Imaging Findings of Human Papillomavirus-Positive and Human Papillomavirus-Negative Oropharyngeal Squamous Cell Carcinoma Associated with Recurrence
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Imaging Technique
2.3. Imaging Assessment
2.4. Statistical Analysis
3. Results
3.1. Patient Characteristics
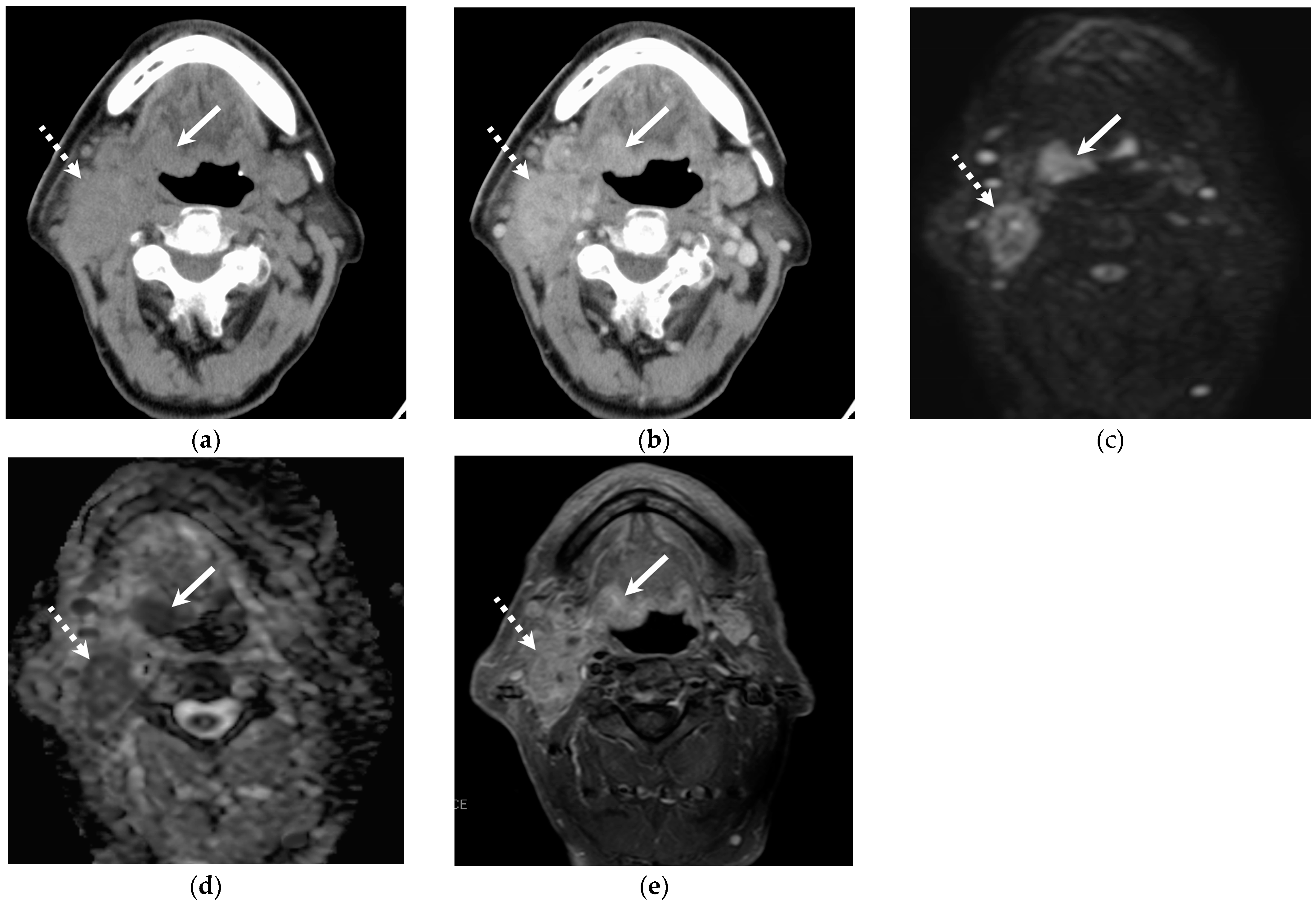
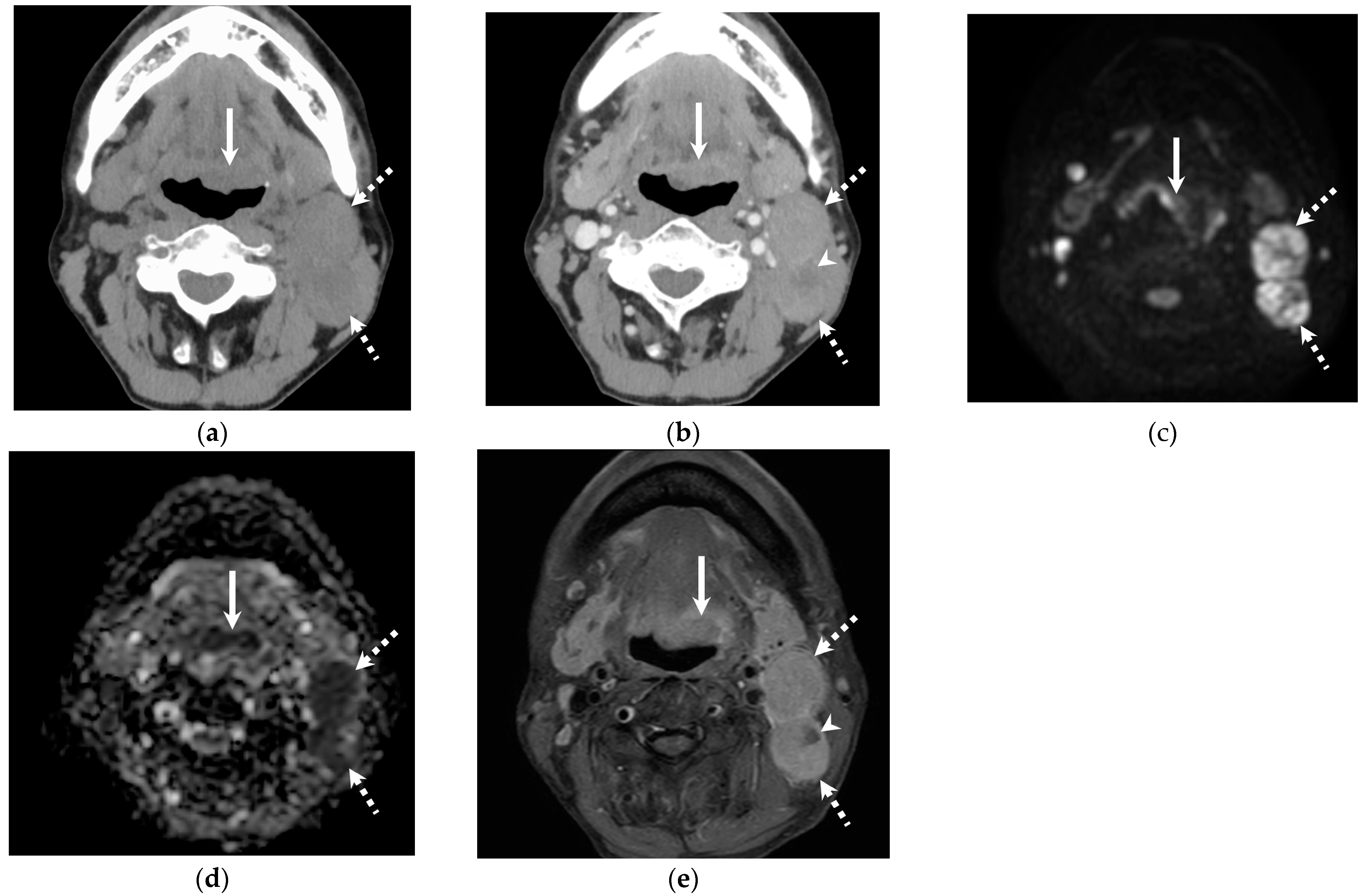
3.2. Quantitative and Qualitative Imaging Findings of the Primary Lesion
3.3. Quantitative Imaging Findings of Cervical Lymph Node Metastasis
3.4. Qualitative Imaging Findings of Cervical Lymph Node Metastasis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lechner, M.; Liu, J.; Masterson, L.; Fenton, T.R. HPV-associated oropharyngeal cancer: Epidemiology, molecular biology and clinical management. Nat. Rev. Clin. Oncol. 2022, 19, 306–327. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, K.; Hisamatsu, K.; Suzui, N.; Hara, A.; Tomita, H.; Miyazaki, T. A Review of HPV-Related Head and Neck Cancer. J. Clin. Med. 2018, 7, 241. [Google Scholar] [CrossRef]
- Consalvo, F.; De Simone, M.; Scarpa, A.; Acerra, A.; Salzano, F.A.; Fineschi, V.; Santurro, A. Challenges and Complications in the Management of Advanced Oropharyngeal Carcinoma: Role of Post-Mortem Diagnosis and Future Perspectives. J. Clin. Med. 2024, 13, 5198. [Google Scholar] [CrossRef]
- D’Souza, G.; Kreimer, A.R.; Viscidi, R.; Pawlita, M.; Fakhry, C.; Koch, W.M.; Westra, W.H.; Gillison, M.L. Case-control study of human papillomavirus and oropharyngeal cancer. N. Engl. J. Med. 2007, 356, 1944–1956. [Google Scholar] [CrossRef]
- Lydiatt, W.M.; Patel, S.G.; O’Sullivan, B.; Brandwein, M.S.; Ridge, J.A.; Migliacci, J.C.; Loomis, A.M.; Shah, J.P. Head and Neck cancers-major changes in the American Joint Committee on cancer eighth edition cancer staging manual. CA Cancer J. Clin. 2017, 67, 122–137. [Google Scholar] [CrossRef]
- Cantrell, S.C.; Peck, B.W.; Li, G.; Wei, Q.; Sturgis, E.M.; Ginsberg, L.E. Differences in imaging characteristics of HPV-positive and HPV-Negative oropharyngeal cancers: A blinded matched-pair analysis. AJNR Am. J. Neuroradiol. 2013, 34, 2005–2009. [Google Scholar] [CrossRef] [PubMed]
- Bhattasali, O.; Thompson, L.D.R.; Schumacher, A.J.; Iganej, S. Radiographic nodal prognostic factors in stage I HPV-related oropharyngeal squamous cell carcinoma. Head Neck 2019, 41, 398–402. [Google Scholar] [CrossRef] [PubMed]
- Morey, T.; Hodge, J.C.; Stern, C.; Krishnan, S.; Foreman, A. Correlation between radiologic and pathologic extranodal extension in HPV-associated oropharyngeal cancer: Systematic review. Head Neck 2022, 44, 2875–2885. [Google Scholar] [CrossRef] [PubMed]
- Billfalk-Kelly, A.; Yu, E.; Su, J.; O’Sullivan, B.; Waldron, J.; Ringash, J.; Bartlett, E.; Perez-Ordonez, B.; Weinreb, I.; Bayley, A.; et al. Radiologic Extranodal Extension Portends Worse Outcome in cN+ TNM-8 Stage I Human Papillomavirus-Mediated Oropharyngeal Cancer. Int. J. Radiat. Oncol. Biol. Phys. 2019, 104, 1017–1027. [Google Scholar] [CrossRef] [PubMed]
- Huang, S.H.; O’Sullivan, B.; Su, J.; Bartlett, E.; Kim, J.; Waldron, J.N.; Ringash, J.; de Almeida, J.R.; Bratman, S.; Hansen, A.; et al. Prognostic importance of radiologic extranodal extension in HPV-positive oropharyngeal carcinoma and its potential role in refining TNM-8 cN-classification. Radiother. Oncol. 2020, 144, 13–22. [Google Scholar] [CrossRef]
- Choi, Y.; Nam, Y.; Jang, J.; Shin, N.Y.; Ahn, K.J.; Kim, B.S.; Lee, Y.S.; Kim, M.S. Prediction of Human Papillomavirus Status and Overall Survival in Patients with Untreated Oropharyngeal Squamous Cell Carcinoma: Development and Validation of CT-Based Radiomics. AJNR Am. J. Neuroradiol. 2020, 41, 1897–1904. [Google Scholar] [CrossRef]
- Kawaguchi, M.; Kato, H.; Tomita, H.; Hara, A.; Suzui, N.; Miyazaki, T.; Matsuo, M. Comparison of Imaging Findings between Human Papillomavirus-positive and -Negative Squamous Cell Carcinomas of the Maxillary Sinus. J. Clin. Imaging Sci. 2020, 10, 59. [Google Scholar] [CrossRef] [PubMed]
- Hiyama, T.; Kuno, H.; Nagaki, T.; Sekiya, K.; Oda, S.; Fujii, S.; Hayashi, R.; Kobayashi, T. Extra-nodal extension in head and neck cancer: How radiologists can help staging and treatment planning. Jpn. J. Radiol. 2020, 38, 489–506. [Google Scholar] [CrossRef] [PubMed]
- Kanda, Y. Investigation of the freely available easy-to-use software ’EZR’ for medical statistics. Bone Marrow Transplant. 2013, 48, 452–458. [Google Scholar] [CrossRef] [PubMed]
- Lassen, P.; Eriksen, J.G.; Hamilton-Dutoit, S.; Tramm, T.; Alsner, J.; Overgaard, J. Effect of HPV-associated p16INK4A expression on response to radiotherapy and survival in squamous cell carcinoma of the head and neck. J. Clin. Oncol. 2009, 27, 1992–1998. [Google Scholar] [CrossRef] [PubMed]
- Maxwell, J.H.; Kumar, B.; Feng, F.Y.; Worden, F.P.; Lee, J.S.; Eisbruch, A.; Wolf, G.T.; Prince, M.E.; Moyer, J.S.; Teknos, T.N.; et al. Tobacco use in human papillomavirus-positive advanced oropharynx cancer patients related to increased risk of distant metastases and tumor recurrence. Clin. Cancer Res. 2010, 16, 1226–1235. [Google Scholar] [CrossRef]
- Nomura, F.; Sugimoto, T.; Kitagaki, K.; Ito, T.; Kawachi, H.; Eishi, Y.; Watanabe, K.; Igaue, M.; Shimizu, N.; Tomita, M.; et al. Clinical characteristics of Japanese oropharyngeal squamous cell carcinoma positive for human papillomavirus infection. Acta Otolaryngol. 2014, 134, 1265–1274. [Google Scholar] [CrossRef] [PubMed]
- Mizumachi, T.; Kano, S.; Sakashita, T.; Hatakeyama, H.; Suzuki, S.; Homma, A.; Oridate, N.; Fukuda, S. Improved survival of Japanese patients with human papillomavirus-positive oropharyngeal squamous cell carcinoma. Int. J. Clin. Oncol. 2013, 18, 824–828. [Google Scholar] [CrossRef]
- Sistonen, H.J.; Aro, K.; Atula, T.; Jouhi, L.; Lindén, R.; Tapiovaara, L.; Loimu, V.; Markkola, A. Prognostic Value of Apparent Diffusion Coefficient in Oropharyngeal Carcinoma. Clin. Neuroradiol. 2021, 31, 1037–1048. [Google Scholar] [CrossRef] [PubMed]
- Chang, C.M.; Chen, M.M.; Bellile, E.L.; Rozek, L.S.; Carey, T.E.; Spector, M.E.; Wolf, G.T.; Taylor, J.M.; Chinn, S.B. Impact of Nodal Metastases in HPV-Negative Oropharyngeal Cancer. Cancer Epidemiol. Biomark. Prev. 2022, 31, 1554–1563. [Google Scholar] [CrossRef] [PubMed]
- Yin, L.X.; D’Souza, G.; Westra, W.H.; Wang, S.J.; van Zante, A.; Zhang, Y.; Rettig, E.M.; Ryan, W.R.; Ha, P.K.; Wentz, A.; et al. Prognostic factors for human papillomavirus-positive and negative oropharyngeal carcinomas. Laryngoscope 2018, 128, E287–E295. [Google Scholar] [CrossRef]
- Amin, M.B.; Greene, F.L.; Edge, S.B.; Compton, C.C.; Gershenwald, J.E.; Brookland, R.K.; Meyer, L.; Gress, D.M.; Byrd, D.R.; Winchester, D.P. The Eighth Edition AJCC Cancer Staging Manual: Continuing to build a bridge from a population-based to a more “personalized” approach to cancer staging. CA Cancer J. Clin. 2017, 67, 93–99. [Google Scholar] [CrossRef] [PubMed]
- Kumar, B.; Cipolla, M.J.; Old, M.O.; Brown, N.V.; Kang, S.Y.; Dziegielewski, P.T.; Durmus, K.; Ozer, E.; Agrawal, A.; Carrau, R.L.; et al. Surgical management of oropharyngeal squamous cell carcinoma: Survival and functional outcomes. Head Neck 2016, 38 (Suppl. 1), E1794–E1802. [Google Scholar] [CrossRef] [PubMed]
- Cai, C.; Chernock, R.D.; Pittman, M.E.; El-Mofty, S.K.; Thorstad, W.L.; Lewis, J.S., Jr. Keratinizing-type squamous cell carcinoma of the oropharynx: p16 overexpression is associated with positive high-risk HPV status and improved survival. Am. J. Surg. Pathol. 2014, 38, 809–815. [Google Scholar] [CrossRef] [PubMed]
- Ravanelli, M.; Grammatica, A.; Maddalo, M.; Ramanzin, M.; Agazzi, G.M.; Tononcelli, E.; Battocchio, S.; Bossi, P.; Vezzoli, M.; Maroldi, R.; et al. Pretreatment DWI with Histogram Analysis of the ADC in Predicting the Outcome of Advanced Oropharyngeal Cancer with Known Human Papillomavirus Status Treated with Chemoradiation. AJNR Am. J. Neuroradiol. 2020, 41, 1473–1479. [Google Scholar] [CrossRef]
- Huang, Y.H.; Yeh, C.H.; Cheng, N.M.; Lin, C.Y.; Wang, H.M.; Ko, S.F.; Toh, C.H.; Yen, T.C.; Liao, C.T.; Ng, S.H. Cystic nodal metastasis in patients with oropharyngeal squamous cell carcinoma receiving chemoradiotherapy: Relationship with human papillomavirus status and failure patterns. PLoS ONE 2017, 12, e0180779. [Google Scholar] [CrossRef] [PubMed]
- Ting, Y.; Chee, J.; Charn, T.C.; Loh, K.S.; Choong, C.C.; Ting, E.; Lim, C.M. Prognostic significance of cystic lymph nodal metastasis in nasopharyngeal carcinoma. Head Neck 2017, 39, 1832–1839. [Google Scholar] [CrossRef]
- Rath, T.J.; Narayanan, S.; Hughes, M.A.; Ferris, R.L.; Chiosea, S.I.; Branstetter, B.F.t. Solid Lymph Nodes as an Imaging Biomarker for Risk Stratification in Human Papillomavirus-Related Oropharyngeal Squamous Cell Carcinoma. AJNR Am. J. Neuroradiol. 2017, 38, 1405–1410. [Google Scholar] [CrossRef]
- Benchetrit, L.; Torabi, S.J.; Givi, B.; Haughey, B.; Judson, B.L. Prognostic Significance of Extranodal Extension in HPV-Mediated Oropharyngeal Carcinoma: A Systematic Review and Meta-analysis. Otolaryngol. Head Neck Surg. 2021, 164, 720–732. [Google Scholar] [CrossRef] [PubMed]
| All Patients | HPV-Positive OPSCC | HPV-Negative OPSCC | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Recurrence | p | Recurrence | p | Recurrence | p | ||||
| Yes (n = 17) | No (n = 51) | Yes (n = 7) | No (n = 41) | Yes (n = 10) | No (n = 10) | ||||
| Age (years) | 71 [67–75] | 66 [52–71] | 0.013 | 73 [70–75] | 60 [51–68] | 0.045 | 69 [67–74] | 70 [52–76] | 0.73 |
| Male | 7 (41%) | 38 (75%) | >0.99 | 5 (71%) | 30 (73%) | >0.99 | 8 (80%) | 8 (80%) | >0.99 |
| Smoking | 13 (76%) | 34 (67%) | 0.55 | 5 (71%) | 27 (66%) | >0.99 | 8 (80%) | 7 (70%) | >0.99 |
| Surgery | 8 (47%) | 37 (73%) | 0.08 | 4 (57%) | 12 (29%) | 0.20 | 5 (50%) | 8 (80%) | 0.35 |
| Chemotherapy | 14 (82%) | 28 (55%) | 0.049 | 5 (71%) | 23 (56%) | 0.68 | 9 (90%) | 5 (50%) | 0.14 |
| Radiation | 15 (88%) | 35 (69%) | 0.20 | 6 (86%) | 29 (70%) | 0.66 | 9 (90%) | 6 (60%) | 0.30 |
| T stage | 0.02 | 0.52 | 0.04 | ||||||
| T1 | 1 (6%) | 9 (18%) | 1 (14%) | 6 (15%) | 0 (0%) | 3 (30%) | |||
| T2 | 6 (35%) | 31 (61%) | 4 (57%) | 26 (63%) | 2 (20%) | 5 (50%) | |||
| T3 | 4 (24%) | 2 (4%) | 1 (14%) | 1 (2%) | 3 (30%) | 1 (10%) | |||
| T4 | 6 (35%) | 9 (18%) | 1 (14%) | 8 (20%) | 5 (50%) | 1 (10%) | |||
| N stage | 0.35 | >0.99 | 0.04 | ||||||
| N0 | 1 (6%) | 10 (20%) | 1 (14%) | 6 (15%) | 0 (0%) | 4 (40%) | |||
| N1 | 8 (47%) | 27 (53%) | 5 (71%) | 27 (66%) | 3 (30%) | 0 (0%) | |||
| N2 | 7 (41%) | 12 (24%) | 1 (14%) | 8 (20%) | 6 (60%) | 4 (40%) | |||
| N3 | 1 (6%) | 2 (4%) | 0 (0%) | 0 (0%) | 1 (10%) | 2 (20%) | |||
| M stage | NA | NA | NA | ||||||
| M1 | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | |||
| Quantitative Imaging Findings of Primary Lesion | |||||||
|---|---|---|---|---|---|---|---|
| HPV-Positive OPSCC | HPV-Negative OPSCC | ||||||
| Recurrence | p | Recurrence | p | ||||
| Yes (n = 7) | No (n = 41) | Yes (n = 10) | No (n = 10) | ||||
| Maximum diameter (mm) | 21.9 [18.2–26.6] | 28.4 [19.7–34.7] | 0.18 | 32.7 [26.0–45.4] | 20.8 [19.3–33.9] | 0.04 | |
| CT | |||||||
| Attenuation on UECT (HU) | 50.3 [41.6–55.7] | 50.4 [43.4–55.4] | 0.81 | 42.1 [38.7–44.6] | 49.4 [46.6–50.6] | <0.01 | |
| Attenuation on CECT (HU) | 85.7 [82.3–93.7] | 85.0 [78.4–97.3] | 0.88 | 90.2 [76.1–95.2] | 90.7 [83.8–97.8] | 0.87 | |
| MRI | |||||||
| SIR on T1WI | 1.04 [0.98–1.06] | 0.98 [0.93–1.06] | 0.42 | 0.99 [0.92–1.03] | 0.94 [0.92–0.99] | 0.63 | |
| SIR on T2WI | 1.12 [1.09–1.14] | 1.06 [1.00–1.15] | 0.37 | 1.02 [0.87–1.09] | 1.16 [1.06–1.22] | 0.089 | |
| SIR on DWI | 1.66 [1.57–1.79] | 1.32 [1.08–1.46] | <0.01 | 1.15 [0.99–1.36] | 1.23 [0.95–1.55] | 0.58 | |
| SIR on CET1WI | 2.05 [1.92–2.21] | 1.82 [1.63–1.99] | 0.02 | 2.04 [1.76–2.19] | 1.97 [1.91–2.07] | 0.91 | |
| ADC value (×10−3 mm2/s) | 0.82 [0.69–1.05] | 0.80 [0.73–0.89] | 0.98 | 0.91 [0.76–1.06] | 1.02 [0.91–1.08] | 0.51 | |
| 18F-FDG-PET/CT | |||||||
| SUVmax | 15.3 [10.6–18.3] | 12.61 [8.9–15.9] | 0.58 | 16.5 [14.5–20.5] | 18.5 [12.0–20.7] | 0.96 | |
| Qualitative imaging findings of primary lesion | |||||||
| CT | |||||||
| Well-defined margin | 5 (71%) | 23 (56%) | 0.68 | 5 (50%) | 4 (40%) | >0.99 | |
| Necrosis | 1 (14%) | 9 (22%) | >0.99 | 2 (20%) | 1 (10%) | >0.99 | |
| MRI | |||||||
| Well-defined margin | 7 (100%) | 33 (80%) | 0.58 | 4 (40%) | 7 (70%) | 0.37 | |
| Necrosis | 2 (29%) | 8 (20%) | 0.63 | 3 (30%) | 2 (20%) | >0.99 | |
| Marginal invasion | 1 (14%) | 6 (15%) | >0.99 | 5 (50%) | 3 (30%) | 0.65 | |
| T1WI | Hyperintensity Isointensity Hypointensity | 1 (14%) 2 (29%) 4 (57%) | 2 (5%) 19 (46%) 20 (49%) | 0.41 | 1 (10%) 3 (30%) 6 (60%) | 0 (0%) 5 (50%) 5 (50%) | 0.65 |
| T2WI | Hyperintensity Isointensity Hypointensity | 5 (71%) 2 (29%) 0 (0%) | 32 (78%) 8 (20%) 1 (2%) | 0.68 | 7 (70%) 2 (20%) 1 (10%) | 9 (90%) 0 (0%) 1 (10%) | 0.72 |
| CET1WI | Hyperintensity | 7 (100%) | 41 (100%) | NA | 10 (100%) | 10 (100%) | NA |
| DWI | Hyperintensity Isointensity Hypointensity | 6 (86%) 1 (14%) 0 (0%) | 33 (80%) 5 (12%) 3 (7%) | >0.99 | 10 (100%) 0 (0%) 0 (0%) | 8 (80%) 1 (10%) 1 (10%) | 0.47 |
| Nodal Metastasis From HPV-Positive OPSCC | Nodal Metastasis From HPV-Negative OPSCC | |||||
|---|---|---|---|---|---|---|
| Recurrence | p | Recurrence | p | |||
| Yes (n = 24) | No (n = 96) | Yes (n = 24) | No (n = 6) | |||
| Maximum diameter (mm) | 17.8 [14.0–22.5] | 16.8 [13.5–22.0] | 0.15 | 18.5 [15.3–26.5] | 19.3 [16.5–22.3] | 0.83 |
| CT (HU) | ||||||
| UECT | 44.1 [38.6–47.9] | 47.1 [44.4–51.6] | 0.01 | 45.6 [42.8–48.8] | 41.2 [34.3–47.1] | 0.27 |
| CECT | 82.2 [71.5–96.7] | 86.2 [75.4–98.4] | 0.53 | 79.4 [68.2–84.3] | 87.9 [86.8–95.6] | 0.03 |
| Necrosis of NCCT | 38.3 [31.4–41.0] | 33.6 [27.2–44.2] | 0.45 | 31.4 [25.8–40.2] | 28.3 [27.5–34.0] | 0.82 |
| Necrosis of CECT | 49.0 [36.8–66.5] (n = 13) | 42.3 [33.2–55.5] (n = 62) | 0.28 | 39.3 [29.8–47.0] (n = 17) | 33.9 [31.4–56.6] (n = 5) | 0.65 |
| MRI | ||||||
| SIR on T1WI | 1.00 [0.93–1.04] | 0.97 [0.90–1.02] | 0.14 | 0.94 [0.89–1.02] | 0.89 [0.87–0.93] | 0.35 |
| SIR on T2WI | 1.09 [0.96–1.36] | 1.12 [0.99–1.32] | 0.69 | 1.23 [0.95–1.37] | 1.31 [1.15–1.47] | 0.16 |
| SIR on DWI | 1.43 [1.12–1.62] | 1.47 [1.19–1.83] | 0.67 | 1.49 [1.18–1.72] | 1.50 [1.45–2.11] | 0.44 |
| SIR on CE-T1WI | 1.90 [1.74–2.04] | 1.79 [1.57–2.03] | 0.17 | 1.79 [1.64–2.08] | 2.41 [1.97–2.38] | 0.04 |
| ADC value (×10−3 mm2/s) | 0.87 [0.68–0.99] | 0.86 [0.76–1.05] | 0.34 | 0.83 [0.72–1.02] | 1.13 [0.99–1.37] | 0.06 |
| 18F-FDG-PET/CT | ||||||
| SUVmax | 9.52 [5.91–12.7] | 7.78 [4.51–11.0] | 0.28 | 7.86 [4.40–15.5] | 4.31 [3.78–4.78] | 0.07 |
| Nodal Metastasis From HPV-Positive OPSCC | Nodal Metastasis From HPV-Negative OPSCC | ||||||
|---|---|---|---|---|---|---|---|
| Recurrence | p | Recurrence | p | ||||
| Yes (n = 24) | No (n = 96) | Yes (n = 24) | No (n = 9) | ||||
| CT | |||||||
| ENE | 2 (8%) | 8 (8%) | >0.99 | 1 (4%) | 4 (44%) | 0.01 | |
| Unenhanced area
- pure cystic - pure cystic + mural nodule - necrosis | 12 (50%) 4 (17%) 1 (4%) 7 (29%) | 62 (65%) 7 (7%) 14 (15%) 41 (43%) | 0.24 0.15 | 17 (71%) 3 (13%) 4 (17%) 10 (42%) | 6 (67%) 2 (22%) 0 (0%) 4 (44%) | >0.99 0.55 | |
| MRI | |||||||
| ENE | 2 (8%) | 8 (8%) | >0.99 | 1 (4%) | 4 (44%) | 0.01 | |
| Unenhanced area
- pure cystic - pure cystic + mural nodule - necrosis | 18 (75%) 5 (21%) 3 (13%) 10 (42%) | 64 (67%) 5 (5%) 14 (15%) 46 (48%) | 0.48 0.08 | 18 (75%) 4 (17%) 3 (13%) 10 (42%) | 8 (89%) 1 (11%) 1 (11%) 6 (67%) | 0.64 0.72 | |
| Solid component | |||||||
| T1WI | Hyperintensity Isointensity Hypointensity | 0 (0%) 15 (63%) 9 (37%) | 0 (0%) 40 (42%) 56 (58%) | 0.11 | 3 (13%) 12 (50%) 9 (37%) | 1 (11%) 2 (22%) 6 (67%) | 0.35 |
| T2WI | Hyperintensity Isointensity Hypointensity | 12 (50%) 11 (46%) 1 (4%) | 59 (61%) 30 (31%) 7 (7%) | 0.50 | 16 (67%) 7 (29%) 1 (4%) | 5 (56%) 3 (33%) 1 (11%) | 0.70 |
| DWI | Hyperintensity Isointensity Hypointensity | 20 (83%) 4 (17%) 0 (0%) | 85 (89%) 9 (9%) 2 (2%) | 0.55 | 21 (88%) 2 (8%) 1 (4%) | 7 (78%) 2 (22%) 0 (0%) | 0.68 |
| CE-T1WI | Hyperintensity Isointensity Hypointensity | 24 (100%) 0 (0%) 0 (0%) | 95 (99%) 1 (1%) 0 (0%) | >0.99 | 24 (100%) 0 (0%) 0 (0%) | 9 (100%) 0 (0%) 0 (0%) | NA |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Suto, T.; Kawaguchi, M.; Kato, H.; Shibata, H.; Ogawa, T.; Ando, T.; Noda, Y.; Hyodo, F.; Matsuo, M. Imaging Findings of Human Papillomavirus-Positive and Human Papillomavirus-Negative Oropharyngeal Squamous Cell Carcinoma Associated with Recurrence. J. Clin. Med. 2025, 14, 1027. https://doi.org/10.3390/jcm14031027
Suto T, Kawaguchi M, Kato H, Shibata H, Ogawa T, Ando T, Noda Y, Hyodo F, Matsuo M. Imaging Findings of Human Papillomavirus-Positive and Human Papillomavirus-Negative Oropharyngeal Squamous Cell Carcinoma Associated with Recurrence. Journal of Clinical Medicine. 2025; 14(3):1027. https://doi.org/10.3390/jcm14031027
Chicago/Turabian StyleSuto, Taketo, Masaya Kawaguchi, Hiroki Kato, Hirofumi Shibata, Takenori Ogawa, Tomohiro Ando, Yoshifumi Noda, Fuminori Hyodo, and Masayuki Matsuo. 2025. "Imaging Findings of Human Papillomavirus-Positive and Human Papillomavirus-Negative Oropharyngeal Squamous Cell Carcinoma Associated with Recurrence" Journal of Clinical Medicine 14, no. 3: 1027. https://doi.org/10.3390/jcm14031027
APA StyleSuto, T., Kawaguchi, M., Kato, H., Shibata, H., Ogawa, T., Ando, T., Noda, Y., Hyodo, F., & Matsuo, M. (2025). Imaging Findings of Human Papillomavirus-Positive and Human Papillomavirus-Negative Oropharyngeal Squamous Cell Carcinoma Associated with Recurrence. Journal of Clinical Medicine, 14(3), 1027. https://doi.org/10.3390/jcm14031027






