Monitoring Hip Joint Muscle Function in Osteoarthritis Patients Following Arthroplasty: A Prospective Cohort Study
Abstract
1. Introduction
2. Materials and Methods
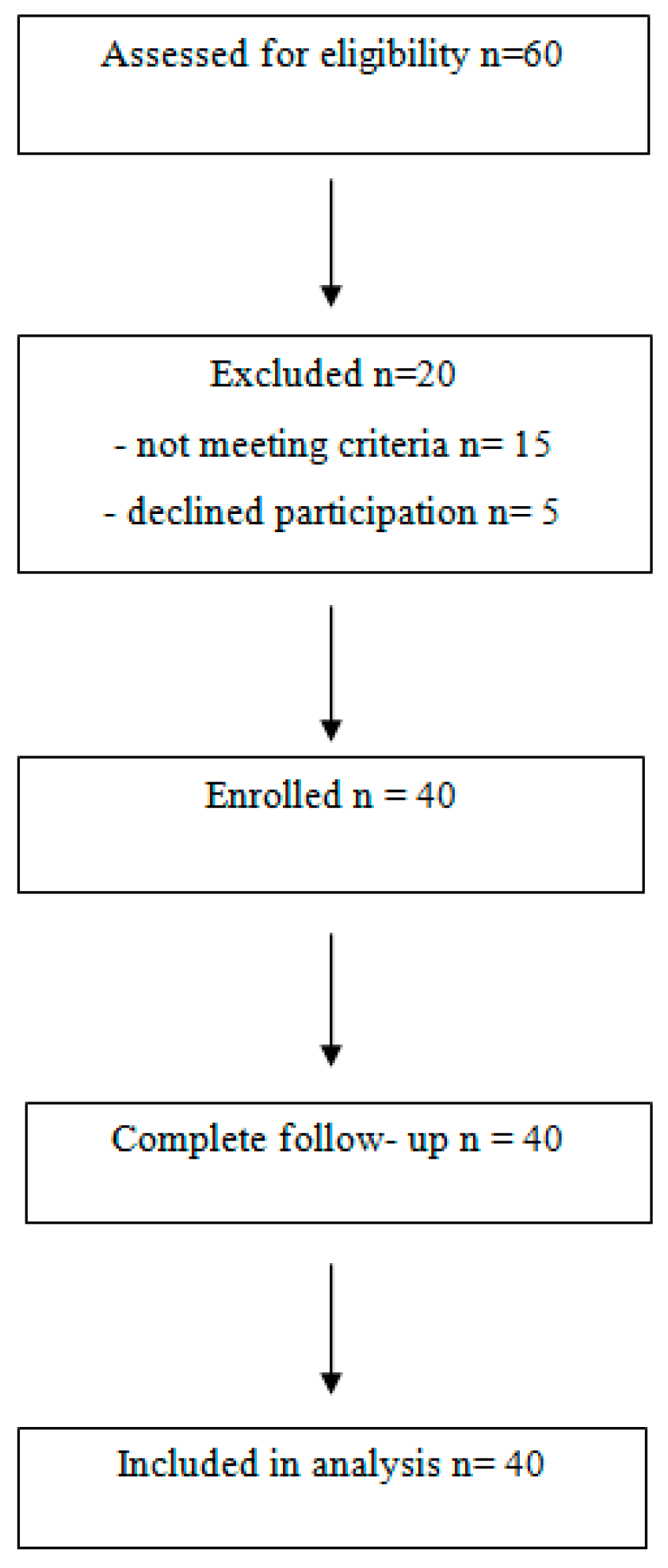
2.1. Study Design
2.2. Study Population
2.3. Patients’ Evaluation
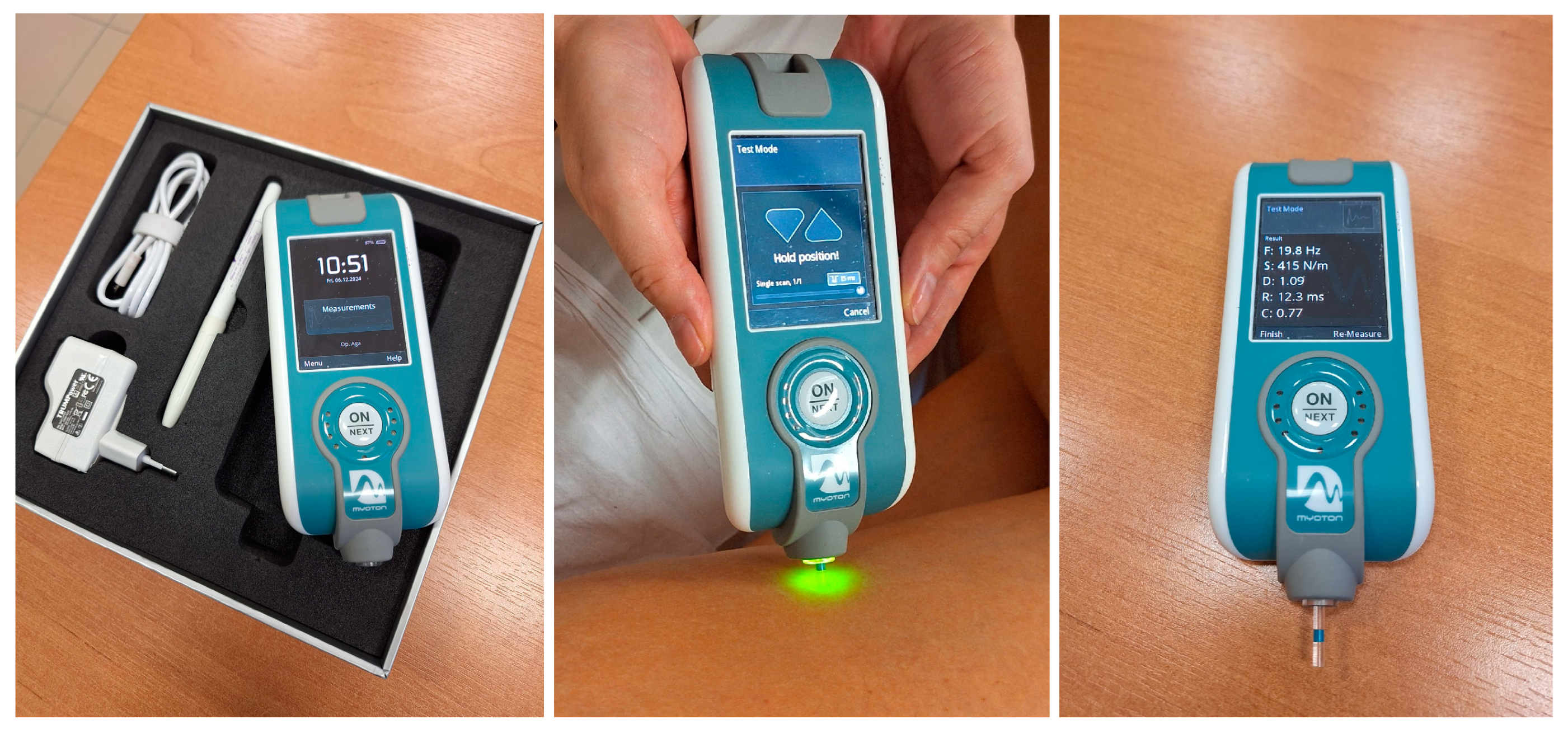
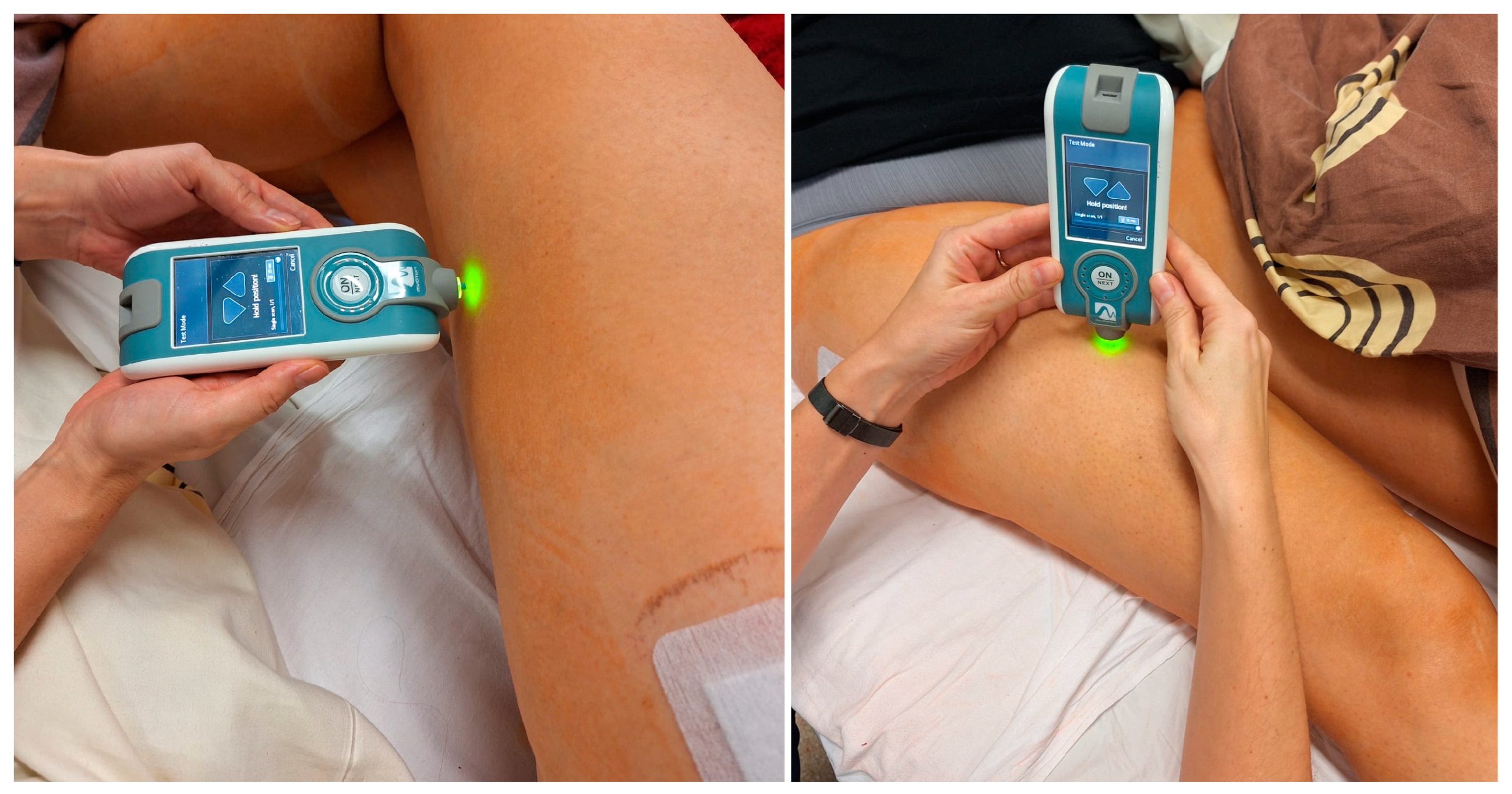
2.4. MyotonPro Measurements
2.5. Statistical Analysis
3. Results
3.1. Characteristics of the Research Group
3.2. Myoton Measurements
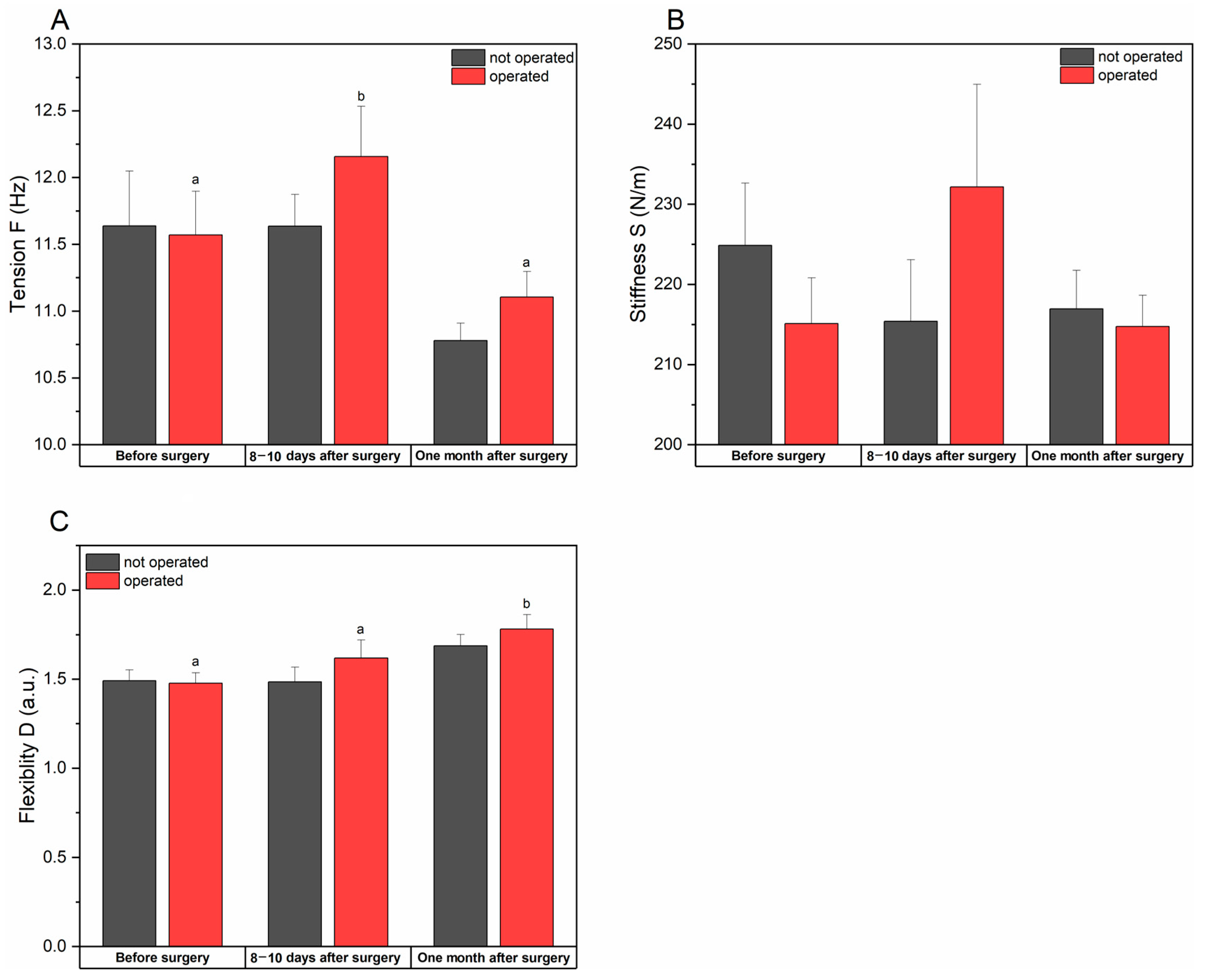
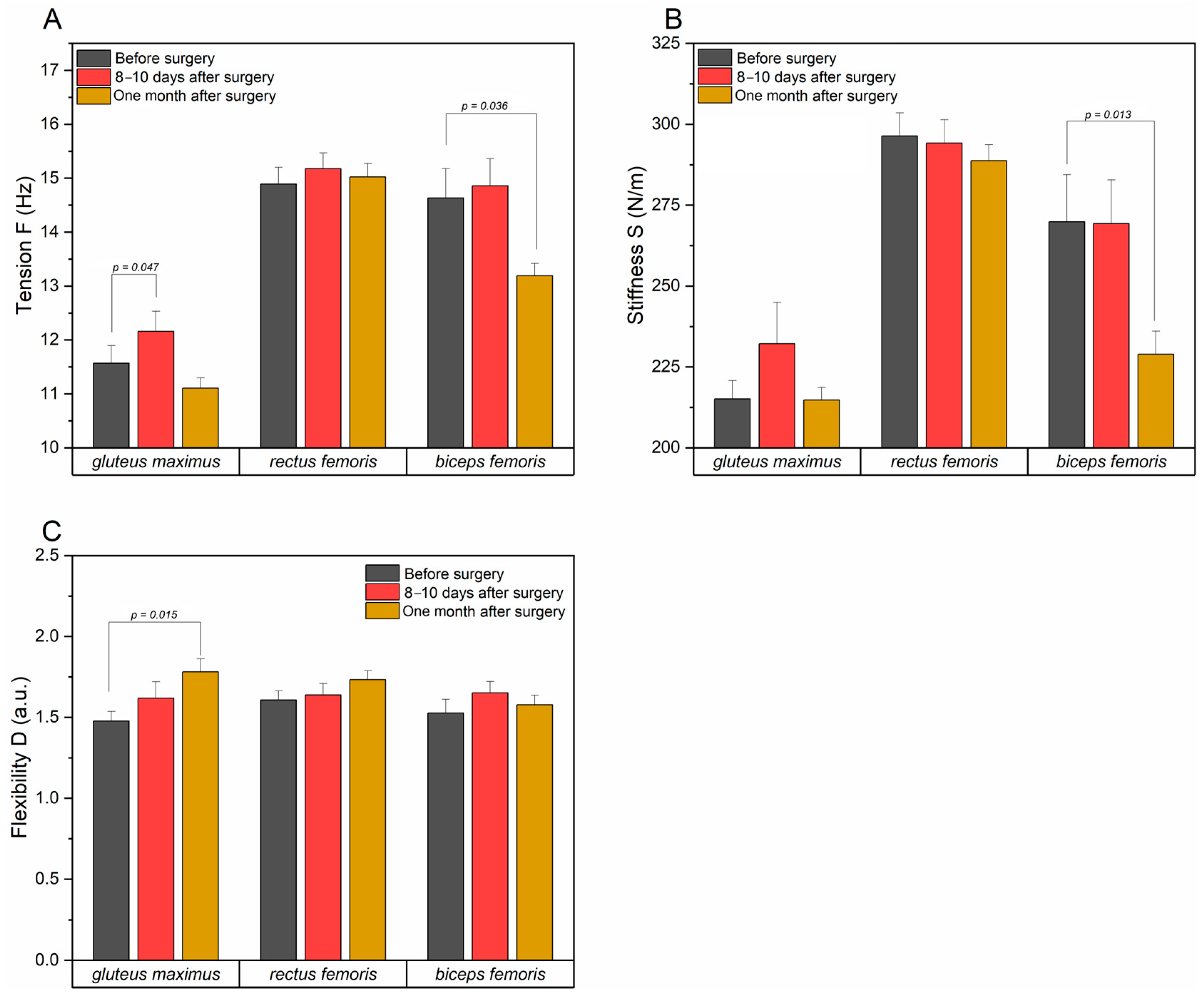
3.2.1. Tension, Stiffness, and Flexibility of the Gluteus Maximus Muscle
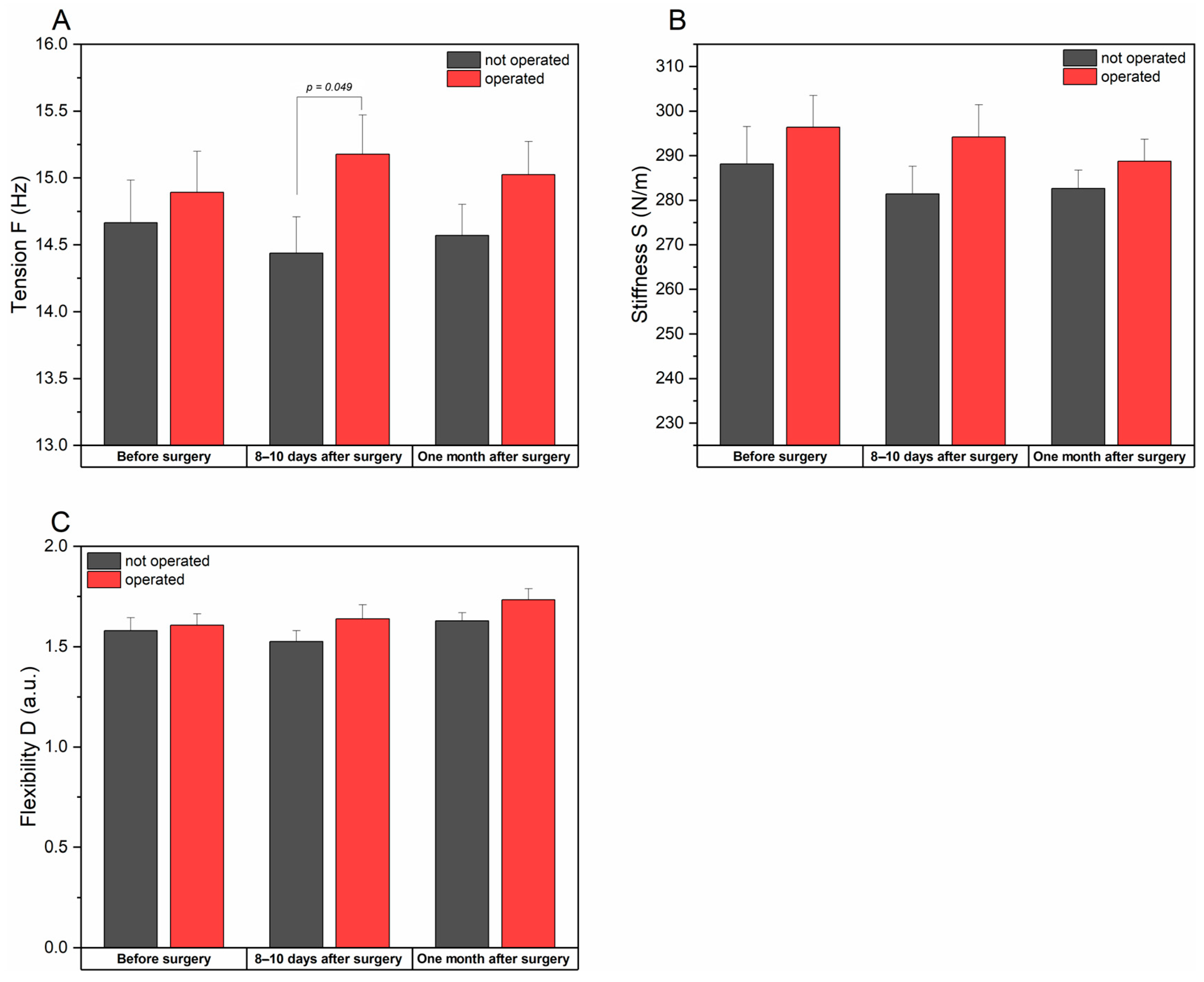
3.2.2. Tension, Stiffness, and Flexibility of the Rectus Femoris Muscle
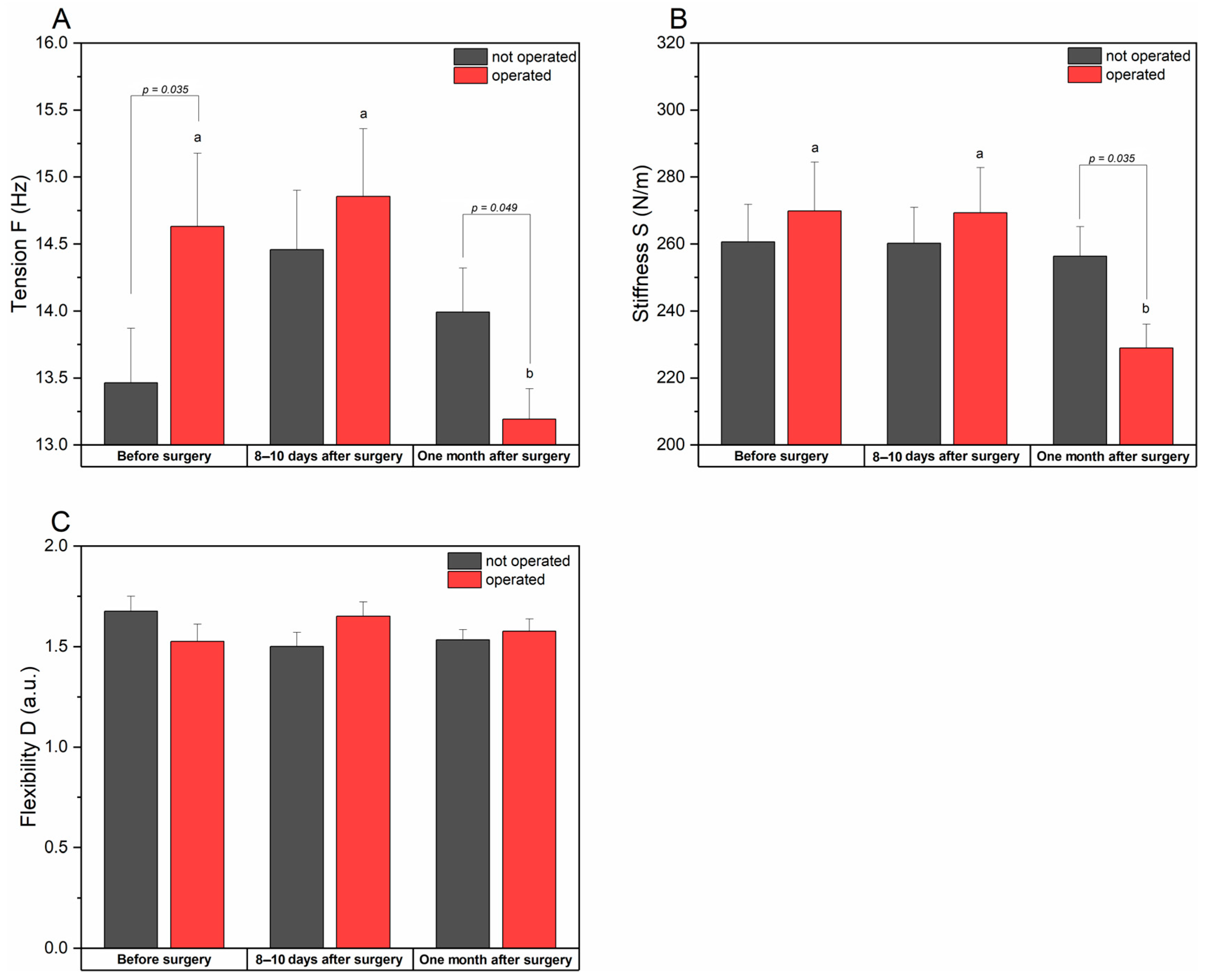
3.2.3. Tension, Stiffness, and Flexibility of the Biceps Femoris Muscle
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- O’Neill, T.W.; McCabe, P.S.; McBeth, J. Update on the epidemiology, risk factors and disease outcomes of osteoarthritis. Best Pract. Res. Clin. Rheumatol. 2018, 32, 312–326. [Google Scholar] [CrossRef] [PubMed]
- Bliddal, H. Definition, pathology and pathogenesis of osteoarthritis. Ugeskr. Laeger 2020, 182, V06200477. [Google Scholar]
- Sandiford, N.; Kendoff, D.; Muirhead-Allwood, S. Osteoarthritis of the hip: Aetiology, pathophysiology and current aspects of management. Ann. Joint 2020, 5, 8. [Google Scholar] [CrossRef]
- Katz, J.N.; Arant, K.R.; Loeser, R.F. Diagnosis and treatment of hip and knee osteoarthritis: A review. JAMA 2021, 325, 568–578. [Google Scholar] [CrossRef] [PubMed]
- Hawker, G.A. Osteoarthritis is a serois disease. Clin. Exp. Rheumatol. 2019, 37, 3–6. [Google Scholar] [PubMed]
- Allen, K.D.; Thoma, L.M.; Golightly, Y.M. Epidemiology of osteoarthritis. Osteoarthr. Cartil. 2022, 30, 184–195. [Google Scholar] [CrossRef] [PubMed]
- Zijuan, F.; Yan, L.; Liu, H.; Li, X.; Fan, K.; Liu, Q.; Li, J.-J.; Wang, B. The prevalence of hip osteoarthritis: A systematic review and meta-analysis. Arthrits Res. Ther. 2023, 25, 51. [Google Scholar]
- Jang, S.; Lee, K.; Ju, J.H. Recent Updates of Diagnosis, Pathophysiology, and Treatment on Osteoarthritis of the Knee. Int. J. Mol. Sci. 2021, 22, 2619. [Google Scholar] [CrossRef] [PubMed]
- Coaccioli, S.; Sarzi-Puttini, P.; Zis, P.; Rinonapoli, G.; Varrassi, G. Osteoarthritis: New Insight on Its Pathophysiology. J. Clin. Med. 2022, 11, 6013. [Google Scholar] [CrossRef]
- Shen, X.; Wang, S.; Chen, J.; Li, J.; Li, C.; Xiang, R.; Zhao, C.; Xu, X. Inter-rater reliability and test-retest reliability of the foot posture index (FPI-6) for assessing static foot posture in elderly female patients with knee osteoarthritis and its association with quadriceps muscle tone and stiffness. Front. Bioeng. Biotechnol. 2024, 12, 1385986. [Google Scholar] [CrossRef]
- Dias, T.T.; Shruthi, R.; Prabhakar, A.J.; Dineshbhai, P.V.; Eapen, C. Hip abductor strengthening in patients diagnosed with knee osteoarthritis- a systematic review and meta-analysis. BMC Musculoskeleta Disord. 2022, 23, 622. [Google Scholar]
- Rostron, Z.P.J.; Green, R.A.; Kingsley, M.; Zacharias, A. Efficacy of Exercise-Based Rehabilitation Programs for Improving Muscle Function and Size in People with Hip Osteoarthritis: A Systematic Review with Meta-Analysis. Biology 2021, 10, 1251. [Google Scholar] [CrossRef] [PubMed]
- Papalia, R.; Campi, S.; Vorini, F.; Zampogna, B.; Vasta, S.; Papalia, G.; Fossati Ch Torre, G.; Denaro, V. The Role of Physical Activity and Rehabilitation Following Hip and Knee Arthroplasty in the Elderly. J. Clin. Med. 2020, 9, 1401. [Google Scholar] [CrossRef] [PubMed]
- Lettner, J.; Królikowska, A.; Ramadanov, N.; Oleksy, Ł.; Hakam, H.T.; Becker, R.; Prill, R. Evaluating the Reliability of MyotonPro in Assessing Muscle Properties: A Systematic Review of Diagnostic Test Accuracy. Medicina 2024, 60, 851. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.-P.; Liu, C.-L.; Zhang, Z.-J. Feasibility of Using a Portable MyotonPRO Device to Quantify the Elastc Propoerties of Skeletal Muscle. Med. Sci. Monit. 2022, 28, e934121. [Google Scholar]
- Bravo-Sánchez, A.; Abián, P.; Sánchez-Infante, J.; Esteban-Gacía, P.; Jiménez, F.; Abián Vicén, J. Objective Assessment of Regional Stiffness in Vastus Lateralis with Different Measurement Methods: A Reliability Study. Sensors 2021, 21, 3213. [Google Scholar] [CrossRef]
- Ismailidis, P.; Kvarda, P.; Vach, W.; Cadosch, D.; Appnzeller-Horzog Ch Mundermann, A. Abductor Muscle Strength Deficit in Patients After Total Hip Arthroplasty: A Sytematci Review and Meta-Analysis. J. Arthroplast. 2021, 36, 3015–3027. [Google Scholar] [CrossRef]
- Lee, Y.; Kim, M.; Lee, H. The Measurement of Stiffness for Major Muscles with Shear Wave Elastography and Myoton: A Quantitative Analysis Study. Diagnostics 2021, 11, 524. [Google Scholar] [CrossRef]
- Li, Y.; Feng, Y.; Liu, C.; Zhang, Z. Paraffin therapy induces a decrease in the passive stiffness of gastrocnemius muscle belly and Achilles tendon: A randomized controlled trial. Medicine 2020, 99, e19519. [Google Scholar] [CrossRef]
- Chang, T.-T.; Zhu, Y.-C.; Li, Z.; Li, F.; Li, Y.-P.; Guo, J.-Y.; Wang, X.-Q.; Zhang, Z.-J. Modulation in the Stiffness of Specific Muscles of Quadriceps in Patients with Knee Osteoarthritis and Their Relationship with Functional Ability. Front. Bioeng. Biotechnol. 2022, 9, 781672. [Google Scholar] [CrossRef]
- Li, J.; Wu, Z.; Lu, B.; Li, C.; Wang, S.; Zhang, J.; Shen, X.; Xiang, R.; Chen, J.; Jiang, T.; et al. The Differences in Parameters in Ultrasound Imaging and Biomechanical Properties of the Quadriceps Femoris with Unilateral Knee Osteoarthritis in the Elderly: A Preliminary Observational Study. Clin. Interv. Aging 2024, 19, 1479–1491. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Pozas, O.; Sanchez-Romero, E.A.; Beltran-Alacreu, H.; Arribas-Romero, A.; Cuenca-Martinez, F.; Villafane, J.H.; Fernandez-Carnero, J. Effects of Orthopedic Manual Therapy on Pain Sensitization in Patients With Chronic Musculosceletal Pain: An Umbrela Review with Meta-Meta-analysis. Am. J. Phys. Med. Rehabil. 2023, 102, 879–885. [Google Scholar]
| Variable | Research Group (n = 40) | |
|---|---|---|
| Age [years] | M | 63.35 ± 2.55 |
| F | 66.18 ± 1.84 | |
| Height [cm] | M | 175.43 ± 1.21 a |
| F | 162.88 ± 1.22 b | |
| Weight [kg] | M | 93.04 ± 3.05 a |
| F | 74.47 ± 2.18 b | |
| BMI | M | 29.23 ± 0.90 |
| F | 28.48 ± 1.01 | |
| Marital status | single | - |
| married | 80% (32) | |
| widower | 15% (6) | |
| divorced | 5% (2) | |
| Education | primary | 2.5% (1) |
| basic vocational | 7.5% (3) | |
| secondary | 47.5% (19) | |
| higher | 42.5% (17) | |
| Place of residence | village | 12.5% (5) |
| town | 32.5% (13) | |
| city | 55% (22) | |
| Time since diagnosis [years] | 0–1 | 17.5% (7) |
| 2–5 | 60% (24) | |
| 6–10 | 22.5% (9) | |
| over 10 | - | |
| Duration of pain [years] | 0–1 | 7.5% (3) |
| 2–5 | 57.5% (23) | |
| 6–10 | 32.5% (13) | |
| 12 | - | |
| over 15 | 2.5% (1) | |
| Scale | Before Surgery | 8–10 Days After Surgery | One Month After Surgery | Statistics | |
|---|---|---|---|---|---|
| VAS | 6.38 a (±0.28) | 4.78 b (±0.30) | 1.88 c (±0.22) | χ2 = 63.373 W = 0.792 p < 0.001 | |
| WOMAC scale | 49.84 a (±2.25) | 46.90 a (±1.64) | 23.39 b (±1.49) | χ2 = 62.18 W = 0.778 p < 0.001 | |
| Tinetti scale | balance | 10.38 a (±0.34) | 7.55 b (±0.30) | 10.90 a (±0.33) | χ2 = 34.06 W = 0.426 p < 0.001 |
| gait | 8.80 a (±0.37) | 7.78 b (±0.29) | 9.90 a (±0.20) | χ2 = 34.57 W = 0.432 p < 0.001 | |
| balance level | 18.73 a (±0.74) | 15.33 b (±0.47) | 20.80 a (±0.43) | χ2 = 31.56 W = 0.395 p < 0.001 | |
| Before Surgery | 8–10 Days After Surgery | One Month After Surgery | p-Valuetime (ES) | ||||
|---|---|---|---|---|---|---|---|
| Not Operated Limb | Operated Limb | Not Operated Limb | Operated Limb | Not Operated Limb | Operated Limb | ||
| Tension F (Hz) | 11.63 ±0.41 | 11.57 a ±0.32 | 11.63 ±0.23 | 12.15 b ±0.38 | 10.78 ±0.13 | 11.10 a ±0.19 | p = 0.086 (0.061) |
| p = 0.009 (0.118) | |||||||
| p-valueside | p = 0.969 (<0.001) | p = 0.363 (0.021) | p = 0.179 (0.046) | ||||
| Stiffness S (N/m) | 224.9 ±7.8 | 215.1 ±5.7 | 215.4 ±7.7 | 232.2 ±12.8 | 216.9 ±4.8 | 214.7 ±3.9 | p = 0.368 (0.025) |
| p = 0.397 (0.023) | |||||||
| p-valueside | p = 0.355 (0.021) | p = 0.088 (0.067) | p = 0.737 (0.002) | ||||
| Flexibility D (a.u.) | 1.49 ±0.06 | 1.48 a ±0.06 | 1.62 ±0.08 | 1.61 a ±0.10 | 1.68 ±0.06 | 1.78 b ±0.08 | p = 0.052 (0.079) |
| p = 0.014 (0.131) | |||||||
| p-valueside (ES) | p = 0.988 (<0.001) | p = 0.488 (0.012) | p = 0.529 (0.010) | ||||
| Before Surgery | 8–10 Days After Surgery | One Month After Surgery | p-Valuetime (ES) | ||||
|---|---|---|---|---|---|---|---|
| Not Operated Limb | Operated Limb | Not Operated Limb | Operated Limb | Not Operated Limb | Operated Limb | ||
| Tension F (Hz) | 14.67 ±0.32 | 14.89 ±0.31 | 14.44 ±0.27 | 15.18 ±0.29 | 14.57 ±0.23 | 15.05 ±0.25 | p = 0.944 (0.001) |
| p = 0.733 (0.008) | |||||||
| p-valueside (ES) | p = 0.534 (0.009) | p = 0.049 (0.095) | p = 0.161 (0.049) | ||||
| Stiffness S (N/m) | 288.2 ±8.4 | 296.4 ±7.1 | 281.40 ±6.2 | 294.2 ±7.2 | 282.6 ±4.1 | 288.7 ±4.9 | p = 0.498 (0.018) |
| p = 0.905 (0.003) | |||||||
| p-valueside (ES) | p = 0.747 (0.003) | p = 0.173 (0.046) | p = 0.292 (0.028) | ||||
| Flexibility D (a.u.) | 1.58 ±0.06 | 1.61 ±0.06 | 1.52 ±0.05 | 1.64 ±0.07 | 1.63 ±0.04 | 1.73 ±0.06 | p = 0.265 (0.033) |
| p = 0.103 (0.057) | |||||||
| p-valueside (ES) | p = 0.689 (0.004) | p = 0.246 (0.065) | p = 0.225 (0.037) | ||||
| Before Surgery | 8–10 Days After Surgery | Month After Surgery | p-Valuetime (ES) | ||||
|---|---|---|---|---|---|---|---|
| Not Operated Limb | Operated Limb | Not Operated Limb | Operated Limb | Not Operated Limb | Operated Limb | ||
| Tension F (Hz) | 13.46 ±0.41 | 14.63 a ±0.55 | 14.46 ±0.44 | 14.86 a ±0.55 | 13.99 ±0.33 | 13.19 b ±0.28 | p = 0.248 (0.032) |
| p = 0.015 (0.155) | |||||||
| p-valueside | p = 0.035 (0.099) | p = 0.477 (0.013) | p = 0.049 (0.084) | ||||
| Stiffness S (N/m) | 260.6 ±11.2 | 269.8 a ±14.6 | 260.3 ±10.7 | 269.3 a ±13.5 | 256.4 ±8.8 | 228.9 b ±7.2 | p = 0.756 (0.008) |
| p = 0.001 (0.182) | |||||||
| p-valueside | p = 0.749 (0.003) | p = 0.572 (0.007) | p = 0.035 (0.109) | ||||
| Flexibility D (a.u.) | 1.68 ±0.07 | 1.53 ±0.09 | 1.50 ±0.07 | 1.65 ±0.07 | 1.53 ±0.05 | 1.58 ±0.06 | p = 0.182 (0.038) |
| p = 0.251 (0.037) | |||||||
| p-valueside | p = 0.207 (0.040) | p = 0.132 (0.056) | p = 0.724 (0.003) | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Staniak, D.; Wójcik-Załuska, A.; Sokołowski, K.; Drelich, M.; Świetlicka, I.; Prendecka-Wróbel, M.; Małecka-Massalska, T. Monitoring Hip Joint Muscle Function in Osteoarthritis Patients Following Arthroplasty: A Prospective Cohort Study. J. Clin. Med. 2025, 14, 976. https://doi.org/10.3390/jcm14030976
Staniak D, Wójcik-Załuska A, Sokołowski K, Drelich M, Świetlicka I, Prendecka-Wróbel M, Małecka-Massalska T. Monitoring Hip Joint Muscle Function in Osteoarthritis Patients Following Arthroplasty: A Prospective Cohort Study. Journal of Clinical Medicine. 2025; 14(3):976. https://doi.org/10.3390/jcm14030976
Chicago/Turabian StyleStaniak, Dorota, Alicja Wójcik-Załuska, Krzysztof Sokołowski, Małgorzata Drelich, Izabela Świetlicka, Monika Prendecka-Wróbel, and Teresa Małecka-Massalska. 2025. "Monitoring Hip Joint Muscle Function in Osteoarthritis Patients Following Arthroplasty: A Prospective Cohort Study" Journal of Clinical Medicine 14, no. 3: 976. https://doi.org/10.3390/jcm14030976
APA StyleStaniak, D., Wójcik-Załuska, A., Sokołowski, K., Drelich, M., Świetlicka, I., Prendecka-Wróbel, M., & Małecka-Massalska, T. (2025). Monitoring Hip Joint Muscle Function in Osteoarthritis Patients Following Arthroplasty: A Prospective Cohort Study. Journal of Clinical Medicine, 14(3), 976. https://doi.org/10.3390/jcm14030976






