Colistin Use for the Treatment of Multi-Drug-Resistant Gram-Negative Severe Infections in ICU Patients: A Single-Center Study
Abstract
1. Introduction
2. Methods
2.1. Study Population
2.2. Data Collection
2.3. Infection Diagnosis
2.4. Study Outcomes
2.5. Statistical Assessment
3. Results
3.1. Study Population
3.2. Colistin Therapy
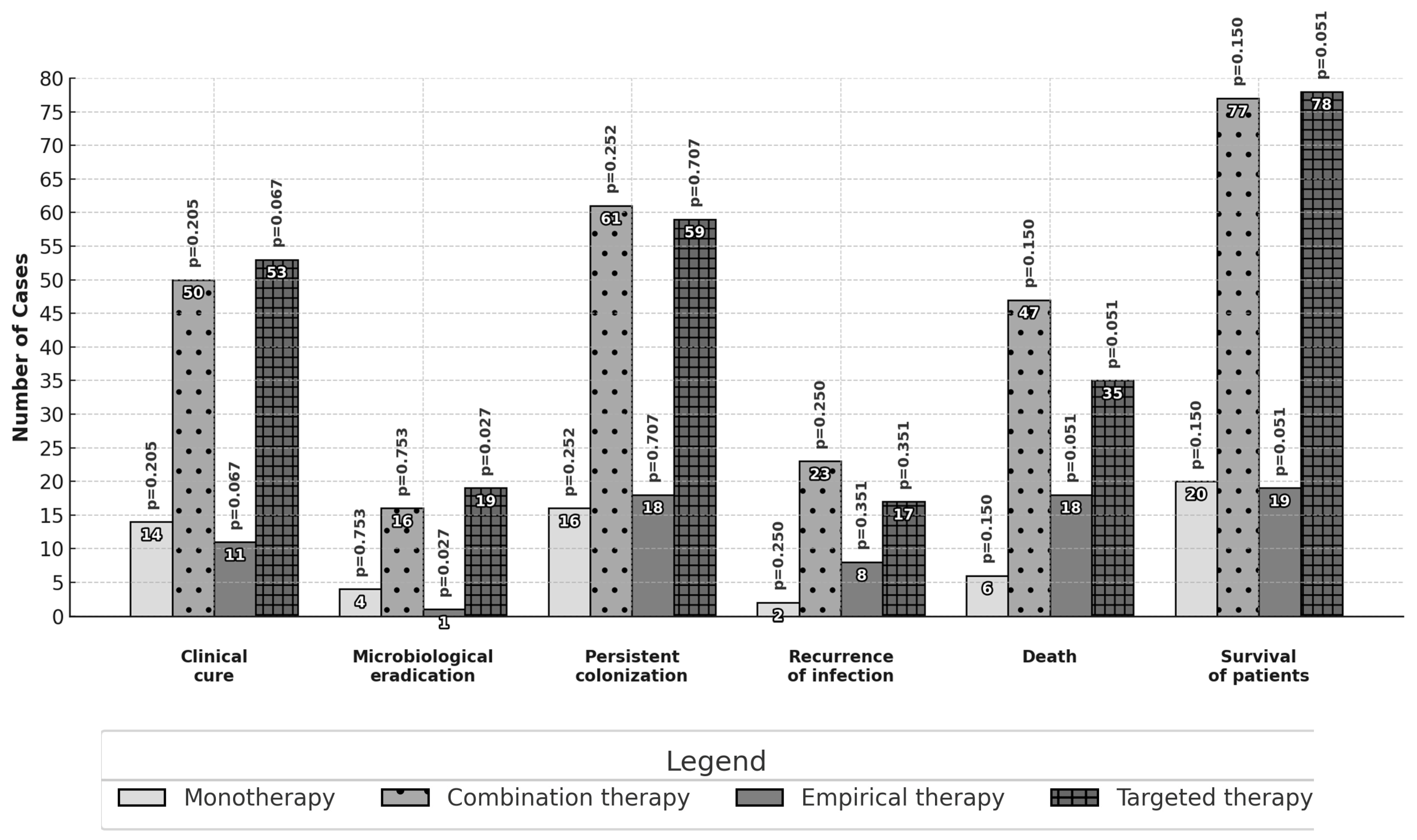
3.3. Primary and Secondary Outcomes
3.4. Subgroup Analyses
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Weiner, L.M.; Webb, A.K.; Limbago, B.; Dudeck, M.A.; Patel, J.; Kallen, A.J.; Edwards, J.R.; Sievert, D.M. Antimicrobial-Resistant Pathogens Associated with Healthcare-Associated Infections: Summary of Data Reported to the National Healthcare Safety Network at the Centers for Disease Control and Prevention, 2011–2014. Infect. Control Hosp. Epidemiol. 2016, 37, 1288–1301. [Google Scholar] [CrossRef] [PubMed]
- Duszyńska, W.; Litwin, A.; Rojek, S.; Szczęsny, A.; Ciasullo, A.; Goździk, W. Analysis of Acinetobacter baumannii hospital infections in patients treated at the intensive care unit of the University Hospital, Wroclaw, Poland: A 6-year, single-center, retrospective study. Infect. Drug Resist. 2018, 11, 629–635. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Nation, R.L.; Kaye, K.S. Polymyxin Antibiotics: From Laboratory Bench to Bedside; Springer Nature Switzerland AG: Cham, Switzerland, 2019. [Google Scholar]
- Rychlícková, J.; Kubícková, V.; Suk, P.; Urbánek, K. Challenges of Colistin Use in ICU and Therapeutic Drug Monitoring: A Literature Review. Antibiotics 2023, 12, 437. [Google Scholar] [CrossRef] [PubMed]
- Simsek, F.; Gedik, H.; Yildirmak, M.T.; Iris, N.E. A Colistin against colistin-only-susceptable Acinetobacter baumanii-related infections: Monotherapy or combination therapy. Indian J. Med. Microbiol. 2012, 30, 448–452. [Google Scholar] [CrossRef]
- Vardakas, K.Z.; Mavroudis, A.D.; Georgiou, M.; Falagas, M.E. Intravenous colistin combination antimicrobial treatment vs. monotherapy: A systematic review and meta-analysis. Int. J. Antimicrob. Agents 2018, 4, 535–547. [Google Scholar] [CrossRef]
- Kalil, A.C.; Metersky, M.L.; Klompas, M.; Muscedere, J.; Sweeney, D.A.; Palmer, L.B.; Napolitano, L.M.; O’Grady, N.P.; Bartlett, J.G.; Carratalà, J.; et al. Management of adults with health-acquired and ventilator-associated pneumonia: Clinical practice guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin. Infect. Dis. 2016, 63, e61–e111. [Google Scholar] [CrossRef]
- Rhodes, A.; Evans, L.E.; Alhazzani, W.; Levy, M.M.; Antonelli, M.; Ferrer, R.; Kumar, A.; Sevransky, J.E.; Sprung, C.L.; Nunnally, M.E.; et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Intensive Care Med. 2017, 43, 304–377. [Google Scholar] [CrossRef]
- Alshaya, A.I.; Bin Saleh, K.; Aldhaeefi, M.; A Baderldin, H.; Alamoudi, F.; A Alhamdan, Q.; Almusallam, M.; Alshaya, O.; Al Sulaiman, K.; Alshareef, S.; et al. Colistin Loading Dose in Septic Patients with Gram Negative Infections. Infect. Drug Resist. 2022, 15, 2159–2166. [Google Scholar] [CrossRef]
- Knaus, W.A.; Draper, E.A.; Wagner, D.P.; Zimmerman, J.E. APACHE II: A severity of disease classification system. Crit. Care Med. 1985, 13, 818–829. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control. Point Prevalence Survey of Healthcare-Associated Infections and Antimicrobial Use in European Acute Care Hospitals; ECDC: Stockholm, Sweden, 2013; Available online: https://www.ecdc.europa.eu/sites/default/files/media/en/publications/Publications/healthcare-associated-infections-antimicrobial-use-PPS.pdf (accessed on 13 June 2020).
- Menichetti, F.; Sganga, G. Definition and Classification of Intra-abdominal Infections. J. Chemother. 2013, 21 (Suppl. S1), 3–4. [Google Scholar] [CrossRef]
- The European Committee on Antimicrobial Susceptibility Testing. Breakpoint Tables for Interpretation of MICs and Zone Diameters. Version 6.0. 2016. Available online: https://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/Breakpoint_tables/v_6.0_Breakpoint_table.pdf (accessed on 1 January 2020).
- Litwin, A.; Rojek, S.; Gozdzik, W.; Duszynska, W. Pseudomonas aeruginosa device associated—Healthcare associated infections and its multidrug resistance at intensive care unit of University Hospital: Polish, 8.5-year, prospective, single-centre study. BMC Infect. Dis. 2021, 21, 180. [Google Scholar] [CrossRef] [PubMed]
- Magiorakos, A.-P.; Srinivasan, A.; Carey, R.B.; Carmeli, Y.; Falagas, M.E.; Giske, C.G.; Harbarth, S.; Hindler, J.F.; Kahlmeter, G.; Olsson-Liljequist, B.; et al. Multidrug-resistant, extensively drug-resistant and pandrug–resistant bacteria: An international expert proposal for interim standard definitions for acquired resistance. Clin. Microbiol. Infect. 2012, 18, 268–281. [Google Scholar] [CrossRef] [PubMed]
- Kellum, J.A.; Lameire, N.; Aspelin, P.; Barsoum, R.S.; Burdmann, E.A.; Goldstein, S.L.; Herzog, C.A.; Joannidis, M.; Kribben, A.; Levey, A.S.; et al. Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group. KDIGO Clinical Practice Guideline for Acute Kidney Injury. Kidney Int. Suppl. 2012, 2, 1–138. [Google Scholar]
- Cockcroft, D.W.; Gault, M.H. Prediction of creatinine clearance from serum creatinine. Nephron 1976, 16, 31–41. [Google Scholar] [CrossRef]
- Giacobbe, D.R.; Saffioti, C.; Losito, A.R.; Rinaldi, M.; Aurilio, C.; Bolla, C.; Boni, S.; Borgia, G.; Carannante, N.; Cassola, G.; et al. Use of colistin in adult patients: A cross-sectional study. J. Glob. Antimicrob. Resist. 2020, 20, 43–49. [Google Scholar] [CrossRef]
- Kofteridis, D.P.; Alexopoulou, C.; Valachis, A.; Maraki, S.; Dimopoulou, D.; Georgopoulos, D.; Samonis, G. Aerosolized plus intravenous colistin versus intravenous colistin alone for the treatment of ventilator-associated pneumonia: A matched case-control study. Clin. Infect. Dis. 2010, 51, 1238–1244. [Google Scholar] [CrossRef]
- Markou, N.; Markantonis, S.L.; Dimitrakis, E.; Panidis, D.; Boutzouka, E.; Karatzas, S.; Rafailidis, P.; Apostolakos, H.; Baltopoulos, G. Colistin serum concentrations after intravenous administration in critically patients with serious multidrug-resistant gram-negative bacilli infections: A prospective, open-label, uncontrolled study. Clin. Ther. 2008, 30, 143–151. [Google Scholar] [CrossRef]
- Dalfino, L.; Puntillo, F.; Mosca, A.; Monno, R.; Spada, M.L.; Coppolecchia, S.; Miragliotta, G.; Bruno, F.; Brienza, N. High-dose, extended-interval colistin administration in critically ill patients: Is this the right dosing strategy? A preliminary study. Clin. Infect. Dis. 2012, 54, 1720–1726. [Google Scholar] [CrossRef]
- Cisneros, J.M.; Rosso-Fernández, C.M.; Roca-Oporto, C.; De Pascale, G.; Jiménez-Jorge, S.; Fernández-Hinojosa, E.; Matthaiou, D.K.; Ramírez, P.; Díaz-Miguel, R.O.; Estella, A.; et al. Colistin versus meropenem in the empirical treatment of ventilator-associated pneumonia (Magic Bullet study): An investigator-driven, open-label, randomized, noninferiority controlled trial. Crit. Care 2019, 23, 383. [Google Scholar] [CrossRef]
- Zak-Doron, Y.; Dishon Benattar, Y.; Pfeffer, I.; Daikos, G.L.; Skiada, A.; Antoniadou, A.; Durante-Mangoni, E.; Andini, R.; Cavezza, G.; Leibovici, L.; et al. The Association Between Empirical Antibiotic Treatment and Mortality in Severe Infections Caused by Carbapenem-resistant Gram-negative Bacteria: A Prospective Study. Clin. Infect. Dis. 2018, 67, 1815–1823. [Google Scholar] [CrossRef]
- Falagas, M.E.; Rafailidis, P.I.; Kasiakou, S.K.; Hatzopoulou, P.; Michalopoulos, A. Effectiveness and nephrotoxicity of colistin monotherapy vs. colistin-meropenem combination therapy for multidrug-resistant gram-negative bacterial infections. Clin. Microbiol. Infect. 2006, 12, 1227–1230. [Google Scholar] [CrossRef] [PubMed]
- Qureshi, Z.A.; Paterson, D.L.; Potoski, B.A.; Kilayko, M.C.; Sandovsky, G.; Sordillo, E.; Polsky, B.; Adams-Haduch, J.M.; Doi, Y. Treatment outcome of bacteremia due to KPC-producing Klebsiella pneumoniae: Superiority of combination antimicrobial regimens. Antimicrob. Agents Chemother. 2012, 56, 2108–2113. [Google Scholar] [CrossRef] [PubMed]
- Batirel, A.; Balkan, I.I.; Karabay, O.; Agalar, C.; Akalin, S.; Alici, O.; Alp, E.; Altay, F.A.; Altin, N.; Arslan, F.; et al. Comparison of colistin-carbapenem, colistin-sulbactam, and colistin plus other antibacterial agents for the treatment of extremely drug-resistant Acinetobacter baumannii bloodstream infections. Eur. J. Clin. Microbiol. Infect. Dis. 2014, 33, 1311–1322. [Google Scholar] [CrossRef] [PubMed]
- Paul, M.; Daikos, G.L.; Durante-Mangoni, E.; Yahav, D.; Carmeli, Y.; Benattar, Y.D.; Skiada, A.; Andini, R.; Eliakim-Raz, N.; Nutman, A.; et al. Colistin alone versus colistin plus meropenem for treatment of severe infections caused by carbapenem-resistant Gram-negative bacteria: An open-label, randomised controlled trial. Lancet Infect. Dis. 2018, 18, 391–400. [Google Scholar] [CrossRef]
- Katip, W.; Meechoui, M.; Thawornwittayakom, P.; Chinwong, D.; Oberdorfer, P. Efficacy and Safety of High Loading Dose of Colistin in Multidrug-Resistant Acinetobacter baumannii: A Prospective Cohort Study. J. Intensive Care Med. 2019, 34, 996–1002. [Google Scholar] [CrossRef]
- Lu, Q.; Luo, R.; Bodin, L.; Yang, J.; Zahr, N.; Aubry, A.; Goldmard, J.L.; Rouby, J.J.; The Nebulized Antibiotics Study Group. Efficacy of high–dose nebulized Colistin in Ventilator-associated Pneumonia Caused by multidrug-resistant Pseudomonas aeruginosa and Acinetobacter baumannii. Anaesthesiology 2012, 117, 1335–1347. [Google Scholar] [CrossRef]
- Demirdal, T.; Sari, U.S.; Nemli, S.A. Is inhaled colistin beneficial in ventilator associated pneumonia or nosocomial pneumonia caused by Acinetobacter baumannii? Ann. Clin. Microbiol. Antimicrob. 2016, 15, 11. [Google Scholar] [CrossRef]
- Cui, H.M.; Lin, X.; Liu, Y.Y.; Shen, Y.H. Comparison of different colistin regimens for the treatment of pneumonia caused by multidrug-resistant microorganisms: A systematic review and meta-analysis. Eur. Rev. Med. Pharmacol. Sci. 2021, 25, 5275–5292. [Google Scholar]
- Franzone, J.P.; Mackow, N.A.; van Duin, D. Current treatment options for pneumonia caused by carbapenem-resistant Acinetobacter baumannii. Curr. Opin. Infect. Dis. 2024, 37, 137–143. [Google Scholar] [CrossRef]
- Zhang, X.; Cui, X.; Jiang, M.; Huang, S.; Yang, M. Nebulized colistin as the adjunctive treatment for ventilator-associated pneumonia: A systematic review and meta-analysis. J. Crit. Care 2023, 77, 154315. [Google Scholar] [CrossRef]
- Tamma, P.D.; Heil, E.L.; Justo, J.A.; Mathers, A.J.; Satlin, M.J.; Bonomo, R.A. Infectious Diseases Society of America 2024 Guidance on the Treatment of Antimicrobial-Resistant Gram-Negative Infections. Clin. Infect. Dis. 2024, ciae403. [Google Scholar] [CrossRef] [PubMed]
- Paul, M.; Carrara, E.; Retamar, P.; Tängdén, T.; Bitterman, R.; Bonomo, R.A.; De Waele, J.; Daikos, G.L.; Akova, M.; Harbarth, S.; et al. European Society of Clinical Microbiology and Infectious Diseases (ESCMID) guidelines for the treatment of infections caused by multidrug-resistant Gram-negative bacilli (endorsed by European society of intensive care medicine). Clin. Microbiol. Infect. 2022, 28, 521–547. [Google Scholar] [CrossRef] [PubMed]

| Therapy | Full Test n = 150 | Variables | |||
|---|---|---|---|---|---|
| Targeted n = 113 | Empirical n = 37 | Combination n = 124 | Monotherapy n = 26 | ||
| Sex, n (%) | |||||
| 31 (27.4) | 14 (37.8) | 37 (29.8) | 8 (30.8) | 45 (30.0) | Women |
| 82 (72.6) | 23 (62.2) | 87 (70.2) | 18 (69.2) | 105 (70.0) | Men |
| 59.1 (18.7) | 63.7 (16.1) | 60.3 (18.5) | 60.0 (16.3) | 60.3 (18.1) | Age, M (SD) |
| 18.0 (13.0–23.0) | 17.0 (13.5–23.0) | 17.5 (13.0–23.0) | 17.0 (13.5–23.0) | 17.0 (13.0–23.0) | APACHE II, Me (IQR) |
| 78 (69.0) | 19 (51.4) | 77 (62.1) | 20 (76.9) | 97 (64.7) | Survival, n (%) |
| 29.0 (17.0–41.0) | 24.0 (16.0–36.0) | 28.0 (17.0–41.0) | 28.0 (15.0–43.5) | 28.0 (17.0–40.5) | Time of ICU stay, Me (IQR) |
| 33.8 (29.6) | 25.5 (15.1) | 30.4 (17.5) | 38.3 (52.8) | 31.8 (27.0) | Time of ICU stay, M (SD) |
| 69 (61.1) | 23 (62.2) | 77 (62.1) | 15 (57.7) | 92 (61.3) | Medical patients, n (%) |
| 44 (38.9) | 14 (37.8) | 47 (37.9) | 11 (42.3) | 58 (38.7) | Surgical patients, n (%) |
| 32 (28.3) | 15 (40.5) | 42 (33.9) | 5 (19.2) | 47 (31.3) | Sepsis/Septic shock, n (%) |
| 112 (99.1) | 36 (97.3) | 124 (100.0) | 24 (92.3) | 148 (98.7) | Mechanical ventilation, n (%) |
| 70 (61.9) | 28 (75.7) | 85 (68.5) | 13 (50.0) | 98 (65.3) | Circulatory failure, need for the use of catecholamines, n (%) |
| 14 (12.4) | 3 (8.1) | 0 (0) | 17 (13.7) | 17 (11.3) | Other nephrotoxic agents, n (%) |
| 28 (24.8) | 8 (21.6) | 35 (28.2) | 1 (3.8) | 36 (24.0) | Aminoglycosides, n (%) |
| 62 (54.9) | 18 (48.6) | 73 (58.9) | 7 (26.9) | 80 (53.3) | Vancomycin, n (%) |
| 42 (37.2) | 21 (56.8) | 54 (43.5) | 9 (34.6) | 63 (42.0) | Diuretics, n (%) |
| n = 141 | n = 38 | n = 149 | n = 30 | n = 179 | The type of infection, n (%) |
| 45 (31.9) | 15 (39.5) | 51 (34.3) | 9 (30.0) | 60 (33.5) | HAP |
| 62 (44.0) | 18 (47.5) | 67 (45.0) | 13 (43.3) | 80 (44.7) | VAP |
| 6 (4.3) | 1 (2.6) | 7 (4.7) | 0 (0) | 7 (3.9) | CLA-BSI |
| 5 (3.5) | 1 (2.6) | 6 (4.0) | 0 (0) | 6 (3.4) | Peritonitis |
| 7 (5.0) | 1 (2.6) | 3 (2.0) | 5 (16.7) | 8 (4.5) | UTI or urosepsis |
| 2 (1.4) | 1 (2.6) | 3 (2.0) | 0 (0) | 3 (1.6) | OUN Infection |
| 14 (9.9) | 1 (2.6) | 12 (8.0) | 3 (10.0) | 15 (8.4) | Others |
| Pathogen detected, n (%) | |||||
| 112 (99.1) | 34 (91.9) | 120 (96.8) | 26 (100.0) | 146 (97.3) | Acinetobacter baumannii |
| 1 (0.9) | 3 (8.1) | 4 (3.2) | 0 (0) | 4 (2.7) | Pseudomonas aeruginosa |
| 37.1 (0.8) | 36.8 (0.6) | 37.0 (0.8) | 36.8 (0.7) | 37.0 (0.8) | Temperature C, M (SD) |
| 12.7 (8.2–19.1) | 15.1 (9.8–30.9) | 14.1 (9.5–21.9) | 11.0 (6.3–16.1) | 13.3 (8.9–20.4) | WBC 103/mm3, Me (IQR) |
| 1.3 (0.4–5.1) | 4.6 (0.7–23.1) | 1.9 (0.5–8.2) | 0.6 (0.1–5.1) | 1.6 (0.5–7.7) | PCT ng/mL, Me (IQR) |
| 161.4 (102.6–238.9) | 141.3 (109.0–266.9) | 174.0 (106.5–250.7) | 122.9 (59.6–211.8) | 161.4 (102.6–243.0) | CRP ng/mL, Me (IQR) |
| 0.8 (0.6–1.5) | 1.3 (0.8–2.2) | 1.0 (0.7–1.8) | 0.8 (0.6–1.1) | 0.9 (0.7–1.8) | Serum creatinine at the initiation of the treatment mg/dL, Me (IQR) |
| 85.5 (54.9–113.7) | 49.0 (28.0–140.9) | 78.5 (35.1–131.7) | 98.0 (68.7–133.4) | 81.0 (38.0–131.3) | Creatinine clearance at the initiation of the treatment, mL/min, Me (IQR) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rojek, S.W.; Wojtowicz, I.; Taccone, F.S.; Duszynska, W. Colistin Use for the Treatment of Multi-Drug-Resistant Gram-Negative Severe Infections in ICU Patients: A Single-Center Study. J. Clin. Med. 2025, 14, 797. https://doi.org/10.3390/jcm14030797
Rojek SW, Wojtowicz I, Taccone FS, Duszynska W. Colistin Use for the Treatment of Multi-Drug-Resistant Gram-Negative Severe Infections in ICU Patients: A Single-Center Study. Journal of Clinical Medicine. 2025; 14(3):797. https://doi.org/10.3390/jcm14030797
Chicago/Turabian StyleRojek, Stanislaw Wojciech, Iga Wojtowicz, Fabio Silvio Taccone, and Wieslawa Duszynska. 2025. "Colistin Use for the Treatment of Multi-Drug-Resistant Gram-Negative Severe Infections in ICU Patients: A Single-Center Study" Journal of Clinical Medicine 14, no. 3: 797. https://doi.org/10.3390/jcm14030797
APA StyleRojek, S. W., Wojtowicz, I., Taccone, F. S., & Duszynska, W. (2025). Colistin Use for the Treatment of Multi-Drug-Resistant Gram-Negative Severe Infections in ICU Patients: A Single-Center Study. Journal of Clinical Medicine, 14(3), 797. https://doi.org/10.3390/jcm14030797







