Stress, Anxiety and Depressive Symptoms, Burnout and Insomnia Among Greek Nurses One Year After the End of the Pandemic: A Moderated Chain Mediation Model
Abstract
1. Introduction
2. Materials and Methods
2.1. Research Design
2.2. Study Participants
2.3. Ethical Considerations
2.4. Measurement Tools
2.4.1. Depression Anxiety Stress Scale (DASS-21)
2.4.2. Copenhagen Burnout Inventory (CBI)
2.4.3. Athens Insomnia Scale (AIS)
2.5. Statistical Analysis
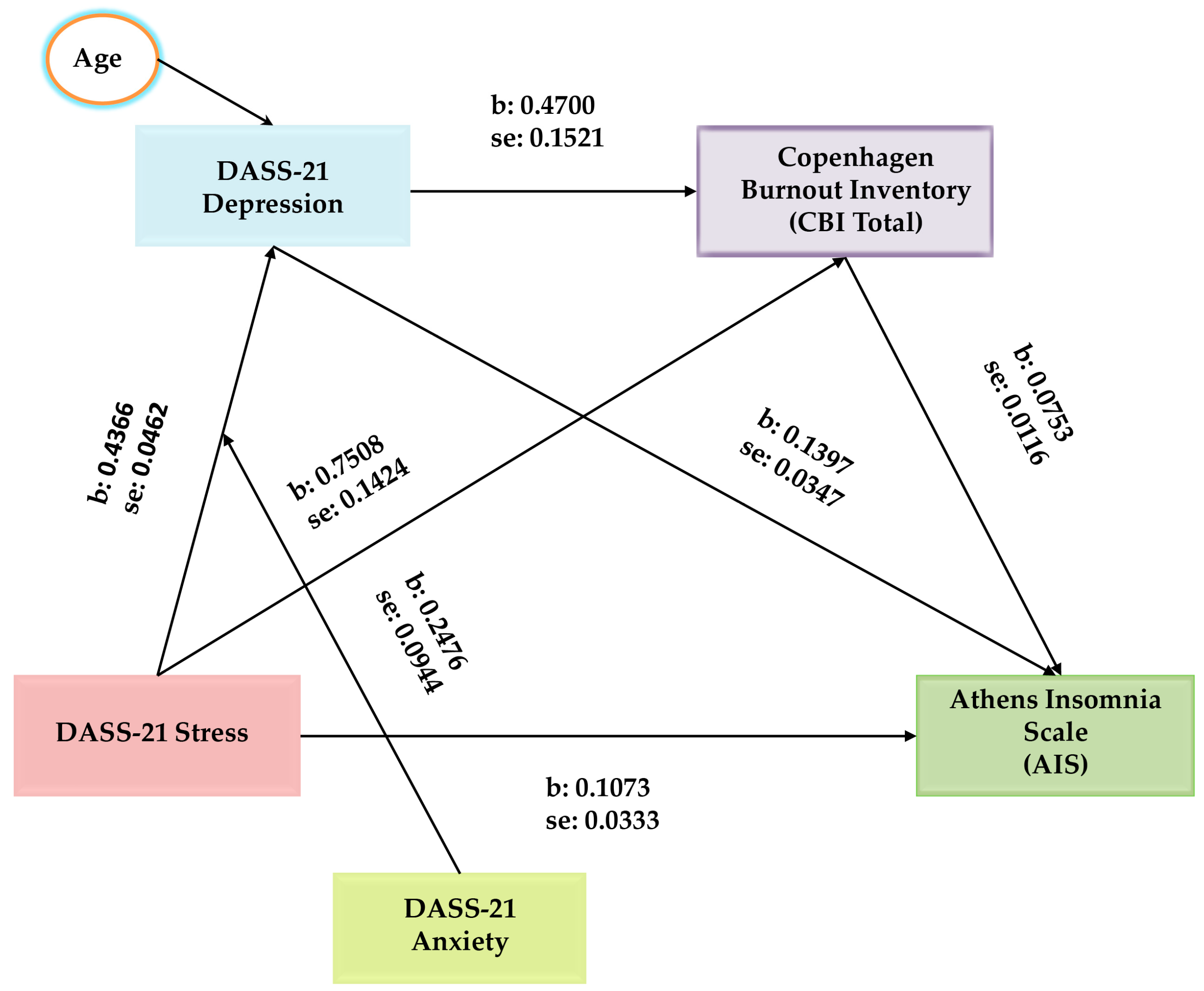
3. Results
4. Discussion
4.1. The Influence of Stress on Insomnia
4.2. The Mediating Role of Depressive Symptoms
4.3. The Mediating Role of Burnout
4.4. The Chain Mediating Role of Depressive Symptoms and Burnout
4.5. The Moderating Role of Anxiety Symptoms
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO Statement (31 January 2020). “Statement on the Second Meeting of the International Health Regulations (2005) Emergency Committee Regarding the Outbreak of Novel Coronavirus (2019-nCoV)”; World Health Organization: Geneva, Switzerland, 2020.
- WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19—11 March 2020; World Health Organization: Geneva, Switzerland, 2020.
- Statement on the Fifteenth Meeting of the International Health Regulations (2005) Emergency Committee Regarding the Coronavirus Disease (COVID-19) Pandemic. Available online: https://www.who.int/news/item/05-05-2023-statement-on-the-fifteenth-meeting-of-the-international-health-regulations-%282005%29-emergency-committee-regarding-the-coronavirus-disease-%28covid-19%29-pandemic (accessed on 5 May 2023).
- Mofijur, M.; Fattah, I.M.R.; Alam, M.A.; Islam, A.S.; Ong, H.; Rahman, S.M.; Najafi, G.; Ahmed, S.; Uddin, M.A.; Mahlia, T.M. Impact of COVID-19 on the social, economic, environmental and energy domains: Lessons learnt from a global pandemic. Sustain. Prod. Consum. 2021, 26, 343–359. [Google Scholar] [CrossRef] [PubMed]
- Saladino, V.; Algeri, D.; Auriemma, V. The Psychological and Social Impact of COVID-19: New Perspectives of Well-Being. Front. Psychol. 2020, 11, 577684. [Google Scholar] [CrossRef]
- Marzo, R.R.; Ismail, Z.; Nu Htay, M.N.; Bahari, R.; Ismail, R.; Villanueva, E.Q., III; Singh, A.; Lotfizadeh, M.; Respati, T.; Irasanti, S.N.; et al. Psychological distress during pandemic COVID-19 among adult general population: Result across 13 countries. Clin. Epidemiol. Glob. Health 2021, 10, 100708. [Google Scholar] [CrossRef]
- Jaber, M.J.; AlBashaireh, A.M.; AlShatarat, M.H.; Alqudah, O.M.; Du Preez, S.E.; AlGhamdi, K.S.; AlTmaizy, H.M.; Abo Dawass, M.A. Stress, depression, anxiety, and burnout among healthcare workers during the COVID-19 pandemic: A cross-sectional study in a tertiary centre. Open Nurs. J. 2022, 16, 1–13. [Google Scholar] [CrossRef]
- Kunz, M.; Strasser, M.; Hasan, A. Impact of the coronavirus disease 2019 pandemic on healthcare workers: Systematic comparison between nurses and medical doctors. Curr. Opin. Psychiatry 2021, 34, 413–419. [Google Scholar] [CrossRef] [PubMed]
- Imes, C.C.; Tucker, S.J.; Trinkoff, A.M.; Chasens, E.R.; Weinstein, S.M.; Dunbar-Jacob, J.; Patrician, P.A.; Redeker, N.S.; Baldwin, C.M. Wake-up call: Night shifts adversely affect nurse health and retention, patient and public safety, and costs. Nurs. Adm. Q. 2023, 47, E38–E53. [Google Scholar] [CrossRef] [PubMed]
- Sagherian, K.; Cho, H.; Steege, L.M. The insomnia, fatigue, and psychological well-being of hospital nurses 18 months after the COVID-19 pandemic began: A cross-sectional study. J. Clin. Nurs. 2024, 33, 273–287. [Google Scholar] [CrossRef]
- Janatolmakan, M.; Naghipour, A.; Khatony, A. Prevalence and factors associated with poor sleep quality among nurses in COVID-19 wards. Sci. Rep. 2024, 14, 16616. [Google Scholar] [CrossRef]
- Norful, A.A.; Haghighi, F.; Shechter, A. Assessing sleep health dimensions in frontline registered nurses during the COVID-19 pandemic: Implications for psychological health and wellbeing. Sleep Adv. 2022, 4, zpac046. [Google Scholar] [CrossRef]
- Huang, Q.; Tian, C.; Zeng, X.T. Poor Sleep Quality in Nurses Working or Having Worked Night Shifts: A Cross-Sectional Study. Front. Neurosci. 2021, 15, 638973. [Google Scholar] [CrossRef]
- Chung, Y.; Kim, H.; Koh, D.H.; Park, J.H.; Yoon, S. Relationship Between Shift Intensity and Insomnia Among Hospital Nurses in Korea: A Cross-sectional Study. J. Prev. Med. Public Health 2021, 54, 46–54. [Google Scholar] [CrossRef] [PubMed]
- Kalmbach, D.A.; Anderson, J.R.; Drake, C.L. The impact of stress on sleep: Pathogenic sleep reactivity as a vulnerability to insomnia and circadian disorders. J. Sleep Res. 2018, 27, e12710. [Google Scholar] [CrossRef] [PubMed]
- Tselebis, A.; Lekka, D.; Sikaras, C.; Tsomaka, E.; Tassopoulos, A.; Ilias, I.; Bratis, D.; Pachi, A. Insomnia, Perceived Stress, and Family Support among Nursing Staff during the Pandemic Crisis. Healthcare 2020, 8, 434. [Google Scholar] [CrossRef] [PubMed]
- Sikaras, C.; Tsironi, M.; Zyga, S.; Panagiotou, A. Anxiety, insomnia and family support in nurses, two years after the onset of the pandemic crisis. AIMS Public Health 2023, 10, 252–267. [Google Scholar] [CrossRef] [PubMed]
- Peng, P.; Liang, M.; Wang, Q.; Lu, L.; Wu, Q.; Chen, Q. Night shifts, insomnia, anxiety, and depression among Chinese nurses during the COVID-19 pandemic remission period: A network approach. Front. Public Health 2022, 10, 1040298. [Google Scholar] [CrossRef] [PubMed]
- Bennaroch, K.; Shochat, T. Psychobiological risk factors for insomnia and depressed mood among hospital female nurses working shifts. Front. Sleep 2023, 2, 1206101. [Google Scholar] [CrossRef]
- Sagherian, K.; Steege, L.M.; Cobb, S.J.; Cho, H. Insomnia, fatigue and psychosocial well-being during COVID-19 pandemic: A cross-sectional survey of hospital nursing staff in the United States. J. Clin. Nurs. 2023, 32, 5382–5395. [Google Scholar] [CrossRef] [PubMed]
- Oh, C.M.; Kim, H.Y.; Na, H.K.; Cho, K.H.; Chu, M.K. The Effect of Anxiety and Depression on Sleep Quality of Individuals With High Risk for Insomnia: A Population-Based Study. Front. Neurol. 2019, 10, 849. [Google Scholar] [CrossRef]
- Rudman, A.; Arborelius, L.; Dahlgren, A.; Finnes, A.; Gustavsson, P. Consequences of early career nurse burnout: A prospective long-term follow-up on cognitive functions, depressive symptoms, and insomnia. EClinicalMedicine 2020, 27, 100565. [Google Scholar] [CrossRef]
- Zhang, X.; Zhang, L. Risk prediction of sleep disturbance in clinical nurses: A nomogram and artificial neural network model. BMC Nurs. 2023, 22, 289. [Google Scholar] [CrossRef] [PubMed]
- Ye, L.; Zhang, F.; Wang, L.; Chen, Y.; Shi, J.; Cai, T. Identification of the risk factors for insomnia in nurses with long COVID-19. BMC Nurs. 2024, 23, 532. [Google Scholar] [CrossRef] [PubMed]
- Burn-Out an “Occupational Phenomenon”: International Classification of Diseases. Available online: https://www.who.int/news/item/28-05-2019-burn-out-an-occupational-phenomenon-international-classification-of-diseases (accessed on 9 November 2023).
- Quesada-Puga, C.; Izquierdo-Espin, F.J.; Membrive-Jiménez, M.J.; Aguayo-Estremera, R.; Cañadas-De La Fuente, G.A.; Romero-Béjar, J.L.; Gómez-Urquiza, J.L. Job satisfaction and burnout syndrome among intensive-care unit nurses: A systematic review and meta-analysis. Intensive Crit. Care Nurs. 2024, 82, 103660. [Google Scholar] [CrossRef]
- Friganović, A.; Selič, P.; Ilić, B.; Sedić, B. Stress and burnout syndrome and their associations with coping and job satisfaction in critical care nurses: A literature review. Psychiatr. Danub. 2019, 31 (Suppl. S1), 21–31. [Google Scholar]
- Freudenberger, H.J. Staff burn-out. J. Soc. Issues 1974, 30, 159–165. [Google Scholar] [CrossRef]
- Kousloglou, S.; Mouzas, O.; Bonotis, K.; Roupa, Z.; Vasilopoulos, A.; Angelopoulos, N. Insomnia and burnout in Greek Nurses. Hippokratia 2014, 18, 150–155. [Google Scholar] [PubMed] [PubMed Central]
- Bratis, D.; Tselebis, A.; Sikaras, C.; Moulou, A.; Giotakis, K.; Zoumakis, E.; Ilias, I. Alexithymia and its association with burnout, depression and family support among Greek nursing staff. Hum. Resour. Health 2009, 7, 72. [Google Scholar] [CrossRef]
- Sikaras, C.; Ilias, I.; Tselebis, A.; Pachi, A.; Zyga, S.; Tsironi, M.; Gil, A.P.R.; Panagiotou, A. Nursing staff fatigue and burnout during the COVID-19 pandemic in Greece. AIMS Public Health 2021, 9, 94–105. [Google Scholar] [CrossRef]
- Membrive-Jiménez, M.J.; Pradas-Hernández, L.; Suleiman-Martos, N.; Vargas-Román, K.; Cañadas-De la Fuente, G.A.; Gomez-Urquiza, J.L.; De la Fuente-Solana, E.I. Burnout in Nursing Managers: A Systematic Review and Meta-Analysis of Related Factors, Levels and Prevalence. Int. J. Environ. Res. Public Health 2020, 17, 3983. [Google Scholar] [CrossRef]
- Monsalve-Reyes, C.S.; San Luis-Costas, C.; Gómez-Urquiza, J.L.; Albendín-García, L.; Aguayo, R.; Cañadas-De la Fuente, G.A. Burnout syndrome and its prevalence in primary care nursing: A systematic review and meta-analysis. BMC Fam. Pract. 2018, 19, 59. [Google Scholar] [CrossRef] [PubMed]
- Pachi, A.; Sikaras, C.; Ilias, I.; Panagiotou, A.; Zyga, S.; Tsironi, M.; Baras, S.; Tsitrouli, L.A.; Tselebis, A. Burnout, Depression and Sense of Coherence in Nurses during the Pandemic Crisis. Healthcare 2022, 10, 134. [Google Scholar] [CrossRef] [PubMed]
- Stelnicki, A.M.; Jamshidi, L.; Angehrn, A.; Hadjistavropoulos, H.D.; Carleton, R.N. Associations Between Burnout and Mental Disorder Symptoms Among Nurses in Canada. Can. J. Nurs. Res. 2021, 53, 254–263. [Google Scholar] [CrossRef] [PubMed]
- Schonfeld, I.S.; Bianchi, R. Burnout and depression: Two entities or one? J. Clin. Psychol. 2016, 72, 22–37. [Google Scholar] [CrossRef] [PubMed]
- Iacovides, A.; Fountoulakis, K.N.; Kaprinis, S.; Kaprinis, G. The relationship between job stress, burnout and clinical depression. J. Affect. Disord. 2003, 75, 209–221. [Google Scholar] [CrossRef]
- Parker, G.; Tavella, G. Distinguishing burnout from clinical depression: A theoretical differentiation template. J. Affect. Disord. 2021, 281, 168–173. [Google Scholar] [CrossRef]
- Koutsimani, P.; Montgomery, A.; Georganta, K. The Relationship Between Burnout, Depression, and Anxiety: A Systematic Review and Meta-Analysis. Front. Psychol. 2019, 10, 284. [Google Scholar] [CrossRef]
- Noh, E.Y.; Park, Y.H.; Chai, Y.J.; Kim, H.J.; Kim, E. Frontline Nurses’ Burnout and its Associated Factors during the COVID-19 Pandemic in South Korea. Appl. Nurs. Res. 2022, 67, 151622. [Google Scholar] [CrossRef]
- Serrão, C.; Duarte, I.; Castro, L.; Teixeira, A. Burnout and Depression in Portuguese Healthcare Workers during the COVID-19 Pandemic—The Mediating Role of Psychological Resilience. Int. J. Environ. Res. Public Health 2021, 18, 636. [Google Scholar] [CrossRef] [PubMed]
- Mazure, C.M. Life stressors as risk factors in depression. Clin. Psychol. Sci. Pract. 1998, 5, 291–313. [Google Scholar] [CrossRef]
- Hammen, C. Stress and depression. Annu. Rev. Clin. Psychol. 2005, 1, 293–319. [Google Scholar] [CrossRef]
- Maslach, C.; Leiter, M.P. Understanding the burnout experience: Recent research and its implications for psychiatry. World Psychiatry 2016, 15, 103–111. [Google Scholar] [CrossRef] [PubMed]
- Kamal, A.M.; Ahmed, W.S.E.; Wassif, G.O.M.; Greda, M.H.A.A. Work Related Stress, Anxiety and Depression among School Teachers in general education. Qjm Int. J. Med. 2021, 114 (Suppl. S1), hcab118.003. [Google Scholar] [CrossRef]
- Wang, M.F.; Shao, P.; Wu, C.; Zhang, L.Y.; Zhang, L.F.; Liang, J.; Du, J. The relationship between occupational stressors and insomnia in hospital nurses: The mediating role of psychological capital. Front. Psychol. 2023, 13, 1070809. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, H.-F.; Liu, Y.; Hsu, H.-T.; Ma, S.C.; Wang, H.H.; Ko, C.H. Relations between Stress and Depressive Symptoms in Psychiatric Nurses: The Mediating Effects of Sleep Quality and Occupational Burnout. Int. J. Environ. Res. Public Health 2021, 18, 7327. [Google Scholar] [CrossRef] [PubMed]
- Al Maqbali, M.; Al Sinani, M.; Al-Lenjawi, B. Prevalence of stress, depression, anxiety and sleep disturbance among nurses during the COVID-19 pandemic: A systematic review and meta-analysis. J. Psychosom. Res. 2021, 141, 110343. [Google Scholar] [CrossRef]
- Ge, M.W.; Hu, F.H.; Jia, Y.J.; Tang, W.; Zhang, W.Q.; Chen, H.L. Global prevalence of nursing burnout syndrome and temporal trends for the last 10 years: A meta-analysis of 94 studies covering over 30 countries. J. Clin. Nurs. 2023, 32, 5836–5854. [Google Scholar] [CrossRef] [PubMed]
- Tao, R.; Wang, S.; Lu, Q.; Liu, Y.; Xia, L.; Mo, D.; Geng, F.; Liu, T.; Liu, Y.; Jiang, F.; et al. Interconnected mental health symptoms: Network analysis of depression, anxiety, stress, and burnout among psychiatric nurses in the context of the COVID-19 pandemic. Front. Psychiatry 2024, 15, 1485726. [Google Scholar] [CrossRef] [PubMed]
- Akova, İ.; Hasdemir, Ö.; Kiliç, E. Evaluation of the relationship between burnout, depression, anxiety, and stress levels of primary health-care workers (Center Anatolia). Alex. J. Med. 2021, 57, 52–60. [Google Scholar] [CrossRef]
- Kwee, C.; Dos Santos, L. The Relationships Between Sleep Disorders, Burnout, Stress and Coping Strategies of Health Professionals During the COVID-19 Pandemic: A Literature Review. Curr. Sleep Med. Rep. 2023, 9, 274–280. [Google Scholar] [CrossRef]
- Pachi, A.; Panagiotou, A.; Soultanis, N.; Ivanidou, M.; Manta, M.; Sikaras, C.; Ilias, I.; Tselebis, A. Resilience, Anger, and Insomnia in Nurses after the End of the Pandemic Crisis. Epidemiologia 2024, 5, 643–657. [Google Scholar] [CrossRef] [PubMed]
- Powell, M.A.; Oyesanya, T.O.; Scott, S.D.; Allen, D.H.; Walton, A. Beyond Burnout: Nurses’ Perspectives on Chronic Suffering During and After the COVID-19 Pandemic. Glob. Qual. Nurs. Res. 2024, 11, 1–11. [Google Scholar] [CrossRef]
- Grasmann, L.; Morawa, E.; Adler, W.; Schug, C.; Borho, A.; Geiser, F.; Beschoner, P.; Jerg-Bretzke, L.; Albus, C.; Weidner, K.; et al. Depression and anxiety among nurses during the COVID-19 pandemic: Longitudinal results over 2 years from the multicentre VOICE-EgePan study. J. Clin. Nurs. 2024; early view. [Google Scholar] [CrossRef]
- Ding, W.; Wang, M.Z.; Zeng, X.W.; Liu, Z.H.; Meng, Y.; Hu, H.T.; Zhang, Y.; Guan, Y.G.; Meng, F.G.; Zhang, J.G.; et al. Mental health and insomnia problems in healthcare workers after the COVID-19 pandemic: A multicenter cross-sectional study. World J. Psychiatry 2024, 14, 704–714. [Google Scholar] [CrossRef] [PubMed]
- Liu, D.; Zhou, Y.; Tao, X.; Cheng, Y.; Tao, R. Mental health symptoms and associated factors among primary healthcare workers in China during the post-pandemic era. Front. Public Health 2024, 12, 1374667. [Google Scholar] [CrossRef]
- Galanis, P.; Moisoglou, I.; Katsiroumpa, A.; Vraka, I.; Siskou, O.; Konstantakopoulou, O.; Meimeti, E.; Kaitelidou, D. Increased Job Burnout and Reduced Job Satisfaction for Nurses Compared to Other Healthcare Workers after the COVID-19 Pandemic. Nurs. Rep. 2023, 13, 1090–1100. [Google Scholar] [CrossRef]
- Xiao, J.; Liu, L.; Peng, Y.; Wen, Y.; Lv, X.; Liang, L.; Fan, Y.; Chen, J.; Chen, Y.; Hu, H.; et al. Anxiety, depression, and insomnia among nurses during the full liberalization of COVID-19: A multicenter cross-sectional analysis of the high-income region in China. Front. Public Health 2023, 11, 1179755. [Google Scholar] [CrossRef]
- Zhou, Y.; Gao, W.; Li, H.; Yao, X.; Wang, J.; Zhao, X. Network analysis of resilience, anxiety and depression in clinical nurses. BMC Psychiatry 2024, 24, 719. [Google Scholar] [CrossRef]
- Jager, J.; Putnick, D.L.; Bornstein, M.H. More than Just Convenient: The Scientific Merits of Homogeneous Convenience Samples. Monogr. Soc. Res. Child. Dev. 2017, 82, 13–30. [Google Scholar] [CrossRef]
- Cochran, W.G. Sampling Techniques, 2nd ed.; John Wiley and Sons, Inc.: New York, NY, USA, 1963. [Google Scholar]
- Khalid, A.S. How to Choose a Sampling Technique and Determine Sample Size for Research: A Simplified Guide for Researchers (September 22, 2024). Oral Oncol. Rep. 2024, 12, 100662. [Google Scholar] [CrossRef]
- Tziallas, D.; Goutzias, E.; Konstantinidou, E.; Dimakopoulos, G.; Anagnostopoulos, F. Quantitative and qualitative assessment of nurse staffing indicators across NHS public hospitals in Greece. Hell J. Nurs. 2018, 57, 420–449. [Google Scholar]
- Lovibond, S.H.; Lovibond, P.F. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav. Res. Ther. 1995, 33, 335–343. [Google Scholar] [CrossRef]
- Cowles, B.; Medvedev, O.N. Depression, Anxiety and Stress Scales (DASS). In Handbook of Assessment in Mindfulness Research; Medvedev, O.N., Krägeloh, C.U., Siegert, R.J., Singh, N.N., Eds.; Springer: Cham, Switzerland, 2022. [Google Scholar] [CrossRef]
- Pezirkianidis, C.; Karakasidou, E.; Lakioti, A.; Stalikas, A.; Galanakis, M. Psychometric Properties of the Depression, Anxiety, Stress Scales-21 (DASS-21) in a Greek Sample. Psychology 2018, 9, 2933–2950. [Google Scholar] [CrossRef]
- Rönkkö, M.; Cho, E. An Updated Guideline for Assessing Discriminant Validity. Organ. Res. Methods 2022, 25, 6–14. [Google Scholar] [CrossRef]
- Kristensen, T.S.; Borritz, M.; Villadsen, E.; Christensen, K.B. The Copenhagen Burnout Inventory: A new tool for the assessment of burnout. Work Stress 2005, 19, 192–207. [Google Scholar] [CrossRef]
- Papaefstathiou, E.; Tsounis, A.; Malliarou, M.; Sarafis, P. Translation and validation of the Copenhagen Burnout Inventory amongst Greek doctors. Health Psychol. Res. 2019, 7, 7678. [Google Scholar] [CrossRef] [PubMed]
- Henriksen, L.; Lukasse, M. Burnout among Norwegian midwives and the contribution of personal and work-related factors: A cross-sectional study. Sex. Reprod. Healthc. Off. J. Swed. Assoc. Midwives 2016, 9, 42–47. [Google Scholar] [CrossRef]
- Madsen, I.E.; Lange, T.; Borritz, M.; Rugulies, R. Burnout as a risk factor for antidepressant treatment—A repeated measures time-to-event analysis of 2936 Danish human service workers. J. Psychiatr. Res. 2015, 65, 47–52. [Google Scholar] [CrossRef]
- Hovland, I.S.; Skogstad, L.; Diep, L.M.; Ekeberg, Ø.; Ræder, J.; Stafseth, S.K.; Hem, E.; Rø, K.I.; Lie, I. Burnout among intensive care nurses, physicians and leaders during the COVID-19 pandemic: A national longitudinal study. Acta Anaesthesiol. Scand. 2024, 68, 1426–1435. [Google Scholar] [CrossRef]
- Benson, S.; Sammour, T.; Neuhaus, S.J.; Findlay, B.; Hill, A.G. Burnout in Australasian Younger Fellows. ANZ J. Surg. 2009, 79, 590–597. [Google Scholar] [CrossRef]
- Chou, L.P.; Li, C.Y.; Hu, S.C. Job stress and burnout in hospital employees: Comparisons of different medical professions in a regional hospital in Taiwan. BMJ Open 2014, 4, e004185. [Google Scholar] [CrossRef] [PubMed]
- Kwan, K.Y.H.; Chan, L.W.Y.; Cheng, P.W.; Leung, G.K.K.; Lau, C.S. Burnout and well-being in young doctors in Hong Kong: A territory-wide cross-sectional survey. Hong Kong Med. J. 2021, 27, 330–337. [Google Scholar] [CrossRef] [PubMed]
- Creedy, D.K.; Sidebotham, M.; Gamble, J.; Pallant, J.; Fenwick, J. Prevalence of burnout, depression, anxiety and stress in Australian midwives: A cross-sectional survey. BMC Pregnancy Childbirth 2017, 17, 13. [Google Scholar] [CrossRef] [PubMed]
- Soldatos, C.R.; Dikeos, D.G.; Paparrigopoulos, T.J. The diagnostic validity of the Athens Insomnia Scale. J. Psychosom. Res. 2003, 55, 263–267. [Google Scholar] [CrossRef]
- Soldatos, C.R.; Dikeos, D.G.; Paparrigopoulos, T.J. Athens Insomnia Scale: Validation of an instrument based on ICD-10 criteria. J. Psychosom. Res. 2000, 48, 555–560. [Google Scholar] [CrossRef] [PubMed]
- Podsakoff, P.M.; MacKenzie, S.B.; Lee, J.-Y.; Podsakoff, N.P. Common method biases in behavioral research: A critical review of the literature and recom mended remedies. J. Appl. Psychol. 2003, 88, 879–903. [Google Scholar] [CrossRef]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach; The Guilford Press: New York, NY, USA, 2013; Available online: http://www.afhayes.com (accessed on 25 March 2023).
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis. A Regression-Based Approach, 3rd ed.; The Guilford Press: New York, NY, USA, 2022; Available online: http://www.guilford.com/p/hayes3 (accessed on 9 December 2024).
- Henry, J.D.; Crawford, J.R. The short-form version of the Depression Anxiety Stress Scales (DASS-21): Construct validity and normative data in a large non-clinical sample. Br. J. Clin. Psychol. 2005, 44, 227–239. [Google Scholar] [CrossRef]
- Aymerich, C.; Pedruzo, B.; Pérez, J.L.; Laborda, M.; Herrero, J.; Blanco, J.; Mancebo, G.; Andrés, L.; Estévez, O.; Fernandez, M.; et al. COVID-19 pandemic effects on health worker’s mental health: Systematic review and meta-analysis. Eur. Psychiatry 2022, 65, e10. [Google Scholar] [CrossRef]
- García-Vivar, C.; Rodríguez-Matesanz, I.; San Martín-Rodríguez, L.; Soto-Ruiz, N.; Ferraz-Torres, M.; Escalada-Hernández, P. Analysis of mental health effects among nurses working during the COVID-19 pandemic: A systematic review. J. Psychiatr. Ment. Health Nurs. 2023, 30, 326–340. [Google Scholar] [CrossRef] [PubMed]
- Sikaras, C.; Zyga, S.; Tsironi, M.; Tselebis, A.; Pachi, A.; Ilias, I.; Panagiotou, A. The Mediating Role of Depression and of State Anxiety οn the Relationship between Trait Anxiety and Fatigue in Nurses during the Pandemic Crisis. Healthcare 2023, 11, 367. [Google Scholar] [CrossRef]
- Pachi, A.; Tselebis, A.; Sikaras, C.; Sideri, E.P.; Ivanidou, M.; Baras, S.; Milionis, C.; Ilias, I. Nightmare distress, insomnia and resilience of nursing staff in the post-pandemic era. AIMS Public Health 2023, 11, 36–57. [Google Scholar] [CrossRef] [PubMed]
- Moisoglou, I.; Katsiroumpa, A.; Malliarou, M.; Papathanasiou, I.V.; Gallos, P.; Galanis, P. Social Support and Resilience Are Protective Factors against COVID-19 Pandemic Burnout and Job Burnout among Nurses in the Post-COVID-19 Era. Healthcare 2024, 12, 710. [Google Scholar] [CrossRef]
- Abdulmohdi, N. The relationships between nurses’ resilience, burnout, perceived organisational support and social support during the second wave of the COVID-19 pandemic: A quantitative cross-sectional survey. Nurs. Open 2024, 11, e2036. [Google Scholar] [CrossRef] [PubMed]
- Health at a Glance: Europe 2020. STATE OF HEALTH IN THE EU CYCLE. Available online: https://ec.europa.eu/health/system/files/2020-12/2020_healthatglance_rep_en_0.pdf (accessed on 19 August 2024).
- Health at a Glance 2023: OECD Indicators. Available online: https://www.oecd.org/en/publications/health-at-a-glance-2023_7a7afb35-en.html (accessed on 19 August 2024).
- Zhang, W.R.; Wang, K.; Yin, L.; Zhao, W.F.; Xue, Q.; Peng, M.; Min, B.Q.; Tian, Q.; Leng, H.X.; Du, J.L. Mental Health and Psychosocial Problems of Medical Health Workers during the COVID-19 Epidemic in China. Psychother. Psychosom. 2020, 89, 242–250. [Google Scholar] [CrossRef]
- Mo, Y.; Deng, L.; Zhang, L.; Lang, Q.; Liao, C.; Wang, N.; Qin, M.; Huang, H. Work stress among Chinese nurses to support Wuhan in fighting against COVID-19 epidemic. J. Nurs. Manag. 2020, 28, 1002–1009. [Google Scholar] [CrossRef]
- El Ghaziri, M.; Dugan, A.G.; Zhang, Y.; Gore, R.; Castro, M.E. Sex and gender role differences in occupational exposures and work outcomes among registered nurses in correctional settings. Ann. Work. Expo. Health 2019, 63, 568–582. [Google Scholar] [CrossRef] [PubMed]
- Woo, T.; Ho, R.; Tang, A.; Tam, W. Global prevalence of burnout symptoms among nurses: A systematic review and meta-analysis. J. Psychiatr. Res. 2020, 123, 9–20. [Google Scholar] [CrossRef]
- Hur, G.; Cinar, N.; Suzan, O.K. Impact of COVID-19 pandemic on nurses’ burnout and related factors: A rapid systematic review. Arch. Psychiatr. Nurs. 2022, 41, 248–263. [Google Scholar] [CrossRef] [PubMed]
- Alyami, H.; Krägeloh, C.U.; Medvedev, O.N.; Alghamdi, S.; Alyami, M.; Althagafi, J.; Lyndon, M.; Hill, A.G. Investigating Predictors of Psychological Distress for Healthcare Workers in a Major Saudi COVID-19 Center. Int. J. Environ. Res. Public Health 2022, 19, 4459. [Google Scholar] [CrossRef]
- Chueh, K.-H.; Chen, K.-R.; Lin, Y.-H. Psychological Distress and Sleep Disturbance Among Female Nurses: Anxiety or Depression? J. Transcult. Nurs. 2021, 32, 14–20. [Google Scholar] [CrossRef]
- Simães, C.; Rui Gomes, A. Psychological Distress on Nurses: The Role of Personal and Professional Characteristics. In Occupational and Environmental Safety and Health. Studies in Systems, Decision and Control; Arezes, P.M., Baptista, J.S., Barroso, M.P., Carneiro, P., Cordeiro, P., Costa, N., Melo, R.B., Miguel, A.S., Perestrelo, G., Eds.; Springer: Cham, Switzerland, 2019; Volume 202. [Google Scholar] [CrossRef]
- Dor, A.; Mashiach Eizenberg, M.; Halperin, O. Hospital nurses in comparison to community nurses: Motivation, empathy, and the mediating role of burnout. Can. J. Nurs. Res. 2019, 51, 72–83. [Google Scholar] [CrossRef] [PubMed]
- Muhamad Robat, R.; Mohd Fauzi, M.F.; Mat Saruan, N.A.; Mohd Yusoff, H.; Harith, A.A. Why so stressed? A comparative study on stressors and stress between hospital and non-hospital nurses. BMC Nurs. 2021, 20, 2. [Google Scholar] [CrossRef]
- Seo, E.H.; Lee, J.H.; MacDougall, A.; Liu, N.; Hofkirchner, A.; Sharma, S.; Elfakhani, M.; Yoon, H.J. Anxiety Symptoms and Associated Psychological and Job-Related Factors Among Hospital Nurses. Psychiatry Investig. 2024, 21, 100–108. [Google Scholar] [CrossRef]
- Tokac, U.; Razon, S. Nursing professionals’ mental well-being and workplace impairment during the COVID-19 crisis: A Network analysis. J. Nurs. Manag. 2021, 29, 1653–1659. [Google Scholar] [CrossRef] [PubMed]
- Roberts, N.J.; McAloney-Kocaman, K.; Lippiett, K.; Ray, E.; Welch, L.; Kelly, C. Levels of resilience, anxiety and depression in nurses working in respiratory clinical areas during the COVID pandemic. Respir. Med. 2021, 176, 106219. [Google Scholar] [CrossRef]
- Jiang, H.; Huang, N.; Jiang, X.; Yu, J.; Zhou, Y.; Pu, H. Factors related to job burnout among older nurses in Guizhou province, China. PeerJ 2021, 9, e12333. [Google Scholar] [CrossRef]
- Mattila, E.; Kaunonen, M.; Helminen, M.; Neva, M.H.; Parkkila, A.K.; Peltokoski, J. Finnish nurses’ anxiety levels in the early stages of the COVID-19 pandemic and 18 months later: A cross-sectional survey. Nord. J. Nurs. Res. 2024, 44, 1–9. [Google Scholar] [CrossRef]
- Middleton, R.; Loveday, C.; Hobbs, C.; Almasi, E.; Moxham, L.; Green, H.; Halcomb, E.; Fernandez, R. The COVID-19 pandemic—A focus on nurse managers’ mental health, coping behaviours and organisational commitment. Collegian 2021, 28, 703–708. [Google Scholar] [CrossRef] [PubMed]
- Buckley, T.; Schatzberg, A. On the interactions of the Hypothalamic-Pituitary-Adrenal (HPA) axis and sleep: Normal HPA axis activity and circadian rhythm, exemplary sleep disorders. J. Clin. Endocrinol. Metab. 2005, 90, 3106–3114. [Google Scholar] [CrossRef] [PubMed]
- Drake, C.L.; Roth, T. Predisposition in the evolution of insomnia: Evidence, potential mechanisms, and future directions. Sleep Med. Clin. 2006, 1, 333–349. [Google Scholar] [CrossRef]
- Lukan, J.; Bolliger, L.; Pauwels, N.S.; Luštrek, M.; Bacquer, D.; Clays, E. Work environment risk factors causing day-to-day stress in occupational settings: A systematic review. BMC Public Health 2022, 22, 240. [Google Scholar] [CrossRef]
- Yang, B.; Wang, Y.; Cui, F.; Huang, T.; Sheng, P.; Shi, T.; Huang, C.; Lan, Y.; Huang, Y.N. Association between insomnia and job stress: A meta-analysis. Sleep Breath. 2018, 22, 1221–1231. [Google Scholar] [CrossRef]
- Cao, Q.; Wu, H.; Tang, X.; Zhang, Q.; Zhang, Y. Effect of occupational stress and resilience on insomnia among nurses during COVID-19 in China: A structural equation modelling analysis. BMJ Open 2024, 14, e080058. [Google Scholar] [CrossRef] [PubMed]
- Hjörleifsdóttir, E.; Sigurðardóttir, Þ.; Óskarsson, G.K.; Halapi, E.C. Stress, burnout and coping among nurses working on acute medical wards and in the community: A quantitative study. Scand. J. Caring Sci. 2024, 38, 636–647. [Google Scholar] [CrossRef]
- Luo, Y.; Fei, S.; Gong, B.; Sun, T.; Meng, R. Understanding the Mediating Role of Anxiety and Depression on the Relationship Between Perceived Stress and Sleep Quality Among Health Care Workers in the COVID-19 Response. Nat. Sci. Sleep 2021, 13, 1747–1758. [Google Scholar] [CrossRef] [PubMed]
- Łosiak, W.; Blaut, A.; Kłosowska, J.; Łosiak-Pilch, J. Stressful Life Events, Cognitive Biases, and Symptoms of Depression in Young Adults. Front. Psychol. 2019, 10, 2165. [Google Scholar] [CrossRef] [PubMed]
- Palamarchuk, I.S.; Vaillancourt, T. Mental Resilience and Coping With Stress: A Comprehensive, Multi-level Model of Cognitive Processing, Decision Making, and Behavior. Front. Behav. Neurosci. 2021, 15, 719674. [Google Scholar] [CrossRef] [PubMed]
- Espie, C.A. Insomnia: Conceptual issues in the development, persistence and treatment of sleep disorders in adults. Annu. Rev. Psychol. 2002, 53, 215–243. [Google Scholar] [CrossRef] [PubMed]
- Yalvaç, E.B.K.; Gaynor, K. Emotional dysregulation in adults: The influence of rumination and negative secondary appraisals of emotion. J. Affect. Disord. 2021, 282, 656–661. [Google Scholar] [CrossRef]
- Chahar Mahali, S.; Beshai, S.; Feeney, J.R.; Mishra, S. Associations of negative cognitions, emotional regulation, and depression symptoms across four continents: International support for the cognitive model of depression. BMC Psychiatry 2020, 20, 18. [Google Scholar] [CrossRef]
- Fernández-Mendoza, J.; Vela-Bueno, A.; Vgontzas, A.N.; Ramos-Platón, M.J.; Olavarrieta-Bernardino, S.; Bixler, E.O.; De la Cruz-Troca, J.J. Cognitive-emotional hyperarousal as a premorbid characteristic of individuals vulnerable to insomnia. Psychosom. Med. 2010, 72, 397–403. [Google Scholar] [CrossRef]
- Palagini, L.; Moretto, U.; Dell’Osso, L.; Carney, C. Sleep-related cognitive processes, arousal, and emotion dysregulation in insomnia disorder: The role of insomnia-specific rumination. Sleep Med. 2017, 30, 97–104. [Google Scholar] [CrossRef]
- Xie, M.; Huang, Y.; Cai, W.; Zhang, B.; Huang, H.; Li, Q.; Qin, P.; Han, J. Neurobiological Underpinnings of Hyperarousal in Depression: A Comprehensive Review. Brain Sci. 2024, 14, 50. [Google Scholar] [CrossRef] [PubMed]
- Sikaras, C.; Pachi, A.; Alikanioti, S.; Ilias, I.; Sideri, E.P.; Tselebis, A.; Panagiotou, A. Occupational Burnout and Insomnia in Relation to Psychological Resilience Among Greek Nurses in the Post-Pandemic Era. Behav. Sci. 2025, 15, 126. [Google Scholar] [CrossRef]
- Grossi, G.; Perski, A.; Osika, W.; Savic, I. Stress-related exhaustion disorder--clinical manifestation of burnout? A review of assessment methods, sleep impairments, cognitive disturbances, and neuro-biological and physiological changes in clinical burnout. Scand. J. Psychol. 2015, 56, 626–636. [Google Scholar] [CrossRef]
- Toker, S.; Melamed, S. Stress recovery sleep burnout. In The Handbook of Stress and Health: A Guide to Research and Practice; Cooper, C.L., Quick, J.C., Eds.; Wiley Blackwell: Hoboken, NJ, USA, 2017; pp. 168–185. [Google Scholar] [CrossRef]
- Armon, G.; Shirom, A.; Shapira, I.; Melamed, S. On the nature of burnout-insomnia relationships: A prospective study of employed adults. J. Psychosom. Res. 2008, 65, 5–12. [Google Scholar] [CrossRef]
- Höglund, P.; Hakelind, C.; Nordin, M.; Nordin, S. Risk factors for insomnia and burnout: A longitudinal population-based cohort study. Stress Health 2023, 39, 798–812. [Google Scholar] [CrossRef] [PubMed]
- Sørengaard, T.A.; Saksvik-Lehouillier, I. Associations between burnout symptoms and sleep among workers during the COVID-19 pandemic. Sleep Med. 2022, 90, 199–203. [Google Scholar] [CrossRef]
- Membrive-Jiménez, M.J.; Gómez-Urquiza, J.L.; Suleiman-Martos, N.; Velando-Soriano, A.; Ariza, T.; De la Fuente-Solana, E.I.; Cañadas-De la Fuente, G.A. Relation between Burnout and Sleep Problems in Nurses: A Systematic Review with Meta-Analysis. Healthcare 2022, 10, 954. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Wu, C.; Ma, J.; Liu, F.; Shen, C.; Sun, J.; Ma, Z.; Hu, W.; Lang, H. Relationship between depression and burnout among nurses in Intensive Care units at the late stage of COVID-19: A network analysis. BMC Nurs. 2024, 23, 224. [Google Scholar] [CrossRef]
- Chen, C.; Meier, S.T. Burnout and depression in nurses: A systematic review and meta-analysis. Int. J. Nurs. Stud. 2021, 124, 104099, Erratum in Int. J. Nurs. Stud. 2022, 127, 104180. [Google Scholar] [CrossRef] [PubMed]
- Mbanga, C.; Makebe, H.; Tim, D.; Fonkou, S.; Toukam, L.; Njim, T. Burnout as a predictor of depression: A cross-sectional study of the sociodemographic and clinical predictors of depression amongst nurses in Cameroon. BMC Nurs. 2019, 18, 50. [Google Scholar] [CrossRef] [PubMed]
- Hakanen, J.J.; Schaufeli, W.B. Do burnout and work engagement predict depressive symptoms and life satisfaction? A three-wave seven-year prospective study. J. Affect. Disord. 2012, 141, 415–424. [Google Scholar] [CrossRef]
- Papathanasiou, I.V. Work-related Mental Consequences: Implications of Burnout on Mental Health Status Among Health Care Providers. Acta Inform. Med. 2015, 23, 22–28. [Google Scholar] [CrossRef] [PubMed]
- Nyklícek, I.; Pop, V.J. Past and familial depression predict current symptoms of professional burnout. J. Affect. Disord. 2005, 88, 63–68. [Google Scholar] [CrossRef] [PubMed]
- Bianchi, R.; Schonfeld, I.S.; Laurent, E. Burnout–depression overlap: A review. Clin. Psychol. Rev. 2015, 36, 28–41. [Google Scholar] [CrossRef]
- Verkuilen, J.; Bianchi, R.; Schonfeld, I.S.; Laurent, E. Burnout-Depression Overlap: Exploratory Structural Equation Modeling Bifactor Analysis and Network Analysis. Assessment 2021, 28, 1583–1600. [Google Scholar] [CrossRef]
- Bianchi, R.; Brisson, R. Burnout depression: Causal attributions construct overlap. J. Health Psychol. 2019, 24, 1574–1580. [Google Scholar] [CrossRef] [PubMed]
- Wurm, W.; Vogel, K.; Holl, A.; Ebner, C.; Bayer, D.; Mörkl, S.; Szilagyi, I.S.; Hotter, E.; Kapfhammer, H.P.; Hofmann, P. Depression-Burnout Overlap in Physicians. PLoS ONE 2016, 11, e0149913. [Google Scholar] [CrossRef]
- Schonfeld, I.S.; Bianchi, R. From Burnout to Occupational Depression: Recent Developments in Research on Job-Related Distress and Occupational Health. Front. Public Health 2021, 9, 796401. [Google Scholar] [CrossRef] [PubMed]
- Bianchi, R.; Schonfeld, I.S.; Laurent, E. Burnout Syndrome and Depression. In Understanding Depression; Kim, Y.K., Ed.; Springer: Singapore, 2018. [Google Scholar] [CrossRef]
- Zisook, S.; Doshi, A.P.; Fergerson, B.D.; Shapiro, D.N. Differentiating Burnout from Depression. In Workplace Wellness: From Resiliency to Suicide Prevention and Grief Management; Davidson, J.E., Richardson, M., Eds.; Springer: Cham, Switzerland, 2023. [Google Scholar] [CrossRef]
- Rothe, N.; Schulze, J.; Kirschbaum, C.; Buske-Kirschbaum, A.; Penz, M.; Wekenborg, M.K.; Walther, A. Sleep disturbances in major depressive and burnout syndrome: A longitudinal analysis. Psychiatry Res. 2020, 286, 112868. [Google Scholar] [CrossRef]
- Yupanqui-Lorenzo, D.E.; Caycho-Rodríguez, T.; Baños-Chaparro, J.; Arauco-Lozada, T.; Palao-Loayza, L.; Rivera, M.E.L.; Barrios, I.; Torales, J. Mapping of the network connection between sleep quality symptoms, depression, generalized anxiety, and burnout in the general population of Peru and El Salvador. Psicol. Refl. Crít. 2024, 37, 27. [Google Scholar] [CrossRef] [PubMed]
- Herbison, C.E.; Allen, K.; Robinson, M.; Newnham, J.; Pennell, C. The impact of life stress on adult depression and anxiety is dependent on gender and timing of exposure. Dev. Psychopathol. 2017, 29, 1443–1454. [Google Scholar] [CrossRef] [PubMed]
- Lowery-Gionta, E.G.; Crowley, N.A.; Bukalo, O.; Silverstein, S.; Holmes, A.; Kash, T.L. Chronic stress dysregulates amygdalar output to the prefrontal cortex. Neuropharmacology 2018, 139, 68–75. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Li, L.; Zhu, X.; Wang, Y.; Zhang, J.; Zhao, L.; Li, L.; Yang, Y. Comparison of characteristics of anxiety sensitivity across career stages and its relationship with nursing stress among female nurses in Hunan, China. BMJ Open 2016, 6, e010829. [Google Scholar] [CrossRef]
- Baglioni, C.; Spiegelhalder, K.; Lombardo, C.; Riemann, D. Sleep and emotions: A focus on insomnia. Sleep Med. Rev. 2010, 14, 227–238. [Google Scholar] [CrossRef]
- Bard, H.A.; O’Driscoll, C.; Miller, C.B.; Henry, A.L.; Cape, J.; Espie, C.A. Insomnia, depression, and anxiety symptoms interact and individually impact functioning: A network and relative importance analysis in the context of insomnia. Sleep Med. 2023, 101, 505–514. [Google Scholar] [CrossRef]
- Kirwan, M.; Pickett, S.M.; Jarrett, N.L. Emotion regulation as a moderator between anxiety symptoms and insomnia symptom severity. Psychiatry Res. 2017, 254, 40–47. [Google Scholar] [CrossRef] [PubMed]
- Bélanger, L.; Morin, C.M.; Gendron, L.; Blais, F.C. Presleep cognitive activity and thought control strategies in insomnia. J. Cogn. Psychother. 2005, 19, 19–28. [Google Scholar] [CrossRef]
- Van Egeren, L.; Hayness, S.N.; Franzen, M.; Hamilton, J. Presleep cognitions and attributions in sleep onset insomnia. J. Behav. Med. 1983, 6, 217–232. [Google Scholar] [CrossRef]
- Carney, C.E.; Edinger, J.D.; Meyer, B.; Lindman, L.; Istre, T. Symptom-focused rumination and sleep disturbance. Behav. Sleep Med. 2006, 4, 228–241. [Google Scholar] [CrossRef] [PubMed]
- Watts, F.N.; Coyle, K.; East, M.P. The contribution of worry to insomnia. Br. J. Clin. Psychol. 1994, 33, 211–220. [Google Scholar] [CrossRef]
- Jansson-Fröjmark, M.; Lindblom, K. A bidirectional relationship between anxiety and depression, and insomnia? A prospective study in the general population. J. Psychosom. Res. 2008, 64, 443–449. [Google Scholar] [CrossRef]
- Alvaro, P.K.; Roberts, R.M.; Harris, J.K. A Systematic Review Assessing Bidirectionality between Sleep Disturbances, Anxiety, and Depression. Sleep 2013, 36, 1059–1068. [Google Scholar] [CrossRef] [PubMed]
- Hartz, A.J.; Daly, J.M.; Kohatsu, N.D.; Stromquist, A.M.; Jogerst, G.J.; Kukoyi, O.A. Risk factors for insomnia in a rural population. Ann. Epidemiol. 2007, 17, 940–947. [Google Scholar] [CrossRef]
- Ohayon, M.M. Prevalence and correlates of nonrestorative sleep complaints. Arch. Intern. Med. 2005, 165, 35–41. [Google Scholar] [CrossRef] [PubMed]
- Dolsen, E.A.; Asarnow, L.D.; Harvey, A.G. Insomnia as a transdiagnostic process in psychiatric disorders. Curr. Psychiatry Rep. 2014, 16, 471. [Google Scholar] [CrossRef] [PubMed]
- Scott, B.A.; Judge, T.A. Insomnia, Emotions, and Job Satisfaction: A Multilevel Study. J. Manag. 2006, 32, 622–645. [Google Scholar] [CrossRef]
- Trauer, J.M.; Qian, M.Y.; Doyle, J.S.; Rajaratnam, S.M.; Cunnington, D. Cognitive behavioral therapy for chronic insomnia: A systematic review and meta-analysis. Ann. Intern. Med. 2015, 163, 191–204. [Google Scholar] [CrossRef] [PubMed]
- Sforza, M.; Galbiati, A.; Zucconi, M.; Casoni, F.; Hensley, M.; Ferini-Strambi, L.; Castronovo, V. Depressive and stress symptoms in insomnia patients predict group cognitive-behavioral therapy for insomnia long-term effectiveness: A data-driven analysis. J. Affect. Disord. 2021, 289, 117–124. [Google Scholar] [CrossRef] [PubMed]
- Mirchandaney, R.; Barete, R.; Asarnow, L.D. Moderators of Cognitive Behavioral Treatment for Insomnia on Depression and Anxiety Outcomes. Curr. Psychiatry Rep. 2022, 24, 121–128. [Google Scholar] [CrossRef] [PubMed]
- Alkhawaldeh, J.M.; Soh, K.L.; Mukhtar, F.; Peng, O.C.; Alkhawaldeh, H.M.; Al-Amer, R.; Anshasi, H.A. Stress management training program for stress reduction and coping improvement in public health nurses: A randomized controlled trial. J. Adv. Nurs. 2020, 76, 3123–3135. [Google Scholar] [CrossRef] [PubMed]
- Sulosaari, V.; Unal, E.; Cinar, F.I. The effectiveness of mindfulness-based interventions on the psychological well-being of nurses: A systematic review. Appl. Nurs. Res. 2022, 64, 151565. [Google Scholar] [CrossRef] [PubMed]
- Conversano, C.; Ciacchini, R.; Orrù, G.; Di Giuseppe, M.; Gemignani, A.; Poli, A. Mindfulness, Compassion, and Self-Compassion Among Health Care Professionals: What’s New? A Systematic Review. Front. Psychol. 2020, 11, 1683. [Google Scholar] [CrossRef] [PubMed]
- Williams, S.G.; Fruh, S.; Barinas, J.L.; Graves, R.J. Self-Care in Nurses. J. Radiol. Nurs. 2022, 41, 22–27. [Google Scholar] [CrossRef] [PubMed]
- Aguirre-Urreta, M.I.; Hu, J. Detecting Common Method Bias: Performance of the Harman’s Single-Factor Test. Data Base 2019, 50, 45–70. [Google Scholar] [CrossRef]


| Gender | Age | Work Experience (in Years) | Athens Insomnia Scale | Copenhagen Burnout Inventory | Depression Anxiety Stress Scale | ||||
|---|---|---|---|---|---|---|---|---|---|
| DASS-21 Total | Stress Subscale | Anxiety Subscale | Depression Subscale | ||||||
| Male | Mean | 47.57 * | 21.89 | 6.35 | 44.91 * | 22.67 * | 10.67 * | 5.05 | 6.94 |
| N | 74 | 74 | 74 | 74 | 74 | 74 | 74 | 74 | |
| S.D. | 10.85 | 11.92 | 4.23 | 17.93 | 21.88 | 8.2 | 7.52 | 7.99 | |
| Female | Mean | 44.58 * | 19.92 | 7.31 | 49.64 * | 29.53 * | 13.47 * | 7.17 | 8.88 |
| N | 306 | 306 | 306 | 306 | 306 | 306 | 306 | 306 | |
| S.D. | 10.41 | 11.47 | 4.92 | 19.03 | 27.42 | 10.26 | 9.06 | 9.67 | |
| Total | Mean | 45.16 | 20.30 | 7.12 | 48.72 | 28.2 | 12.93 | 6.75 | 8.5 |
| N | 380 | 380 | 380 | 380 | 380 | 380 | 380 | 380 | |
| S.D. | 10.55 | 11.57 | 4.80 | 18.89 | 26.54 | 9.95 | 8.81 | 9.39 | |
|
Pearson Correlation
N: 380 | Age | Work Experience (in Years) | AIS | CBI | DASS-21 Total | DASS-21 (Stress Subscale) |
DASS-21 (Anxiety
Subscale) | DASS-21 (Depression Subscale) | |
|---|---|---|---|---|---|---|---|---|---|
| Work experience (in years) | r | 0.894 ** | |||||||
| p | 0.001 | ||||||||
| Athens Insomnia Scale (AIS) | r | −0.064 | −0.126 * | ||||||
| p | 0.214 | 0.014 | |||||||
| Copenhagen Burnout Inventory (CBI) | r | −0.031 | −0.058 | 0.587 ** | 0.72104 | ||||
| p | 0.552 | 0.257 | 0.001 | ||||||
| Depression Anxiety Stress Scale (DASS-21 Total) | r | −0.072 | −0.132 * | 0.662 ** | 0.586 ** | ||||
| p | 0.161 | 0.010 | 0.001 | 0.001 | |||||
| DASS-21 (Stress subscale) | r | −0.051 | −0.089 | 0.633 ** | 0.590 ** | 0.949 ** | |||
| p | 0.323 | 0.083 | 0.001 | 0.001 | 0.001 | ||||
| DASS-21 (Anxiety subscale) | r | −0.123 * | −0.186 ** | 0.600 ** | 0.499 ** | 0.939 ** | 0.840 ** | ||
| p | 0.016 | 0.000 | 0.001 | 0.001 | 0.001 | 0.001 | |||
| DASS-21 (Depression subscale) | r | −0.034 | −0.104 * | 0.637 ** | 0.563 ** | 0.940 ** | 0.835 ** | 0.822 ** | 0.76289 |
| p | 0.508 | 0.044 | 0.001 | 0.001 | 0.001 | 0.001 | 0.001 | ||
| AVE (Average Variance Extracted) | 0.5199 | 0.582 | |||||||
| Dependent Variable: Athens Insomnia Scale | R Square | R Square Change | Beta | t | p | VIF | Durbin–Watson |
|---|---|---|---|---|---|---|---|
| DASS-21 (Depression subscale) | 0.406 | 0.406 | 0.290 | 4.310 | 0.001 * | 3.382 | 1.843 |
| Copenhagen Burnout Inventory (CBI) | 0.483 | 0.076 | 0.296 | 6.438 | 0.001 * | 1.573 | |
| DASS-21 (Stress subscale) | 0.496 | 0.013 | 0.217 | 3.143 | 0.002 * | 3.545 |
| Variable | b | SE | t | p | 95% Confidence Interval | |
|---|---|---|---|---|---|---|
| LLCI | ULCI | |||||
| DASS-21 Stress → DASS-21 Depression | 0.7809 | 0.0267 | 29.2765 | 0.0000 | 0.7284 | 0.8333 |
| DASS-21 Stress → CBI | 0.7508 | 0.1424 | 5.2712 | 0.0000 | 0.4708 | 1.0309 |
| DASS-21 Depression → CBI | 0.4700 | 0.1521 | 3.0906 | 0.0021 | 0.1710 | 0.7690 |
| DASS-21 Stress → AIS | 0.1073 | 0.0333 | 3.2235 | 0.0014 | 0.0418 | 0.1727 |
| DASS-21 Depression → AIS | 0.1397 | 0.0347 | 4.0234 | 0.0001 | 0.0714 | 0.2079 |
| CBI → AIS | 0.0753 | 0.0116 | 6.4684 | 0.0000 | 0.0524 | 0.0982 |
| (1) DASS-21 Stress → DASS-21 Depression → AIS | 0.1091 | 0.0290 | 3.7620 | 0.0513 | 0.1655 | |
| (2) DASS-21 Stress →CBI → AIS | 0.0565 | 0.0146 | 3.8698 | 0.0306 | 0.0885 | |
| (3) DASS-21 Stress→ DASS-21 Depression → CBI →AIS | 0.0276 | 0.0091 | 3.0329 | 0.0109 | 0.0464 | |
| Covariates | ||||||
| Age → DASS-21 Depression | 0.1540 | 0.0560 | 2.7505 | 0.0062 | 0.0439 | 0.2641 |
| W.E. → DASS-21 Depression | −0.1498 | 0.0512 | −2.9254 | 0.0036 | −0.2505 | −0.0491 |
| W.E. → AIS | −0.0853 | 0.0369 | −2.3117 | 0.0213 | −0.1578 | −0.0127 |
| Effects | ||||||
| Direct | 0.1073 | 0.0333 | 3.2235 | 0.0014 | 0.0418 | 0.1727 |
| * Total Indirect | 0.1932 | 0.0309 | 0.1311 | 0.1655 | ||
| Total | 0.3005 | 0.0192 | 15.6336 | 0.0000 | 0.2627 | 0.3383 |
| Direct Relationships | ||||||
|---|---|---|---|---|---|---|
| Variable | b | SE | t | p | 95% Confidence Interval | |
| LLCI | ULCI | |||||
| DASS-21 Stress → DASS-21 Depression | 0.4366 | 0.0462 | 9.4585 | 0.0000 | 0.3459 | 0.5274 |
| DASS-21 Anxiety → DASS-21 Depression | 0.2476 | 0.0944 | 2.6214 | 0.0091 | 0.0616 | 0.4333 |
| DASS-21 Stress × DASS-21 Anxiety → DASS-21 Depression | 0.0066 | 0.0028 | 2.3841 | 0.0176 | 0.0012 | 0.0121 |
| DASS-21 Stress → CBI | 0.7508 | 0.1424 | 5.2712 | 0.0000 | 0.4708 | 1.0309 |
| DASS-21 Depression → CBI | 0.4700 | 0.1521 | 3.0906 | 0.0021 | 0.1710 | 0.7690 |
| DASS-21 Stress → AIS | 0.1073 | 0.0333 | 3.2235 | 0.0014 | 0.0418 | 0.1727 |
| DASS-21 Depression → AIS | 0.1397 | 0.0347 | 4.0234 | 0.0001 | 0.0714 | 0.2079 |
| CBI → AIS | 0.0753 | 0.0116 | 6.4684 | 0.0000 | 0.0524 | 0.0982 |
| Covariates | ||||||
| Age → DASS-21 Depression | 0.1038 | 0.0516 | 2.0101 | 0.0451 | 0.0023 | 0.2053 |
| Effects | ||||||
| Direct | 0.1073 | 0.0333 | 3.2235 | 0.0014 | 0.0418 | 0.1727 |
| Moderated Indirect Relationships | ||||||
| Indirect 1: DASS-21 Stress → DASS-21 Depression → AIS | ||||||
| DASS-21 Anxiety (mean − 1SD) | 0.0610 | 0.0173 | 3.5260 | 0.0288 | 0.0972 | |
| DASS-21 Anxiety (mean) | 0.0672 | 0.0188 | 3.5744 | 0.0322 | 0.1062 | |
| DASS-21 Anxiety (mean + 1SD) | 0.0754 | 0.0213 | 3.5399 | 0.0359 | 0.1189 | |
| Index of Moderated Mediation | 0.0009 | 0.0005 | 0.0001 | 0.0019 | ||
| Indirect 2: DASS-21 Stress → CBI → AIS | 0.0565 | 0.0147 | 3.8435 | 0.0309 | 0.0886 | |
| Indirect 3: DASS-21 Stress→ DASS-21 Depression → CBI → AIS | ||||||
| DASS-21 Anxiety (mean − 1SD) | 0.0155 | 0.0053 | 2.9245 | 0.0059 | 0.0266 | |
| DASS-21 Anxiety (mean) | 0.0170 | 0.0058 | 2.9310 | 0.0066 | 0.0293 | |
| DASS-21 Anxiety (mean + 1SD) | 0.0191 | 0.0066 | 2.8939 | 0.0073 | 0.0333 | |
| Index of Moderated Mediation | 0.0002 | 0.0001 | 0.0000 | 0.0005 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pachi, A.; Sikaras, C.; Melas, D.; Alikanioti, S.; Soultanis, N.; Ivanidou, M.; Ilias, I.; Tselebis, A. Stress, Anxiety and Depressive Symptoms, Burnout and Insomnia Among Greek Nurses One Year After the End of the Pandemic: A Moderated Chain Mediation Model. J. Clin. Med. 2025, 14, 1145. https://doi.org/10.3390/jcm14041145
Pachi A, Sikaras C, Melas D, Alikanioti S, Soultanis N, Ivanidou M, Ilias I, Tselebis A. Stress, Anxiety and Depressive Symptoms, Burnout and Insomnia Among Greek Nurses One Year After the End of the Pandemic: A Moderated Chain Mediation Model. Journal of Clinical Medicine. 2025; 14(4):1145. https://doi.org/10.3390/jcm14041145
Chicago/Turabian StylePachi, Argyro, Christos Sikaras, Dimitrios Melas, Sofia Alikanioti, Nikolaos Soultanis, Maria Ivanidou, Ioannis Ilias, and Athanasios Tselebis. 2025. "Stress, Anxiety and Depressive Symptoms, Burnout and Insomnia Among Greek Nurses One Year After the End of the Pandemic: A Moderated Chain Mediation Model" Journal of Clinical Medicine 14, no. 4: 1145. https://doi.org/10.3390/jcm14041145
APA StylePachi, A., Sikaras, C., Melas, D., Alikanioti, S., Soultanis, N., Ivanidou, M., Ilias, I., & Tselebis, A. (2025). Stress, Anxiety and Depressive Symptoms, Burnout and Insomnia Among Greek Nurses One Year After the End of the Pandemic: A Moderated Chain Mediation Model. Journal of Clinical Medicine, 14(4), 1145. https://doi.org/10.3390/jcm14041145










