Mapping of Patellar Fracture Patterns: A Multicenter Study of 237 Patients
Abstract
:1. Introduction
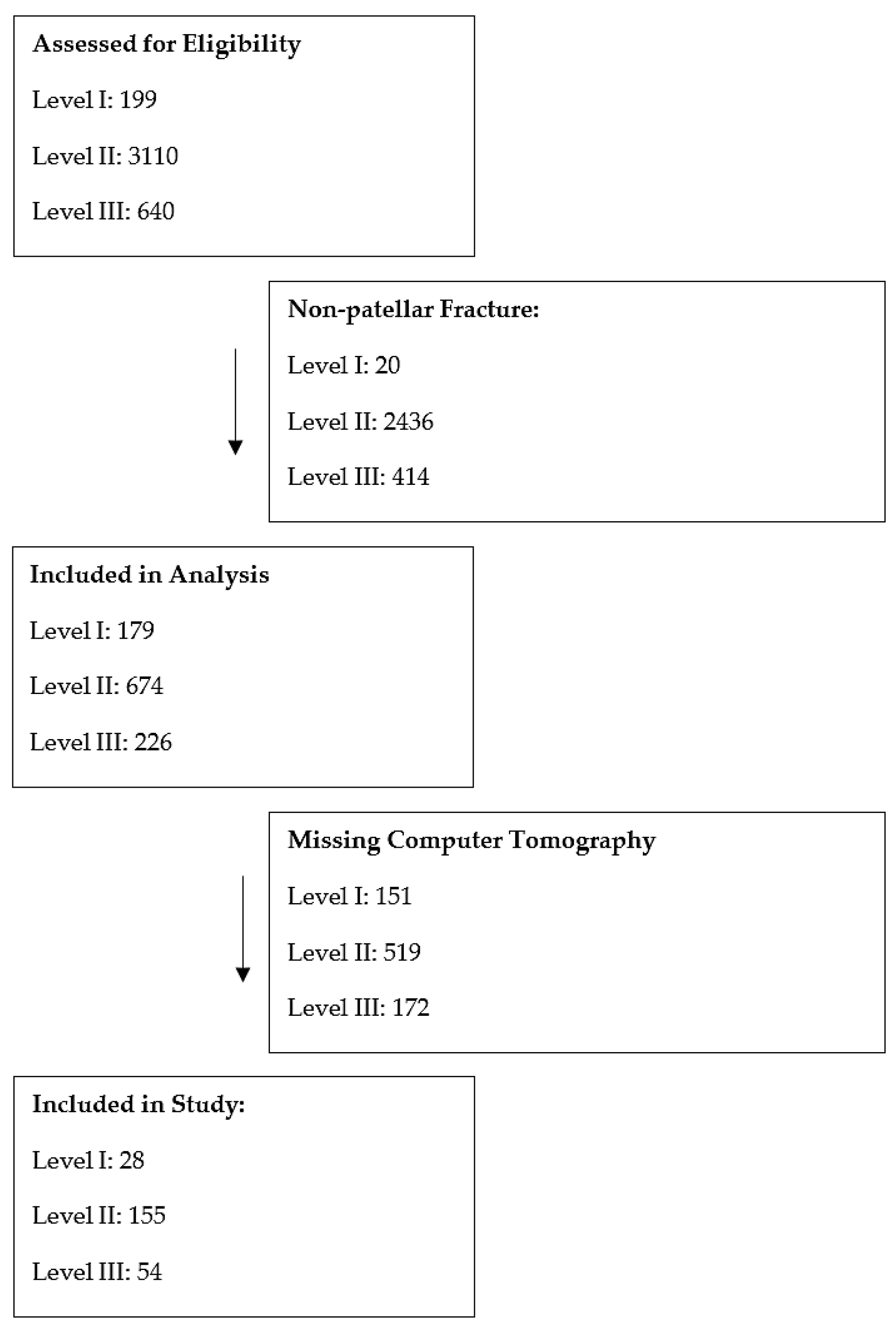
2. Materials and Methods
2.1. Study Population
2.2. Radiological Evaluation
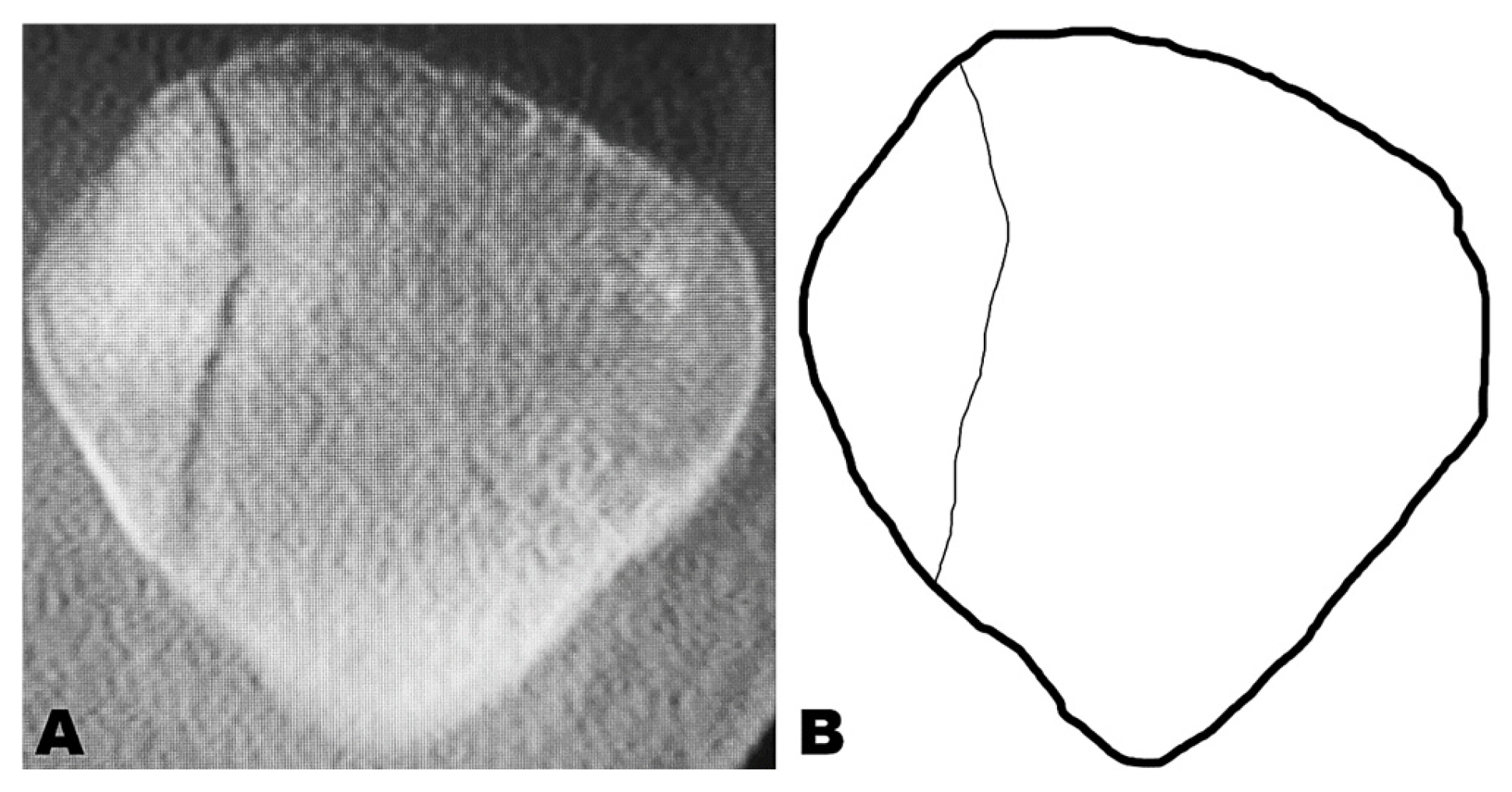
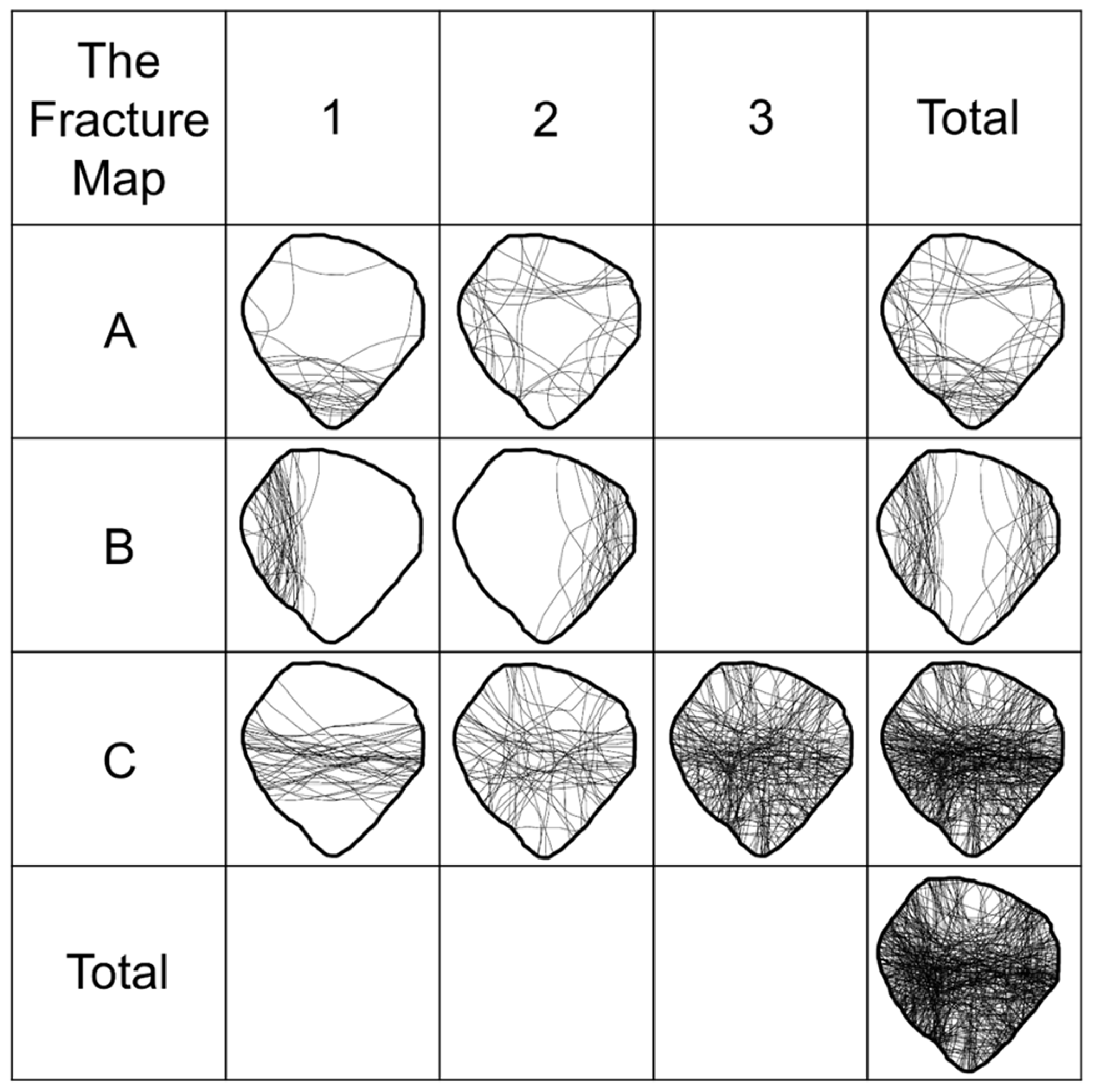
2.3. Fracture Mapping
2.4. Data Analysis
3. Results
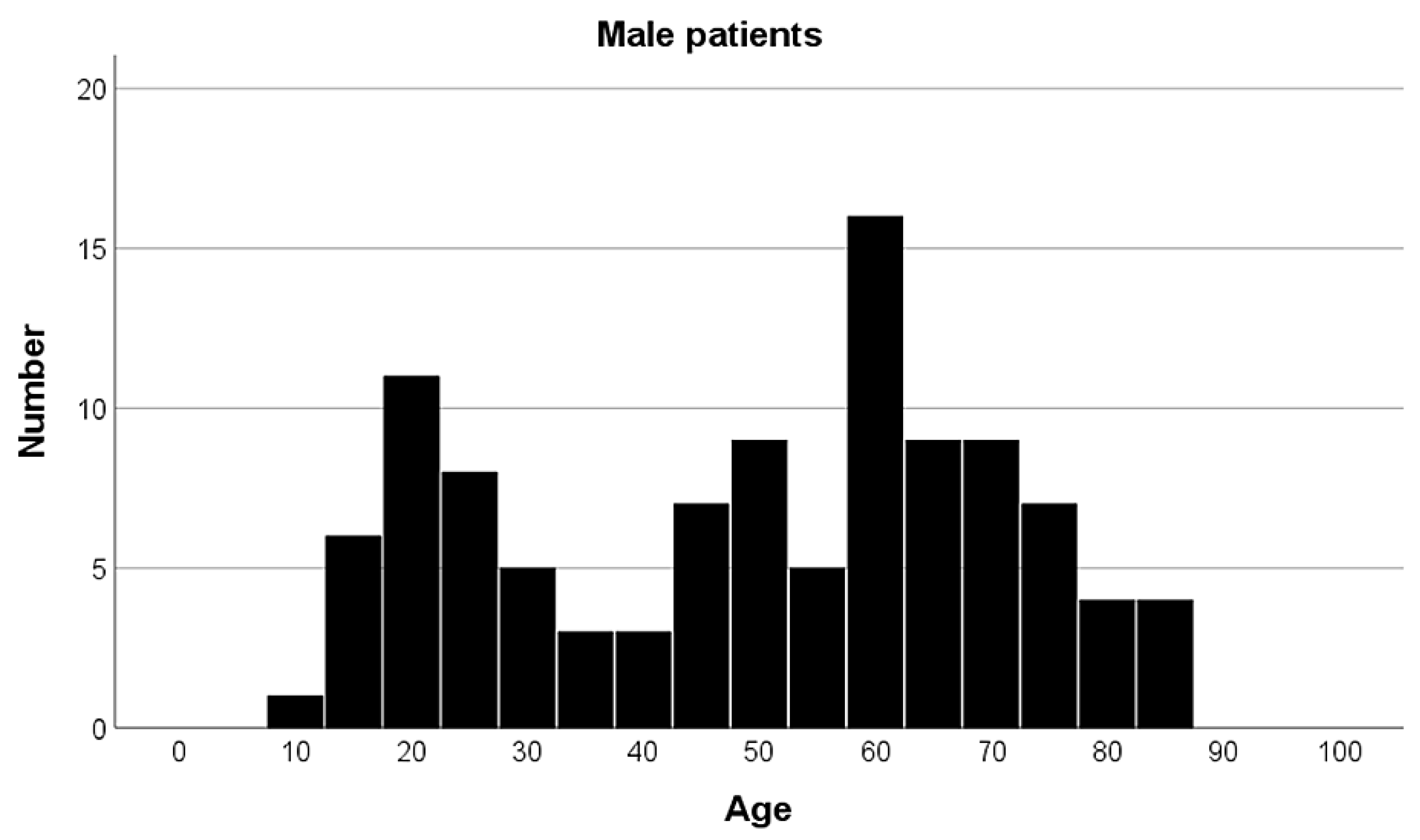
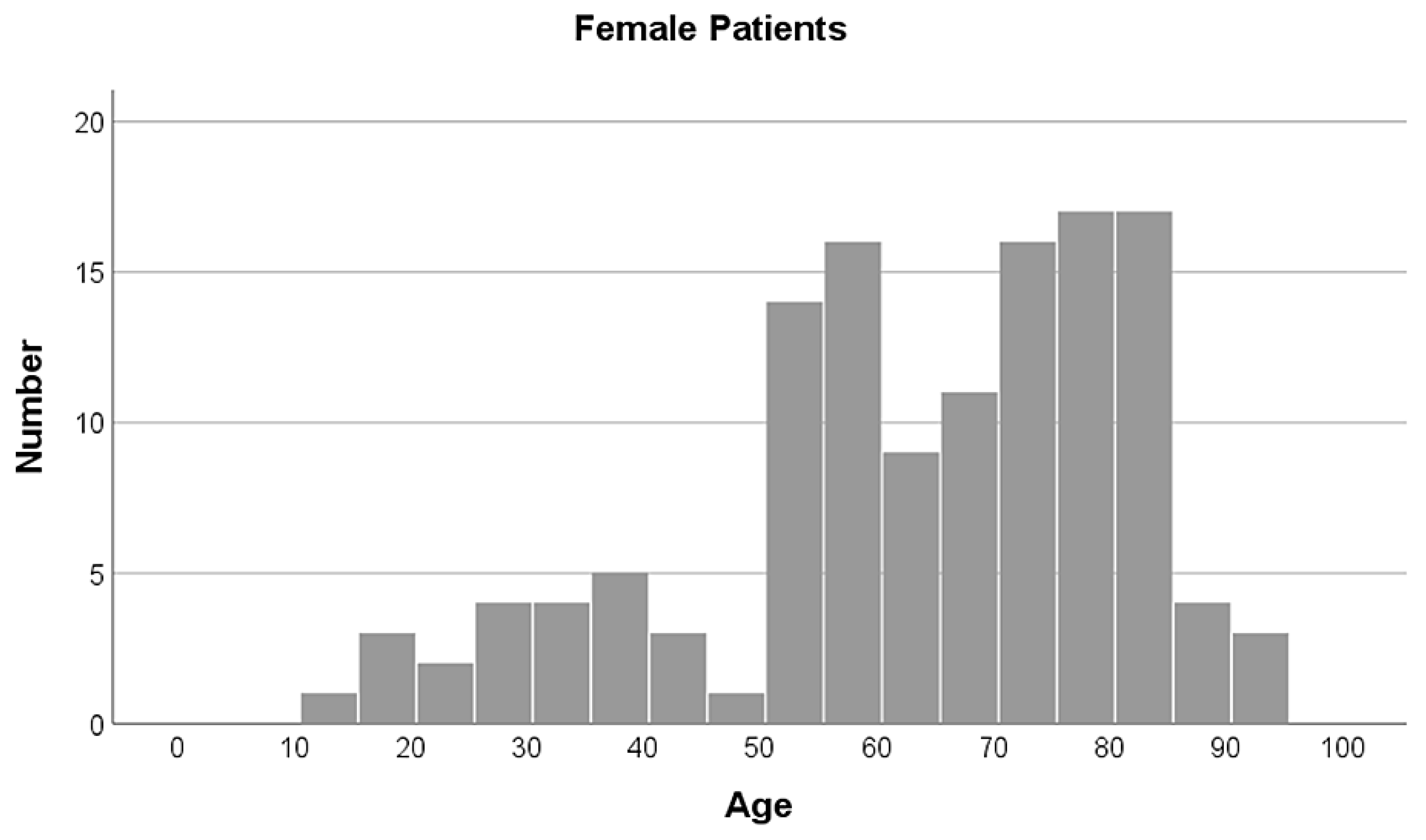
3.1. Demographics
3.2. AO/OTA Classification
3.3. Significant Influence of the Level of Trauma Center on AO/OTA Classification
3.4. Significant Influence of Age on AO/OTA Classification
3.5. No Influence of Sex on AO/OTA Classification
3.6. Fracture Mapping
4. Discussion
4.1. Demographics
4.2. AO/OTA Classification
4.3. Significant Influence of the Level of Trauma Center on AO/OTA Classification
4.4. Significant Influence of Age on AO/OTA Classification
4.5. Fracture Mapping
4.6. Applications of Research
4.7. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CT | Computed Tomography |
| ORIF | Open reduction internal fixation |
| AO | Arbeitsgemeinschaft für Osteosynthesefragen |
| OTA | Orthopaedic Trauma Association |
References
- Gwinner, C.; Märdian, S.; Schwabe, P.; Schaser, K.-D.; Krapohl, B.D.; Jung, T.M. Current concepts review: Fractures of the patella. GMS Interdiscip. Plast. Reconstr. Surg. DGPW 2016, 5, Doc01. [Google Scholar] [CrossRef]
- Henrichsen, J.L.; Wilhem, S.K.; Siljander, M.P.; Kalma, J.J.; Karadsheh, M.S. Treatment of Patella Fractures. Orthopedics 2018, 41, E747–E755. [Google Scholar] [CrossRef] [PubMed]
- Howatt, J.; Liew, A.S.; Wilkin, G. Patellar Fractures. J. Bone Jt. Surg. 2021, 103, 2237–2246. [Google Scholar] [CrossRef] [PubMed]
- Melvin, S.J.; Mehta, S. Patellar Fractures in Adults. J. Am. Acad. Orthop. Surg. 2011, 19, 198–207. [Google Scholar] [CrossRef] [PubMed]
- Müller, E.C.; Frosch, K.-H. Patellafrakturen. Chirurg 2019, 90, 243–254. [Google Scholar] [CrossRef]
- Fehske, K.; Berninger, M.T.; Alm, L.; Hoffmann, R.; Zellner, J.; Kösters, C.; Barzen, S.; Raschke, M.J.; Izadpanah, K.; Herbst, E.; et al. Aktueller Versorgungsstandard von Patellafrakturen in Deutschland. Unfallchirurg 2020, 124, 832–838. [Google Scholar] [CrossRef]
- Schüttrumpf, J.P.; Stürmer, K.M.; Piatek, S. S2e-Leitlinie “Patellafraktur”. Chirurgie 2022, 93, 1106. [Google Scholar] [CrossRef]
- Berninger, M.T.; Frosch, K.-H. Wandel in der Behandlung der Patellafrakturen. Unfallchirurgie 2022, 125, 518–526. [Google Scholar] [CrossRef]
- Hargett, D.I.; Sanderson, B.R.; Little, M.T. Patella Fractures: Approach to Treatment. J. Am. Acad. Orthop. Surg. 2021, 29, 244–253. [Google Scholar] [CrossRef]
- Byun, S.-E.; Shon, O.-J.; Sim, J.-A.; Joo, Y.-B.; Kim, J.-W.; Na, Y.-G.; Choi, W. Application of Three-Dimensional Computed Tomography Improved the Interrater Reliability of the AO/OTA Classification Decision in a Patellar Fracture. J. Clin. Med. 2021, 10, 3256. [Google Scholar] [CrossRef]
- Xie, X.; Zhan, Y.; Wang, Y.; Lucas, J.F.; Zhang, Y.; Luo, C. Comparative Analysis of Mechanism-Associated 3-Dimensional Tibial Plateau Fracture Patterns. J. Bone Jt. Surg. 2019, 102, 410–418. [Google Scholar] [CrossRef] [PubMed]
- Dreizin, D.; Edmond, T.; Zhang, T.; Sarkar, N.; Turan, O.; Nascone, J. CT of Periarticular Adult Knee Fractures: Classification and Management Implications. RadioGraphics 2024, 44, e240014. [Google Scholar] [CrossRef] [PubMed]
- Cole, P.A.; Mehrle, R.K.; Bhandari, M.M.; Zlowodzki, M. The Pilon Map. J. Orthop. Trauma 2013, 27, e152–e156. [Google Scholar] [CrossRef] [PubMed]
- Kerschbaum, M.; Tyczka, M.; Klute, L.; Heller, M.T.; Koch, M.; Popp, D.; Lang, S.; Alt, V.; Worlicek, M. The Tibial Plateau Map: Fracture Line Morphology of Intra-Articular Proximal Tibial Fractures. BioMed. Res. Int. 2021, 2021, 9920189. [Google Scholar] [CrossRef]
- Shi, B.Y.; Zukotynski, B.K.; Upfill-Brown, A.; Brodke, D.J.; Kelley, B.V.; Devana, S.K.; Mayer, E.N.; Shah, A.A.; Lee, C. Fracture Lines and Patterns in Intra-articular Distal Femur Fractures. J. Am. Acad. Orthop. Surg. 2024, 32, e1020–e1026. [Google Scholar] [CrossRef]
- Molenaars, R.J.; Mellema, J.J.; Doornberg, J.N.; Kloen, P. Tibial Plateau Fracture Characteristics: Computed Tomography Mapping of Lateral, Medial, and Bicondylar Fractures. J. Bone Jt. Surg. 2015, 97, 1512–1520. [Google Scholar] [CrossRef]
- The American College of Surgeons. Resources for Optimal Care of the Injured Patient (2022 Standards); The American College of Surgeons: Chicago, IL, USA, 2022. [Google Scholar]
- Marsh, J.L.; Slongo, T.F.; Agel, J.; Broderick, J.S.; Creevey, W.; DeCoster, T.A.; Prokuski, L.; Sirkin, M.S.; Ziran, B.; Henley, B.; et al. Fracture and dislocation classification compendium-2007: Orthopaedic Trauma Association classification, database and outcomes committee. J. Orthop. Trauma 2007, 21, S1–S6. [Google Scholar] [CrossRef]
- Lazaro, L.E.; Wellman, D.S.; Pardee, N.C.; Gardner, M.J.; Toro, J.B.; MacIntyre, N.R.; Helfet, D.L.; Lorich, D.G. Effect of Computerized Tomography on Classification and Treatment Plan for Patellar Fractures. J. Orthop. Trauma 2013, 27, 336–344. [Google Scholar] [CrossRef]
- Kruse, M.; Wolf, O.; Mukka, S.; Brüggemann, A. Epidemiology, classification and treatment of patella fractures: An observational study of 3194 fractures from the Swedish Fracture Register. Eur. J. Trauma Emerg. Surg. 2022, 48, 4727–4734. [Google Scholar] [CrossRef]
- Larsen, P.; Court-Brown, C.M.; Vedel, J.O.; Vistrup, S.; Elsoe, R. Incidence and Epidemiology of Patellar Fractures. Orthopedics 2016, 39, e1154–e1158. [Google Scholar] [CrossRef]
- Misir, A.; Kizkapan, T.B.; Uzun, E.; Oguzkaya, S.; Cukurlu, M.; Golgelioglu, F. Fracture Patterns and Comminution Zones in OTA/AO 34C Type Patellar Fractures. J. Orthop. Trauma 2020, 34, e159–e164. [Google Scholar] [CrossRef] [PubMed]
- Byun, S.-E.; Sim, J.-A.; Joo, Y.B.; Kim, J.W.; Choi, W.; Na, Y.G.; Shon, O.-J. Changes in patellar fracture characteristics: A multicenter retrospective analysis of 1596 patellar fracture cases between 2003 and 2017. Injury 2019, 50, 2287–2291. [Google Scholar] [CrossRef] [PubMed]
- Rau, Y.; Huynh, T.; Frosch, K.-H.; Schultz, C.; Schulz, A.-P. Developments in the epidemiology and surgical management of patella fractures in Germany. BMC Musculoskelet. Disord. 2023, 24, 83. [Google Scholar] [CrossRef] [PubMed]
- Tang, A.; Hashmi, A.; Pandit, V.; Joseph, B.; Kulvatunyou, N.; Vercruysse, G.; Zangbar, B.; Gries, L.; O’Keeffe, T.M.; Green, D.; et al. A critical analysis of secondary overtriage to a Level I trauma center. J. Trauma Acute Care Surg. 2014, 77, 969–973. [Google Scholar] [CrossRef]
- Würdemann, F.S.; Smeeing, D.P.J.; Ferree, S.; Nawijn, F.; Verleisdonk, E.J.M.M.; Leenen, L.P.H.; Houwert, R.M.; Hietbrink, F. Differentiation in an inclusive trauma system: Allocation of lower extremity fractures. World J. Emerg. Surg. 2018, 13, 18. [Google Scholar] [CrossRef]
- Sim, J.-A.; Joo, Y.B.; Choi, W.; Byun, S.-E.; Na, Y.G.; Shon, O.-J.; Kim, J.W. Patellar fractures in elderly patients: A multicenter computed tomography-based analysis. Arch. Orthop. Trauma Surg. 2020, 141, 1439–1445. [Google Scholar] [CrossRef]
- Almigdad, A.; Mustafa, A.; Alazaydeh, S.; Alshawish, M.; Mustafa, M.B.; Alfukaha, H. Bone Fracture Patterns and Distributions according to Trauma Energy. Adv. Orthop. 2022, 2022, 8695916. [Google Scholar] [CrossRef]
- Rosillo, I.; Germosen, C.; Agarwal, S.; Rawal, R.; Colon, I.; Bucovsky, M.; Kil, N.; Shane, E.; Walker, M. Patella fractures are associated with bone fragility—A retrospective study. J. Bone Miner. Res. 2024, 39, 1752–1761. [Google Scholar] [CrossRef]
- Cho, J.-W.; Yang, Z.; Lim, E.J.; Sakong, S.; Choi, W.; Son, W.S.; Kim, H.; Chang, A.S.; Lim, D.-Y.; Kim, Y.; et al. Multifragmentary patellar fracture has a distinct fracture pattern which makes coronal split, inferior pole, or satellite fragments. Sci. Rep. 2021, 11, 22836. [Google Scholar] [CrossRef]
- Wurm, S.; Augat, P.; Bühren, V. Biomechanical Assessment of Locked Plating for the Fixation of Patella Fractures. J. Orthop. Trauma 2015, 29, e305–e308. [Google Scholar] [CrossRef]
- Huang, D.; Teng, T.Z.J.; Razak, H.R.B.A. Metal vs. non-metal fixation methods for patellar fractures: A systematic review and meta-analysis of clinical and radiographic outcomes. J. Clin. Orthop. Trauma 2023, 47, 102314. [Google Scholar] [CrossRef] [PubMed]
- Chang, C.-H.; Shih, C.-A.; Kuan, F.-C.; Hong, C.-K.; Su, W.-R.; Hsu, K.-L. Surgical treatment of inferior pole fractures of the patella: A systematic review. J. Exp. Orthop. 2023, 10, 58. [Google Scholar] [CrossRef] [PubMed]
- Filho, J.S.; Lenza, M.; Tamaoki, M.J.; Matsunaga, F.T.; Belloti, J.C. Interventions for treating fractures of the patella in adults. Cochrane Database Syst. Rev. 2021, 2021, CD009651. [Google Scholar] [CrossRef]
- Zhan, Y.; Zhang, Y.; Xie, X.; Luo, C. Three-dimensional fracture mapping of multi-fragmentary patella fractures (AO/OTA 34C3). Ann. Transl. Med. 2021, 9, 1364. [Google Scholar] [CrossRef]
- Dey, R. Mapping of Orthopaedic Fractures for Optimal Surgical Guidance. Exp. Med. Biol. 2023, 1392, 43–59. [Google Scholar] [CrossRef]
- Krause, M.; Frosch, K.-H.; Linke, P. Anterior plate osteosynthesis for multifragmentary patella fracture with additive stabilization of the distal pole using suture cerclage. Unfallchirurgie 2023, 126, 586–590. [Google Scholar] [CrossRef]
- Bickel, S.; Jensen, K.O.; Klingebiel, F.K.-L.; Teuben, M.P.J.; Pfeifer, R.; Pape, H.-C.; Hierholzer, C.; Kalbas, Y. Clinical and functional outcomes of locked plating vs. cerclage compression wiring for AO type C patellar fractures—A retrospective single-center cohort study. Eur. J. Trauma Emerg. Surg. 2024, 50, 2975–2985. [Google Scholar] [CrossRef]
- Mensel, C.; Gundtoft, P.H.; Brink, O. Preoperative templating in orthopaedic fracture surgery: The past, present and future. Injury 2022, 53, S42–S46. [Google Scholar] [CrossRef]
- Liu, J.; Zhang, Z.; Qu, J.; Piao, C. Progress of fracture mapping technology based on CT three-dimensional reconstruction. Front. Bioeng. Biotechnol. 2024, 12, 1471470. [Google Scholar] [CrossRef]
- von Rüden, C.; Trapp, O.; Augat, P.; Stuby, F.M.; Friederichs, J. Evolution of imaging in surgical fracture management. Injury 2020, 51, S51–S56. [Google Scholar] [CrossRef]
| AO/OTA Classification | 1 | 2 | 3 | Total |
|---|---|---|---|---|
| A | 22 (9.3%) | 15 (6.3%) | 37 (15.6%) | |
| B | 42 (17.7%) | 29 (12.2%) | 71 (29.9%) | |
| C | 41 (17.3%) | 36 (15.2%) | 52 (21.9%) | 129 (54.4%) |
| Total | 237 (100%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lenz, J.E.; Schraag, A.D.; Plank, L.; von Rüden, C.; Alt, V.; Weber, J. Mapping of Patellar Fracture Patterns: A Multicenter Study of 237 Patients. J. Clin. Med. 2025, 14, 1335. https://doi.org/10.3390/jcm14041335
Lenz JE, Schraag AD, Plank L, von Rüden C, Alt V, Weber J. Mapping of Patellar Fracture Patterns: A Multicenter Study of 237 Patients. Journal of Clinical Medicine. 2025; 14(4):1335. https://doi.org/10.3390/jcm14041335
Chicago/Turabian StyleLenz, Julia Elisabeth, Amadeus Dominik Schraag, Luis Plank, Christian von Rüden, Volker Alt, and Johannes Weber. 2025. "Mapping of Patellar Fracture Patterns: A Multicenter Study of 237 Patients" Journal of Clinical Medicine 14, no. 4: 1335. https://doi.org/10.3390/jcm14041335
APA StyleLenz, J. E., Schraag, A. D., Plank, L., von Rüden, C., Alt, V., & Weber, J. (2025). Mapping of Patellar Fracture Patterns: A Multicenter Study of 237 Patients. Journal of Clinical Medicine, 14(4), 1335. https://doi.org/10.3390/jcm14041335








