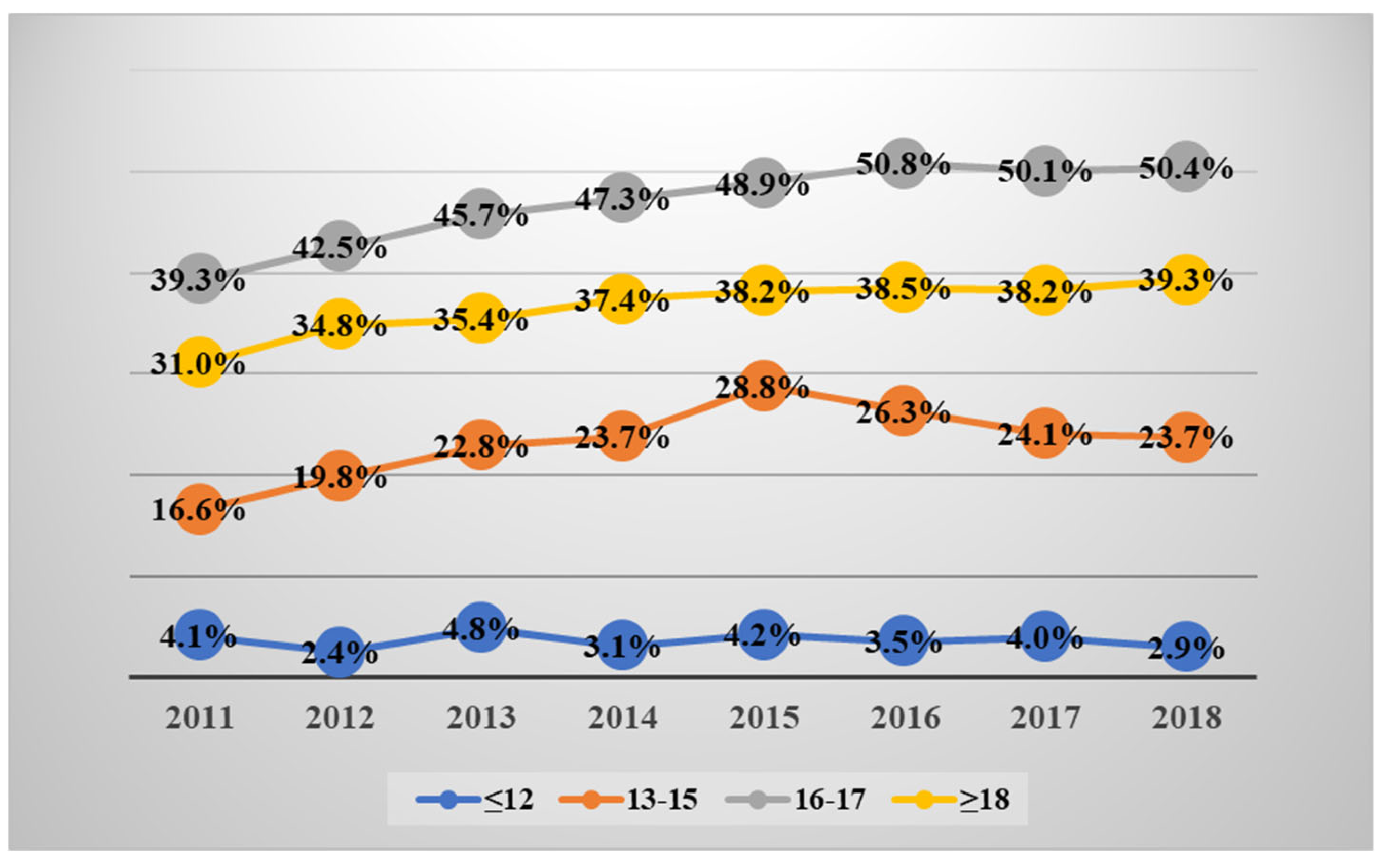
| 2011 | 41 | 4.1 | 169 | 16.6 | 494 | 39.3 | 8973 | 31.0 | 9677 | 30.1 |
| 2012 | 20 | 2.4 | 211 | 19.8 | 579 | 42.5 | 9607 | 34.8 | 10,417 | 33.8 |
| 2013 | 37 | 4.8 | 252 | 22.8 | 624 | 45.7 | 9726 | 35.4 | 10,639 | 34.6 |
| 2014 | 22 | 3.1 | 263 | 23.7 | 705 | 47.3 | 9704 | 37.4 | 10,694 | 36.5 |
| 2015 | 30 | 4.2 | 327 | 28.8 | 751 | 48.9 | 9762 | 38.2 | 10,870 | 37.5 |
| 2016 | 26 | 3.5 | 290 | 26.3 | 775 | 50.8 | 9575 | 38.5 | 10,666 | 37.7 |
| 2017 | 27 | 4.0 | 228 | 24.1 | 738 | 50.1 | 9158 | 38.2 | 10,151 | 37.5 |
| 2018 | 21 | 2.9 | 220 | 23.7 | 701 | 50.4 | 9076 | 39.3 | 10,018 | 38.3 |
| ≤12 | 13–15 | 16–17 | ≥18 | Total | ||||||
| Male | ||||||||||
| No. | % | No. | % | No. | % | No. | % | No. | % | |
| 2011 | 27 | 4.0 | 97 | 13.0 | 378 | 38.9 | 7325 | 36.9 | 7827 | 35.2 |
| 2012 | 10 | 1.8 | 128 | 16.5 | 472 | 44.1 | 7714 | 40.1 | 8324 | 38.4 |
| 2013 | 23 | 4.6 | 157 | 19.7 | 493 | 47.5 | 7735 | 40.8 | 8408 | 39.5 |
| 2014 | 13 | 2.5 | 158 | 20.0 | 548 | 47.2 | 7834 | 42.6 | 8553 | 41.0 |
| 2015 | 22 | 4.5 | 204 | 24.9 | 600 | 50.2 | 7938 | 43.6 | 8764 | 42.3 |
| 2016 | 11 | 2.2 | 170 | 22.1 | 612 | 51.3 | 7657 | 43.4 | 8450 | 42.0 |
| 2017 | 16 | 3.4 | 128 | 19.4 | 568 | 50.0 | 7210 | 43.0 | 7922 | 41.6 |
| 2018 | 12 | 2.5 | 112 | 17.9 | 565 | 51.1 | 7220 | 44.7 | 7909 | 43.0 |
| Female | ||||||||||
| No. | % | No. | % | No. | % | No. | % | No. | % | |
| 2011 | 14 | 4.5 | 72 | 26.6 | 116 | 40.7 | 1648 | 18.2 | 1850 | 18.6 |
| 2012 | 10 | 3.9 | 83 | 28.7 | 107 | 36.9 | 1893 | 22.6 | 2093 | 22.8 |
| 2013 | 14 | 5.3 | 95 | 31.1 | 131 | 40.2 | 1991 | 23.4 | 2231 | 23.7 |
| 2014 | 9 | 4.4 | 105 | 33.2 | 157 | 47.9 | 1870 | 24.6 | 2141 | 25.4 |
| 2015 | 8 | 3.5 | 123 | 39.1 | 151 | 44.3 | 1824 | 24.8 | 2106 | 25.5 |
| 2016 | 15 | 5.9 | 120 | 35.9 | 163 | 48.8 | 1918 | 26.5 | 2216 | 27.2 |
| 2017 | 11 | 5.2 | 100 | 35.0 | 170 | 50.2 | 1948 | 27.1 | 2229 | 27.8 |
| 2018 | 9 | 3.9 | 108 | 35.6 | 136 | 47.6 | 1856 | 26.7 | 2019 | 27.2 |
| IRR | 95% CI | p Value | |
|---|---|---|---|
| Total | |||
| Year | 1.03 | 1.02–1.03 | <0.001 |
| Sex | |||
| Male | Reference | - | |
| Female | 0.62 | 0.61–0.63 | <0.001 |
| Region | |||
| Urban | Reference | - | - |
| Rural | 0.52 | 0.50–0.55 | <0.001 |
| Age group | |||
| ≤12 | Reference | - | - |
| 13–15 | 6.03 | 5.25–6.93 | <0.001 |
| 16–17 | 11.70 | 10.23–13.37 | <0.001 |
| ≥18 | 9.40 | 8.25–10.72 | <0.001 |
| IRR | 95% CI | p Value | |
|---|---|---|---|
| ≤12 | 0.99 | 0.93–1.04 | 0.6834 |
| 13–15 | 1.04 | 1.02–1.06 | <0.001 |
| 16–17 | 1.03 | 1.02–1.05 | <0.001 |
| ≥18 | 1.03 | 1.02–1.03 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hwang, J.; Kwon, Y.-M.; Lee, C.; Kim, S.J.; Seo, Y.-J. Trends of Pediatric Anterior Cruciate Ligament Reconstruction Surgery in Korea: Nationwide Population-Based Study. J. Clin. Med. 2025, 14, 1389. https://doi.org/10.3390/jcm14041389
Hwang J, Kwon Y-M, Lee C, Kim SJ, Seo Y-J. Trends of Pediatric Anterior Cruciate Ligament Reconstruction Surgery in Korea: Nationwide Population-Based Study. Journal of Clinical Medicine. 2025; 14(4):1389. https://doi.org/10.3390/jcm14041389
Chicago/Turabian StyleHwang, Jihyun, Young-Min Kwon, Collin Lee, Sung Jae Kim, and Young-Jin Seo. 2025. "Trends of Pediatric Anterior Cruciate Ligament Reconstruction Surgery in Korea: Nationwide Population-Based Study" Journal of Clinical Medicine 14, no. 4: 1389. https://doi.org/10.3390/jcm14041389
APA StyleHwang, J., Kwon, Y.-M., Lee, C., Kim, S. J., & Seo, Y.-J. (2025). Trends of Pediatric Anterior Cruciate Ligament Reconstruction Surgery in Korea: Nationwide Population-Based Study. Journal of Clinical Medicine, 14(4), 1389. https://doi.org/10.3390/jcm14041389







