Evaluation of Thrombomodulin, Heart-Type Fatty-Acid-Binding Protein, Pentraxin-3 and Galectin-3 Levels in Patients with Myocardial Infarction, with and Without ST Segment Elevation
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Considerations
2.2. Subjects
2.3. Inclusion Criteria
2.4. Exclusion Criteria
2.5. Blood Collection
2.6. Assessment of Serum Thrombomodulin (TM) Levels
2.7. Assessment of Serum Heart-Fatty-Acid-Binding Protein (H-FABP) Levels
2.8. Measurement of Serum Pentraxin 3 (PTX-3) Levels
2.9. Measurement of Serum Galectin-3 (Gal-3) Levels
2.10. Statistical Analysis
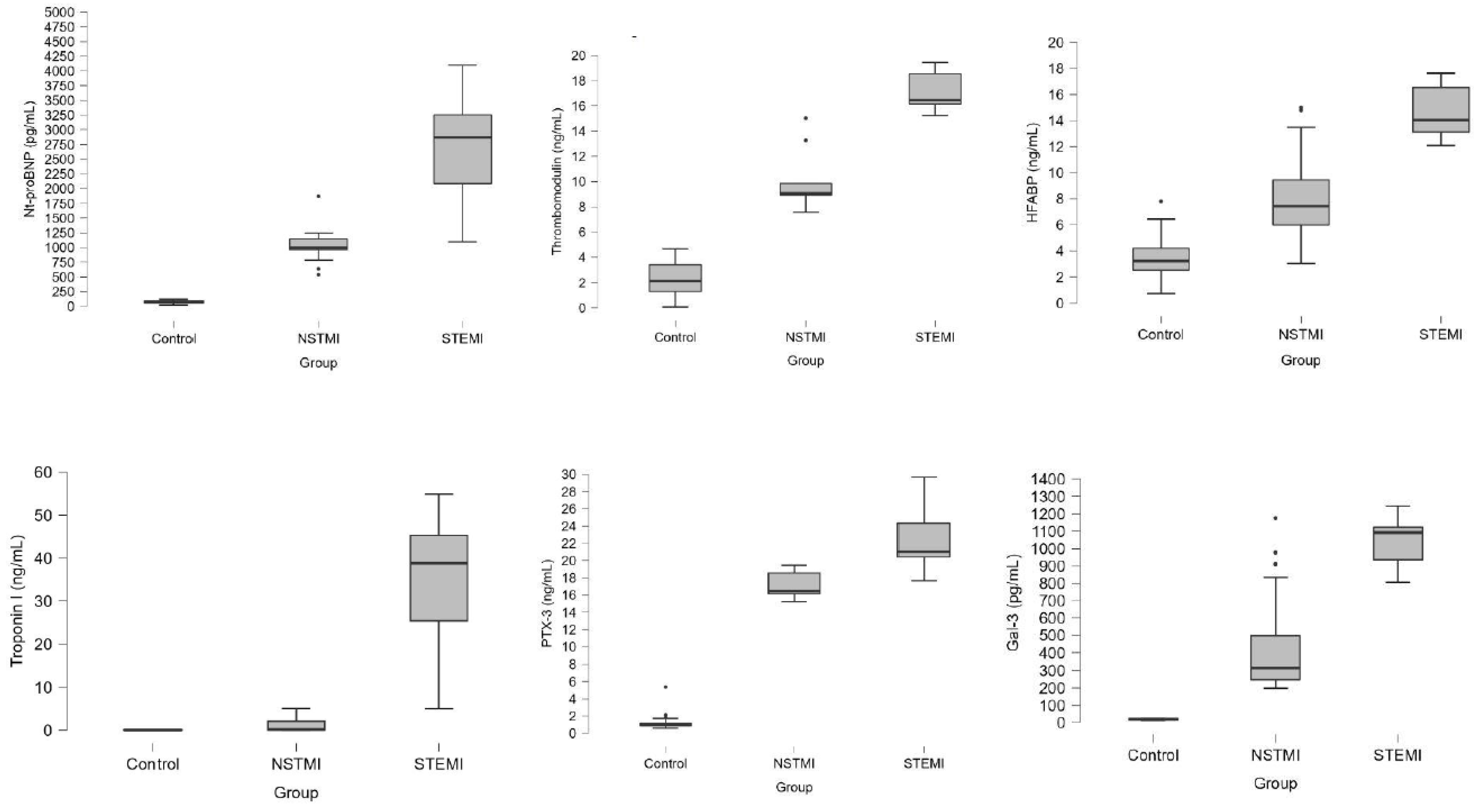
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lu, L.; Liu, M.; Sun, R.; Zheng, Y.; Zhang, P. Myocardial Infarction: Symptoms and Treatments. Cell Biochem. Biophys. 2015, 72, 865–867. [Google Scholar] [CrossRef]
- Hedayati, T.; Yadav, N.; Khanagavi, J. Non– ST-Segment Acute Coronary Syndromes. Cardiol. Clin. 2018, 36, 37–52. [Google Scholar] [CrossRef]
- Shavadia, J.S.; Alemayehu, W.; Defilippi, C.; Westerhout, C.M.; Tromp, J.; Granger, C.B.; Armstrong, P.W.; van Diepen, S. Novel multi-marker proteomics in phenotypically matched patients with ST-segment myocardial infarction: Association with clinical outcomes. J. Thromb. Thrombolysis 2022, 53, 841–850. [Google Scholar] [CrossRef] [PubMed]
- Cai, X.; Shi, J.; Xu, Y.; Fu, L.; Feng, X.; Zhao, R. An important diagnostic marker of acute myocardial infarction patients: Plasma miRNA133 levels. Medicine 2024, 103, e38781. [Google Scholar] [CrossRef]
- Liu, G.; Huang, L.; Lv, X.; Guan, Y.; Li, L. Thrombomodulin as a potential diagnostic marker of acute myocardial infarction and correlation with immune infiltration: Comprehensive analysis based on multiple machine learning. Transpl. Immunol. 2024, 85, 102070. [Google Scholar] [CrossRef] [PubMed]
- Jameson, J.L.; Fauci, A.S.; Kasper, D.L.; Hauser, S.L.; Longo, D.L.; Loscalzo, J. Harrison’s Principles of Internal Medicine, 20th ed.; Cenveo® Publisher Services: Stamford, CT, USA, 2018; p. 1505. [Google Scholar]
- Van Dreden, P.; Rousseau, A.; Savoure, A.; Lenormand, B.; Fontaine, S.; Vasse, M. Plasma thrombomodulin activity, tissue factor activity and high levels of circulating procoagulant phospholipid as prognostic factors for acute myocardial infarction. Blood Coagul. Fibrinolysis 2009, 20, 635–641. [Google Scholar] [CrossRef] [PubMed]
- Kondo, T.; Takahashi, M.; Yamasaki, G.; Sugimoto, M.; Kuse, A.; Morichika, M.; Nakagawa, K.; Sakurada, M.; Asano, M.; Ueno, Y. Immunohistochemical analysis of thrombomodulin expression in myocardial tissue from autopsy cases of ischemic heart disease. Leg. Med. 2021, 51, 101897. [Google Scholar] [CrossRef] [PubMed]
- Dogra, R.; Das, R.; Ahluwalia, J.; Kumar, R.M.; Talwar, K.K. Association of thrombomodulin gene polymorphisms and plasma thrombomodulin levels with acute myocardial infarction in north Indian patients. Clin. Appl. Thromb. Hemost. 2013, 19, 637–643. [Google Scholar] [CrossRef]
- Glatz, J.F.; van der Vusse, G.J.; Simoons, M.L.; A Kragten, J.; van Dieijen-Visser, M.; Hermens, W.T. Fatty acid binding protein and the early detection of acute myocardial infarction. Clin. Chim. Acta 1998, 272, 87–92. [Google Scholar] [CrossRef]
- Van Nieuwenhoven, F.A.; Kleine, A.H.; Wodzig, K.W.H.; Hermens, W.T.; Kragten, H.A.; Maessen, J.G.; Punt, C.D.; Van Dieijen, M.P.; Van Der Vusse, G.J.; Glatz, J.F. Discrimination between myocardial and skeletal muscle injury by assesment of the plasma ratio of myoglobin over fatty acid binding protein. Circulation 1995, 92, 2848–2854. [Google Scholar] [CrossRef]
- Xu, L.Q.; Yang, Y.M.; Tong, H.; Xu, C.F. Early diagnostic performance of heart-type fatty acid binding protein in suspected acute myocardial infarction: Evidence from a meta-analysis of contemporary studies. Heart Lung Circ. 2018, 27, 503–512. [Google Scholar] [CrossRef] [PubMed]
- Glatz, J.F.C.; Renneberg, R. Added value of H-FABP as plasma biomarker for the early evaluation of suspected acute coronary syndrome. Clin. Lipidol. 2014, 9, 205–220. [Google Scholar] [CrossRef]
- Tanaka, T.; Hirota, Y.; Sohmiya, K.; Nishimura, S.; Kawamura, K. Serum and urinary human heart fatty acid-binding protein in acute myocardial infarction. Clin. Biochem. 1991, 24, 195–201. [Google Scholar] [CrossRef] [PubMed]
- Mantovani, A.; Garlanda, C.; Bottazzi, B. Pentraxin 3, a non-redundant soluble pattern recognition receptor involved in innate immunity. Vaccine 2003, 21 (Suppl. S2), S43–S47. [Google Scholar] [CrossRef] [PubMed]
- Savchenko, A.; Imamura, M.; Ohashi, R.; Jiang, S.; Kawasaki, T.; Hasegawa, G.; Emura, I.; Iwanari, H.; Sagara, M.; Tanaka, T.; et al. Expression of pentraxin 3 (PTX3) in human atherosclerotic lesions. J. Pathol. 2008, 215, 48–55. [Google Scholar] [CrossRef]
- Peri, G.; Introna, M.; Corradi, D.; Iacuitti, G.; Signorini, S.; Avanzini, F.; Pizzetti, F.; Maggioni, A.P.; Moccetti, T.; Metra, M.; et al. PTX3, A prototypical long pentraxin, is an early indicator of acute myocardial infarction in humans. Circulation 2000, 102, 636–641. [Google Scholar] [CrossRef]
- Yu, L.; Ruifrok, W.P.; Meissner, M.; Bos, E.M.; Van Goor, H.; Sanjabi, B.; Van Der Harst, P.; Pitt, B.; Goldstein, I.J.; Koerts, J.A.; et al. Genetic and pharmacological inhibition of galectin-3 prevents cardiac remodeling by interfering with myocardial fibrogenesis. Circ. Heart Fail. 2013, 6, 107–117. [Google Scholar] [CrossRef]
- Lok, D.J.; Lok, S.I.; Bruggink-Andre de la Porte, P.W.; Badings, E.; Lipsic, E.; van Wijngaarden, J.; de Boer, R.A.; van Veldhuisen, D.J.; van der Meer, P. Galectin-3 is an independent marker for ventricular remodeling and mortality in patients with chronic heart failure. Clin. Res. Cardiol. 2013, 102, 103–110. [Google Scholar] [CrossRef]
- Asleh, R.; Enriquez-Sarano, M.; Jaffe, A.S.; Manemann, S.M.; Weston, S.A.; Jiang, R.; Roger, V.L. Galectin-3 Levels and Outcomes After Myocardial Infarction: A Population-Based Study. J. Am. Coll. Cardiol. 2019, 73, 2286–2295. [Google Scholar] [CrossRef]
- Demirtas, A.O.; Karabag, T.; Demirtas, D. Ischemic Modified Albumin Predicts Critical Coronary Artery Disease in Unstable Angina Pectoris and Non-STElevation Myocardial Infarction. J. Clin. Med. Res. 2018, 10, 570–575. [Google Scholar] [CrossRef]
- Liu, J.; Ren, Y.G.; Zhang, L.H.; Tong, Y.W.; Kang, L. Serum salusin-β levels are associated with the presence and severity of coronary artery disease. J. Investig. Med. 2015, 63, 632–635. [Google Scholar] [CrossRef]
- Thygesen, K.; Alpert, J.S.; Jaffe, A.S.; Chaitman, B.R.; Bax, J.J.; Morrow, D.A.; White, H.D.; Executive Group on behalf of the Joint European Society of Cardiology (ESC)/American College of Cardiology (ACC)/American Heart Association (AHA)/World Heart Federation (WHF) Task Force for the Universal Definition of Myocardial Infarction. Fourth Universal Definition of Myocardial Infarction. Circulation 2018, 138, e618–e651. [Google Scholar] [CrossRef] [PubMed]
- Pushkov, A.A.; Blagodatskikh, K.A.; Nikitin, A.G.; IuV, A.; Brovkin, A.N.; Chudakova, D.A.; Evdokimova, M.A.; OIu, A.; Osmolovskaia, V.S.; Minushkina, L.O.; et al. Polymorphic markers Ala455Val of the THBD gene and Arg353Gln of the F7 gene and association with unfavorable outcomes of coronary atherosclerosis in patients with a history of acute ischemic heart disease. Genetika 2011, 47, 1386–1392. [Google Scholar] [CrossRef] [PubMed]
- Tsiourantani, F.; Koutouzis, M.; Pouliakis, A.; Terpos, E.; Gialeraki, A.; Politou, M. Hemostasis Disorders in Coronary Artery Disease: A Prospective Comparative Study of 130 Patients. Georgian Med. News 2022, 332, 12–21. [Google Scholar]
- Pavel, A.L.; Kundnani, N.R.; Morariu, S.; Tudor, A.; Man, D.E.; Duda-Seiman, D.M.; Velimirovici, D.E.; Valcovici, M.D.; Calin, P.; Dragan, S.R. Importance of H-FABP in Early Diagnosis of Acute Myocardial Infarction. Int. J. Gen. Med. 2024, 17, 4335–4346. [Google Scholar] [CrossRef]
- Chmurzyńska, A. The multigene family of fatty acid-binding proteins (FABPs): Function, structure and polymorphism. J. Appl. Genet. 2006, 47, 39–48. [Google Scholar] [CrossRef]
- Ye, X.-D.; He, Y.; Wang, S.; Wong, G.T.; Irwin, M.G.; Xia, Z. Heart-type fatty acid binding protein (H-FABP) as a biomarker for acute myocardial injury and long-term post-ischemic prognosis. Acta Pharmacol. Sin. 2018, 39, 1155–1163. [Google Scholar] [CrossRef]
- Isailă, O.-M.; Ion, O.M.; Luta, R.; Catinas, R.; Ionita, A.; Haisan, D.; Hostiuc, S. Postmortem Immunohistochemical Findings in Early Acute Myocardial Infarction: A Systematic Review. Int. J. Mol. Sci. 2024, 25, 7625. [Google Scholar] [CrossRef]
- Befekadu, R.; Grenegård, M.; Larsson, A.; Christensen, K.; Ramström, S. Dynamic Changes in Pentraxin-3 and Neprilysin in ST Segment Elevation Myocardial Infarction. Biomedicines 2022, 10, 275. [Google Scholar] [CrossRef]
- Jenny, N.S.; Arnold, A.M.; Kuller, L.H.; Tracy, R.P.; Psaty, B.M. Associations of pentraxin 3 with cardiovascular disease and all-cause death: The Cardiovascular Health Study. Arterioscler. Thromb. Vasc. Biol. 2009, 29, 594–599. [Google Scholar] [CrossRef]
- Napoleone, E.; Di Santo, A.; Peri, G.; Mantovani, A.; De Gaetano, G.; Donati, M.B.; Lorenzet, R. The long pentraxin PTX3 up-regulates tissue factor in activated monocytes: Another link between inflammation and clotting activation. J. Leukoc. Biol. 2004, 76, 203–209. [Google Scholar] [CrossRef] [PubMed]
- Helseth, R.; Solheim, S.; Opstad, T.; Hoffmann, P.; Arnesen, H.; Seljeflot, I. The time profile of Pentraxin 3 in patients with acute ST-elevation myocardial infarction and stable angina pectoris undergoing percutaneous coronary intervention. Mediat. Inflamm. 2014, 2014, 608414. [Google Scholar] [CrossRef]
- Haibo, L.; Xiaofang, G.; Chunming, W.; Jie, Y.; Guozhong, C.; Limei, Z.; Yong, C.; Yu, F.; Yingchun, B.; Wangjun, Y.; et al. Prognostic value of plasma pentraxin-3 levels in patients with stable coronary artery disease after drug-eluting stent implantation. Mediat. Inflamm. 2014, 2014, 963096. [Google Scholar] [CrossRef] [PubMed]
- Guo, R.; Li, Y.; Wen, J.; Li, W.; Xu, Y. Elevated plasma level of pentraxin-3 predicts in-hospital and 30-day clinical outcomes in patients with non-ST-segment elevation myocardial infarction who have undergone percutaneous coronary intervention. Cardiology 2014, 129, 178–188. [Google Scholar] [CrossRef]
- Firouzjahi, A.; Eris, S.; Jalali, S.F.; Bijani, A.; Ranaee, M. Evaluation of Serum Pentraxin-3 Level in Patients with Acute Myocardial Infarction Compared with Control Group. Iran. J. Pathol. 2021, 16, 243–247. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Yuan, Y.; Guo, K.; Lao, Y.; Huang, X.; Feng, L. Value of Galectin-3 in Acute Myocardial Infarction. Am. J. Cardiovasc. Drugs 2020, 20, 333–342. [Google Scholar] [CrossRef] [PubMed]
- Berezin, A.E.; Berezin, A.A. Adverse Cardiac Remodelling after Acute Myocardial Infarction: Old and New Biomarkers. Dis. Markers 2020, 2020, 1215802. [Google Scholar] [CrossRef]
- Meijers, W.C.; van der Velde, A.R.; Pascual-Figal, D.A.; de Boer, R.A. Galectin-3 and post-myocardial infarction cardiac remodeling. Eur. J. Pharmacol. 2015, 763 Pt A, 115–121. [Google Scholar] [CrossRef]
- Sygitowicz, G.; Maciejak-Jastrzębska, A.; Sitkiewicz, D. The Diagnostic and therapeutic potential of galectin-3 in cardiovascular diseases. Biomolecules 2021, 12, 46. [Google Scholar] [CrossRef]
- Di Tano, G.; Caretta, G.; De Maria, R.; Bettari, L.; Parolini, M.; Testa, S.; Pirelli, S. Galectin-3 and outcomes after anterior-wall myocardial infarction treated by primary percutaneous coronary intervention. Biomark. Med. 2018, 12, 21–26. [Google Scholar] [CrossRef]
- Vucic, R.M.; Andrejic, O.M.; Stokanovic, D.; Stoimenov, T.J.; McClements, L.; Nikolic, V.N.; Sreckovic, M.; Veselinovic, M.; Aleksandric, S.; Popadic, V.; et al. Galectin-3 as a Prognostic Biomarker in Patients with First Acute Myocardial Infarction without Heart Failure. Diagnostics 2023, 13, 3348. [Google Scholar] [CrossRef]
- Karakasis, P.; Fragakis, N.; Kouskouras, K.; Karamitsos, T.; Patoulias, D.; Rizzo, M. Sodium-Glucose Cotransporter-2 Inhibitors in Patients With Acute Coronary Syndrome: A Modern Cinderella? Clin. Ther. 2024, 46, 841–850. [Google Scholar] [CrossRef] [PubMed]
- Mitsis, A.; Gragnano, F. Myocardial Infarction with and without ST-segment Elevation: A Contemporary Reappraisal of Similarities and Differences. Curr. Cardiol. Rev. 2021, 17, e230421189013. [Google Scholar] [CrossRef] [PubMed]
- Montalescot, G.; Van’t Hof, A.W.; Lapostolle, F.; Silvain, J.; Lassen, J.F.; Bolognese, L.; Cantor, W.J.; Cequier, Á.; Chettibi, M.; Goodman, S.G.; et al. Prehospital ticagrelor in ST-segment elevation myocardial infarction. N. Engl. J. Med. 2014, 371, 1016–1027. [Google Scholar] [CrossRef] [PubMed]
- Dörler, J.; Edlinger, M.; Alber, H.F.; Altenberger, J.; Benzer, W.; Grimm, G.; Huber, K.; Pachinger, O.; Schuchlenz, H.; Siostrzonek, P.; et al. Clopidogrel pre-treatment is associated with reduced in-hospital mortality in primary percutaneous coronary intervention for acute ST-elevation myocardial infarction. Eur. Heart J. 2011, 32, 2954–2961. [Google Scholar] [CrossRef]
- Möckel, M. The new ESC acute coronary syndrome guideline and its impact in the CPU and emergency department setting. Die neue ESC-Leitlinie zum akuten Koronarsyndrom und ihre Auswirkungen auf die Chest Pain Unit und zentrale Notaufnahme. Herz 2024, 49, 185–189. [Google Scholar] [CrossRef]
| Group | |||||||
|---|---|---|---|---|---|---|---|
| Control | NSTMI | STEMI | |||||
| n | % | n | % | n | % | p Value | |
| Sex | |||||||
| Female | 52 | 57.8% | 42 | 46.7% | 40 | 44.4% | 0.159 |
| Male | 38 | 42.2% | 48 | 53.3% | 50 | 55.6% | |
| Smoking | 0 | 0.0% | 22 | 24.4% | 60 | 66.7% | <0.001 |
| Alcohol | 0 | 0.0% | 17 | 18.9% | 17 | 18.9% | <0.001 |
| Co-morbidity | 0 | 0.0% | 46 | 51.1% | 55 | 61.1% | <0.001 |
| Diabetes mellitus (DM) | 0 | 0.0% | 19 | 21.1% | 45 | 50.0% | <0.001 |
| Hypertension (HT) | 0 | 0.0% | 44 | 48.9% | 49 | 54.4% | <0.001 |
| Cardiovascular complications | 0 | 0.0% | 9 | 10.0% | 12 | 13.3% | 0.002 |
| Control (n:90) | NSTEMI (n:90) | STEMI (n:90) | p Value | |
|---|---|---|---|---|
| Age (Year) | 58.22 ± 8.11 | 59.36 ± 7.74 | 58.81 ± 9.27 | 0.664 |
| BMI (kg/m2) | 24.03 ± 1.39 a | 26.9 ± 3.76 b | 27.18 ± 3.36 b | <0.001 |
| SBP (mmHg) | 125 (120–129) a | 135 (130–155) b | 145 (144–155) c | <0.001 |
| DBP (mmHg) | 74.5 (68–75) a | 83.5 (78–86) b | 82.5 (77–95) | <0.001 |
| Pulse (bpm) | 78 (72–80) a | 75 (66–80) a | 80 (77–88) b | <0.001 |
| Fasting blood glucose (FBG) (mg/dL) | 93 (86–96) a | 91.5 (85–100) a | 109.5 (91–141) b | <0.001 |
| HbA1c (%) | 5.2 (5.1–5.5) a | 5.7 (5.1–5.8) b | 6 (5.6–7.9) c | <0.001 |
| T. cholesterol (mg/dL) | 165.5 (150–184) a | 196 (180–222) b | 235 (184–243) b | <0.001 |
| LDL (mg/dL) | 91.5 (83–102) a | 100 (85–112) a | 150 (124–182) b | <0.001 |
| HDL (mg/dL) | 45 (36–49) a | 39 (34–45) b | 36 (30–40) c | <0.001 |
| Triglycerid (mg/dL) | 96 (78–114) a | 120 (79–139) b | 119 (96–150) b | <0.001 |
| Fibrinogen (g/L) | 2.89 (2.44–3.4) a | 5.2 (4.2–5.57) b | 4.99 (4.63–5.9) b | <0.001 |
| High-sensitivity troponin (hs-TnI) (ng/mL) | 0.05 (0.04–0.07) a | 0.21 (0.07–2.13) b | 38.77 (24.65–45.36) c | <0.001 |
| Creatin kinase -MB (CK-MB) (ng/mL) | 14.4 (11.55–18.6) a | 87.64 (82.03–92.07) b | 257 (200–395) c | <0.001 |
| C-Reactive Protein (CRP) (mg/L) | 2.7 (2.51–3.23) a | 17.55 (9.48–22.6) b | 19.75 (11.97–32.02) b | <0.001 |
| NT-proBNP (pg/mL) | 74 (59–96) a | 998 (963–1152) b | 2869 (2086–3254) c | <0.001 |
| Thrombomodulin (TM) (ng/mL) | 2.12 (1.23–3.45) a | 9.06 (8.92–9.86) b | 16.45 (16.15–18.56) c | <0.001 |
| Heart-type fatty-acid-binding protein (H-FABP) (ng/mL) | 3.23 (2.51–4.23) a | 7.42 (5.9–9.45) b | 14.04 (13.12–16.54) c | <0.001 |
| Pentraxin-3 (PTX-3) (ng/mL) | 0.98 (0.85–1.2) a | 16.45 (16.15–18.56) b | 21.03 (20.42–24.32) c | <0.001 |
| Galectin-3 (Gal-3) (pg/mL) | 19.23 (16.23–23.1) a | 313.8 (245.65–498.45) b | 1092.78 (936.75–1124.02) c | <0.001 |
| Control | NSTEMI | STEMI | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| NT-proBNP | TM | H-FABP | PTX-3 | Gal-3 | NT-proBNP | TM | H-FABP | PTX-3 | Gal-3 | Nt-proBNP | TM | H-FABP | PTX-3 | Gal-3 | ||
| NT-proBNP (pg/mL) | r | −0.137 | −0.081 | −0.067 | 0.134 | 0.053 | −0.039 | 0.081 | 0.042 | 0.961 | 0.891 | 0.915 | 0.979 | |||
| p | 0.196 | 0.446 | 0.532 | 0.209 | 0.621 | 0.716 | 0.450 | 0.696 | <0.001 | <0.001 | <0.001 | <0.001 | ||||
| TM (ng/mL) | r | −0.153 | 0.076 | −0.074 | −0.005 | 0.044 | 0.048 | 0.861 | 0.870 | 0.950 | ||||||
| p | 0.150 | 0.478 | 0.490 | 0.963 | 0.680 | 0.652 | <0.001 | <0.001 | <0.001 | |||||||
| H-FABP (ng/mL) | r | 0.048 | −0.031 | 0.151 | 0.082 | 0.866 | 0.892 | |||||||||
| p | 0.651 | 0.769 | 0.156 | 0.442 | <0.001 | <0.001 | ||||||||||
| PTX-3 (ng/mL) | r | −0.128 | 0.065 | 0.950 | ||||||||||||
| p | 0.228 | 0.541 | <0.001 | |||||||||||||
| hs-Tn I (ng/mL) | r | −0.061 | −0.133 | −0.110 | 0.025 | −0.017 | −0.056 | 0.006 | −0.052 | 0.029 | −0.084 | 0.010 | −0.019 | −0.017 | −0.062 | −0.026 |
| p | 0.569 | 0.211 | 0.301 | 0.816 | 0.873 | 0.599 | 0.954 | 0.623 | 0.789 | 0.433 | 0.925 | 0.857 | 0.875 | 0.563 | 0.811 | |
| Variable(s) | AUC | 95% CI for AUC | p Value | Cut-Off | Sensitivity | Specificity | |
|---|---|---|---|---|---|---|---|
| C vs. ST | Nt_proBNP (pg/mL) | 1.000 | 1–1 | <0.001 | 125 | 100% | 100% |
| Thrombomodulin (ng/mL) | 1.000 | 1–1 | <0.001 | 5 | 100% | 100% | |
| HFABP (ng/mL) | 1.000 | 1–1 | <0.001 | 10 | 100% | 100% | |
| PTX-3 (ng/mL) | 1.000 | 1–1 | <0.001 | 5.5 | 100% | 100% | |
| Gal-3 (pg/mL) | 1.000 | 1–1 | <0.001 | 30 | 100% | 100% | |
| Troponin I | 1.000 | 1–1 | <0.001 | 0.10 | 100% | 100% | |
| CK-MB | 1.000 | 1–1 | <0.001 | 30 | 100% | 100% | |
| C vs. NST | Nt_proBNP (pg/mL) | 1.000 | 1–1 | <0.001 | 125 | 100% | 100% |
| Thrombomodulin (ng/mL) | 1.000 | 1–1 | <0.001 | 5 | 100% | 100% | |
| HFABP (ng/mL) | 0.922 | 0.884–0.959 | <0.001 | 4.75 | 93.3% | 78.9% | |
| PTX-3 (ng/mL) | 1.000 | 1–1 | <0.001 | 5.5 | 100% | 100% | |
| Gal-3 (pg/mL) | 1.000 | 1–1 | <0.001 | 30 | 100% | 100% | |
| Troponin I | 0.779 | 0.699–0.860 | <0.001 | 0.10 | 71.1% | 100% | |
| CK-MB | 1.000 | 1–1 | <0.001 | 30 | 100% | 100% | |
| NST vs. ST | Nt_proBNP (pg/mL) | 0.966 | 0.944–0.989 | <0.001 | 1250 | 88.89% | 98.89% |
| Thrombomodulin (ng/mL) | 1.000 | 1–1 | <0.001 | 15 | 100% | 100% | |
| HFABP (ng/mL) | 0.926 | 0.885–0.66 | <0.001 | 10 | 100.00% | 85.56% | |
| PTX-3 (ng/mL) | 0.953 | 0.924–0.981 | <0.001 | 19.5 | 86.67% | 100.00% | |
| Gal-3 (pg/mL) | 0.981 | 0.961–1 | <0.001 | 600 | 100.00% | 94.44% | |
| Troponin I | 1.000 | 0.999–1 | <0.001 | 5 | 100% | 98.9% | |
| CK-MB | 1.000 | 1–1 | <0.001 | 110 | 100% | 100% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Misirlioglu, N.F.; Orucoglu, G.G.; Bıcakhan, B.; Kucuk, S.H.; Himmetoglu, S.; Sayili, S.B.; Ozen, G.D.; Uzun, H. Evaluation of Thrombomodulin, Heart-Type Fatty-Acid-Binding Protein, Pentraxin-3 and Galectin-3 Levels in Patients with Myocardial Infarction, with and Without ST Segment Elevation. J. Clin. Med. 2025, 14, 1015. https://doi.org/10.3390/jcm14031015
Misirlioglu NF, Orucoglu GG, Bıcakhan B, Kucuk SH, Himmetoglu S, Sayili SB, Ozen GD, Uzun H. Evaluation of Thrombomodulin, Heart-Type Fatty-Acid-Binding Protein, Pentraxin-3 and Galectin-3 Levels in Patients with Myocardial Infarction, with and Without ST Segment Elevation. Journal of Clinical Medicine. 2025; 14(3):1015. https://doi.org/10.3390/jcm14031015
Chicago/Turabian StyleMisirlioglu, Naile Fevziye, Gulbahar Guler Orucoglu, Burcu Bıcakhan, Suat Hayri Kucuk, Solen Himmetoglu, Sena Baykara Sayili, Gulenay Defne Ozen, and Hafize Uzun. 2025. "Evaluation of Thrombomodulin, Heart-Type Fatty-Acid-Binding Protein, Pentraxin-3 and Galectin-3 Levels in Patients with Myocardial Infarction, with and Without ST Segment Elevation" Journal of Clinical Medicine 14, no. 3: 1015. https://doi.org/10.3390/jcm14031015
APA StyleMisirlioglu, N. F., Orucoglu, G. G., Bıcakhan, B., Kucuk, S. H., Himmetoglu, S., Sayili, S. B., Ozen, G. D., & Uzun, H. (2025). Evaluation of Thrombomodulin, Heart-Type Fatty-Acid-Binding Protein, Pentraxin-3 and Galectin-3 Levels in Patients with Myocardial Infarction, with and Without ST Segment Elevation. Journal of Clinical Medicine, 14(3), 1015. https://doi.org/10.3390/jcm14031015






