Applications of 3D Printing and Virtual Modeling in the Assessment of Visceral and Renal Artery Aneurysms
Abstract
1. Introduction
2. Materials and Methods
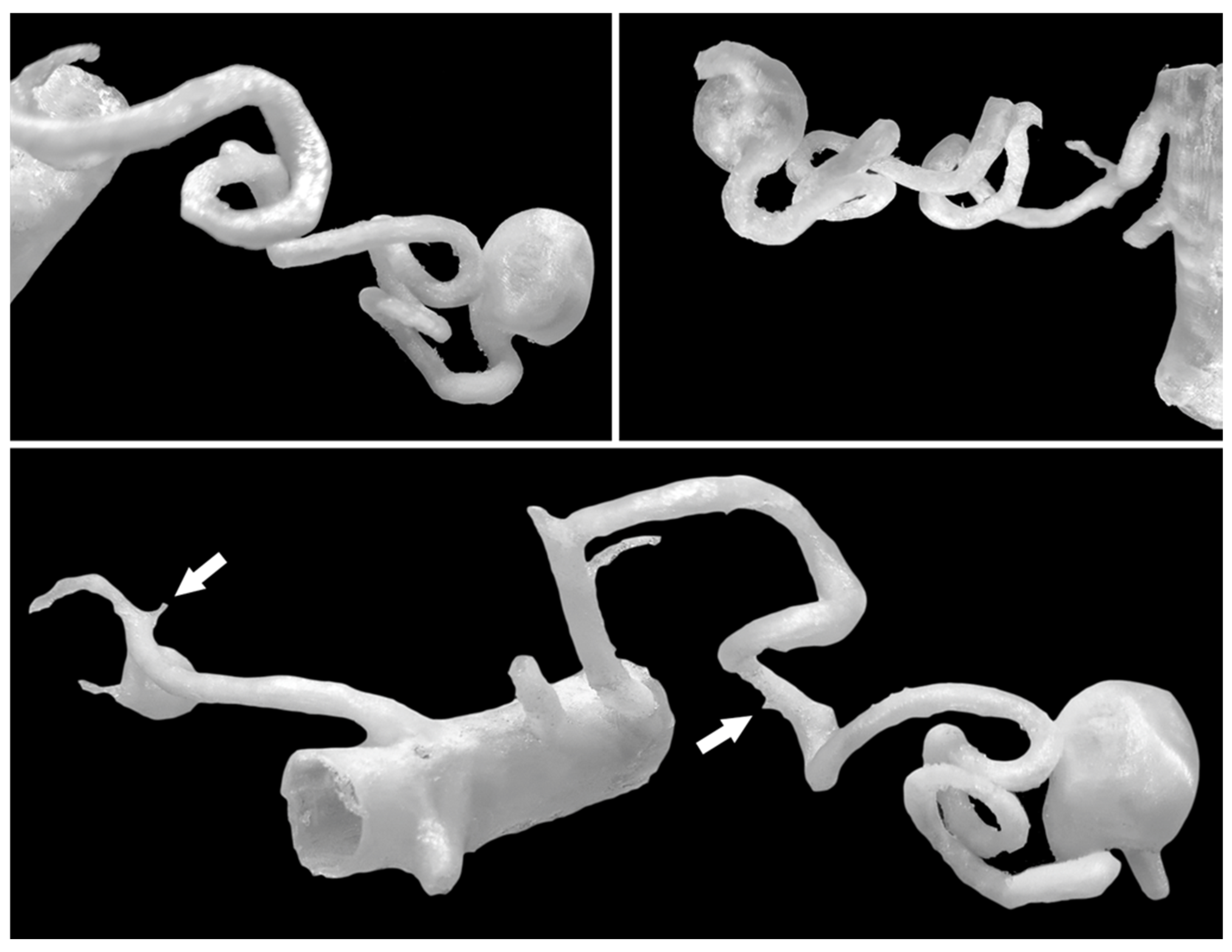
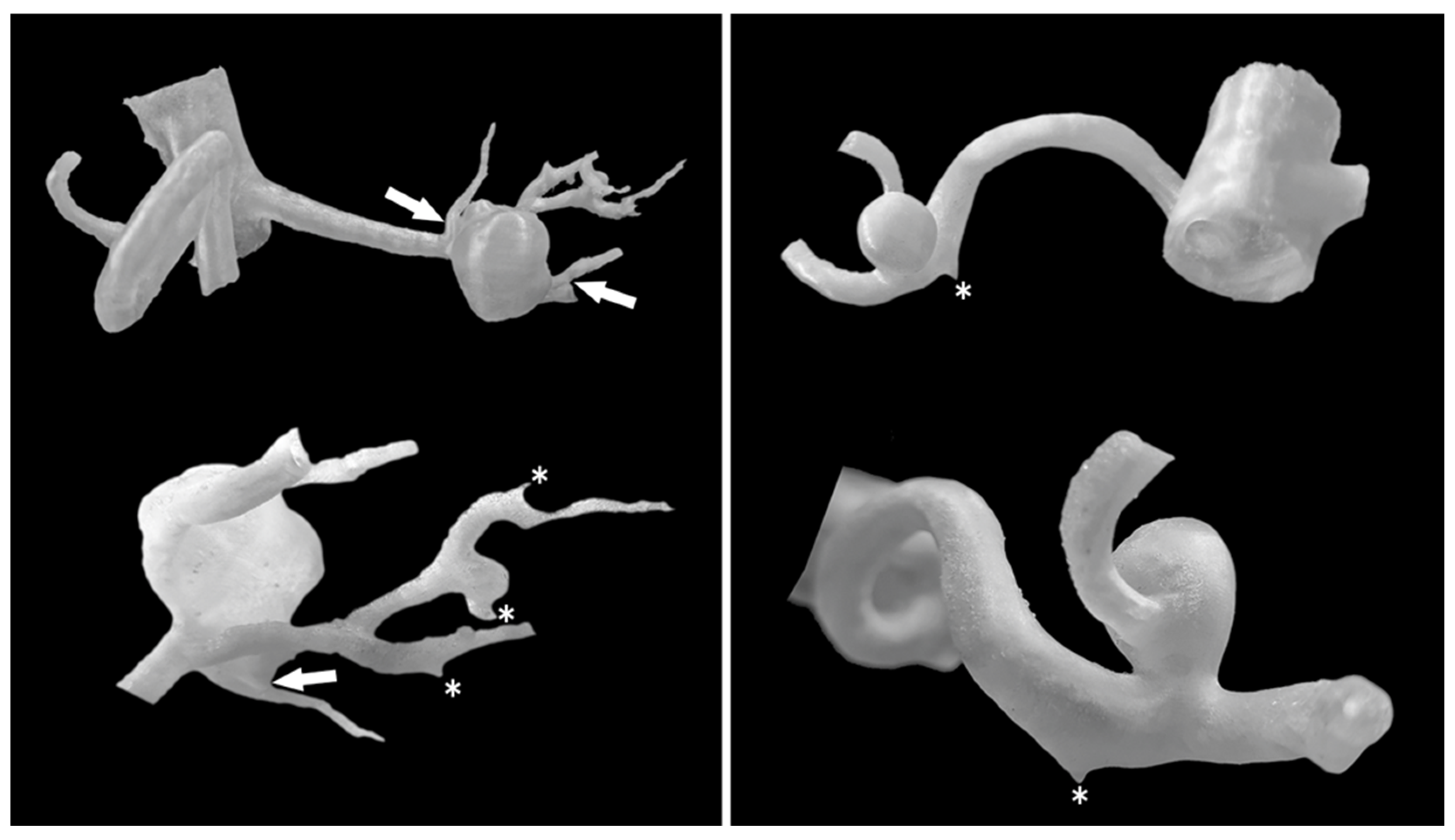
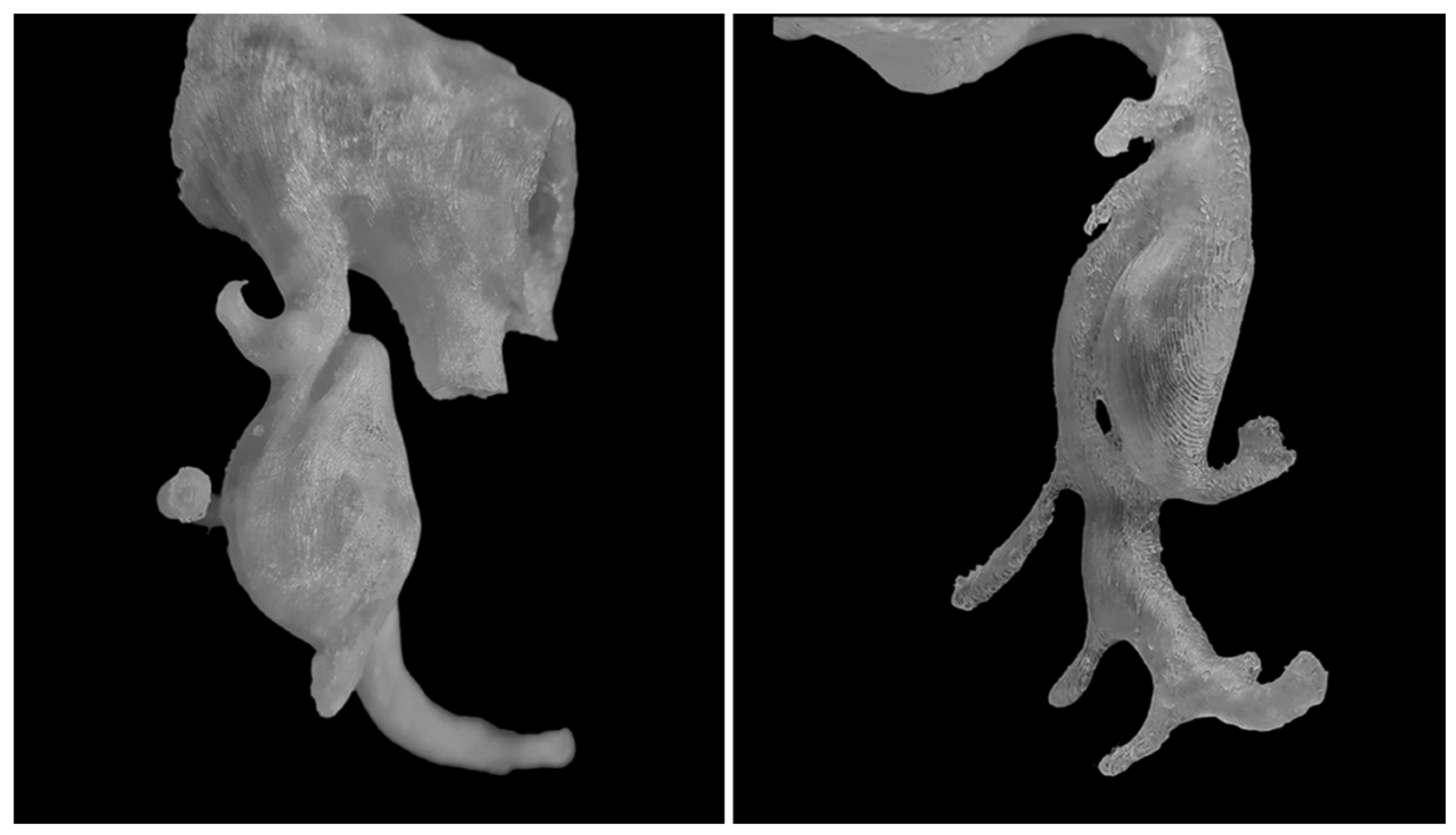
3. Results
4. Discussion
Technical and Clinical Limitations in Medical 3D Printing
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| N/A | Not Applicable |
| 3D printing | Three-Dimensional Printing |
| AA | Abdominal Aorta |
| CHA | Common Hepatic Artery |
| CHAA | Common Hepatic Artery Aneurysm |
| CIA | Common Iliac Artery |
| CT | Celiac Trunk |
| CTA | Computed Tomography Angiography |
| FFF | Fused Filament Fabrication |
| GDA | Gastroduodenal Artery |
| HAA | Hepatic Artery Aneurysm |
| HA | Hepatic Artery |
| IPDA | Inferior Pancreaticoduodenal Artery |
| LGA | Left Gastric Artery |
| LGEAA | Left Gastroepiploic Artery Aneurysm |
| LHA | Left Hepatic Artery |
| LRA | Left Renal Artery |
| MALS | Median Arcuate Ligament Syndrome |
| RA | Renal Artery |
| RAA | Renal Artery Aneurysm |
| RAAs | Renal Artery Aneurysms |
| RHA | Right Hepatic Artery |
| RRA | Right Renal Artery |
| RRAA | Right Renal Artery Aneurysm |
| SA | Splenic Artery |
| SAA | Splenic Artery Aneurysm |
| SMA | Superior Mesenteric Artery |
| SPDA | Superior Pancreaticoduodenal Artery |
| VAAs | Visceral Artery Aneurysms |
References
- Marconi, S.; Pugliese, L.; Botti, M.; Peri, A.; Cavazzi, E.; Latteri, S.; Auricchio, F.; Pietrabissa, A. Value of 3D printing for the comprehension of surgical anatomy. Surg. Endosc. 2017, 31, 4102–4110. [Google Scholar] [CrossRef]
- Meyer-Szary, J.; Luis, M.S.; Mikulski, S.; Patel, A.; Schulz, F.; Tretiakow, D.; Fercho, J.; Jaguszewska, K.; Frankiewicz, M.; Pawłowska, E.; et al. The Role of 3D Printing in Planning Complex Medical Procedures and Training of Medical Professionals—Cross-Sectional Multispecialty Review. Int. J. Environ. Res. Public Health 2022, 19, 3331. [Google Scholar] [CrossRef]
- Salazar, D.; Thompson, M.; Rosen, A.; Zuniga, J. Using 3D Printing to Improve Student Education of Complex Anatomy: A Systematic Review and Meta-analysis. Med. Sci. Educ. 2022, 32, 1209–1218. [Google Scholar] [CrossRef] [PubMed]
- Körfer, D.; Grond-Ginsbach, C.; Hakimi, M.; Böckler, D.; Erhart, P. Arterial Aneurysm Localization Is Sex-Dependent. J. Clin. Med. 2022, 11, 2450. [Google Scholar] [CrossRef] [PubMed]
- Vougadiotis, I.; Karampelias, V.; Chrysikos, D.; Antonopoulos, I.; Solia, E.; Spanidis, Y.; Tsakotos, G.; Troupis, T. Anatomical Variations in the Celiac Trunk: A Short Review. Acta Medica Acad. 2023, 52, 134–141. [Google Scholar] [CrossRef] [PubMed]
- dos Santos, P.V.; Barbosa, A.B.M.; Targino, V.A.; Silva, N.d.A.; Silva, Y.C.d.M.; Barbosa, F.; Oliveira, A.d.S.B.; Assis, T.d.O. Anatomical Variations of the Celiac Trunk: A Systematic Review. Arq. Bras. Cir. Dig. 2018, 31, e1403. [Google Scholar] [CrossRef]
- Wang, T.; Wang, J.; Zhao, J.; Yuan, D.; Huang, B. Endovascular Treatment of Aberrant Splenic Artery Aneurysm Presenting with Painless Progressive Jaundice: A Case Report and Literature Review. Vasc. Endovasc. Surg. 2021, 55, 756–760. [Google Scholar] [CrossRef]
- Pandey, S.; Bhattacharya, S.; Mishra, R.N.; Shukla, V. Anatomical variations of the splenic artery and its clinical implications. Clin. Anat. 2004, 17, 497–502. [Google Scholar] [CrossRef]
- Manatakis, D.K.; Piagkou, M.; Loukas, M.; Tsiaoussis, J.; Delis, S.G.; Antonopoulos, I.; Chytas, D.; Natsis, K. A systematic review of splenic artery variants based on cadaveric studies. Surg. Radiol. Anat. 2021, 43, 1337–1347. [Google Scholar] [CrossRef]
- Hekimoglu, A.; Ergun, O. Evaluation of renal vascular variations with computed tomography. Afr. J. Urol. 2022, 28, 21. [Google Scholar] [CrossRef]
- Lareyre, F.; Raffort, J.; Carboni, J.; Chikande, J.; Massiot, N.; Voury-Pons, A.; Umbdenstock, E.; Hassen-Khodja, R.; Jean-Baptiste, E. Impact of Polar Renal Artery Coverage after Fenestrated Endovascular Aortic Repair for Juxtarenal and Type IV Thoracoabdominal Aortic Aneurysms. Ann. Vasc. Surg. 2019, 58, 45–53.e1. [Google Scholar] [CrossRef] [PubMed]
- Szczurowska, A.; Guziński, M.; Sobczyk, P.; Silicki, J.; Sąsiadek, M. The analysis of renal artery cross-section area and kidney volume in computed tomography angiography. Folia Morphol. 2020, 79, 93–97. [Google Scholar] [CrossRef]
- Mihaylova, E.; Groudeva, V.; Nedevska, M. Multidetector computed tomography angiography study of the renal arterial vasculature anatomy and its variations in a Bulgarian adult population. Surg. Radiol. Anat. 2023, 45, 289–296. [Google Scholar] [CrossRef] [PubMed]
- Delasotta, L.A.; Olivieri, B.; Malik, A.; Nguyen, C.; Bhatia, V.; Burke, W. Thoracic renal artery: A rare variant. A case study and literature review. Surg. Radiol. Anat. 2015, 37, 561–564. [Google Scholar] [CrossRef]
- Panagouli, E.; Venieratos, D.; Lolis, E.; Skandalakis, P. Variations in the anatomy of the celiac trunk: A systematic review and clinical implications. Ann. Anat. Anat. Anz. 2013, 195, 501–511. [Google Scholar] [CrossRef]
- Mashiko, T.; Otani, K.; Kawano, R.; Konno, T.; Kaneko, N.; Ito, Y.; Watanabe, E. development of three-dimensional hollow elastic model for cerebral aneurysm clipping simulation enabling rapid and low cost prototyping. World Neurosurg. 2015, 83, 351–361. [Google Scholar] [CrossRef]
- Jeising, S.; Liu, S.; Blaszczyk, T.; Rapp, M.; Beez, T.; Cornelius, J.F.; Schwerter, M.; Sabel, M. Combined use of 3D printing and mixed reality technology for neurosurgical training: Getting ready for brain surgery. Neurosurg. Focus 2024, 56, E12. [Google Scholar] [CrossRef]
- Rorden, C.; McCormick, M.; Hanayik, T.; Masoud, M.; Plis, S.M. brain2print AI powered web tool for creating 3D printable brain models. Sci. Rep. 2025, 15, 15664. [Google Scholar] [CrossRef]
- Stana, J.; Grab, M.; Kargl, R.; Tsilimparis, N. 3D printing in the planning and teaching of endovascular procedures. Radiologie 2022, 62, 28–33. [Google Scholar] [CrossRef]
- Langridge, B.; Momin, S.; Coumbe, B.; Woin, E.; Griffin, M.; Butler, P. Systematic Review of the Use of 3-Dimensional Printing in Surgical Teaching and Assessment. J. Surg. Educ. 2019, 75, 209–221. [Google Scholar] [CrossRef]
- Soliński, D.G.; Celer, M.; Dyś, K.; Witkiewicz, W.; Wiewióra, M. 3D printing in the endovascular treatment of visceral artery aneurysms. Medicine 2023, 102, e35844. [Google Scholar] [CrossRef] [PubMed]
- Shibata, E.; Takao, H.; Amemiya, S.; Ohtomo, K.; Abe, O. Embolization of visceral arterial aneurysms: Simulation with 3D-printed models. Vascular 2020, 28, 259–266. [Google Scholar] [CrossRef] [PubMed]
- Takao, H.; Amemiya, S.; Shibata, E.; Ohtomo, K. 3D Printing of Preoperative Simulation Models of a Splenic Artery Aneurysm: Precision and Accuracy. Acad. Radiol. 2017, 24, 650–653. [Google Scholar] [CrossRef] [PubMed]
- Soliński, D.G.; Celer, M.; Dyś, K.; Wiewióra, M. 3D printing in the preoperative planning and endovascular treatment of splenic artery aneurysm. Own clinical experience and literature review. Videosurgery Other Miniinvasive Tech. 2022, 17, 110–115. [Google Scholar] [CrossRef]
- Shibata, E.; Takao, H.; Amemiya, S.; Ohtomo, K. 3D-Printed Visceral Aneurysm Models Based on CT Data for Simulations of Endovascular Embolization: Evaluation of Size and Shape Accuracy. AJR Am. J. Roentgenol. 2017, 209, 243–247. [Google Scholar] [CrossRef]
- Mari, F.S.; Nigri, G.; Pancaldi, A.; De Cecco, C.N.; Gasparrini, M.; Dall’oGlio, A.; Pindozzi, F.; Laghi, A.; Brescia, A. Role of CT angiography with three-dimensional reconstruction of mesenteric vessels in laparoscopic colorectal resections: A randomized controlled trial. Surg. Endosc. 2013, 27, 2058–2067. [Google Scholar] [CrossRef]
- Chen, Y.; Bian, L.; Zhou, H.; Wu, D.; Xu, J.; Gu, C.; Fan, X.; Liu, Z.; Zou, J.; Xia, J.; et al. Usefulness of three-dimensional printing of superior mesenteric vessels in right hemicolon cancer surgery. Sci. Rep. 2020, 10, 11660. [Google Scholar] [CrossRef]
- Lin, J.C.; Myers, E. Three-dimensional printing for preoperative planning of renal artery aneurysm surgery. J. Vasc. Surg. 2016, 64, 810. [Google Scholar] [CrossRef]
- Holzem, K.M.; Jayarajan, S.; Zayed, M.A. Surgical planning with three-dimensional printing of a complex renal artery aneurysm. J. Vasc. Surg. Cases Innov. Tech. 2018, 4, 19. [Google Scholar] [CrossRef]

| No. | Sex | Age | Aneurysm Location/Morphology | Diameter (mm) of the Aneurysm Sac (Angio-CT) | Diameter (mm) of the Aneurysm Sac (3D Printed Model) | Diameter Dimensional Deviation (mm) | Diameter (mm) of the Artery Before and After the Aneurysm Sac | Additional Information and Anatomical Vascular Variants |
|---|---|---|---|---|---|---|---|---|
| 1. | F | 58 | SAA in the splenic hilum with 2 branches, complicated morphology of the aneurysm | 20 | 20.25 | 0.25 | 4/3 | N/A |
| 2. | F | 62 | SAA, the tortuous course of the SA, wide neck of the aneurysm sac | 18 | 17.67 | 0.33 | 4/5 | The LGA originates from the AA superior to the CT. The RHA arises from the SMA. an additional LRA originates from the AA. |
| SAA in the splenic hilum, branch of SA | 3 | N/A | N/A | N/A | ||||
| 3. | F | 42 | SAA, the tortuous course of the SA, wide neck of the aneurysm sac | 25 | 24.92 | 0.08 | 6/7 | N/A |
| SAA in the splenic hilum | 4 | N/A | N/A | N/A | ||||
| 4. | F | 55 | SAA on the SA division with branches, in the splenic hilum | 19 | 19.33 | 0.33 | 5/N/A | The RHA arises from the SMA. |
| LGEAA with marginal calcifications and mural thrombi | 13 | 13.37 | 0.37 | 4/N/A | ||||
| 5. | M | 52 | SAA on SA trunk | 25 | 24.73 | 0.27 | 7/7 | Additional upper pole LRA. High division of the RRA. |
| 6. | F | 82 | SAA, largest saccular aneurysm of the SA trunk with a wide neck | 15 | 15.02 | 0.02 | 7/10 | Well-defined marginal calcification of aneurysm sacs. |
| SAA in the splenic hilum | 16 | 16.26 | 0.26 | 3/N/A | ||||
| SAA in the splenic hilum | 9 | 9.34 | 0.34 | 3/3 | ||||
| 7. | F | 65 | SAA, largest aneurysm on the distal main SA trunk with mural thrombus up to 3 mm and calcifications | 18 | 18.02 | 0.02 | 4/5 | Additional lower pole LRA. |
| SAA on SA trunk | 5 | 4.94 | 0.06 | N/A | ||||
| SAA in the splenic hilum | 11 | 11.1 | 0.1 | 3/N/A | ||||
| SAA in the splenic hilum | 13 | 13.29 | 0.29 | 4/4 | ||||
| 8. | F | 49 | SAA on the SA division in the splenic hilum | 11 | 10.87 | 0.13 | 4/N/A | CHA originates from the SMA. Dissection of distal AA extending to the left CIA. |
| 9. | F | 46 | SAA in the splenic hilum | 16 | 15.88 | 0.12 | 4/N/A | N/A |
| 10. | F | 34 | SAA, saccular aneurysm in the distal SA segment with two branching vessels | 16 | 16.25 | 0.25 | 5/3 | Isolated origin of the LGA from the aorta |
| 11. | F | 57 | SAA, saccular aneurysm in the distal SA segment with marginal calcifications | 19 | 19.42 | 0.42 | 4/4 | Highly tortuous SA. RHA arises from the SMA. LHA is noted from the CT. GDA is noted from the CT. |
| RAA of a RRA branch | 10 | 9.95 | 0.05 | N/A | ||||
| 12. | M | 65 | SAA of one branch of the SA, in the splenic hilum, with a wide neck, well-calcified wall with small, mural thrombi | 9 | 9.48 | 0.48 | 2.5/3 | N/A |
| 13. | F | 30 | SAA in the splenic hilum, distal SA segment, with several small branches | 24 | 23.82 | 0.18 | 3.5/N/A | Additional upper pole RRA and LRA. |
| SAA of an SA branch, in splenic hilum | 6 | N/A | N/A | N/A | ||||
| 14. | M | 71 | SAA in the proximal SA segment with calcifications and small mural thrombi | 21 | 21.13 | 0.13 | 4/4 | Highly tortuous course of the distal SA segment. |
| 15. | M | 40 | LRAA in the left renal hilum, complicated morphology | 27 | 27.29 | 0.29 | 6/5 | N/A |
| 16. | M | 68 | RAA on the RRA division with 2 branches | 17 | 17.28 | 0.28 | 4/N/A | N/A |
| 17. | F | 46 | RRAA on a RA division with 3 branches | 16 | 16.1 | 0.1 | N/A | N/A |
| RRAA of main RA trunk | 9 | 9.36 | 0.36 | 5/N/A | ||||
| CT dilatation with CT dissection | 16 | N/A | N/A | N/A | ||||
| 18. | F | 46 | LRAA in the renal hilum at the main trunk division, 3 segmental branches | 17 | 17.58 | 0.58 | 4/N/A | N/A |
| 19. | M | 33 | LRAA on the main LRA trunk branch, 2 segmental branches | 19 | 19.2 | 0.2 | 5/N/A | N/A |
| 20. | M | 74 | RRAA on the main trunk branch | 12 | 12.42 | 0.42 | 8/4 | SA segmentally occluded, distally filled via collateral circulation. |
| SAA, partially thrombosed, in distal SA | 19 | N/A | N/A | N/A | ||||
| 21. | F | 55 | RRAA branch in renal hilum, with several small segmental arteries, aneurysm sac with mural thrombus and calcified atherosclerotic plaques | 10 | 10.32 | 0.32 | 2/N/A | RRA with early division. |
| LRAA on the main trunk branch, with single branch, in renal hilum | 10 | 9.76 | 0.24 | 3/4 | ||||
| 22. | M | 69 | RRAA on the RA division, with 2 branches arising from the sac, calcified plaques and small mural thrombi | 25 | 25.26 | 0.26 | 5/N/A | Post-stentoplasty of the RA—proximal stent end visible in the sac, extending to one branch; stent patent. |
| 23. | M | 44 | HAA in the proximal HA segment constricting the HA | 22 | 22.57 | 0.57 | N/A | MALS |
| Post-stenotic dilatation of the CT | 10 | N/A | N/A | N/A | ||||
| 24. | F | 74 | Multiple dilatations of SPDA and IPDA arteries | 18 | 18.43 | 0.43 | N/A | N/A |
| RRAA | 5 | N/A | N/A | N/A | ||||
| 25. | M | 71 | Aneurysm near the IPDA origin from the SMA, with several jejunal arteries arising from the sac; multiple dilatations of SPDA and IPDA arteries | 34 | 34.4 | 0.4 | 6/6 | CT occluded at origin, subtotally narrowed distally, filled via collateral branches. |
| SAA in the splenic hilum | 8 | N/A | N/A | N/A | ||||
| 26. | F | 55 | Saccular IPDA aneurysm | 14 | 13.92 | 0.08 | 4/2 | CT occluded at origin, subtotally narrowed distally, filled via collateral branches. |
| SAA in the splenic hilum, on SA division | 8 | 8.07 | 0.07 | 4/3 | ||||
| CHAA | 8 | 7.96 | 0.04 | 5/4 | ||||
| Segmental RAA | 13 | 12.94 | 0.06 | 2/N/A | ||||
| 27. | F | 38 | Aneurysm near the IPDA origin from the SMA; several dilatations of SPDA and IPDA arteries | 19 | 19.2 | 0.2 | 4/5 | Severe CT stenosis. |
| 28. | M | 67 | Fusiform, dissecting SMA aneurysm | 14 | 13.82 | 0.18 | 7/6 | Post-treatment of AAA with stent graft. |
| LGA aneurysm | 4.7 | 4.57 | 0.13 | 2/2 | ||||
| 29. | M | 71 | Fusiform CT aneurysm | 15 | 15.03 | 0.03 | 5/5 | Additional lower pole RRA. |
| 30. | M | 62 | Fusiform CT aneurysm proximal to the CT division with the LGA arising from the sac, short-segment CT dissection at the aneurysm neck | 18 | 18.51 | 0.51 | 6/N/A | SA narrow in proximal third, distally occluded; post-splenectomy; high RRA division. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Soliński, D.G.; Wiewióra, H.; Kuczmik, W.; Wiewióra, M. Applications of 3D Printing and Virtual Modeling in the Assessment of Visceral and Renal Artery Aneurysms. J. Clin. Med. 2025, 14, 8915. https://doi.org/10.3390/jcm14248915
Soliński DG, Wiewióra H, Kuczmik W, Wiewióra M. Applications of 3D Printing and Virtual Modeling in the Assessment of Visceral and Renal Artery Aneurysms. Journal of Clinical Medicine. 2025; 14(24):8915. https://doi.org/10.3390/jcm14248915
Chicago/Turabian StyleSoliński, Daniel Grzegorz, Hanna Wiewióra, Wacław Kuczmik, and Maciej Wiewióra. 2025. "Applications of 3D Printing and Virtual Modeling in the Assessment of Visceral and Renal Artery Aneurysms" Journal of Clinical Medicine 14, no. 24: 8915. https://doi.org/10.3390/jcm14248915
APA StyleSoliński, D. G., Wiewióra, H., Kuczmik, W., & Wiewióra, M. (2025). Applications of 3D Printing and Virtual Modeling in the Assessment of Visceral and Renal Artery Aneurysms. Journal of Clinical Medicine, 14(24), 8915. https://doi.org/10.3390/jcm14248915






