Persistently Active Helicobacter pylori Infection Is Associated with the Development of Metabolic Dysfunction-Associated Steatotic Liver Disease
Abstract
1. Introduction
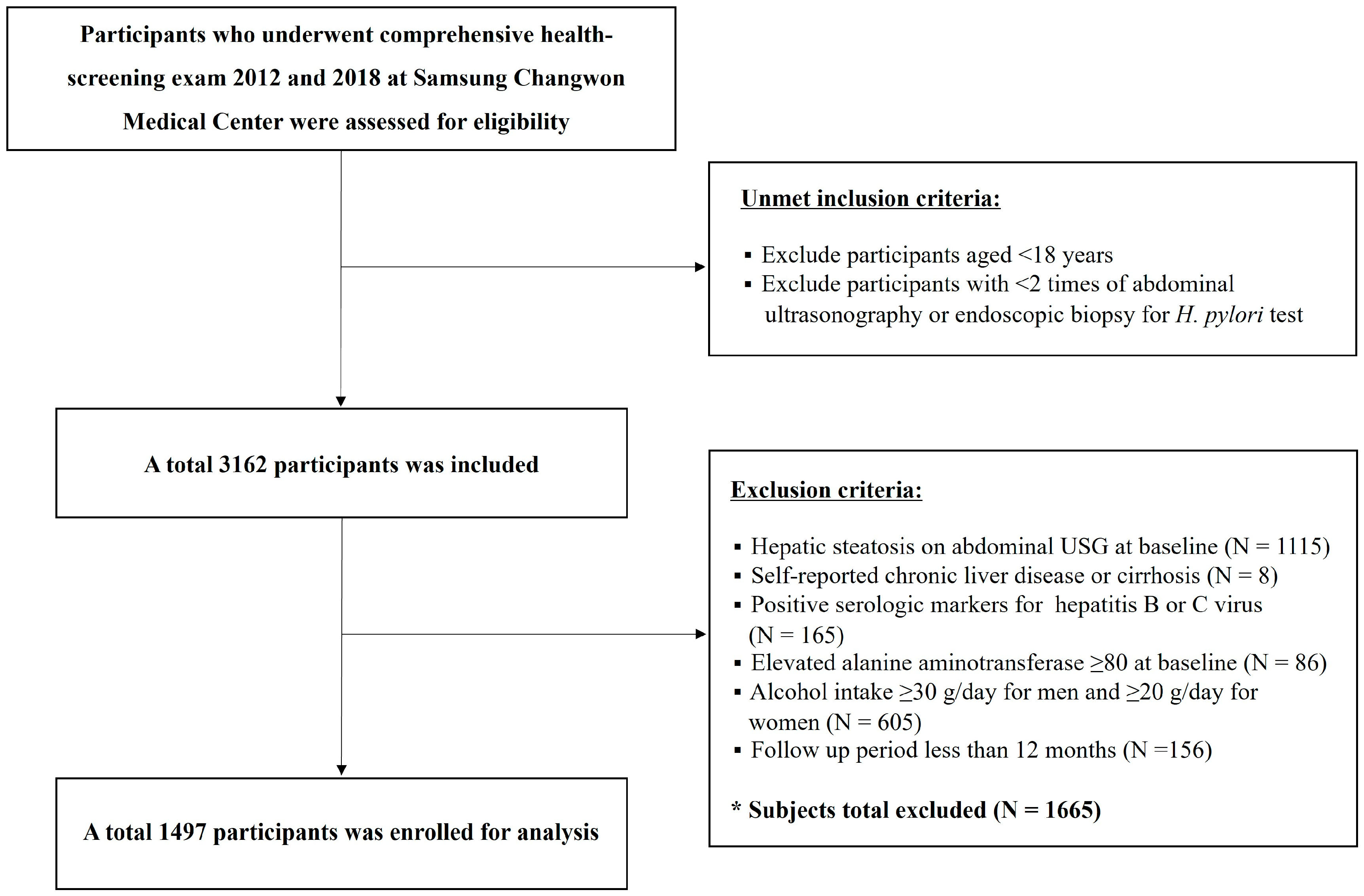
2. Materials and Methods
2.1. Database
2.2. Data Collection and Variables
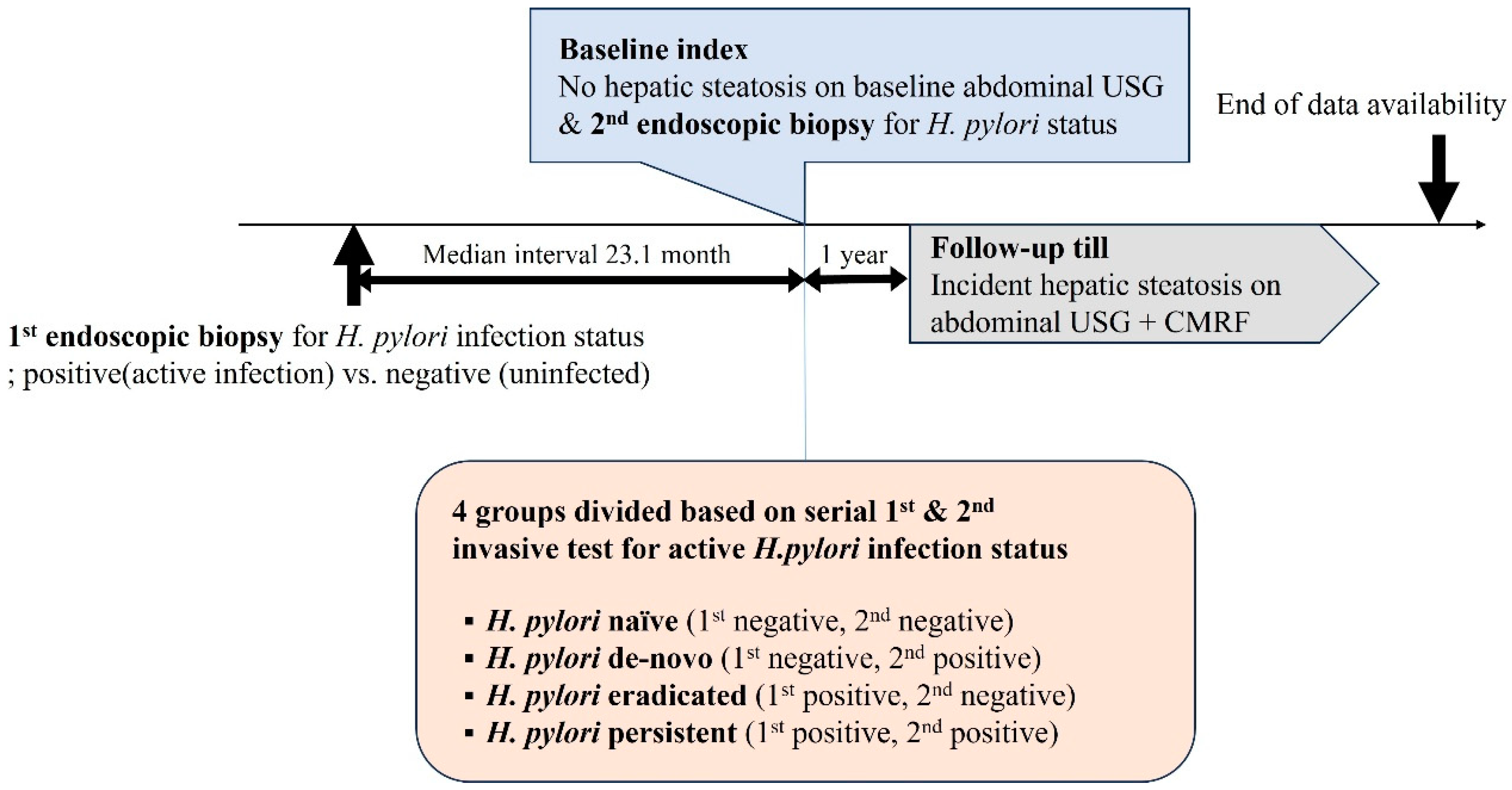
2.3. H. pylori Diagnosis and Definition of Active H. pylori Infection Status
2.4. Definition of MASLD Development
2.5. Statistical Analysis
3. Results
3.1. Basic Characteristics of the Study Cohort
3.2. Factors Associated with MASLD Development
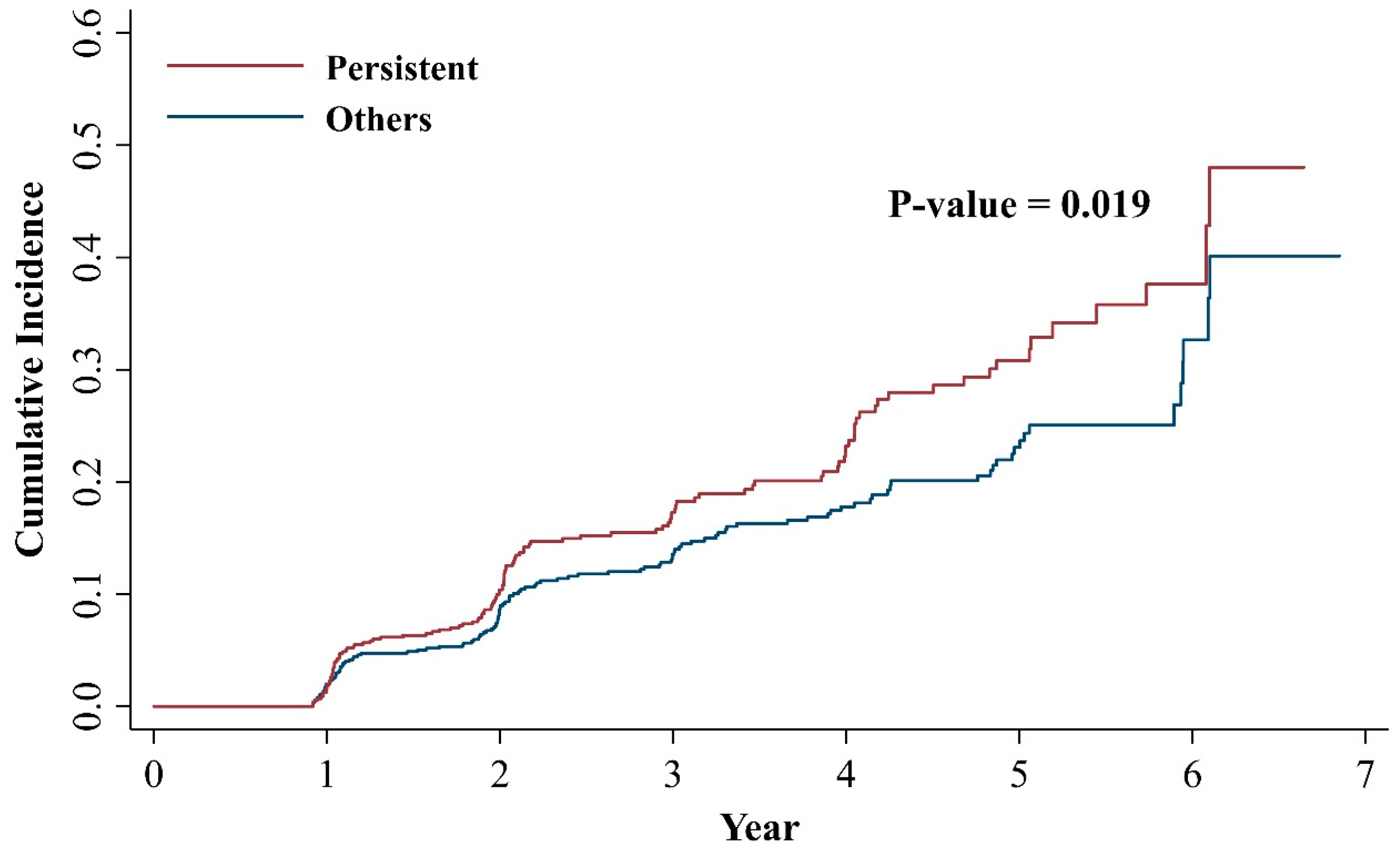
3.3. Active H. pylori Infection and the Development of MASLD
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Coelho, L.G.V.; Marinho, J.R.; Genta, R.; Ribeiro, L.T.; Passos, M.; Zaterka, S.; Assumpcao, P.P.; Barbosa, A.J.A.; Barbuti, R.; Braga, L.L.; et al. Ivth Brazilian Consensus Conference on Helicobacter Pylori Infection. Arq. Gastroenterol. 2018, 55, 97–121. [Google Scholar] [CrossRef]
- Everhart, J.E. Recent developments in the epidemiology of Helicobacter pylori. Gastroenterol. Clin. N. Am. 2000, 29, 559–578. [Google Scholar] [CrossRef]
- Leja, M.; Grinberga-Derica, I.; Bilgilier, C.; Steininger, C. Review: Epidemiology of Helicobacter pylori infection. Helicobacter 2019, 24 (Suppl. S1), e12635. [Google Scholar] [CrossRef]
- Santos, M.L.C.; de Brito, B.B.; da Silva, F.A.F.; Sampaio, M.M.; Marques, H.S.; Oliveira, E.S.N.; de Magalhaes Queiroz, D.M.; de Melo, F.F. Helicobacter pylori infection: Beyond gastric manifestations. World J. Gastroenterol. 2020, 26, 4076–4093. [Google Scholar] [CrossRef]
- Mladenova, I.; Durazzo, M. Transmission of Helicobacter pylori. Minerva Gastroenterol. Dietol. 2018, 64, 251–254. [Google Scholar] [CrossRef]
- Liu, J.; Wang, F.; Shi, S. Helicobacter pylori Infection Increase the Risk of Myocardial Infarction: A Meta-Analysis of 26 Studies Involving more than 20,000 Participants. Helicobacter 2015, 20, 176–183. [Google Scholar] [CrossRef]
- Wang, F.; Liu, J.; Lv, Z. Association of Helicobacter pylori infection with diabetes mellitus and diabetic nephropathy: A meta-analysis of 39 studies involving more than 20,000 participants. Scand. J. Infect. Dis. 2013, 45, 930–938. [Google Scholar] [CrossRef]
- Gunji, T.; Matsuhashi, N.; Sato, H.; Fujibayashi, K.; Okumura, M.; Sasabe, N.; Urabe, A. Helicobacter pylori infection is significantly associated with metabolic syndrome in the Japanese population. Am. J. Gastroenterol. 2008, 103, 3005–3010. [Google Scholar] [CrossRef]
- Younossi, Z.M.; Koenig, A.B.; Abdelatif, D.; Fazel, Y.; Henry, L.; Wymer, M. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology 2016, 64, 73–84. [Google Scholar] [CrossRef] [PubMed]
- Rinella, M.E.; Lazarus, J.V.; Ratziu, V.; Francque, S.M.; Sanyal, A.J.; Kanwal, F.; Romero, D.; Abdelmalek, M.F.; Anstee, Q.M.; Arab, J.P.; et al. A multisociety Delphi consensus statement on new fatty liver disease nomenclature. Ann. Hepatol. 2024, 29, 101133. [Google Scholar] [CrossRef] [PubMed]
- Rinella, M.E.; Sookoian, S. From NAFLD to MASLD: Updated naming and diagnosis criteria for fatty liver disease. J. Lipid Res. 2024, 65, 100485. [Google Scholar] [CrossRef]
- Hagström, H.; Vessby, J.; Ekstedt, M.; Shang, Y. 99% of patients with NAFLD meet MASLD criteria and natural history is therefore identical. J. Hepatol. 2024, 80, e76–e77. [Google Scholar] [CrossRef] [PubMed]
- Buzzetti, E.; Pinzani, M.; Tsochatzis, E.A. The multiple-hit pathogenesis of non-alcoholic fatty liver disease (NAFLD). Metabolism 2016, 65, 1038–1048. [Google Scholar] [CrossRef] [PubMed]
- Schoeler, M.; Caesar, R. Dietary lipids, gut microbiota and lipid metabolism. Rev. Endocr. Metab. Disord. 2019, 20, 461–472. [Google Scholar] [CrossRef]
- Leung, C.; Rivera, L.; Furness, J.B.; Angus, P.W. The role of the gut microbiota in NAFLD. Nat. Rev. Gastroenterol. Hepatol. 2016, 13, 412–425. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Peng, R.; Peng, D.; Liu, D.; Li, R. Helicobacter pylori infection exacerbates metabolic dysfunction-associated steatotic liver disease through lipid metabolic pathways: A transcriptomic study. J. Transl. Med. 2024, 22, 701. [Google Scholar] [CrossRef]
- Kim, T.J.; Sinn, D.H.; Min, Y.W.; Son, H.J.; Kim, J.J.; Chang, Y.; Baek, S.Y.; Ahn, S.H.; Lee, H.; Ryu, S. A cohort study on Helicobacter pylori infection associated with nonalcoholic fatty liver disease. J. Gastroenterol. 2017, 52, 1201–1210. [Google Scholar] [CrossRef]
- Yu, Y.Y.; Tong, Y.L.; Wu, L.Y.; Yu, X.Y. Helicobacter pylori infection eradication for nonalcoholic fatty liver disease: A randomized controlled trial. Sci. Rep. 2022, 12, 19530. [Google Scholar] [CrossRef] [PubMed]
- Liu, R.; Liu, Q.; He, Y.; Shi, W.; Xu, Q.; Yuan, Q.; Lin, Q.; Li, B.; Ye, L.; Min, Y.; et al. Association between Helicobacter pylori infection and nonalcoholic fatty liver: A meta-analysis. Medicine 2019, 98, e17781. [Google Scholar] [CrossRef]
- Mantovani, A.; Lando, M.G.; Borella, N.; Scoccia, E.; Pecoraro, B.; Gobbi, F.; Bisoffi, Z.; Valenti, L.; Tilg, H.; Byrne, C.D.; et al. Relationship between Helicobacter pylori infection and risk of metabolic dysfunction-associated steatotic liver disease: An updated meta-analysis. Liver Int. 2024, 44, 1513–1525. [Google Scholar] [CrossRef] [PubMed]
- Okushin, K.; Takahashi, Y.; Yamamichi, N.; Shimamoto, T.; Enooku, K.; Fujinaga, H.; Tsutsumi, T.; Shintani, Y.; Sakaguchi, Y.; Ono, S.; et al. Helicobacter pylori infection is not associated with fatty liver disease including non-alcoholic fatty liver disease: A large-scale cross-sectional study in Japan. BMC Gastroenterol. 2015, 15, 25. [Google Scholar] [CrossRef]
- Baeg, M.K.; Yoon, S.K.; Ko, S.H.; Noh, Y.S.; Lee, I.S.; Choi, M.G. Helicobacter pylori infection is not associated with nonalcoholic fatty liver disease. World J. Gastroenterol. 2016, 22, 2592–2600. [Google Scholar] [CrossRef]
- Fan, N.; Peng, L.; Xia, Z.; Zhang, L.; Wang, Y.; Peng, Y. Helicobacter pylori Infection Is Not Associated with Non-alcoholic Fatty Liver Disease: A Cross-Sectional Study in China. Front. Microbiol. 2018, 9, 73. [Google Scholar] [CrossRef] [PubMed]
- Wernly, S.; Wernly, B.; Semmler, G.; Völkerer, A.; Rezar, R.; Semmler, L.; Stickel, F.; Aigner, E.; Niederseer, D.; Datz, C. Non-alcoholic fatty liver disease is not independently associated with Helicobacter pylori in a central European screening cohort. Minerva Medica 2022, 113, 936–949. [Google Scholar] [CrossRef] [PubMed]
- Jin, E.S.; Shim, J.S.; Kim, S.E.; Bae, J.H.; Kang, S.; Won, J.C.; Shin, M.J.; Jin, H.Y.; Moon, J.; Lee, H.; et al. Dyslipidemia Fact Sheet in South Korea, 2022. Diabetes Metab. J. 2023, 47, 632–642. [Google Scholar] [CrossRef]
- Seo, J.-y.; Ahn, J.Y. Endoscopic Features According to Helicobacter pylori Infection Status. Korean J. Med. 2023, 98, 117–124. [Google Scholar] [CrossRef]
- Ferraioli, G.; Soares Monteiro, L.B. Ultrasound-based techniques for the diagnosis of liver steatosis. World J. Gastroenterol. 2019, 25, 6053–6062. [Google Scholar] [CrossRef]
- Heydari, K.; Yousefi, M.; Alizadeh-Navaei, R.; Lotfi, P.; Sheydaee, F.; Raei, M.; Vahdatinia, A.; Hessami, A.; Rafati, S.; Moosazadeh, M.; et al. Helicobacter pylori Infection and Non-alcoholic Fatty Liver Disease: A Systematic Review and Meta-Analysis. Turk. J. Gastroenterol. 2022, 33, 171–181. [Google Scholar] [CrossRef]
- Zhou, B.G.; Yang, H.J.; Xu, W.; Wang, K.; Guo, P.; Ai, Y.W. Association between Helicobacter pylori infection and nonalcoholic fatty liver disease: A systematic review and meta-analysis of observational studies. Helicobacter 2019, 24, e12576. [Google Scholar] [CrossRef] [PubMed]
- Mantovani, A.; Turino, T.; Altomari, A.; Lonardo, A.; Zoppini, G.; Valenti, L.; Tilg, H.; Byrne, C.D.; Targher, G. Association between Helicobacter pylori infection and risk of nonalcoholic fatty liver disease: An updated meta-analysis. Metabolism 2019, 96, 56–65. [Google Scholar] [CrossRef] [PubMed]
- Abdel-Razeq, R.; Bitar, L.; Bitar, E.R.; Onwuzo, C.; Abu-Hammour, M.N.; Eren, B.; Mohamed, I.; Johnson, A.; Boustany, A.; Onwuzo, S.; et al. Prevalence and risk factors associated with metabolic dysfunction-associated steatohepatitis in patients with Helicobacter pylori infection: A population-based study. World J. Hepatol. 2024, 16, 1169–1176. [Google Scholar] [CrossRef]
- Doulberis, M.; Srivastava, S.; Polyzos, S.A.; Kountouras, J.; Papaefthymiou, A.; Klukowska-Rotzler, J.; Blank, A.; Exadaktylos, A.K.; Srivastava, D.S. Active Helicobacter pylori Infection is Independently Associated with Nonalcoholic Steatohepatitis in Morbidly Obese Patients. J. Clin. Med. 2020, 9, 933. [Google Scholar] [CrossRef] [PubMed]
- Yu, L.Y.; Hu, K.C.; Liu, C.J.; Hung, C.L.; Bair, M.J.; Chen, M.J.; Wang, H.Y.; Wu, M.S.; Shih, S.C.; Liu, C.C. Helicobacter pylori infection combined with non-alcoholic fatty liver disease increase the risk of atherosclerosis: Focus in carotid artery plaque. Medicine 2019, 98, e14672. [Google Scholar] [CrossRef] [PubMed]
- Lecube, A.; Valladares, S.; López-Cano, C.; Gutiérrez, L.; Ciudin, A.; Fort, J.M.; Reñé, J.M.; Matias-Guiu, X.; de Torres, I.; Bueno, M.; et al. The Role of Morbid Obesity in the Promotion of Metabolic Disruptions and Non-Alcoholic Steatohepatitis by Helicobacter Pylori. PLoS ONE 2016, 11, e0166741. [Google Scholar] [CrossRef] [PubMed]
- Gulati, A.; Roytman, M.; Lin, J.; McGrath, M.; Klar, A.; Boone, K.; Higa, K.; Ma, P. Association between Helicobacter pylori infection, MASLD, and liver fibrosis in patients with severe obesity: A single-center experience. Surg. Endosc. 2024, 38, 6873–6879. [Google Scholar] [CrossRef]
- Córdova-Gallardo, J.; Martínez-Sánchez, F.D.; Medina-Julio, D.; Rojano-Rodríguez, M.E.; Romero-Loera, L.S.; Vargas-Agredano, R.; Méndez-Sánchez, N. Helicobacter pylori infection is associated with liver fibrosis in patients with obesity undergoing bariatric surgery. JGH Open 2024, 8, e70023. [Google Scholar] [CrossRef] [PubMed]
- Miele, L.; Valenza, V.; La Torre, G.; Montalto, M.; Cammarota, G.; Ricci, R.; Mascianà, R.; Forgione, A.; Gabrieli, M.L.; Perotti, G.; et al. Increased intestinal permeability and tight junction alterations in nonalcoholic fatty liver disease. Hepatology 2009, 49, 1877–1887. [Google Scholar] [CrossRef]
- Sabaté, J.M.; Jouët, P.; Harnois, F.; Mechler, C.; Msika, S.; Grossin, M.; Coffin, B. High prevalence of small intestinal bacterial overgrowth in patients with morbid obesity: A contributor to severe hepatic steatosis. Obes. Surg. 2008, 18, 371–377. [Google Scholar] [CrossRef] [PubMed]
- Polyzos, S.A.; Kountouras, J.; Zavos, C.; Deretzi, G. The association between Helicobacter pylori infection and insulin resistance: A systematic review. Helicobacter 2011, 16, 79–88. [Google Scholar] [CrossRef] [PubMed]
- Waluga, M.; Kukla, M.; Żorniak, M.; Bacik, A.; Kotulski, R. From the stomach to other organs: Helicobacter pylori and the liver. World J. Hepatol. 2015, 7, 2136–2146. [Google Scholar] [CrossRef] [PubMed]
- Polyzos, S.A.; Kountouras, J. Novel Advances in the Association Between Helicobacter pylori Infection, Metabolic Syndrome, and Related Morbidity. Helicobacter 2015, 20, 405–409. [Google Scholar] [CrossRef]
- Shin, D.W.; Kwon, H.T.; Kang, J.M.; Park, J.H.; Choi, H.C.; Park, M.S.; Park, S.M.; Son, K.Y.; Cho, B. Association between metabolic syndrome and Helicobacter pylori infection diagnosed by histologic status and serological status. J. Clin. Gastroenterol. 2012, 46, 840–845. [Google Scholar] [CrossRef]
- Upala, S.; Jaruvongvanich, V.; Riangwiwat, T.; Jaruvongvanich, S.; Sanguankeo, A. Association between Helicobacter pylori infection and metabolic syndrome: A systematic review and meta-analysis. J. Dig. Dis. 2016, 17, 433–440. [Google Scholar] [CrossRef] [PubMed]
- Powell, E.E.; Wong, V.W.; Rinella, M. Non-alcoholic fatty liver disease. Lancet 2021, 397, 2212–2224. [Google Scholar] [CrossRef] [PubMed]
- Hernaez, R.; Lazo, M.; Bonekamp, S.; Kamel, I.; Brancati, F.L.; Guallar, E.; Clark, J.M. Diagnostic accuracy and reliability of ultrasonography for the detection of fatty liver: A meta-analysis. Hepatology 2011, 54, 1082–1090. [Google Scholar] [CrossRef]

| Total (n = 1497) | H. pylori Naïve (n = 365) | H. pylori De Novo (n = 203) | H. pylori Eradicated (n = 199) | H. pylori Persistent (n = 730) | p-Value | |
|---|---|---|---|---|---|---|
| Age (years) | 46.71 ± 7.17 | 48.85 ± 7.67 | 47.83 ± 7.14 | 46.72 ± 7.29 | 45.32 ± 6.56 | <0.001 |
| Male (%) | 956 (63.9) | 218 (59.7) | 133 (65.5) | 133 (66.8) | 472 (64.7) | 0.272 |
| Body mass index (kg/m2) | 23.14 ± 2.55 | 23.02 ± 2.42 | 23.18 ± 2.58 | 23.14 ± 2.40 | 23.20 ± 2.65 | 0.740 |
| <18.5 | 44 (2.94) | 10 (2.74) | 5 (2.46) | 5 (2.51) | 24 (3.29) | |
| 18.5–24.9 | 1110 (74.15) | 278 (76.16) | 145 (71.43) | 150 (75.38) | 537 (73.56) | |
| 25–29.9 | 305 (20.37) | 66 (18.08) | 46 (22.66) | 43 (21.61) | 150 (20.55) | |
| ≥30 | 17 (1.14) | 6 (1.64) | 1 (0.49) | 0 (0.00) | 10 (1.37) | |
| Smoking | 0.296 | |||||
| Never smoker | 533 (35.60) | 125 (34.25) | 68 (33.50) | 77 (38.69) | 263 (36.03) | |
| Current(<1 pack/day) | 428 (28.59) | 97 (26.58) | 59 (29.06) | 56 (28.14) | 216 (29.59) | |
| Current(≥1 pack/day) | 268 (17.90) | 59 (16.16) | 38 (18.72) | 37 (18.59) | 134 (18.36) | |
| Alcohol | 0.085 | |||||
| 10 g/day) | 442 (29.53) | 116 (31.78) | 53 (26.11) | 55 (27.64) | 218 (29.86) | |
| Modest (≥10 g/day) | 690 (46.09) | 151 (41.37) | 89 (43.84) | 103 (51.76) | 347 (47.53) | |
| Regular exercise | 229 (19.97) | 74 (20.27) | 34 (16.75) | 44 (22.11) | 147 (20.14) | 0.021 |
| hsCRP (mg/dL) | 1.02 ± 3.29 | 0.96 ± 2.28 | 1.47 ± 5.72 | 1.02 ± 2.19 | 0.93 ± 3.04 | 0.222 |
| SBP (mmHg) | 116.66 ± 11.38 | 116.31 ± 11.65 | 118.79 ± 11.58 | 117.94 ± 10.98 | 115.90 ± 11.22 | 0.005 |
| Fasting glucose (mg/dL) | 89.46 ± 14.74 | 89.46 ± 11.69 | 89.58 ± 21.77 | 89.97 ± 18.96 | 89.28 ± 12.22 | 0.950 |
| AST (U/I) | 22.11 ± 8.37 | 23.30 ± 9.16 | 22.34 ± 8.73 | 22.98 ± 9.46 | 21.21 ± 7.41 | <0.001 |
| ALT (U/I) | 20.29 ± 10.37 | 20.61 ± 10.46 | 20.79 ± 10.40 | 20.87 ± 10.96 | 19.83 ± 10.14 | 0.411 |
| GGT (U/I) | 26.55 ± 28.65 | 24.57 ± 22.89 | 27.71 ± 28.58 | 24.68 ± 21.93 | 27.74 ± 32.58 | 0.247 |
| Dyslipidemia (%) | 27.5 | 26.8 | 29.1 | 25.1 | 28.1 | 0.798 |
| HOMA-IR | 0.94 ± 0.61 | 0.92 ± 0.57 | 0.92 ± 0.66 | 0.95 ± 0.59 | 0.95 ± 0.62 | 0.925 |
| MASLD (%) | 247 (16.5) | 57 (15.6) | 31 (15.3) | 32 (16.1) | 127 (17.4) | |
| Follow up (month) | 31.1 (12, 83.3) | 39.0 (12, 83.3) | 33.8 (12, 77.5) | 31.9 (12, 74.6) | 25.5 (12, 80.8) | |
| Interval between serial biopsy (months) | 23.1 (5.0, 77.5) | 21.6 (5.0, 73.1) | 24.6 (7.4, 70.3) | 22.4 (5.2, 73.7) | 23.2 (5.8, 77.5) |
| Univariable Analysis | Multivariable Analysis | |||
|---|---|---|---|---|
| HR (95% CI) | p-Value | HR (95% CI) | p-Value | |
| Age | 1.02 (1.00, 1.04) | 0.019 | 1.02 (1.00, 1.04) | 0.033 |
| Male sex | 3.00 (2.14, 4.21) | <0.001 | 1.89 (1.18, 3.01) | 0.008 |
| Body mass index (kg/m2) | ||||
| <18.5 | - | - | ||
| 18.5–24.9 | Reference | Reference | ||
| 25–29.9 | 2.87 (2.20, 3.74) | <0.001 | 1.99 (1.49, 2.66) | <0.001 |
| ≥30 | 6.70 (3.52, 12.75) | <0.001 | 6.48 (3.31, 12.69) | <0.001 |
| Smoking | ||||
| Never smoker | Reference | Reference | ||
| Current(<1 pack/day) | 2.50 (1.76, 3.56) | <0.001 | 1.40 (0.92, 2.13) | 0.115 |
| Current(≥1 pack/day) | 2.47 (1.67, 3.65) | <0.001 | 1.17 (0.75, 1.84) | 0.487 |
| Alcohol | ||||
| 10 g/day) | Reference | Reference | ||
| 10 g/day) | 1.64 (1.19, 2.26) | 0.002 | 0.91 (0.64, 1.29) | 0.598 |
| Regular exercise | 0.84 (0.61, 1.17) | 0.315 | 0.83 (0.59, 1.17) | 0.288 |
| hsCRP (mg/dL) | 1.02 (1.00, 1.05) | 0.074 | ||
| SBP (mmHg) | 1.02 (1.01, 1.03) | 0.001 | 1.00 (0.99, 1.01) | 0.726 |
| Fasting glucose (mg/dL) | 1.01 (1.01, 1.02) | <0.001 | 1.01 (1.00, 1.01) | 0.022 |
| AST (U/I) | 1.02 (1.01, 1.04) | <0.001 | 0.99 (0.97, 1.01) | 0.406 |
| ALT (U/I) | 1.04 (1.03, 1.05) | <0.001 | 1.02 (1.01, 1.04) | 0.004 |
| GGT (U/I) | 1.01 (1.01, 1.01) | <0.001 | 1.01 (1.00, 1.01) | 0.003 |
| Dyslipidemia (%) | 2.23 (1.73, 2.86) | <0.001 | 1.51 (1.15, 1.97) | 0.003 |
| Active H. pylori infection | ||||
| H. pylori naïve | Reference | Reference | ||
| H. pylori de novo | 1.21 (0.78, 1.88) | 0.388 | 1.04 (0.65, 1.65) | 0.884 |
| H. pylori eradicated | 1.18 (0.77, 1.82) | 0.446 | 1.18 (0.75, 1.85) | 0.472 |
| H. pylori persistent | 1.48 (1.08, 2.02) | 0.015 | 1.41 (1.01, 1.96) | 0.045 |
| Model 0 | Model 1 | Model 2 | Model 3 | |||||
|---|---|---|---|---|---|---|---|---|
| Adjusted for | - | Age, Sex | Metabolic Risk | Liver Profiles | ||||
| HR (95% CI) | p-Value | HR (95% CI) | p-Value | HR (95% CI) | p-Value | HR (95% CI) | p-Value | |
| Naïve (−/−) | Reference | Reference | Reference | Reference | ||||
| De novo (−/+) | 1.21 (0.78, 1.88) | 0.388 | 1.13 (0.73, 1.76) | 0.573 | 1.11 (0.70, 1.76) | 0.659 | 1.04 (0.65, 1.65) | 0.884 |
| Eradicated (+/−) | 1.18 (0.77, 1.82) | 0.446 | 1.16 (0.75, 1.79) | 0.516 | 1.13 (0.72, 1.76) | 0.596 | 1.18 (0.75, 1.85) | 0.472 |
| Persistent (+/+) | 1.48 (1.08, 2.02) | 0.015 | 1.48 (1.07, 2.04) | 0.017 | 1.39 (1.00, 1.92) | 0.051 | 1.41 (1.01, 1.96) | 0.045 |
| Model 0 | Model 1 | Model 2 | Model 3 | |||||
|---|---|---|---|---|---|---|---|---|
| Adjusted for | - | Age, Sex | Metabolic Risk | Liver Profiles | ||||
| HR (95% CI) | p-Value | HR (95% CI) | p-Value | HR (95% CI) | p-Value | HR (95% CI) | p-Value | |
| Last active H. pylori infection (H. pylori infection at baseline index) | ||||||||
| H. pylori (−) | Reference | Reference | Reference | Reference | ||||
| H. pylori (+) | 1.34 (1.03, 1.74) | 0.029 | 1.32 (1.02, 1.73) | 0.038 | 1.27 (0.97, 1.66) | 0.086 | 1.24 (0.94, 1.63) | 0.122 |
| Persistently active H. pylori infection | ||||||||
| Others | Reference | Reference | Reference | Reference | ||||
| Persistent | 1.35 (1.05, 1.73) | 0.019 | 1.38 (1.07, 1.78) | 0.014 | 1.31 (1.01, 1.69) | 0.043 | 1.33 (1.02, 1.73) | 0.033 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, J.Y.; Kwan, B.S.; Cho, J.H.; Kim, H.I.; Ko, N.G.; Jin, M.; Lee, O.J. Persistently Active Helicobacter pylori Infection Is Associated with the Development of Metabolic Dysfunction-Associated Steatotic Liver Disease. J. Clin. Med. 2025, 14, 1073. https://doi.org/10.3390/jcm14041073
Kim JY, Kwan BS, Cho JH, Kim HI, Ko NG, Jin M, Lee OJ. Persistently Active Helicobacter pylori Infection Is Associated with the Development of Metabolic Dysfunction-Associated Steatotic Liver Disease. Journal of Clinical Medicine. 2025; 14(4):1073. https://doi.org/10.3390/jcm14041073
Chicago/Turabian StyleKim, Jun Young, Byung Soo Kwan, Jung Hwan Cho, Hye In Kim, Nak Gyeong Ko, Mihyeon Jin, and Ok Jae Lee. 2025. "Persistently Active Helicobacter pylori Infection Is Associated with the Development of Metabolic Dysfunction-Associated Steatotic Liver Disease" Journal of Clinical Medicine 14, no. 4: 1073. https://doi.org/10.3390/jcm14041073
APA StyleKim, J. Y., Kwan, B. S., Cho, J. H., Kim, H. I., Ko, N. G., Jin, M., & Lee, O. J. (2025). Persistently Active Helicobacter pylori Infection Is Associated with the Development of Metabolic Dysfunction-Associated Steatotic Liver Disease. Journal of Clinical Medicine, 14(4), 1073. https://doi.org/10.3390/jcm14041073






