Heart Rate Reduction and the Prognosis of Heart Failure Focused on Ivabradine
Abstract
1. Introduction
2. The Relationship Between HR and HF
3. Effects of Ivabradine on HF Prognosis
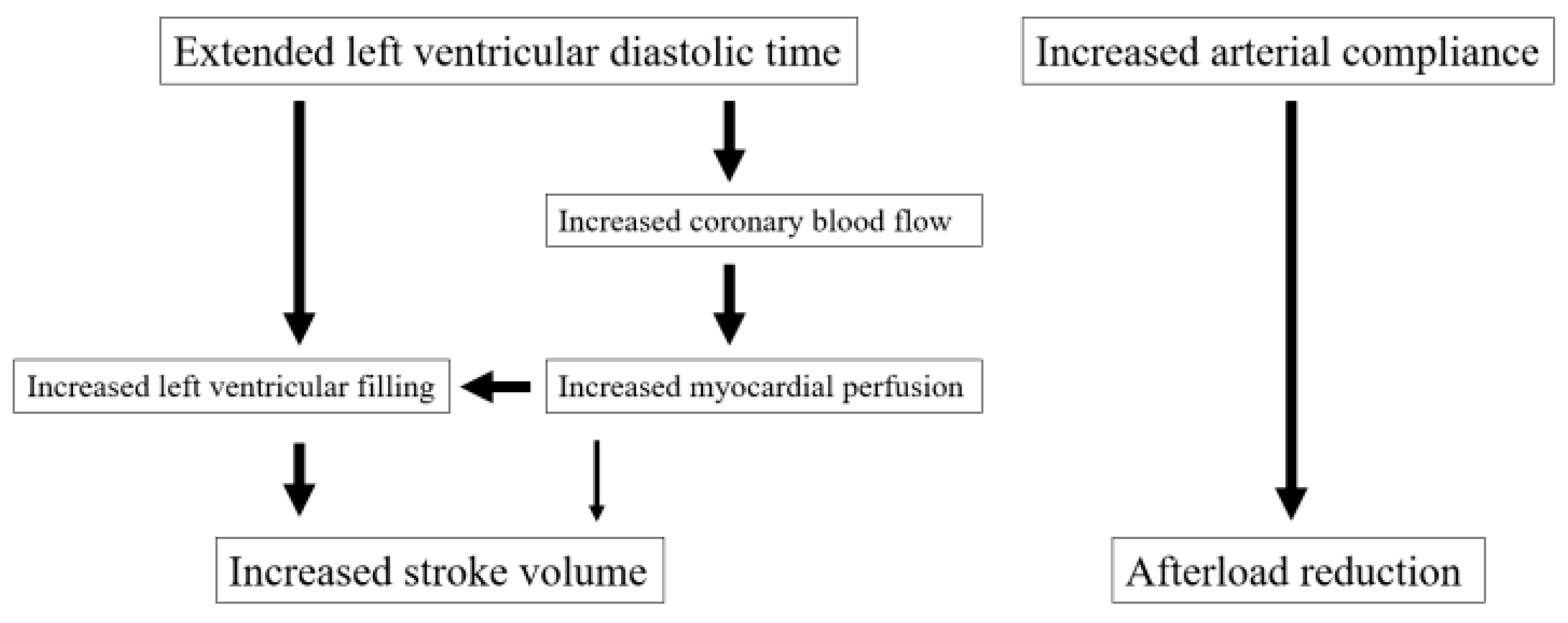
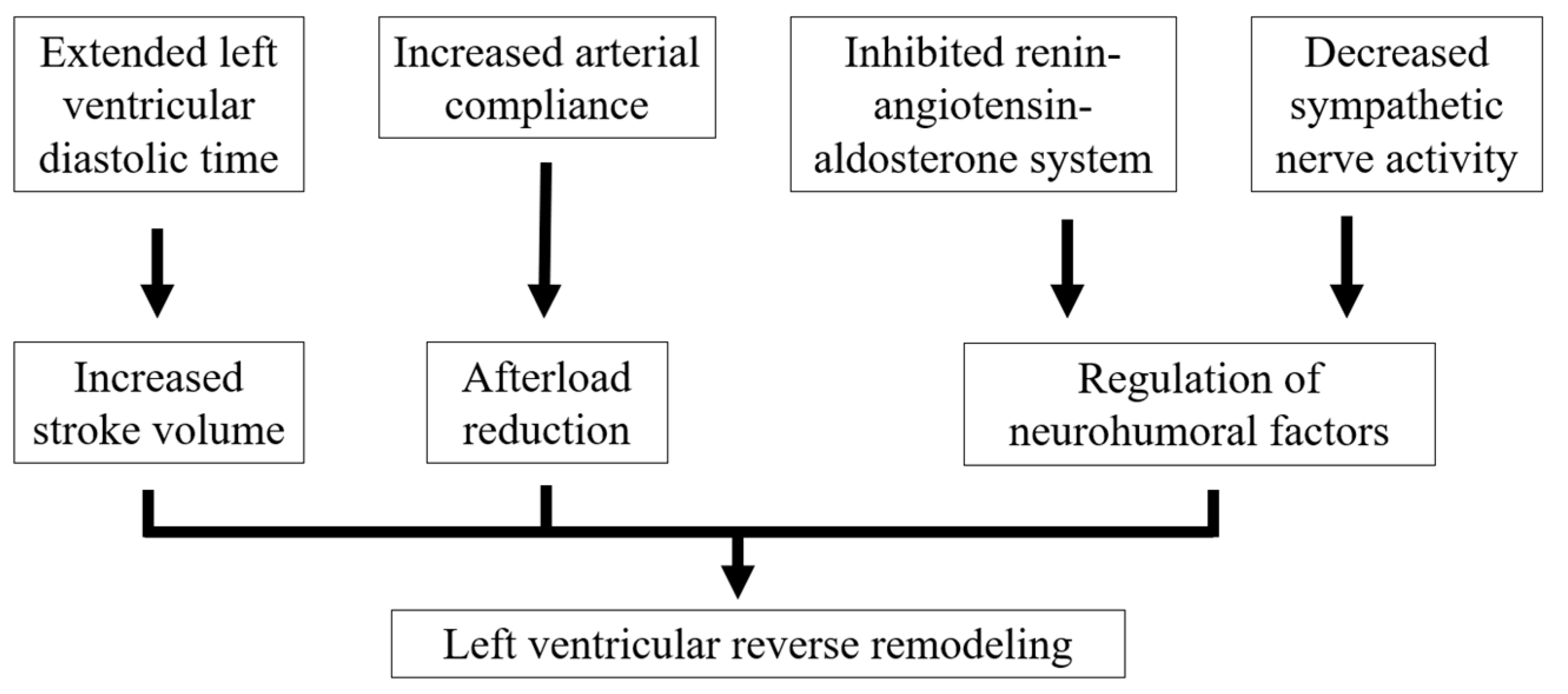
4. Pathophysiology of HFpEF and Use of Ivabradine
5. Cardiac Effects of Ivabradine Administration
6. β-Blockers and Ivabradine
7. Safety Profile of Ivabradine
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Okura, Y.; Ramadan, M.M.; Ohno, Y.; Mitsuma, W.; Tanaka, K.; Ito, M.; Suzuki, K.; Tanabe, N.; Kodama, M.; Aizawa, Y. Impending epidemic: Future projection of heart failure in Japan to the year 2055. Circ. J. 2008, 72, 489–491. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, M.; Ulrichsen, S.P.; Pedersen, L.; Bøtker, H.E.; Sørensen, H.T. Thirty-year trends in heart failure hospitalization and mortality rates and the prognostic impact of co-morbidity: A Danish nationwide cohort study. Eur. J. Heart Fail. 2016, 18, 490–499. [Google Scholar] [CrossRef] [PubMed]
- Shimokawa, H.; Miura, M.; Nochioka, K.; Sakata, Y. Heart failure as a general pandemic in Asia. Eur. J. Heart Fail. 2015, 17, 884–892. [Google Scholar] [CrossRef] [PubMed]
- Ejiri, K.; Noriyasu, T.; Nakamura, K.; Ito, H. Unprecedented crisis-Heart failure hospitalizations in current or future Japan. J. Cardiol. 2019, 74, 426–427. [Google Scholar] [CrossRef] [PubMed]
- Eguchi, S.; Morita, Y.; Mitani, H.; Kanegasaki, A.; Iwasaki, K.; Yoshikawa, T.; Kitagawa, H.; Oyama, N. Burden of Repeated Hospitalization on Patients with Heart Failure: An Analysis of Administrative and Claims Data in Japan. Drugs Real World Outcomes 2022, 9, 377–389. [Google Scholar] [CrossRef]
- Lam, C.S.P.; Butler, J. Victims of Success in Failure. Circulation 2020, 142, 1129–1131. [Google Scholar] [CrossRef]
- Tsutsui, H.; Isobe, M.; Ito, H.; Ito, H.; Okumura, K.; Ono, M.; Kitakaze, M.; Kinugawa, K.; Kihara, Y.; Goto, Y.; et al. JCS 2017/JHFS 2017 Guideline on Diagnosis and Treatment of Acute and Chronic Heart Failure-Digest Version. Circ. J. 2019, 82, 2084–2184. [Google Scholar] [CrossRef]
- Levine, J.H. Rest heart rate and life expectancy. J. Am. Coll. Cardiol. 1997, 30, 1104–1106. [Google Scholar]
- Jouven, X.; Empana, J.P.; Schwartz, P.J.; Desnos, M.; Courbon, D.; Ducimetière, P. Heart-rate profile during exercise as a predictor of sudden death. N. Engl. J. Med. 2005, 352, 1951–1958. [Google Scholar] [CrossRef]
- Fox, K.; Borer, J.S.; Camm, A.J.; Danchin, N.; Ferrari, R.; Lopez Sendon, J.L.; Steg, P.G.; Tardif, J.C.; Tavazzi, L.; Tendera, M.; et al. Resting heart rate in cardiovascular disease. J. Am. Coll. Cardiol. 2007, 50, 823–830. [Google Scholar] [CrossRef]
- Nikolovska Vukadinović, A.; Vukadinović, D.; Cowie, M.; Komajda, M.; Lainscak, M.; Swedberg, K.; Böhm, M. Heart rate and its reduction in chronic heart failure and beyond. Eur. J. Heart Fail. 2017, 19, 1230–1241. [Google Scholar] [CrossRef] [PubMed]
- Li, S.J.; Sartipy, U.; Lund, L.H.; Dahlström, U.; Adiels, M.; Petzold, M.; Fu, M. Prognostic Significance of Resting Heart Rate and Use of β-Blockers in Atrial Fibrillation and Sinus Rhythm in Patients with Heart Failure and Reduced Ejection Fraction: Findings From the Swedish Heart Failure Registry. Circ. Heart Fail. 2015, 8, 871–879. [Google Scholar] [CrossRef] [PubMed]
- Takada, T.; Sakata, Y.; Miyata, S.; Takahashi, J.; Nochioka, K.; Miura, M.; Tadaki, S.; Shimokawa, H.; CHART-2 Investigators. Impact of elevated heart rate on clinical outcomes in patients with heart failure with reduced and preserved ejection fraction: A report from the CHART-2 Study. Eur. J. Heart Fail. 2014, 16, 309–316. [Google Scholar] [CrossRef]
- Grande, D.; Iacoviello, M.; Aspromonte, N. The effects of heart rate control in chronic heart failure with reduced ejection fraction. Heart Fail. Rev. 2018, 23, 527–535. [Google Scholar] [CrossRef]
- Narula, J.; Gerson, M.; Thomas, G.S.; Cerqueira, M.D.; Jacobson, A.F. 123I-MIBG imaging for prediction of mortality and potentially fatal events in heart failure: The ADMIRE HFX study. J. Nucl. Med. 2015, 56, 1011–1018. [Google Scholar] [CrossRef]
- Tsuchihashi-Makaya, M.; Kinugawa, S.; Yokoshiki, H.; Hamaguchi, S.; Yokota, T.; Goto, D.; Goto, K.; Takeshita, A.; Tsutsui, H.; JCARE-CARD Investigators. Beta-blocker use at discharge in patients hospitalized for heart failure is associated with improved survival. Circ. J. 2010, 74, 1364–1371. [Google Scholar] [CrossRef]
- Tsutsui, H.; Momomura, S.I.; Yamashina, A.; Shimokawa, H.; Kihara, Y.; Saito, Y.; Hagiwara, N.; Ito, H.; Yano, M.; Yamamoto, K.; et al. Efficacy and Safety of Ivabradine in Japanese Patients with Chronic Heart Failure-J-SHIFT Study. Circ. J. 2019, 83, 2049–2060. [Google Scholar] [CrossRef]
- Izumida, T.; Imamura, T.; Nakamura, M.; Fukuda, N.; Kinugawa, K. How to consider target heart rate in patients with systolic heart failure. ESC Heart Fail. 2020, 7, 3231–3234. [Google Scholar] [CrossRef]
- Izumida, T.; Imamura, T.; Fukui, T.; Koi, T.; Ueno, Y.; Hori, M.; Nakagaito, M.; Tanaka, S.; Kataoka, N.; Ushijima, R.; et al. How to Estimate the Optimal Heart Rate in Patients with Heart Failure with Preserved Ejection Fraction. Int. Heart J. 2021, 62, 816–820. [Google Scholar] [CrossRef]
- Böhm, M.; Reil, J.C. Heart rate: Surrogate or target in the management of heart failure? Heart 2013, 99, 72–75. [Google Scholar] [CrossRef]
- He, C.; Chen, F.; Li, B.; Hu, Z. Neurophysiology of HCN channels: From cellular functions to multiple regulations. Prog. Neurobiol. 2014, 112, 1–23. [Google Scholar] [CrossRef] [PubMed]
- DiFrancesco, D.; Camm, J.A. Heart rate lowering by specific and selective I(f) current inhibition with ivabradine: A new therapeutic perspective in cardiovascular disease. Drugs 2004, 64, 1757–1765. [Google Scholar] [CrossRef] [PubMed]
- De Ferrari, G.M.; Mazzuero, A.; Agnesina, L.; Bertoletti, A.; Lettino, M.; Campana, C.; Schwartz, P.J.; Tavazzi, L. Favourable effects of heart rate reduction with intravenous administration of ivabradine in patients with advanced heart failure. Eur. J. Heart Fail. 2008, 10, 550–555. [Google Scholar] [CrossRef] [PubMed]
- Swedberg, K.; Komajda, M.; Böhm, M.; Borer, J.S.; Ford, I.; Dubost-Brama, A.; Lerebours, G.; Tavazzi, L.; SHIFT Investigators. Ivabradine and outcomes in chronic heart failure (SHIFT): A randomized placebo-controlled study. Lancet 2010, 37, 875–885. [Google Scholar] [CrossRef]
- Tóth, N.; Soós, A.; Váradi, A.; Hegyi, P.; Tinusz, B.; Vágvölgyi, A.; Orosz, A.; Solymár, M.; Polyák, A.; Varró, A.; et al. Effect of ivabradine in heart failure: A meta-analysis of heart failure patients with reduced versus preserved ejection fraction. Can. J. Physiol. Pharmacol. 2021, 99, 1159–1174. [Google Scholar] [CrossRef] [PubMed]
- Komajda, M.; Isnard, R.; Cohen-Solal, A.; Hegyi, P.; Tinusz, B.; Vágvölgyi, A.; Orosz, A.; Solymár, M.; Polyák, A.; Varró, A.; et al. Effect of ivabradine in patients with heart failure with preserved ejection fraction: The EDIFY randomized placebo-controlled trial. Eur. J. Heart Fail. 2017, 19, 1495–1503. [Google Scholar] [CrossRef]
- Tanaka, H.; Yamauchi, Y.; Imanishi, J.; Hatani, Y.; Odajima, S.; Okamoto, H.; Hayashi, T.; Hirata, K.I. Effect of Ivabradine on Left Ventricular Diastolic Function of Patients with Preserved Ejection Fraction-Results of the IVA-PEF Study. Circ. Rep. 2022, 4, 499–504. [Google Scholar] [CrossRef]
- Cacciapuoti, F.; Magro, V.M.; Caturano, M.; Lama, D.; Cacciapuoti, F. The role of Ivabradine in Diastolic Heart Failure with preserved Ejection Fraction. A Doppler-Echocardiographic study. J. Cardiovasc. Echogr. 2017, 27, 126–131. [Google Scholar] [CrossRef]
- Conceição, L.S.R.; Gois, C.; Fernandes, R.E.S.; Souza, D.S.; Júnior, M.B.G.; Carvalho, V.O. Effect of ivabradine on exercise capacity in individuals with heart failure with preserved ejection fraction. Heart Fail. Rev. 2021, 26, 157–163. [Google Scholar] [CrossRef]
- Kosmala, W.; Holland, D.J.; Rojek, A.; Wright, L.; Przewlocka-Kosmala, M.; Marwick, T.H. Effect of If-channel inhibition on hemodynamic status and exercise tolerance in heart failure with preserved ejection fraction: A randomized trial. J. Am. Coll. Cardiol. 2013, 62, 1330–1338. [Google Scholar] [CrossRef]
- Heidenreich, P.A.; Bozkurt, B.; Aguilar, D.; Allen, L.A.; Byun, J.J.; Colvin, M.M.; Deswal, A.; Drazner, M.H.; Dunlay, S.M.; Evers, L.R.; et al. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 2022, 145, e895–e1032. [Google Scholar] [CrossRef] [PubMed]
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M.; Burri, H.; Butler, J.; Čelutkienė, J.; Chioncel, O.; et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 2021, 42, 3599–3726. [Google Scholar] [CrossRef] [PubMed]
- Reddy, Y.N.V.; Carter, R.E.; Obokata, M.; Redfield, M.M.; Borlaug, B.A. A Simple, Evidence-Based Approach to Help Guide Diagnosis of Heart Failure with Preserved Ejection Fraction. Circulation 2018, 138, 861–870. [Google Scholar] [CrossRef] [PubMed]
- Butler, J.; Usman, M.S.; Khan, M.S.; Greene, S.J.; Friede, T.; Vaduganathan, M.; Filippatos, G.; Coats, A.J.S.; Anker, S.D. Efficacy and safety of SGLT2 inhibitors in heart failure: Systematic review and meta-analysis. ESC Heart Fail. 2020, 7, 3298–3309. [Google Scholar] [CrossRef]
- Kiuchi, S.; Hisatake, S.; Dobashi, S.; Murakami, Y.; Ikeda, T. Role of Vascular Function in the Prognosis of Heart Failure Patients. J. Clin. Med. 2024, 13, 2719. [Google Scholar] [CrossRef]
- Mebazaa, A.; Gheorghiade, M.; Piña, I.L.; Harjola, V.P.; Hollenberg, S.M.; Follath, F.; Rhodes, A.; Plaisance, P.; Roland, E.; Nieminen, M.; et al. Practical recommendations for prehospital and early in-hospital management of patients presenting with acute heart failure syndromes. Crit. Care Med. 2008, 36 (Suppl. S1), S129–S139. [Google Scholar] [CrossRef]
- Sano, T.; Kiuchi, S.; Hisatake, S.; Kabuki, T.; Oka, T.; Fujii, T.; Dobashi, S.; Ikeda, T. Cardio-ankle vascular index predicts the 1-year prognosis of heart failure patients categorized in clinical scenario 1. Heart Vessel. 2020, 35, 1537–1544. [Google Scholar] [CrossRef]
- Seo, Y.; Ohte, N. Effects of Heart Rate Reduction by Ivabradine for Heart Failure Beyond β-Blockers. Circ. J. 2019, 83, 1991–1993. [Google Scholar] [CrossRef]
- Solomon, S.D.; McMurray, J.J.V.; Claggett, B.; de Boer, R.A.; DeMets, D.; Hernandez, A.F.; Inzucchi, S.E.; Kosiborod, M.N.; Lam, C.S.P.; Martinez, F.; et al. Dapagliflozin in Heart Failure with Mildly Reduced or Preserved Ejection Fraction. N. Engl. J. Med. 2022, 387, 1089–1098. [Google Scholar] [CrossRef]
- Vaduganathan, M.; Docherty, K.F.; Claggett, B.L.; Jhund, P.S.; de Boer, R.A.; Hernandez, A.F.; Inzucchi, S.E.; Kosiborod, M.N.; Lam, C.S.P.; Martinez, F.; et al. SGLT-2 inhibitors in patients with heart failure: A comprehensive meta-analysis of five randomised controlled trials. Lancet 2022, 400, 757–767. [Google Scholar] [CrossRef]
- Villacorta, A.S.; Villacorta, H.; Caldas, J.A.; Precht, B.C.; Porto, P.B.; Rodrigues, L.U.; Neves, M.; Xavier, A.R.; Kanaan, S.; Mesquita, C.T.; et al. Effects of Heart Rate Reduction with Either Pyridostigmine or Ivabradine in Patients with Heart Failure: A Randomized, Double-Blind Study. J. Cardiovasc. Pharmacol. Ther. 2019, 24, 139–145. [Google Scholar] [CrossRef] [PubMed]
- Sarullo, F.M.; Fazio, G.; Puccio, D.; Fasullo, S.; Paterna, S.; Novo, S.; Di Pasquale, P. Impact of “off-label” use of ivabradine on exercise capacity, gas exchange, functional class, quality of life, and neurohormonal modulation in patients with ischemic chronic heart failure. Cardiovasc. Pharmacol. Ther. 2010, 15, 349–355. [Google Scholar] [CrossRef] [PubMed]
- Pal, N.; Sivaswamy, N.; Mahmod, M.; Yavari, A.; Rudd, A.; Singh, S.; Dawson, D.K.; Francis, J.M.; Dwight, J.S.; Watkins, H.; et al. Effect of Selective Heart Rate Slowing in Heart Failure with Preserved Ejection Fraction. Circulation 2015, 132, 1719–1725. [Google Scholar] [CrossRef] [PubMed]
- Volterrani, M.; Cice, G.; Caminiti, G.; Vitale, C.; D’Isa, S.; Perrone Filardi, P.; Acquistapace, F.; Marazzi, G.; Fini, M.; Rosano, G.M. Effect of Carvedilol, Ivabradine or their combination on exercise capacity in patients with Heart Failure (the CARVIVA HF trial). Int. J. Cardiol. 2011, 151, 218–224. [Google Scholar] [CrossRef]
- Shiga, T.; Suzuki, T.; Kida, K.; Suzuki, A.; Kohno, T.; Ushijima, A.; Kiuchi, S.; Ishii, S.; Murata, M.; Ijichi, T.; et al. Rationale and Design of the Effect of Ivabradine on Exercise Tolerance in Patients with Chronic Heart Failure (EXCILE-HF) Trial-Protocol for a Multicenter Randomized Controlled Trial. Circ. Rep. 2023, 5, 157–161. [Google Scholar] [CrossRef]
- Florea, V.G.; Rector, T.S.; Anand, I.S.; Cohn, J.N. Heart Failure with Improved Ejection Fraction: Clinical Characteristics, Correlates of Recovery, and Survival: Results From the Valsartan Heart Failure Trial. Circ. Heart Fail. 2016, 9, e003123. [Google Scholar] [CrossRef]
- Ceconi, C.; Freedman, S.B.; Tardif, J.C.; Hildebrandt, P.; McDonagh, T.; Gueret, P.; Parrinello, G.; Robertson, M.; Steg, P.G.; Tendera, M.; et al. Effect of heart rate reduction by ivabradine on left ventricular remodling in the echocardiographic substudy of BEAUTIFUL. Int. J. Cardiol. 2011, 146, 408–414. [Google Scholar] [CrossRef]
- Paterek, A.; Sochanowicz, B.; Oknińska, M.; Śmigielski, W.; Kruszewski, M.; Mackiewicz, U.; Mączewski, M.; Leszek, P. Ivabradine prevents deleterious effects of dopamine therapy in heart failure: No role for HCN4 overexpression. Biomed. Pharmacother. 2021, 136, 111250. [Google Scholar] [CrossRef]
- Milliez, P.; Messaoudi, S.; Nehme, J.; Rodriguez, C.; Samuel, J.L.; Delcayre, C. Beneficial effects of delayed ivabradine treatment on cardiac anatomical and electrical remodeling in rat severe chronic heart failure. Am. J. Physiol. Heart Circ. Physiol. 2009, 296, H435–H441. [Google Scholar] [CrossRef]
- Simko, F.; Baka, T.; Stanko, P.; Repova, K.; Krajcirovicova, K.; Aziriova, S.; Domenig, O.; Zorad, S.; Adamcova, M.; Paulis, L. Sacubitril/Valsartan and Ivabradine Attenuate Left Ventricular Remodelling and Dysfunction in Spontaneously Hypertensive Rats: Different Interactions with the Renin-Angiotensin-Aldosterone System. Biomedicines 2022, 10, 1844. [Google Scholar] [CrossRef]
- Lee, Y.H.; Lin, P.L.; Chiou, W.R.; Huang, J.L.; Lin, W.Y.; Liao, C.T.; Chung, F.P.; Liang, H.W.; Hsu, C.Y.; Chang, H.Y. Combination of ivabradine and sacubitril/valsartan in patients with heart failure and reduced ejection fraction. ESC Heart Fail. 2021, 8, 1204–1215. [Google Scholar] [CrossRef] [PubMed]
- Tang, H.; Germinal, K.; Milfort, A.; Chen, W.H.; Chang, S.H.; Huang, W.; Li, Y.; Lu, Y.; Ahmed, M.M.; Kimmel, S.E.; et al. The most effective combination of pharmacological therapy for heart failure with reduced ejection fraction: A network meta-analysis of randomized controlled trials. BMC Cardiovasc. Disord. 2024, 24, 666. [Google Scholar] [CrossRef] [PubMed]
- McMurray, J.J.V.; Packer, M. How Should We Sequence the Treatments for Heart Failure and a Reduced Ejection Fraction?: A Redefinition of Evidence-Based Medicine. Circulation 2021, 143, 875–877. [Google Scholar] [CrossRef]
- Chiu, M.H.; Howlett, J.G.; Sharma, N.C. Initiation of ivabradine in cardiogenic shock. ESC Heart Fail. 2019, 6, 1088–1091. [Google Scholar] [CrossRef] [PubMed]
- Lopatin, Y.M.; Cowie, M.R.; Grebennikova, A.A.; Sisakian, H.S.; Pagava, Z.M.; Hayrapetyan, H.G.; Abdullaev, T.A.; Voronkov, L.G.; Chesnikova, A.I.; Tseluyko, V.I.; et al. Optimaization of heart rate lowering therapy in hospitalized patients with heart failure: Insights from the Optimizr Heart Failure Care Program. Int. J. Cardiol. 2018, 260, 113–117. [Google Scholar] [CrossRef]
- Hori, M.; Imamura, T.; Tanaka, S.; Ueno, H.; Joho, S.; Fukahara, K.; Kajiura, S.; Kinugawa, K. Primary Cardiac Angiosarcoma Accompanying Cardiac Tamponade. Intern. Med. 2022, 61, 1015–1019. [Google Scholar] [CrossRef]
- Hidalgo, F.J.; Anguita, M.; Castillo, J.C.; Rodríguez, S.; Pardo, L.; Durán, E.; Sánchez, J.J.; Ferreiro, C.; Pan, M.; Mesa, D.; et al. Effect of early treatment with ivabradine combined with beta-blockers versus beta-blockers alone in patients hospitalised with heart failure and reduced left ventricular ejection fraction (ETHIC-AHF): A randomised study. Int. J. Cardiol. 2016, 217, 7–11. [Google Scholar] [CrossRef]
- Yang, T.Y.; Tsai, M.S.; Jan, J.Y.; Chang, J.J.; Chung, C.M.; Lin, M.S.; Chen, H.M.; Lin, Y.S. Early administration of ivabradine in patients admitted for acute decompensated heart failure. Front. Cardiovasc. Med. 2022, 9, 1036418. [Google Scholar] [CrossRef]
- Su, Y.; Ma, T.; Wang, Z.; Dong, B.; Tai, C.; Wang, H.; Zhang, F.; Yan, C.; Chen, W.; Xu, Y.; et al. Efficacy of early initiation of ivabradine treatment in patients with acute heart failure: Rationale and design of SHIFT-AHF trial. ESC Heart Fail. 2020, 7, 4465–4471. [Google Scholar] [CrossRef]
- Custodis, F.; Schirmer, S.H.; Baumhäkel, M.; Heusch, G.; Böhm, M.; Laufs, U. Vascular pathophysiology in response to increased heart rate. J. Am. Coll. Cardiol. 2010, 56, 1973–1983. [Google Scholar] [CrossRef]
- Colin, P.; Ghaleh, B.; Monnet, X.; Su, J.; Hittinger, L.; Giudicelli, J.F.; Berdeaux, A. Contributions of heart rate and contractility to myocardial oxygen balance during exercise. Am. J. Physiol. Heart Circ. Physiol. 2003, 284, H676–H682. [Google Scholar] [CrossRef] [PubMed]
- Anantha Narayanan, M.; Reddy, Y.N.; Baskaran, J.; Deshmukh, A.; Benditt, D.G.; Raveendran, G. Ivabradine in the treatment of systolic heart failure—A systematic review and meta-analysis. World J. Cardiol. 2017, 9, 182–190. [Google Scholar] [CrossRef] [PubMed]
- Kiuchi, S.; Hisatake, S.; Kabuki, T.; Oka, T.; Fujii, T.; Dobashi, S.; Sano, T.; Ikeda, T. Efficacy and Safety of Ivabradine in an Elderly Patient with Heart Failure with Reduced Ejection Fraction. Clin. Drug Investig. 2021, 41, 193–196. [Google Scholar] [CrossRef]
- Pay, L.; Yumurtaş, A.Ç.; Tezen, O.; Çetin, T.; Keskin, K.; Eren, S.; Çinier, G.; Hayıroğlu, M.İ.; Çınar, T.; Tekkeşin, A.İ. Effect of ivabradine on ventricular arrhythmias in heart failure patients with reduced ejection fraction. Rev. Assoc. Med. Bras. 2023, 69, e20230703. [Google Scholar] [CrossRef]
- Oknińska, M.; Paterek, A.; Zambrowska, Z.; Mackiewicz, U.; Mączewski, M. Effect of Ivabradine on Cardiac Ventricular Arrhythmias: Friend or Foe? J. Clin. Med. 2021, 10, 4732. [Google Scholar] [CrossRef]
- Wang, Z.; Wang, W.; Li, H.; Zhang, A.; Han, Y.; Wang, J.; Hou, Y. Ivabradine and Atrial Fibrillation: A Meta-Analysis of Randomized Controlled Trials. J. Cardiovasc. Pharmacol. 2022, 79, 549–557. [Google Scholar] [CrossRef]
- Lin, Y.S.; Jan, J.Y.; Chang, J.J.; Lin, M.S.; Yang, T.Y.; Wang, P.C.; Chen, M.C. Ivabradine in heart failure patients with reduced ejection fraction and history of paroxysmal atrial fibrillation. ESC Heart Fail. 2022, 9, 2548–2557. [Google Scholar] [CrossRef]
- Hardison, E.; Cox, Z.L.; Heckman, K.; Kelly, P.A.; Lindenfeld, J. A case report of ivabradine used for heart rate control of atrial fibrillation in acute decompensated heart failure. Eur. Heart J. Case Rep. 2022, 6, ytac077. [Google Scholar] [CrossRef]
- Scridon, A.; Halaţiu, V.B.; Balan, A.I.; Cozac, D.A.; Moldovan, V.; Bănescu, C.; Perian, M.; Şerban, R.C. Long-Term Effects of Ivabradine on Cardiac Vagal Parasympathetic Function in Normal Rats. Front. Pharmacol. 2021, 12, 596956. [Google Scholar] [CrossRef]
- Benezet-Mazuecos, J.; Rubio, J.M.; Farré, J.; Quiñones, M.Á.; Sanchez-Borque, P.; Macía, E. Long-term outcomes of ivabradine in inappropriate sinus tachycardia patients: Appropriate efficacy or inappropriate patients. Pacing Clin. Electrophysiol. 2013, 36, 830–836. [Google Scholar] [CrossRef]
- Doesch, A.O.; Mueller, S.; Erbel, C.; Gleissner, C.A.; Frankenstein, L.; Hardt, S.; Ruhparwar, A.; Ehlermann, P.; Dengler, T.; Katus, H.A. Heart rate reduction for 36 months with ivabradine reduces left ventricular mass in cardiac allograft recipients: A long-term follow-up study. Drug Des. Dev. Ther. 2013, 7, 1323–1328. [Google Scholar] [CrossRef] [PubMed]
- Tavazzi, L.; Swedberg, K.; Komajda, M.; Böhm, M.; Borer, J.S.; Lainscak, M.; Ford, I.; SHIFT Investigators. Efficacy and safety of ivabradine in chronic heart failure across the age spectrum: Insights from the SHIFT study. Eur. J. Heart Fail. 2013, 15, 1296–1303. [Google Scholar] [CrossRef] [PubMed]
- van der Wal, M.H.; Jaarsma, T. Adherence in heart failure in the elderly: Problem and possible solutions. Int. J. Cardiol. 2008, 125, 203–208. [Google Scholar] [CrossRef] [PubMed]
- Ye, F.; Wang, X.; Wu, S.; Ma, S.; Zhang, Y.; Liu, G.; Liu, K.; Yang, Z.; Pang, X.; Xue, L.; et al. Sustained-Release Ivabradine Hemisulfate in Patients with Systolic Heart Failure. J. Am. Coll. Cardiol. 2022, 80, 584–594. [Google Scholar] [CrossRef] [PubMed]
| Study | Number of Subjects | Average Heart Rate (bpm) | Average Follow-Up Period | Induction Rates of β-Blockers | Main Outcomes |
|---|---|---|---|---|---|
| Komajda, M. et al., 2017 [26] | 179 | 72 | 8 years | 74% | HR reduction with ivabradine did not improve outcome |
| Cacciapuoti, F. et al., 2017 [28] | 26 | 81 | 12 weeks | 80% | Ivabradine improved LV diastolic function |
| Conceição, L.S.R. et al., 2021 [29] | 136 | N/A | N/A | N/A | Ivabradine did not improve LV diastolic function |
| Kosmala, W. et al., 2013 [30] | 61 | 72 | 7 days | 57% | Ivabradine increased exercise capacity |
| Tanaka, H. et al., 2022 [27] | 18 | 85 | 3 months | 50% | Ivabradine did not improve LV diastolic function |
| Study | Number of Subjects | Average Age (Years) | Underlying Heart Disease | Type of Heart Failure | Main Outcomes |
|---|---|---|---|---|---|
| Villacorta, A.S. et al., 2019 [41] | 21 | Ivabradine: 56.2 Pyridostigmine: 62.6 | N/A | HFpEF | Ivabradine improved exercise tolerance and neurohormonal and inflammatory profiles |
| Kosmala, W. et al., 2013 [30] | 61 | Ivabradine: 66.5 Placebo: 68.0 | N/A | HFpEF | Ivabradine increased exercise capacity left ventricular filling pressure |
| Sarullo, F.M. et al., 2010 [42] | 60 | 52.7 | Ischemic Cardiomyopathy | HFrEF | Ivabradine improved exercise tolerance, gas exchange, functional heart failure class, and quality of life |
| Pal, N. et al. 2018 [43] | 22 | 74.6 | N/A | HFpEF | Ivabradine compared with placebo worsened the change in peak Vo2 in HFpEF patients |
| Volterrani, M. et al., 2013 [44] | 121 | Ivabradine: 67.2 Carvedilol: 66.7 Combination: 66.5 | Ischemic Cardiomyopathy Ivabradine: 80% Carvedilol: 84% Combination: 79% | HFrEF | Ivabradine alone or in combination with carvedilol is more effective than carvedilol alone in improving exercise tolerance |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kiuchi, S.; Ikeda, T. Heart Rate Reduction and the Prognosis of Heart Failure Focused on Ivabradine. J. Clin. Med. 2025, 14, 1074. https://doi.org/10.3390/jcm14041074
Kiuchi S, Ikeda T. Heart Rate Reduction and the Prognosis of Heart Failure Focused on Ivabradine. Journal of Clinical Medicine. 2025; 14(4):1074. https://doi.org/10.3390/jcm14041074
Chicago/Turabian StyleKiuchi, Shunsuke, and Takanori Ikeda. 2025. "Heart Rate Reduction and the Prognosis of Heart Failure Focused on Ivabradine" Journal of Clinical Medicine 14, no. 4: 1074. https://doi.org/10.3390/jcm14041074
APA StyleKiuchi, S., & Ikeda, T. (2025). Heart Rate Reduction and the Prognosis of Heart Failure Focused on Ivabradine. Journal of Clinical Medicine, 14(4), 1074. https://doi.org/10.3390/jcm14041074






