Associations Between Maximal Passive Knee Extension and Sagittal Plane Kinematic Patterns in Children with Spastic Cerebral Palsy: A Longitudinal Study
Highlights
- A relatively small limitation of passive knee extension was associated with knee flexion during gait that strengthened with age and was more prominent in bilateral CP
- Knee flexion during gait remained stable over time despite the increasing number of children with knee contractures
- Knee flexion during walking is important to consider for early-stage and effective treatment planning, aiming to prevent possible development of knee contractures in children with bilateral CP
Abstract
1. Introduction
2. Materials and Methods
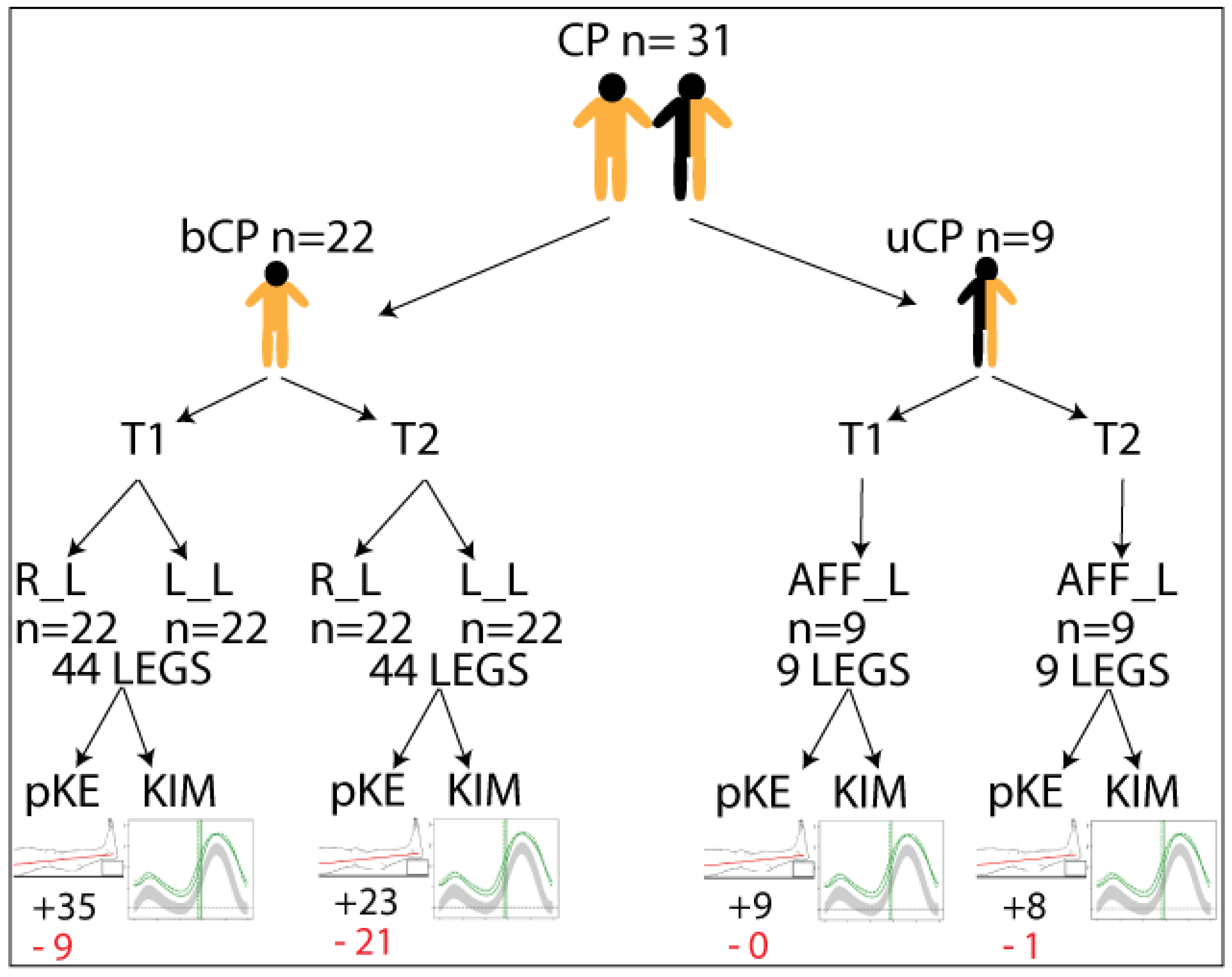
2.1. Participants
2.2. Clinical Examination
2.3. Three-Dimensional Gait Data
2.4. Statistical Analysis
3. Results
3.1. Participants
3.2. Maximal Passive Knee Extension
3.3. Kinematics of the Knee During Gait
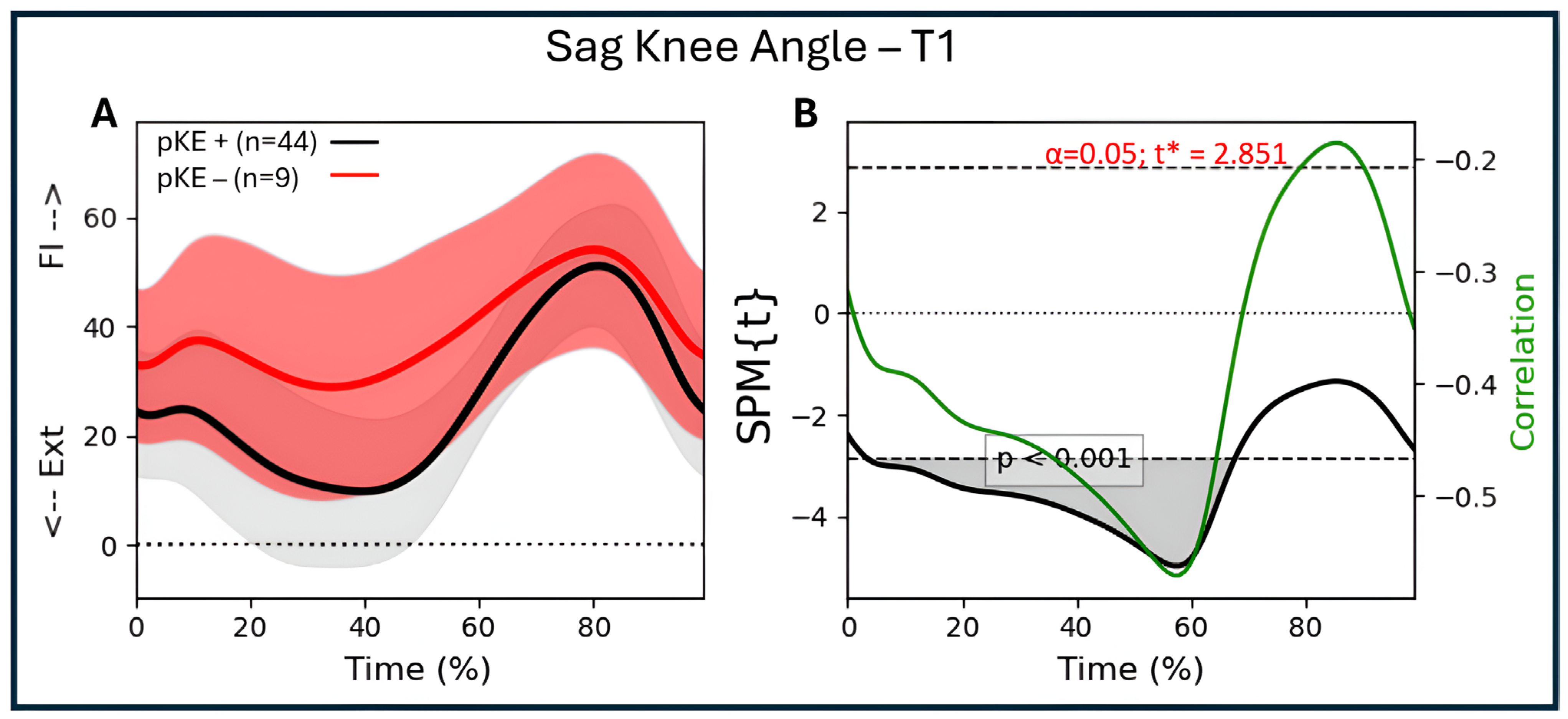
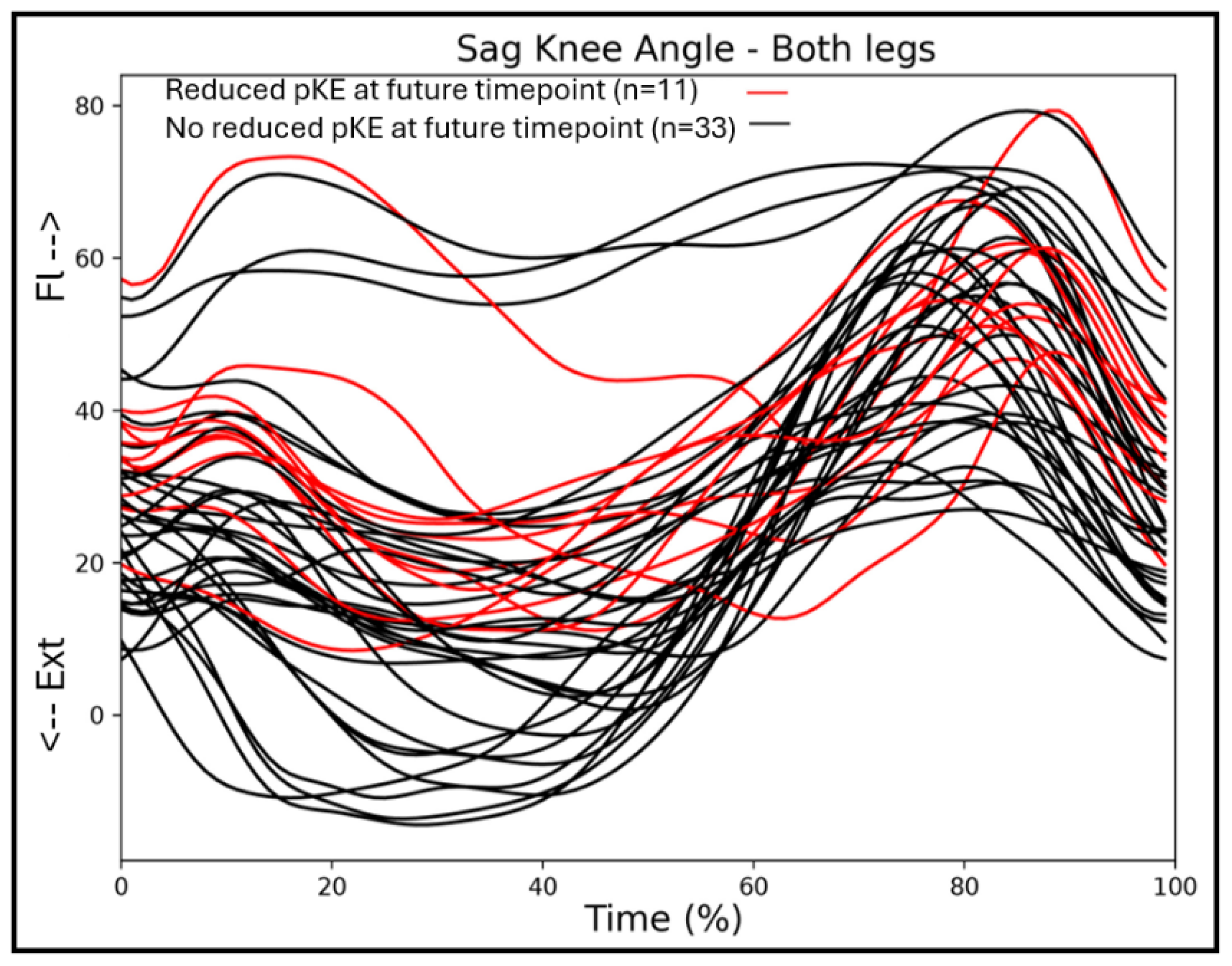
3.4. Associations
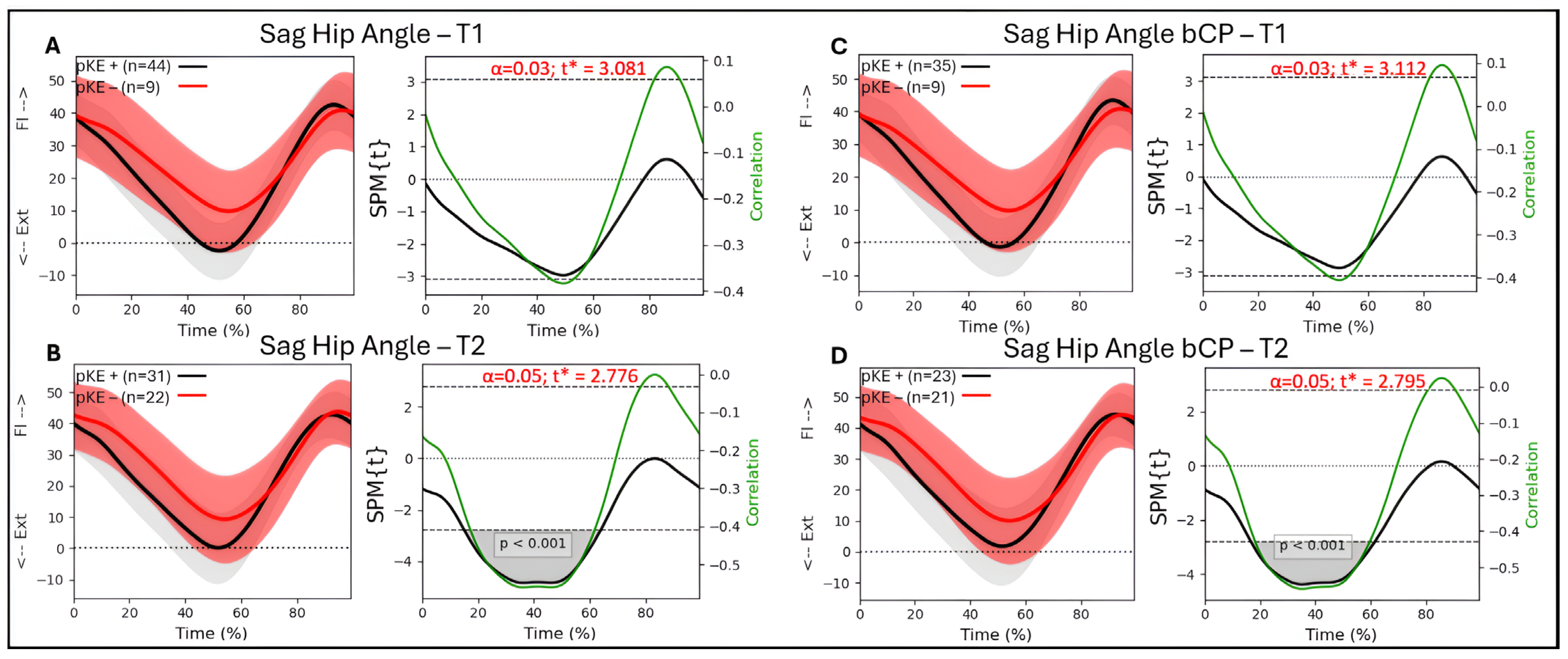
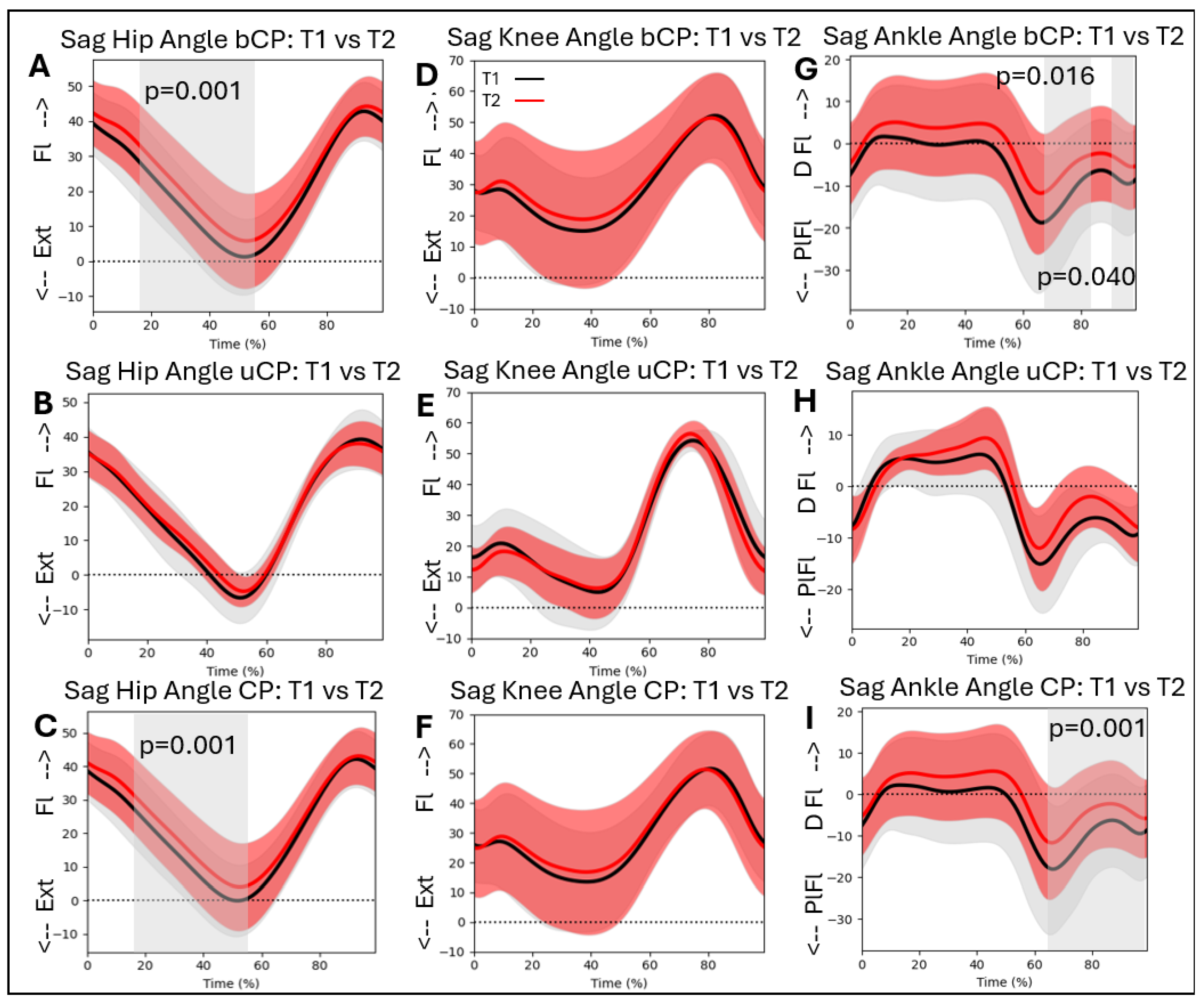
3.5. Associations Between Passive Knee Extension and Hip Kinematics
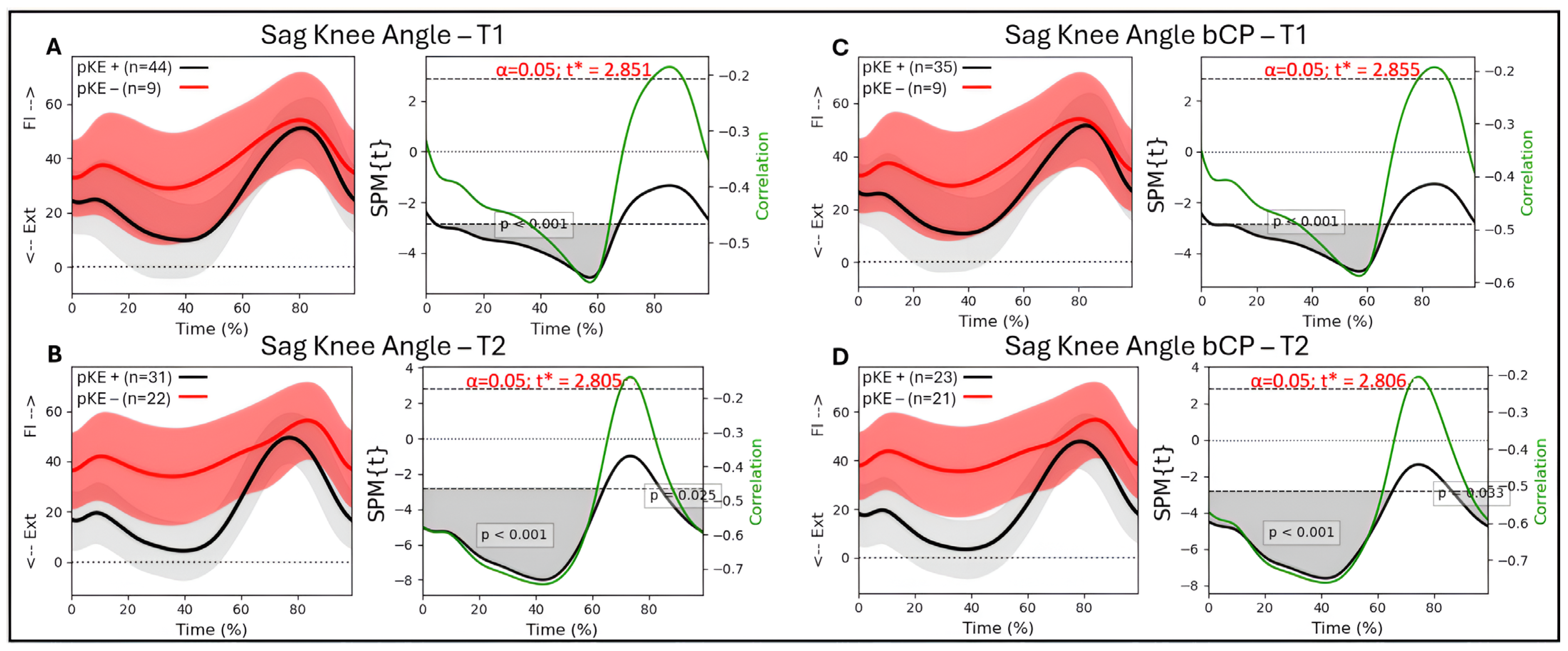
3.6. Associations Between Passive Knee Extension and Knee Kinematics
3.7. Associations Between Passive Knee Extension and Ankle Kinematics
3.8. Kinematic Patterns over Time
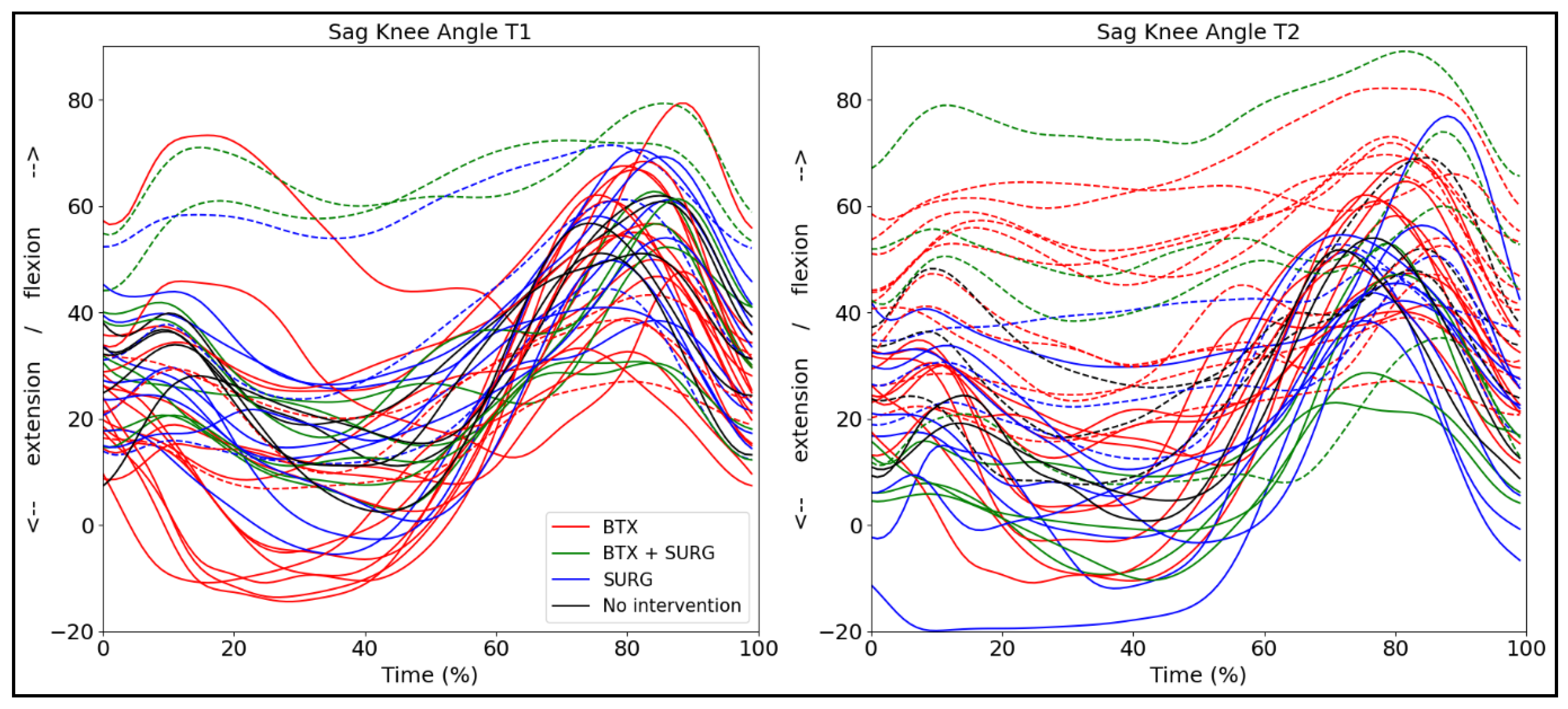
3.9. Kinematic Patterns with Respect to Intervention
4. Discussion
4.1. Associations
4.2. Kinematic Patterns over Time
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CP | Cerebral Palsy |
| SPM | Statistical Parametric Mapping |
| uCP | Unilateral CP |
| bCP | Bilateral CP |
References
- Rosenbaum, P.; Paneth, N.; Leviton, A.; Goldstein, M.; Bax, M.; Damiano, D.; Dan, B.; Jacobsson, B. A report: The definition and classification of cerebral palsy April 2006. Dev. Med. Child Neurol. 2007, 49, 8–14. [Google Scholar] [CrossRef]
- Himmelmann, K.; Beckung, E.; Hagberg, G.; Uvebrant, P. Bilateral spastic cerebral palsy—Prevalence through four decades, motor function and growth. Eur. J. Paediatr. Neurol. 2007, 11, 215–222. [Google Scholar] [CrossRef]
- Cans, C.; Guillem, P.; Baille, F.; Arnaud, C.; Chalmers, J.; Cussen, G.; McManus, V.; Parkes, J.; Dolk, H.; Hagberg, G.; et al. Surveillance of cerebral palsy in Europe: A collaboration of cerebral palsy surveys and registers. Dev. Med. Child Neurol. 2000, 42, 816–824. [Google Scholar] [CrossRef]
- Horber, V.; Fares, A.; Platt, M.J.; Arnaud, C.; Krägeloh-Mann, I.; Sellier, E. Severity of Cerebral Palsy-The Impact of Associated Impairments. Neuropediatrics 2020, 51, 120–128. [Google Scholar] [CrossRef] [PubMed]
- Vameghi, R.; Hoseini, S.A.; Heydarian, S.; Azadeh, H.; Gharib, M. Walking Ability, Participation, and Quality of Life in Children with Spastic Diplegic Cerebral Palsy: A Path Analysis Study. Iran. J. Child. Neurol. 2023, 17, 75–91. [Google Scholar] [CrossRef] [PubMed]
- Larsen, S.M.; Terjesen, T.; Jahnsen, R.B.; Diseth, T.H.; Ramstad, K. Health-related quality of life in adolescents with cerebral palsy; a cross-sectional and longitudinal population-based study. Child Care Health Dev. 2023, 49, 373–381. [Google Scholar] [CrossRef]
- Gómez-Pérez, C.; Vidal Samsó, J.; Puig Diví, A.; Medina Casanovas, J.; Font-Llagunes, J.M.; Martori, J.C. Relationship between spatiotemporal parameters and clinical outcomes in children with bilateral spastic cerebral palsy: Clinical interpretation proposal. J. Orthop. Sci. 2023, 28, 1136–1142. [Google Scholar] [CrossRef]
- Baker, R.; Esquenazi, A.; Benedetti, M.G.; Desloovere, K. Gait analysis: Clinical facts. Eur. J. Phys. Rehabil. Med. 2016, 52, 560–574. [Google Scholar]
- States, R.A.; Salem, Y.; Krzak, J.J.; Godwin, E.M.; McMulkin, M.L.; Kaplan, S.L. Three-Dimensional Instrumented Gait Analysis for Children With Cerebral Palsy: An Evidence-Based Clinical Practice Guideline. Pediatr. Phys. Ther. 2024, 36, 182–206. [Google Scholar] [CrossRef]
- Schwartz, M.H.; Ries, A.J.; Georgiadis, A.G.; Kainz, H. Demonstrating the utility of Instrumented Gait Analysis in the treatment of children with cerebral palsy. PLoS ONE 2024, 19, e0301230. [Google Scholar] [CrossRef] [PubMed]
- Õunpuu, S.; Solomito, M.; Bell, K.; DeLuca, P.; Pierz, K. Long-term outcomes after multilevel surgery including rectus femoris, hamstring and gastrocnemius procedures in children with cerebral palsy. Gait Posture 2015, 42, 365–372. [Google Scholar] [CrossRef]
- Fehlings, D.; Bohn, E.; Switzer, L.; Goldsmith, C.H.; Narayanan, U.; Rosenbaum, P.L.; Wright, F.V.; Foster, G. Three-year outcomes of repeated botulinum neurotoxin A injections to the lower extremities in young children with spastic cerebral palsy in GMFCS levels I to III. Dev. Med. Child Neurol. 2025, in press. [Google Scholar] [CrossRef]
- Pyrzanowska, W.; Chrościńska-Krawczyk, M.; Bonikowski, M. Long-Term Improvement of Gait Kinematics in Young Children with Cerebral Palsy Treated with Botulinum Toxin Injections and Integrated/Intensive Rehabilitation: A 5-Year Retrospective Observational Study. Toxins 2025, 17, 142. [Google Scholar] [CrossRef] [PubMed]
- Papageorgiou, E.; Peeters, N.; Staut, L.; Molenaers, G.; Ortibus, E.; Van Campenhout, A.; Desloovere, K. Botulinum neurotoxin type A responders among children with spastic cerebral palsy: Pattern-specific effects. Eur. J. Paediatr. Neurol. 2024, 49, 131–140. [Google Scholar] [CrossRef]
- Desloovere, K.; Molenaers, G.; Feys, H.; Huenaerts, C.; Callewaert, B.; Van de Walle, P. Do dynamic and static clinical measurements correlate with gait analysis parameters in children with cerebral palsy? Gait Posture 2006, 24, 302–313. [Google Scholar] [CrossRef]
- McMulkin, M.L.; Gulliford, J.J.; Williamson, R.V.; Ferguson, R.L. Correlation of static to dynamic measures of lower extremity range of motion in cerebral palsy and control populations. J. Pediatr. Orthop. 2000, 20, 366–369. [Google Scholar] [CrossRef]
- Maas, J.C.; Huijing, P.A.; Dallmeijer, A.J.; Harlaar, J.; Jaspers, R.T.; Becher, J.G. Decrease in ankle-foot dorsiflexion range of motion is related to increased knee flexion during gait in children with spastic cerebral palsy. J. Electromyogr. Kinesiol. 2015, 25, 339–346. [Google Scholar] [CrossRef]
- Manikowska, F.; Brazevič, S.; Jóźwiak, M.; Lebiedowska, M.K. Contribution of Different Impairments to Restricted Knee Flexion during Gait in Individuals with Cerebral Palsy. J. Pers. Med. 2022, 12, 1568. [Google Scholar] [CrossRef] [PubMed]
- O’Sullivan, R.; French, H.; Horgan, F. A prospective assessment of gait kinematics and related clinical examination measures in cerebral palsy crouch gait. HRB Open Res. 2022, 5, 81. [Google Scholar] [CrossRef] [PubMed]
- Daly, C.; McKeating, H.; Kiernan, D. Age related progression of clinical measures and gait in ambulant children and youth with bilateral cerebral palsy without a history of surgical intervention. Gait Posture 2022, 95, 141–148. [Google Scholar] [CrossRef]
- Pataky, T.C.; Vanrenterghem, J.; Robinson, M.A. The probability of false positives in zero-dimensional analyses of one-dimensional kinematic, force and EMG trajectories. J. Biomech. 2016, 49, 1468–1476. [Google Scholar] [CrossRef]
- Papageorgiou, E.; Simon-Martinez, C.; Molenaers, G.; Ortibus, E.; Campenhout, A.; Desloovere, K. Are spasticity, weakness, selectivity, and passive range of motion related to gait deviations in children with spastic cerebral palsy? A statistical parametric mapping study. PLoS ONE 2019, 14, e0223363. [Google Scholar] [CrossRef]
- Cloodt, E.; Lindgren, A.; Rodby-Bousquet, E. Knee and ankle range of motion and spasticity from childhood into adulthood: A longitudinal cohort study of 3223 individuals with cerebral palsy. Acta Orthop. 2024, 95, 200–205. [Google Scholar] [CrossRef]
- Palisano, R.; Rosenbaum, P.; Walter, S.; Russell, D.; Wood, E.; Galuppi, B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev. Med. Child Neurol. 1997, 39, 214–223. [Google Scholar] [CrossRef] [PubMed]
- British Orthopaedic Association. Joint Motion; Method of Measuring and Recording; British Orthopaedic Association: Edinburgh, UK, 1966. [Google Scholar]
- Davis, R.B.; Õunpuu, S.; Tyburski, D.; Gage, J.R. A gait analysis data collection and reduction technique. Hum. Mov. Sci. 1991, 10, 575–587. [Google Scholar] [CrossRef]
- Fonseca, M.; Gasparutto, X.; Grouvel, G.; Bonnefoy-Mazure, A.; Dumas, R.; Armand, S. Evaluation of lower limb and pelvic marker placement precision among different evaluators and its impact on gait kinematics computed with the Conventional Gait Model. Gait Posture 2023, 104, 22–30. [Google Scholar] [CrossRef]
- Ferrari, A.; Benedetti, M.G.; Pavan, E.; Frigo, C.; Bettinelli, D.; Rabuffetti, M.; Crenna, P.; Leardini, A. Quantitative comparison of five current protocols in gait analysis. Gait Posture 2008, 28, 207–216. [Google Scholar] [CrossRef]
- Hinkle, D.E.; Wiersma, W.; Jurs, S.G. Applied Statistics for the Behavioral Sciences; Houghton Mifflin: Boston, MA, USA, 2003. [Google Scholar]
- Portney, L.G.; Watkins, M.P. Foundations of Clinical Research: Applications to Practice; Pearson/Prentice Hall: London, UK, 2009. [Google Scholar]
- Bartonek, Å.; Lidbeck, C. Knee Flexion While Walking Exceeds Knee Flexion Contracture in Children with Spastic Cerebral Palsy. Children 2023, 10, 1867. [Google Scholar] [CrossRef] [PubMed]
- Papageorgiou, E.; Nieuwenhuys, A.; Vandekerckhove, I.; Van Campenhout, A.; Ortibus, E.; Desloovere, K. Systematic review on gait classifications in children with cerebral palsy: An update. Gait Posture 2019, 69, 209–223. [Google Scholar] [CrossRef] [PubMed]
- Miller, F. Knee Flexion Deformity in Cerebral Palsy. In Cerebral Palsy; Miller, F., Bachrach, S., Lennon, N., O’Neil, M.E., Eds.; Springer International Publishing: Cham, Switzerland, 2020; pp. 2137–2158. [Google Scholar]
- O’Sullivan, R.; Horgan, F.; O’Brien, T.; French, H. The natural history of crouch gait in bilateral cerebral palsy: A systematic review. Res. Dev. Disabil. 2018, 80, 84–92. [Google Scholar] [CrossRef]
- Kanashvili, B.; Niiler, T.A.; Church, C.; Lennon, N.; Shrader, M.W.; Howard, J.J.; Miller, F. The impact of hamstring lengthening on stance knee flexion at skeletal maturity in ambulatory cerebral palsy. J. Pediatr. Orthop. Part B 2025, 34, 320–326. [Google Scholar] [CrossRef]
- Pantzar-Castilla, E.; Chen, B.P.-J.; Miller, F.; Riad, J. The influence of preoperative knee flexion contracture severity on short-term outcome of orthopedic surgery in ambulatory children with bilateral cerebral palsy. BMC Musculoskelet. Disord. 2021, 22, 481. [Google Scholar] [CrossRef]
- Schwartz, M.H.; Rozumalski, A. The gait deviation index: A new comprehensive index of gait pathology. Gait Posture 2008, 28, 351–357. [Google Scholar] [CrossRef]
- Graham, H.K.; Thomason, P.; Willoughby, K.; Hastings-Ison, T.; Stralen, R.V.; Dala-Ali, B.; Wong, P.; Rutz, E. Musculoskeletal Pathology in Cerebral Palsy: A Classification System and Reliability Study. Children 2021, 8, 252. [Google Scholar] [CrossRef]
- Thomason, P.; Graham, K.; Ye, K.; O’Donnell, A.; Kulkarni, V.; Davids, J.R.; Rutz, E. Knee surveillance for ambulant children with cerebral palsy. J. Child. Orthop. 2025, 19, 253–266. [Google Scholar] [CrossRef]
- Johnson, D.C.; Damiano, D.L.; Abel, M.F. The evolution of gait in childhood and adolescent cerebral palsy. J. Pediatr. Orthop. 1997, 17, 392–396. [Google Scholar] [CrossRef] [PubMed]
- Peeters, N.; Papageorgiou, E.; Hanssen, B.; De Beukelaer, N.; Staut, L.; Degelaen, M.; Van den Broeck, C.; Calders, P.; Feys, H.; Van Campenhout, A.; et al. The Short-Term Impact of Botulinum Neurotoxin-A on Muscle Morphology and Gait in Children with Spastic Cerebral Palsy. Toxins 2022, 14, 676. [Google Scholar] [CrossRef] [PubMed]
- Read, F.A.; Boyd, R.N.; Barber, L.A. Longitudinal assessment of gait quality in children with bilateral cerebral palsy following repeated lower limb intramuscular Botulinum toxin-A injections. Res. Dev. Disabil. 2017, 68, 35–41. [Google Scholar] [CrossRef] [PubMed]
| Sex | Age T1 | Age T2 | GMFCS | Max pKE | Max Knee Ext in gait | |||
|---|---|---|---|---|---|---|---|---|
| T1 | T2 | T1 | T2 | |||||
| TOTAL | M = 29; F = 12 | 8.2 (2) | 12.4 (2.8) | I =14; II = 14; III = 3 | R: −0.4 (5.8) L: −0.6 (4) | R: −5.4 (10.7) L: −3.7 (10.4) | R: 12.1 (16.5) L: 8.12 (14.4) | R: 16.4 (22.7) L: 11.5 (16.8) |
| BCP | M = 13; F= 8 | 7.7 (1.9) | 11.9 (2.8) | I = 6; II = 13; III = 3 | R: −0.5 (6.3) L: −0.7 (4.4) | R: −5.9 (11.6) L: −5.2 (11.4) | R: 12.9 (12.2) L: 10.3 (8.1) | R: 19 (22.4) L: 13.2 (20.7) |
| UCP | M = 5; F = 4 | 9.3 (1.7) | 13.6 (2.4) | I = 8; II = 1 | 0 (0) | 0.5 (4.6) | 2.8 (9.9) | 3.16 (6.7) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vanmechelen, I.; Råsberg, E.; Broström, E.; Lidbeck, C. Associations Between Maximal Passive Knee Extension and Sagittal Plane Kinematic Patterns in Children with Spastic Cerebral Palsy: A Longitudinal Study. J. Clin. Med. 2025, 14, 8567. https://doi.org/10.3390/jcm14238567
Vanmechelen I, Råsberg E, Broström E, Lidbeck C. Associations Between Maximal Passive Knee Extension and Sagittal Plane Kinematic Patterns in Children with Spastic Cerebral Palsy: A Longitudinal Study. Journal of Clinical Medicine. 2025; 14(23):8567. https://doi.org/10.3390/jcm14238567
Chicago/Turabian StyleVanmechelen, Inti, Edwin Råsberg, Eva Broström, and Cecilia Lidbeck. 2025. "Associations Between Maximal Passive Knee Extension and Sagittal Plane Kinematic Patterns in Children with Spastic Cerebral Palsy: A Longitudinal Study" Journal of Clinical Medicine 14, no. 23: 8567. https://doi.org/10.3390/jcm14238567
APA StyleVanmechelen, I., Råsberg, E., Broström, E., & Lidbeck, C. (2025). Associations Between Maximal Passive Knee Extension and Sagittal Plane Kinematic Patterns in Children with Spastic Cerebral Palsy: A Longitudinal Study. Journal of Clinical Medicine, 14(23), 8567. https://doi.org/10.3390/jcm14238567







