Physical and Psychological Burden of Bed Rest on Patients Following Free Flap Reconstruction of the Lower Limb: A Systematic Review and Possible Solutions
Abstract
1. Introduction
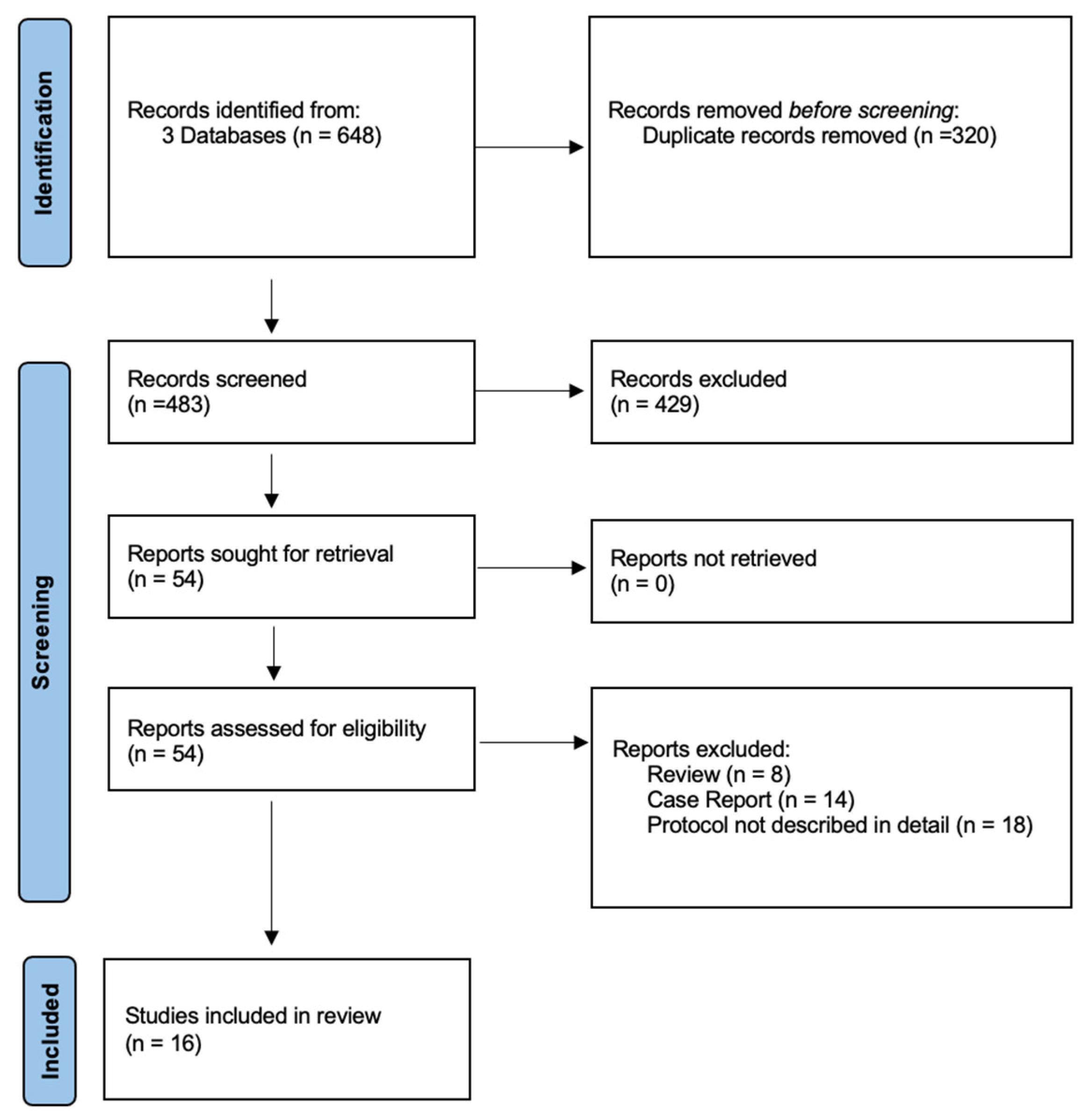
2. Materials and Methods
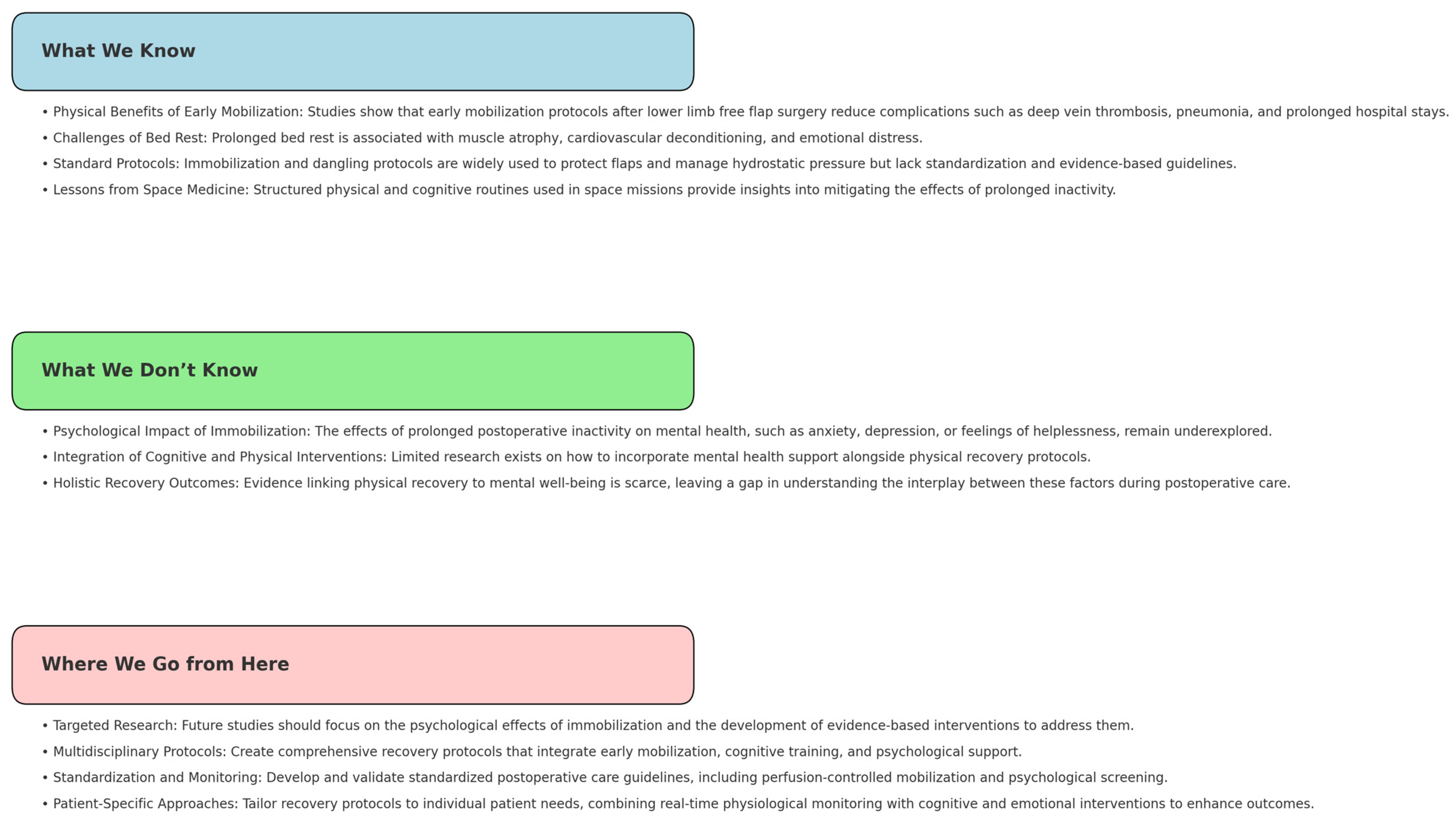
3. Results
3.1. Acceleration of the Postoperative Protocol
3.2. Expert Opinions
3.3. Perfusion-Controlled Mobilization
4. Discussion
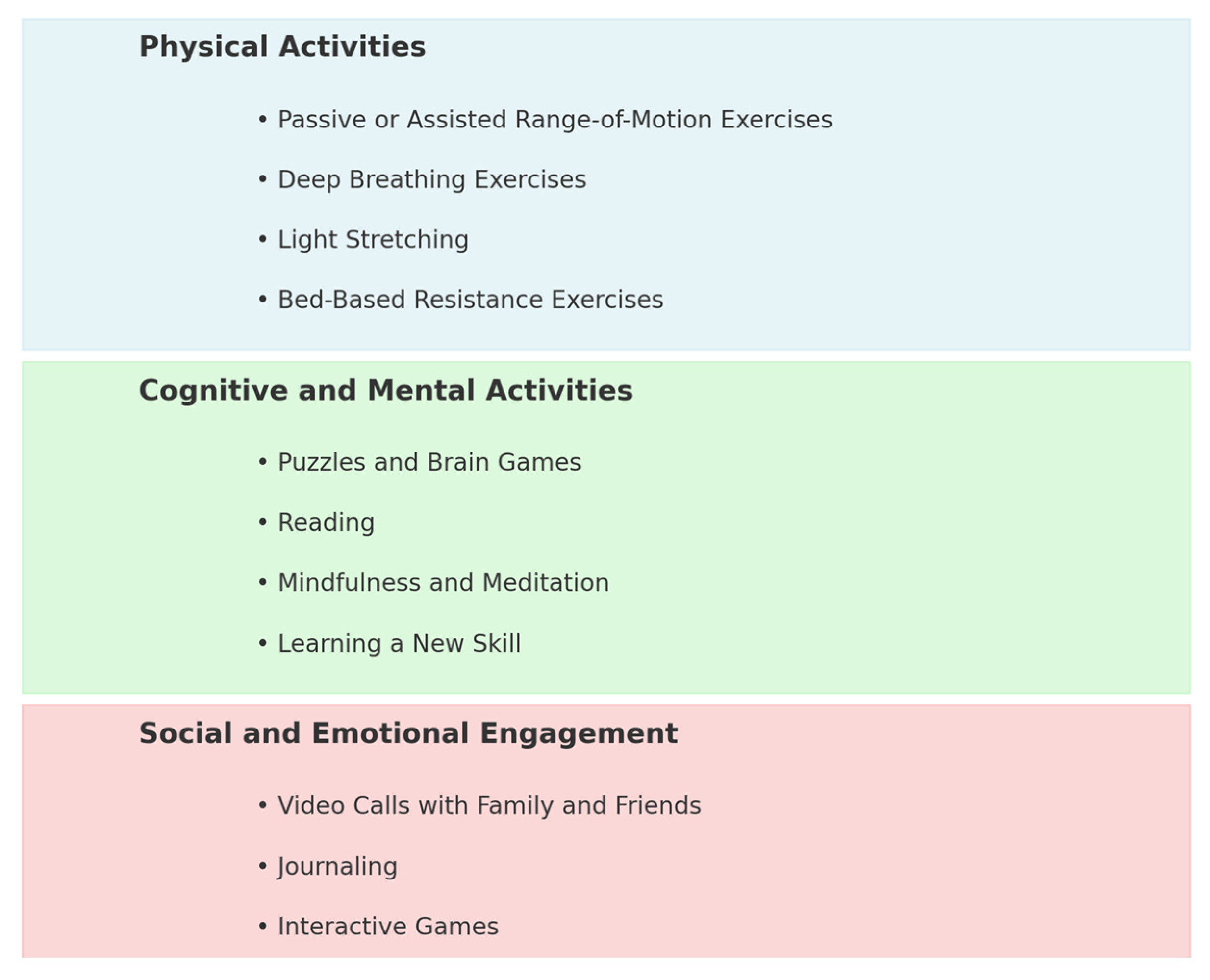
4.1. Lessons Learned from Space Flight
4.1.1. Physical Activities
4.1.2. Cognitive and Mental Activities
4.1.3. Social and Emotional Engagement
4.2. Psychological Benefits of Early Mobilization and the Unexplored Potential for Expanded Mental Support
- Psychological screening: Identifying patients at risk of anxiety or depression early in their recovery;
- Targeted mental health support: Including mindfulness, cognitive behavioral therapy, or stress management techniques in standard care;
- Therapeutic environments: Designing recovery spaces to reduce feelings of isolation and promote wellbeing;
- Technology integration: Using virtual reality or gamified therapy to motivate patients and distract them from stress or discomfort.
4.3. Outlook
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pu, L.L.Q. Free Flaps in Lower Extremity Reconstruction. Clin. Plast. Surg. 2021, 48, 201–214. [Google Scholar] [CrossRef]
- Soteropulos, C.; Chen, J.; Poore, S.; Garland, C. Postoperative Management of Lower Extremity Free Tissue Transfer: A Systematic Review. J. Reconstr. Microsurg. 2019, 35, 001–007. [Google Scholar] [CrossRef]
- Lee, Z.-H.; Ramly, E.P.; Alfonso, A.R.; Daar, D.A.; Kaoutzanis, C.; Kantar, R.S.; Thanik, V.; Saadeh, P.B.; Levine, J.P. Dangle Protocols in Lower Extremity Reconstruction. J. Surg. Res. 2021, 266, 77–87. [Google Scholar] [CrossRef]
- Krijgh, D.D.; Teunis, T.; List, E.B.; Mureau, M.A.M.; Luijsterburg, A.J.M.; Maarse, W.; Schellekens, P.P.A.; Hietbrink, F.; De Jong, T.; Coert, J.H. Mental Health Is Strongly Associated with Capability after Lower Extremity Injury Treated with Free Flap Limb Salvage or Amputation. Eur. J. Trauma Emerg. Surg. 2024, 50, 755–762. [Google Scholar] [CrossRef] [PubMed]
- Maloni, J.A.; Kasper, C.E. Physical and Psychosocial Effects of Anteparturn Hospital Bedrest: A Review of the Literature. Image J. Nurs. Scholarsh. 1991, 23, 187–192. [Google Scholar] [CrossRef] [PubMed]
- Twomey, R.; Matthews, T.W.; Nakoneshny, S.; Schrag, C.; Chandarana, S.P.; Matthews, J.; McKenzie, D.; Hart, R.D.; Li, N.; Sauro, K.M.; et al. Impact of Early Mobilization on Recovery after Major Head and Neck Surgery with Free Flap Reconstruction. Cancers 2021, 13, 2852. [Google Scholar] [CrossRef]
- Harris, B.N.; Bewley, A.F. Minimizing Free Flap Donor-Site Morbidity. Curr. Opin. Otolaryngol. Head Neck Surg. 2016, 24, 447–452. [Google Scholar] [CrossRef]
- Dort, J.C.; Farwell, D.G.; Findlay, M.; Huber, G.F.; Kerr, P.; Shea-Budgell, M.A.; Simon, C.; Uppington, J.; Zygun, D.; Ljungqvist, O.; et al. Optimal Perioperative Care in Major Head and Neck Cancer Surgery With Free Flap Reconstruction: A Consensus Review and Recommendations From the Enhanced Recovery After Surgery Society. JAMA Otolaryngol. Neck Surg. 2017, 143, 292. [Google Scholar] [CrossRef]
- Elhassan, A.; Ahmed, A.; Awad, H.; Humeidan, M.; Urman, R.D.; Labrie-Brown, C.L.; Cornett, E.M.; Kaye, A.D. Enhanced Recovery for Breast Reconstruction Surgery. Curr. Pain Headache Rep. 2019, 23, 27. [Google Scholar] [CrossRef] [PubMed]
- Al-Khalil, M.; Roman, M.; Emam, A.; Marsden, N. Comparison of Outcomes between Early and Delayed Weight Bearing Following Lower Limb Free Flaps: An 18-Month Single-Center Study. Plast. Aesthetic Res. 2023, 10, 15. [Google Scholar] [CrossRef]
- Yeung, J.K.; Harrop, R.; McCreary, O.; Leung, L.T.; Hirani, N.; McKenzie, D.; De Haas, V.; Matthews, T.W.; Nakoneshny, S.; Dort, J.C.; et al. Delayed Mobilization after Microsurgical Reconstruction: An Independent Risk Factor for Pneumonia. Laryngoscope 2013, 123, 2996–3000. [Google Scholar] [CrossRef] [PubMed]
- Neubert, N.; Vogt, P.; May, M.; Boyce, M.; Koenneker, S.; Budde, E.; Jokuszies, A. Does an Early and Aggressive Combined Wrapping and Dangling Procedure Affect the Clinical Outcome of Lower Extremity Free Flaps?—A Randomized Controlled Prospective Study Using Microdialysis Monitoring. J. Reconstr. Microsurg. 2016, 32, 262–270. [Google Scholar] [CrossRef] [PubMed]
- Orseck, M.J.; Smith, C.R.; Kirby, S.; Trujillo, M. Early Ambulation After Microsurgical Reconstruction of the Lower Extremity. Ann. Plast. Surg. 2018, 80, S362–S364. [Google Scholar] [CrossRef]
- Miyamoto, S.; Kayano, S.; Fujiki, M.; Chuman, H.; Kawai, A.; Sakuraba, M. Early Mobilization after Free-Flap Transfer to the Lower Extremities: Preferential Use of Flow-through Anastomosis. Plast. Reconstr.Surg.–Glob. Open 2014, 2, e127. [Google Scholar] [CrossRef]
- Jokuszies, A.; Neubert, N.; Herold, C.; Vogt, P. Early Start of the Dangling Procedure in Lower Extremity Free Flap Reconstruction Does Not Affect the Clinical Outcome. J. Reconstr. Microsurg. 2013, 29, 027–032. [Google Scholar] [CrossRef]
- Yim, G.H.; Pikturnaite, J.; Harry, L.; Clement, R.; Pope-Jones, S.; Emam, A.; Marsden, N. Enhanced Recovery for Acute Open Lower Limb Fracture ‘Fix and Flap’. Injury 2024, 55, 111234. [Google Scholar] [CrossRef] [PubMed]
- Seth, A.; Diamond, S.; Iorio, M. Outcomes of an Early Protocol for Dependent Conditioning in Lower Extremity Microsurgical Free Flaps. J. Reconstr. Microsurg. 2017, 33, 670–678. [Google Scholar] [CrossRef]
- Rohde, C.; Howell, B.; Buncke, G.; Gurtner, G.; Levin, L.; Pu, L.; Levine, J. A Recommended Protocol for the Immediate Postoperative Care of Lower Extremity Free-Flap Reconstructions. J. Reconstr. Microsurg. 2009, 25, 015–019. [Google Scholar] [CrossRef] [PubMed]
- Xipoleas, G.; Levine, E.; Silver, L.; Koch, R.M.; Taub, P.J. A Survey of Microvascular Protocols for Lower Extremity Free Tissue Transfer II: Postoperative Care. Ann. Plast. Surg. 2008, 61, 280–284. [Google Scholar] [CrossRef]
- Trull, B.; Zhang, Z.; Boyd, K.; Allen, M.; Zhang, J. Canadian Postoperative Dependency Protocols Following Lower Limb Microvascular Reconstruction: A National Survey and Literature Review. Plast. Surg. 2021, 29, 122–127. [Google Scholar] [CrossRef]
- Bonapace-Potvin, M.; Govshievich, A.; Tessier, L.; Karunanayake, M.; Tremblay, D.; Chollet, A. Canadian Trends in Free Flap Management for Microsurgical Lower Limb Reconstruction. Plast. Surg. 2023, 31, 70–77. [Google Scholar] [CrossRef] [PubMed]
- Cerny, M.; Schantz, J.-T.; Erne, H.; Schmauss, D.; Giunta, R.; Machens, H.-G.; Schenck, T. Überblick und Vorstellung eines Behandlungskonzeptes zur postoperativen Therapie und Mobilisation nach freier Lappenplastik an der unteren Extremität. Handchir. Mikrochir. Plast. Chir. 2016, 48, 363–369. [Google Scholar] [CrossRef]
- Kolbenschlag, J.; Bredenbroeker, P.; Lehnhardt, M.; Daigeler, A.; Fischer, S.; Harati, K.; Ring, A.; Goertz, O. Advanced Microcirculatory Parameters of Lower Extremity Free Flaps during Dangling and Their Influencing Factors. J. Reconstr. Microsurg. 2015, 31, 500–507. [Google Scholar] [CrossRef]
- Dornseifer, U.; Kleeberger, C.; Kargl, L.; Schönberger, M.; Rohde, D.; Ninkovic, M.; Schilling, A. Perfusion Controlled Mobilization after Lower Extremity Free Flaps—Pushing the Limits of Time and Intensity. J. Reconstr. Microsurg. 2016, 33, 179–185. [Google Scholar] [CrossRef]
- Lindelauf, A.A.M.A.; Van Rooij, J.A.F.; Hartveld, L.; Van Der Hulst, R.R.W.J.; Weerwind, P.W.; Schols, R.M. Tissue Oximetry Changes during Postoperative Dangling in Lower Extremity Free Flap Reconstruction: A Pilot Study. Life 2023, 13, 1158. [Google Scholar] [CrossRef]
- Colen, D.; Colen, L.; Levin, L.; Kovach, S. Godina’s Principles in the Twenty-First Century and the Evolution of Lower Extremity Trauma Reconstruction. J. Reconstr. Microsurg. 2018, 34, 563–571. [Google Scholar] [CrossRef] [PubMed]
- Aljawadi, A.; Islam, A.; Jahangir, N.; Niazi, N.; Elmajee, M.; Reid, A.; Wong, J.; Pillai, A. One-Stage Combined “Fix and Flap” Approach for Complex Open Gustilo–Anderson IIIB Lower Limbs Fractures: A Prospective Review of 102 Cases. Arch. Orthop. Trauma Surg. 2022, 142, 425–434. [Google Scholar] [CrossRef]
- Højvig, J.H.; Charabi, B.W.; Wessel, I.; Jensen, L.T.; Nyberg, J.; Maymann-Holler, N.; Kehlet, H.; Bonde, C.T. Enhanced Recovery after Microvascular Reconstruction in Head and Neck Cancer—A Prospective Study. JPRAS Open 2022, 34, 103–113. [Google Scholar] [CrossRef]
- Batdorf, N.J.; Lemaine, V.; Lovely, J.K.; Ballman, K.V.; Goede, W.J.; Martinez-Jorge, J.; Booth-Kowalczyk, A.L.; Grubbs, P.L.; Bungum, L.D.; Saint-Cyr, M. Enhanced Recovery after Surgery in Microvascular Breast Reconstruction. J. Plast. Reconstr. Aesthetic Surg. 2015, 68, 395–402. [Google Scholar] [CrossRef] [PubMed]
- National Aeronautics and Space Administration (NASA). Human Research Program: Human Factors and Behavioral Health Element. 2019. Available online: https://www.nasa.gov/reference/about-human-factors-and-behavioral-performance/ (accessed on 23 November 2024).
- Palinkas, L.A.; Suedfeld, P. Psychosocial Issues in Isolated and Confined Extreme Environments. Neurosci. Biobehav. Rev. 2021, 126, 413–429. [Google Scholar] [CrossRef]
- Comfort, P.; McMahon, J.J.; Jones, P.A.; Cuthbert, M.; Kendall, K.; Lake, J.P.; Haff, G.G. Effects of Spaceflight on Musculoskeletal Health: A Systematic Review and Meta-Analysis, Considerations for Interplanetary Travel. Sports Med. 2021, 51, 2097–2114. [Google Scholar] [CrossRef] [PubMed]
- Payne, M.W.C.; Williams, D.R.; Trudel, G. Space Flight Rehabilitation. Am. J. Phys. Med. Rehabil. 2007, 86, 583–591. [Google Scholar] [CrossRef] [PubMed]
- Marusic, U.; Narici, M.; Simunic, B.; Pisot, R.; Ritzmann, R. Nonuniform Loss of Muscle Strength and Atrophy during Bed Rest: A Systematic Review. J. Appl. Physiol. 2021, 131, 194–206. [Google Scholar] [CrossRef] [PubMed]
- Le Roux, E.; De Jong, N.P.; Blanc, S.; Simon, C.; Bessesen, D.H.; Bergouignan, A. Physiology of Physical Inactivity, Sedentary Behaviours and Non-exercise Activity: Insights from the Space Bedrest Model. J. Physiol. 2022, 600, 1037–1051. [Google Scholar] [CrossRef] [PubMed]
- Lipnicki, D.M.; Gunga, H.-C. Physical Inactivity and Cognitive Functioning: Results from Bed Rest Studies. Eur. J. Appl. Physiol. 2009, 105, 27–35. [Google Scholar] [CrossRef]
- Exploring the Relationship Between Video Calls and Mental Health. Available online: https://www.storific.com/blog/exploring-the-relationship-between-video-calls-and-mental-health?utm.com (accessed on 16 October 2024).
- Joseph, I.; McCauley, R. Impact of Early Mobilization in the Intensive Care Unit on Psychological Issues. Crit. Care Nurs. Clin. N. Am. 2019, 31, 501–505. [Google Scholar] [CrossRef]
- Kalisch, B.J.; Lee, S.; Dabney, B.W. Outcomes of Inpatient Mobilization: A Literature Review. J. Clin. Nurs. 2014, 23, 1486–1501. [Google Scholar] [CrossRef]
| Author and Year | Study Design | Prospective/Retrospective | Number of Participants | Focus (Investigated Question) | Key Findings |
|---|---|---|---|---|---|
| Al-Khalil et al., 2023 [10] | Cohort Study | Retrospective | 37 (patients) | Impact of early vs. delayed mobilization | Early mobilization reduced recovery time and anxiety. |
| Yeung et al., 2013 [11] | Cohort Study | Retrospective | 62 (patients) | Delayed mobilization and outcomes | Delayed mobilization increased anxiety and complications. |
| Neubert et al., 2016 [12] | RCT | Prospective | 49 (patients) | Aggressive combined wrapping in early mobilization | No significant flap failure differences but higher satisfaction. |
| Orseck et al., 2018 [13] | Cohort Study | Prospective | 36 (patients) | Psychological effects of early ambulation | Positive emotional outcomes with early ambulation. |
| Miyamoto et al., 2014 [14] | Cohort Study | Retrospective | 13 (patients) | Early mobilization effectiveness | Strong evidence for reducing complications. |
| Jokuszies et al., 2013 [15] | RCT | Prospective | 31 (patients) | Dangling protocols for limb recovery | Earlier dangling enhances outcomes. |
| Yim et al., 2024 [16] | Observational Study | Prospective | 161 (patients) | Enhanced recovery for open fractures | Shortened stays and high salvage rates. |
| Seth et al., 2017 [17] | Pilot Study | Retrospective | 26 (patients) | Dependent conditioning outcomes | Improved psychological and physical recovery. |
| Rohde et al., 2009 [18] | Survey Study | N/A * | 5 (experts) | Consensus on postoperative dependency | Suggested standardized recommendations. |
| Xipoleas et al., 2008 [19] | Survey Study | N/A * | 98 (experts) | Postoperative free flap monitoring | Clinical observation remained dominant. |
| Trull et al., 2021 [20] | National Survey | N/A * | 16 (experts) | Canadian trends in dangling protocols | Significant variability in protocols. |
| Bonapace-Potvin et al., 2023 [21] | Survey Study | N/A * | 28 (experts) | Timing of dangling protocols | Early dangling enhanced outcomes. |
| Cerny et al., 2016 [22] | Survey Study | N/A * | 32 (department) | Hydrostatic pressure management | Summarized hydrostatic pressure protocols. |
| Kolbenschlag et al., 2015 [23] | Cohort Study | Prospective | 39 (patients) | Microcirculatory changes in dangling | Revealed benefits of early mobilization. |
| Dornseifer et al., 2016 [24] | Cohort Study | Prospective | 15 (patients) | Perfusion-controlled mobilization | Safe early mobilization with monitoring. |
| Lindelauf et al., 2023 [25] | Pilot Study | Prospective | 10 (patients) | Oximetry during postoperative dangling | Oximetry confirmed safety of early mobilization. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dietrich, L.G.; Zubler, C. Physical and Psychological Burden of Bed Rest on Patients Following Free Flap Reconstruction of the Lower Limb: A Systematic Review and Possible Solutions. J. Clin. Med. 2025, 14, 705. https://doi.org/10.3390/jcm14030705
Dietrich LG, Zubler C. Physical and Psychological Burden of Bed Rest on Patients Following Free Flap Reconstruction of the Lower Limb: A Systematic Review and Possible Solutions. Journal of Clinical Medicine. 2025; 14(3):705. https://doi.org/10.3390/jcm14030705
Chicago/Turabian StyleDietrich, Léna G., and Cédric Zubler. 2025. "Physical and Psychological Burden of Bed Rest on Patients Following Free Flap Reconstruction of the Lower Limb: A Systematic Review and Possible Solutions" Journal of Clinical Medicine 14, no. 3: 705. https://doi.org/10.3390/jcm14030705
APA StyleDietrich, L. G., & Zubler, C. (2025). Physical and Psychological Burden of Bed Rest on Patients Following Free Flap Reconstruction of the Lower Limb: A Systematic Review and Possible Solutions. Journal of Clinical Medicine, 14(3), 705. https://doi.org/10.3390/jcm14030705






