Mechanical Stability and Clinical Outcomes Following Posterior Cervical Fusion Surgery Using C3-6 Lateral Mass Screw Fixation: En Bloc Versus Regional Screw Fixation
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
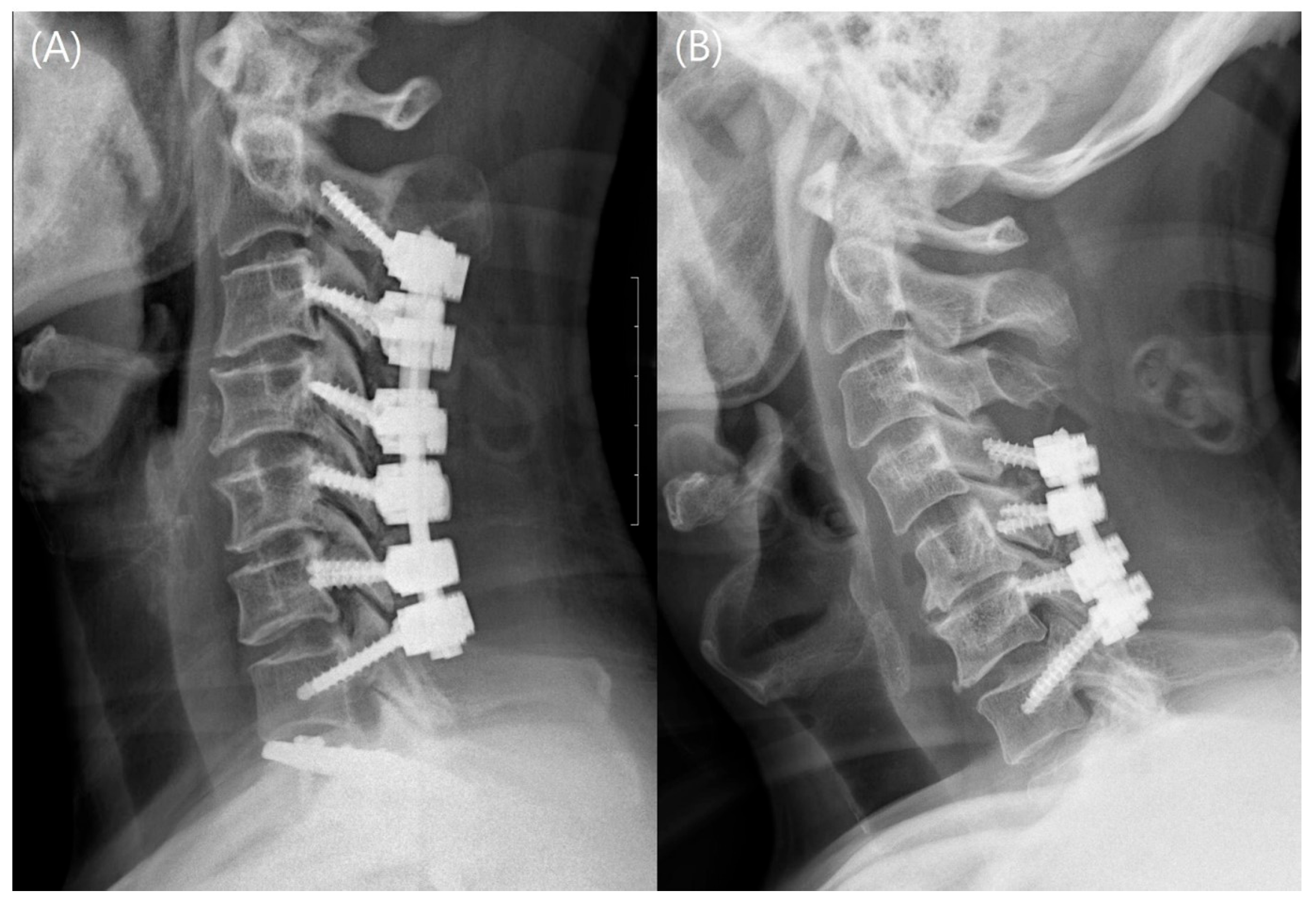
2.2. Surgical Procedures and Postoperative Management
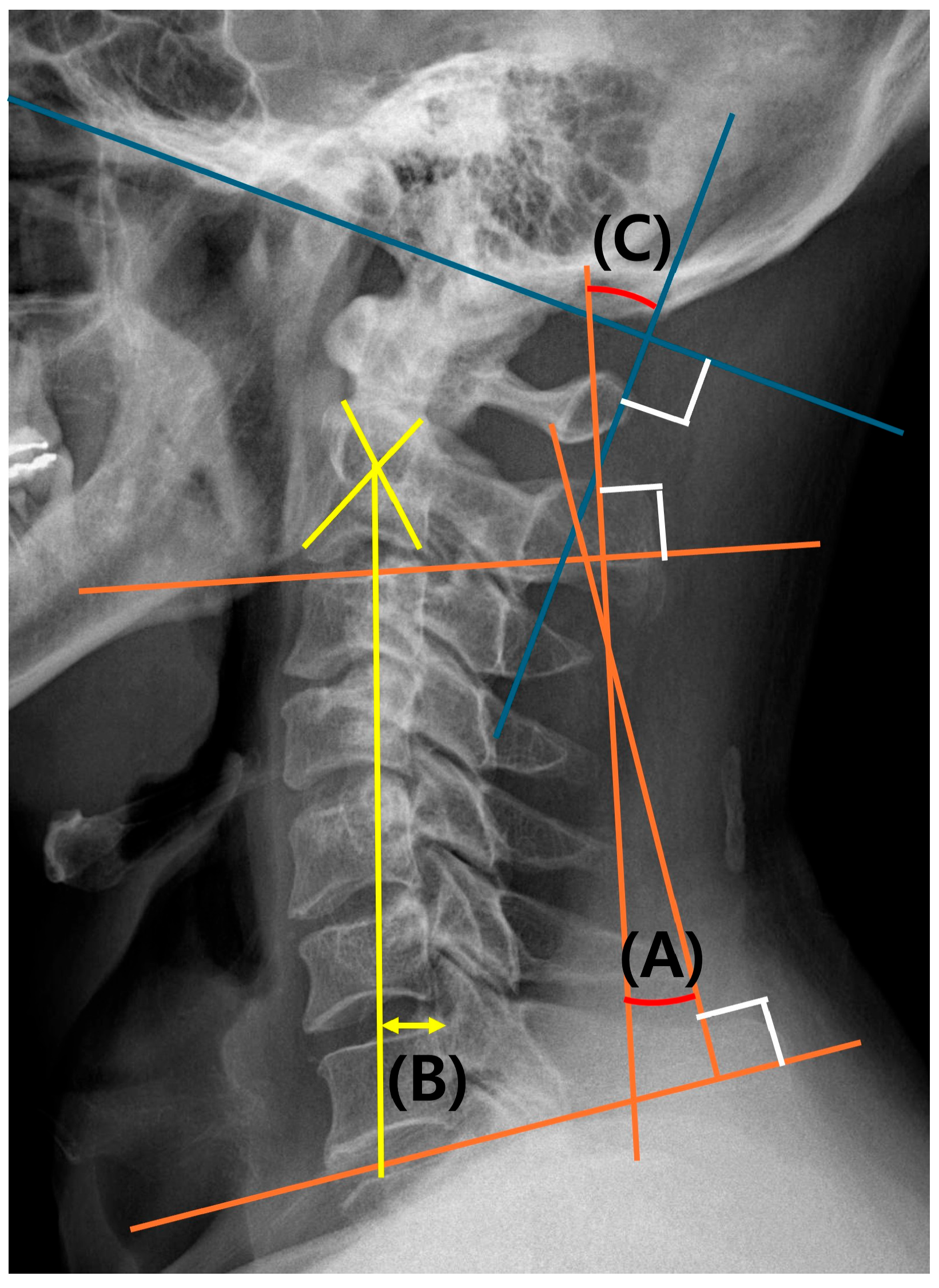
2.3. Radiological Analysis
2.3.1. Evaluation of Fusion-Related Complications
2.3.2. Evaluation of Cervical Alignment
2.4. Clinical Outcomes and Functional Scores
2.5. Statistical Analyses
3. Results
3.1. Demographics and Operative Factors
3.2. Radiological Factors
3.2.1. Fusion-Related Complications
3.2.2. Cervical Alignment
3.3. Clinical Outcomes and Functional Scores
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kim, M.W.; Park, Y.-S.; Kang, C.-N.; Choi, S.H. Cervical spondylotic myelopathy and radiculopathy: A stepwise approach and comparative analysis of surgical outcomes: A narrative review of recent literature. Asian Spine J. 2025; online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Herkowitz, H.N. A comparison of anterior cervical fusion, cervical laminectomy, and cervical laminoplasty for the surgical management of multiple level spondylotic radiculopathy. Spine 1988, 13, 774–780. [Google Scholar] [CrossRef] [PubMed]
- Simon, M.D.; Amoroso, D.; Iaconetta, G. Letter to the Editor Regarding “Does Bone Preservation at the Anterior Edge of the Vertebral Body Affect the Subsidence of Zero-profile Cages After Anterior Cervical Discectomy and Fusion”? World Neurosurg. 2025, 195, 123665. [Google Scholar]
- Anderson, P.A.; Matz, P.G.; Groff, M.W.; Heary, R.F.; Holly, L.T.; Kaiser, M.G.; Mummaneni, P.V.; Ryken, T.C.; Choudhri, T.F.; Vresilovic, E.J.; et al. Laminectomy and fusion for the treatment of cervical degenerative myelopathy. J. Neurosurg. Spine 2009, 11, 150–156. [Google Scholar] [CrossRef] [PubMed]
- Khadivi, M.; Moghadam, N.; Saghebdoust, S.; Khan, F.M.Y.; Eslamian, M.; Jouibari, M.F.; Shafizadeh, M.; Moosavi, M.; Zarei, M.; Kordi, R.; et al. The Impact of Rigid Cervical Collars on Outcome of Patients Who Underwent Posterior Cervical Laminectomy and Fusion: A Retrospective Comparative Study. Asian Spine J. 2023, 17, 322–329. [Google Scholar] [CrossRef]
- Truumees, E.; Singh, D.; Geck, M.J.; Stokes, J.K. Should long-segment cervical fusions be routinely carried into the thoracic spine? A multicenter analysis. Spine J. 2018, 18, 782–787. [Google Scholar] [CrossRef]
- Yoshihara, H.; Passias, P.G.; Errico, T.J. Screw-related complications in the subaxial cervical spine with the use of lateral mass versus cervical pedicle screws: A systematic review. J. Neurosurg. Spine 2013, 19, 614–623. [Google Scholar] [CrossRef]
- Kim, S.-H.; Seo, W.-D.; Kim, K.-H.; Yeo, H.-T.; Choi, G.-H.; Kim, D.-H. Clinical outcome of modified cervical lateral mass screw fixation technique. J. Korean Neurosurg. Soc. 2012, 52, 114–119. [Google Scholar] [CrossRef]
- Barbarawi, M.M.A.; Allou, M.Z. Cervical lateral mass screw-rod fixation: Surgical experience with 2500 consecutive screws, and anlytical review, and long-term outcomes. Br. J. Neurosurg. 2015, 29, 699–704. [Google Scholar] [CrossRef]
- Nagashima, K.; Koda, M.; Abe, T.; Kumagai, H.; Miura, K.; Fujii, K.; Noguchi, H.; Funayama, T.; Miyamoto, T.; Mannoji, C.; et al. Implant failure of pedicle screws in long-segment posterior cervical fusion is likely to occur at C7 and is avoidable by concomitant C6 or T1 buttress pedicle screws. J. Clin. Neurosci. 2019, 63, 106–109. [Google Scholar] [CrossRef]
- Fayed, I.; Toscano, D.T.; Triano, M.J.; Makariou, E.; Lee, C.; Spitz, S.M.; Anaizi, A.N.; Nair, M.N.; Sandhu, F.A.; Voyadzis, J.M. Crossing the Cervicothoracic Junction During Posterior Cervical Decompression and Fusion: Is It Necessary? Neurosurgery 2020, 86, E544–E550. [Google Scholar] [CrossRef] [PubMed]
- Hines, K.; Wilt, Z.T.; Franco, D.; Mahtabfar, A.; Elmer, N.; Gonzalez, G.A.; Montenegro, T.S.; Velagapudi, L.; Patel, P.D.; Detweiler, M.; et al. Long-segment posterior cervical decompression and fusion: Does caudal level affect revision rate? J. Neurosurg. Spine 2021, 35, 1–7. [Google Scholar] [CrossRef] [PubMed]
- An, H.S.; Gordin, R.; Renner, K. Anatomic considerations for plate-screw fixation of the cervical spine. Spine 1991, 16, S548–S551. [Google Scholar] [CrossRef] [PubMed]
- Shabana, A.M.M.; Hanafy, A.F.; Yamany, A.S.; Ashour, R.S. Effect of core stabilization exercises on cervical sagittal balance parameters in patients with forward head posture: A randomized controlled trial in Egypt. Asian Spine J. 2025. [Google Scholar] [CrossRef] [PubMed]
- Tan, L.A.; Riew, K.D.; Traynelis, V.C. Cervical Spine Deformity-Part 1: Biomechanics, Radiographic Parameters, and Classification. Neurosurgery 2017, 81, 197–203. [Google Scholar] [CrossRef]
- Nichols, N.M.; Jamieson, A.; Wang, M.; Chou, D.; Mummaneni, P.V.; Tan, L.A. Characterizing the fusion order and level-specific rates of arthrodesis in 3-level anterior cervical discectomy and fusion: A radiographic study. J. Clin. Neurosci. 2020, 81, 328–333. [Google Scholar] [CrossRef]
- Lee, D.H.; Cho, J.H.; Hwang, C.J.; Lee, C.S.; Cho, S.K.; Kim, C.; Ha, J.K. What Is the Fate of Pseudoarthrosis Detected 1 Year After Anterior Cervical Discectomy and Fusion? Spine 2018, 43, E23–E28. [Google Scholar] [CrossRef]
- Laratta, J.L.; Reddy, H.P.; Bratcher, K.R.; McGraw, K.E.; Carreon, L.Y.; RKirk Owens, I.I. Outcomes and revision rates following multilevel anterior cervical disecectomy and fusion. J. Spine Surg. 2018, 4, 496–500. [Google Scholar] [CrossRef]
- Ito, Z.; Higashino, K.; Kato, S.; Kim, S.S.; Wong, E.; Yoshioka, K.; Hutton, W.C. Pedicle Screws Can be 4 Times Stronger Than Lateral Mass Screws for Insertion in the Micervical Spine: A Biomechanical Study on Strength of Fixation. J. Spinal Disord. Tech. 2014, 27, 80–85. [Google Scholar] [CrossRef]
- Kwon, J.W.; Bang, S.H.; Park, T.H.; Lee, S.J.; Lee, H.M.; Lee, S.B.; Lee, B.H.; Moon, S.H. Biomechanical comparison of cervical disecectomy/fusion model using allograft spacers between anterior and posterior fixation methods (lateral mass and pedicle screw). Clin. Biomech. 2020, 73, 226–233. [Google Scholar] [CrossRef]
- Punyarat, P.; Buchowski, J.M.; Klawson, B.T.; Peters, C.; Lertudomphonwanit, T.; Riew, K.D. Freehand technique for C2 pedicle and pars screw placement: Is it safe? Spine J. 2018, 18, 1197–1203. [Google Scholar] [CrossRef] [PubMed]
- Clifton, W.; Louie, C.; Williams, D.B.; Damon, A.; Dove, C.; Pichelmann, M. Safety and Accuracy of the Freehand Placement of C7 Pedicle Screws in Cervical and Cervicothoracic Constructs. Cureus 2019, 11, e5304. [Google Scholar] [CrossRef] [PubMed]
- Park, M.S.; Mesfin, A.; Stoker, G.E.; Song, K.S.; Kennedy, C.; Riew, K.D. Sagittal range of motion after extensive cerical fusion. Spine J. 2014, 14, 338–343. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.H.; Cho, J.H.; Jung, J.I.; Baik, J.M.; Jun, D.S.; Hwang, C.J.; Lee, C.S. Does stopping at C7 in long posterior cervical fusion accelerate the symptomatic breakdown of cervicothoracic junction? PLoS ONE 2019, 14, e0217792. [Google Scholar] [CrossRef]

| Parameter | EBF Group | RF Group | p-Value |
|---|---|---|---|
| (n = 116) | (n = 62) | ||
| Age | 63.7 ± 12.4 | 60.0 ± 12.8 | 0.192 |
| Sex | 1.000 | ||
| Male | 72 (62.1%) | 40 (64.5%) | |
| Female | 44 (37.9%) | 22 (35.5%) | |
| BMI | 25.4 ± 4.4 | 25.8 ± 4.1 | 0.721 |
| BMD (spine) | 0.68 ± 0.38 | 0.78 ± 0.35 | 0.254 |
| Smoking | 16 (13.7%) | 12 (19.3%) | 0.547 |
| HTN | 48 (41.4%) | 22 (35.5%) | 0.317 |
| DM | 18 (15.5%) | 12 (19.4%) | 0.192 |
| Malignancy | 4 (3.4%) | 0 (0.0%) | 0.713 |
| Decompression levels | 4.2 ± 0.5 | 3.6 ± 0.4 | <0.001 * |
| Fusion levels | 6.0 | 4.4 ± 0.5 | <0.001 * |
| - 4 levels (C2-3-4-5) | 0 | 4 (6.5) | |
| - 4 levels (C3-4-5-6) | 0 | 27 (43.5) | |
| - 4 levels (C4-5-6-7) | 0 | 3 (4.8) | |
| - 5 levels (C2-3-4-5-6) | 0 | 9 (14.5) | |
| - 5 levels (C3-4-5-6-7) | 0 | 19 (30.7) | |
| - 6 levels (C2-3-4-5-6-7) | 116 (100.0) | 0 | |
| Mean lateral mass screw length | 13.8 ± 1.1 | 14.3 ± 1.1 | 0.097 |
| Mean pedicle screw length | 26.2 ± 3.1 | 27.2 ± 2.2 | 0.854 |
| Iliac crest bone graft | 34 (29.3%) | 12 (19.4%) | 0.725 |
| Follow-up (m) | 42.5 ± 16.6 | 41.6 ± 18.0 | 0.812 |
| EBF Group n = 116 | RF Group n = 62 | p-Value | |||
|---|---|---|---|---|---|
| Preoperative | Lordosis (C2-C7) | Degree | −9.7 ± 11.1 | −13.2 ± 11.1 | 0.171 |
| Range of motion | Degree | 49.4 ± 15.6 | 52.8 ± 16.7 | 0.363 | |
| C2-C7 SVA | mm | 19.7 ± 18.0 | 24.3 ± 19.5 | 0.137 | |
| Postoperative, 1 year | Lordosis (C2-C7) | Degree | −16.9 ± 8.5 | −12.3 ± 10.5 | 0.034 * |
| Change | −7.2 ± 13.3 | 0.9 ± 10.1 | <0.001 * | ||
| p-value | <0.001 * | 0.634 | |||
| Range of motion | Degree | 30.6 ± 13.7 | 43.1 ± 16.1 | <0.001 | |
| Change | −18.9 ± 14.6 | −9.8 ± 16.5 | 0.001 | ||
| p-value | <0.001 * | <0.001 * | |||
| C2-C7 SVA | mm | 25.5 ± 15.7 | 24.3 ± 13.2 | 0.724 | |
| Change | 5.7 ± 10.9 | −0.1 ± 15.7 | 0.047 * | ||
| p-value | <0.001 * | 0.915 | |||
| Final follow-up | Lordosis (C2-C7) | Degree | −14.2 ± 10.4 | −12.8 ± 10.3 | 0.553 |
| Change | −4.3 ± 13.9 | 0.4 ± 12.2 | 0.115 | ||
| p-value | 0.027 * | 0.863 | |||
| Range of motion | Degree | 27.1 ± 13.3 | 40.8 ± 15.8 | <0.001 * | |
| Change | −22.1 ± 14.7 | −12.3 ± 16.9 | <0.001 * | ||
| p-value | <0.001 * | <0.001 * | |||
| C2-C7 SVA | mm | 27.7 ± 19.3 | 23.7 ± 14.1 | 0.324 | |
| Change | 7.9 ± 16.5 | −0.6 ± 6.3 | 0.027 * | ||
| p-value | <0.001 * | 0.627 | |||
| Fusion, complications | Fusion (radiograph) | 110 (94.8%) | 48 (77.4%) | 0.038 * | |
| Fusion (CT) | 110 (94.8%) | 48 (77.4%) | 0.038 * | ||
| Mechanical failure | 8 (6.9%) | 16 (25.8%) | 0.047 * | ||
| - Screw loosening | 4 (3.4%) | 14 (22.6%) | <0.001 * | ||
| - Screw broken | 4 (3.4%) | 2 (3.2%) | 1.000 | ||
| ASD | 6 (5.1%) | 2 (3.2%) | 1.000 | ||
| EBF Group n = 116 | RF Group n = 62 | p-Value | |||
|---|---|---|---|---|---|
| Preoperative | Neck pain | VAS score | 4.0 ± 2.7 | 4.8 ± 3.0 | 0.187 |
| Arm pain | VAS score | 4.7 ± 2.9 | 4.4 ± 2.7 | 0.633 | |
| NDI | Score | 18.8 ± 7.5 | 19.6 ± 7.7 | 0.644 | |
| Postoperative, 1 year | Neck pain | VAS score | 2.4 ± 2.2 | 3.2 ± 2.6 | 0.152 |
| Change | −1.6 ± 2.7 | −1.7 ± 3.5 | 0.891 | ||
| p-value | <0.001 * | <0.001 * | |||
| Arm pain | VAS score | 3.1 ± 2.7 | 3.1 ± 2.8 | 0.993 | |
| Change | −1.5 ± 3.1 | −1.3 ± 3.2 | 0.688 | ||
| p-value | <0.001 * | <0.001 * | |||
| NDI | Score | 13.3 ± 7.3 | 13.5 ± 7.6 | 0.914 | |
| Change | −5.5 ± 6.1 | −6.0 ± 7.3 | 0.736 | ||
| p-value | <0.001 * | <0.001 * | |||
| Final follow-up | Neck pain | VAS score | 2.6 ± 2.1 | 2.8 ± 2.4 | 0.595 |
| Change | −1.5 ± 2.0 | −2.0 ± 3.3 | 0.435 | ||
| p-value | <0.001 * | <0.001 * | |||
| Arm pain | VAS score | 3.2 ± 2.6 | 3.1 ± 2.3 | 0.846 | |
| Change | −1.4 ± 3.7 | −1.3 ± 3.1 | 0.813 | ||
| p-value | <0.001 * | <0.001 * | |||
| NDI | Score | 12.4 ± 6.2 | 12.9 ± 7.4 | 0.717 | |
| Change | −6.4 ± 8.0 | −6.6 ± 7.4 | 0.893 | ||
| p-value | <0.001 * | <0.001 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, D.-H.; Seok, S.Y.; Lee, W.S.; Lee, H.R.; Park, S.; Hwang, C.J.; Cho, J.H. Mechanical Stability and Clinical Outcomes Following Posterior Cervical Fusion Surgery Using C3-6 Lateral Mass Screw Fixation: En Bloc Versus Regional Screw Fixation. J. Clin. Med. 2025, 14, 1185. https://doi.org/10.3390/jcm14041185
Lee D-H, Seok SY, Lee WS, Lee HR, Park S, Hwang CJ, Cho JH. Mechanical Stability and Clinical Outcomes Following Posterior Cervical Fusion Surgery Using C3-6 Lateral Mass Screw Fixation: En Bloc Versus Regional Screw Fixation. Journal of Clinical Medicine. 2025; 14(4):1185. https://doi.org/10.3390/jcm14041185
Chicago/Turabian StyleLee, Dong-Ho, Sang Yun Seok, Woon Sang Lee, Hyung Rae Lee, Sehan Park, Chang Ju Hwang, and Jae Hwan Cho. 2025. "Mechanical Stability and Clinical Outcomes Following Posterior Cervical Fusion Surgery Using C3-6 Lateral Mass Screw Fixation: En Bloc Versus Regional Screw Fixation" Journal of Clinical Medicine 14, no. 4: 1185. https://doi.org/10.3390/jcm14041185
APA StyleLee, D.-H., Seok, S. Y., Lee, W. S., Lee, H. R., Park, S., Hwang, C. J., & Cho, J. H. (2025). Mechanical Stability and Clinical Outcomes Following Posterior Cervical Fusion Surgery Using C3-6 Lateral Mass Screw Fixation: En Bloc Versus Regional Screw Fixation. Journal of Clinical Medicine, 14(4), 1185. https://doi.org/10.3390/jcm14041185





