Mulligan Mobilization Combined with Conventional Therapy vs. Conventional Care Alone in Patients with Rotator Cuff Disease: A Systematic Review and Meta-Analysis of Randomized Controlled Trials
Abstract
1. Introduction
2. Methods
2.1. Inclusion/Exclusion Criteria
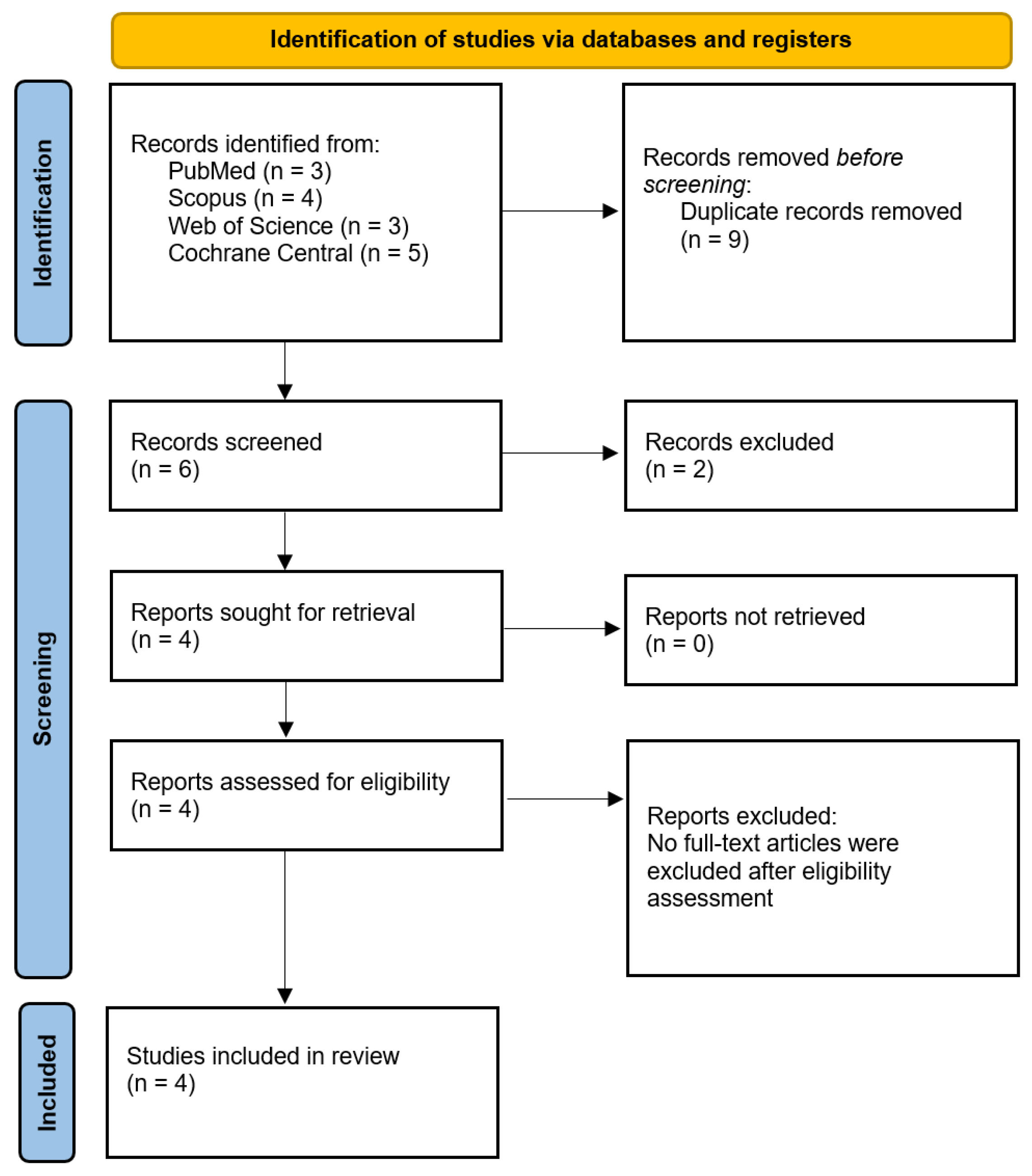
2.2. Literature Search and Data Extraction
2.3. Endpoints and Subgroup Analyses
2.4. Quality Assessment
2.5. Statistical Analysis
3. Results
3.1. Study Selection and Baseline Characteristics
3.2. Pooled Analyses of All Included Studies
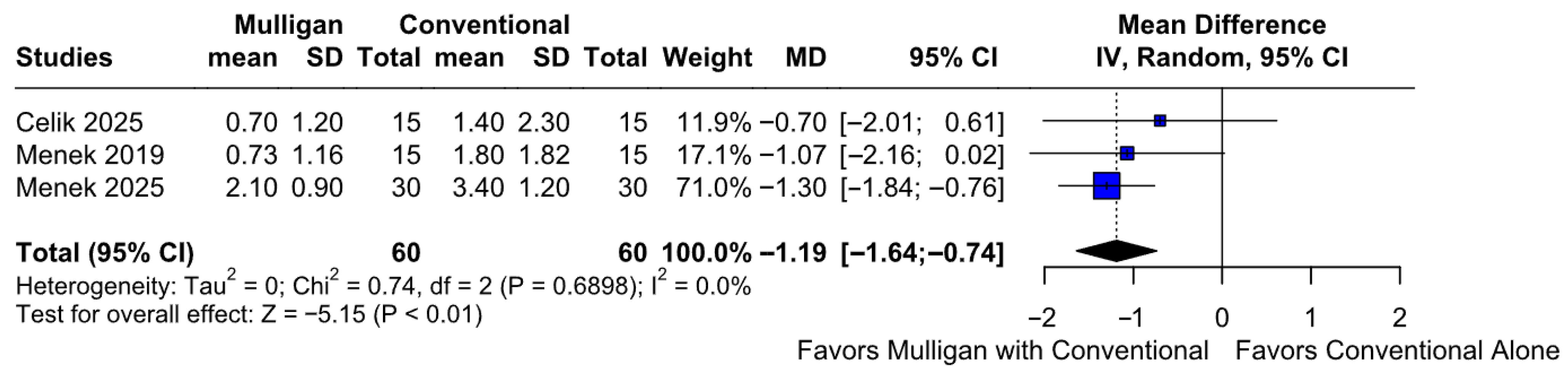
3.2.1. Pain Intensity at Rest
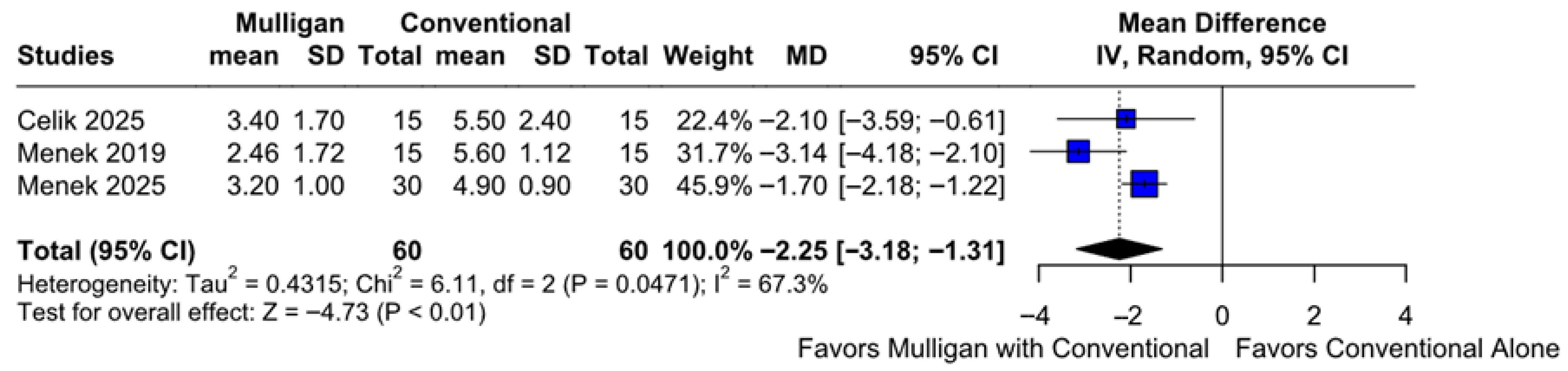
3.2.2. Pain Intensity During Activity
3.2.3. Functionality
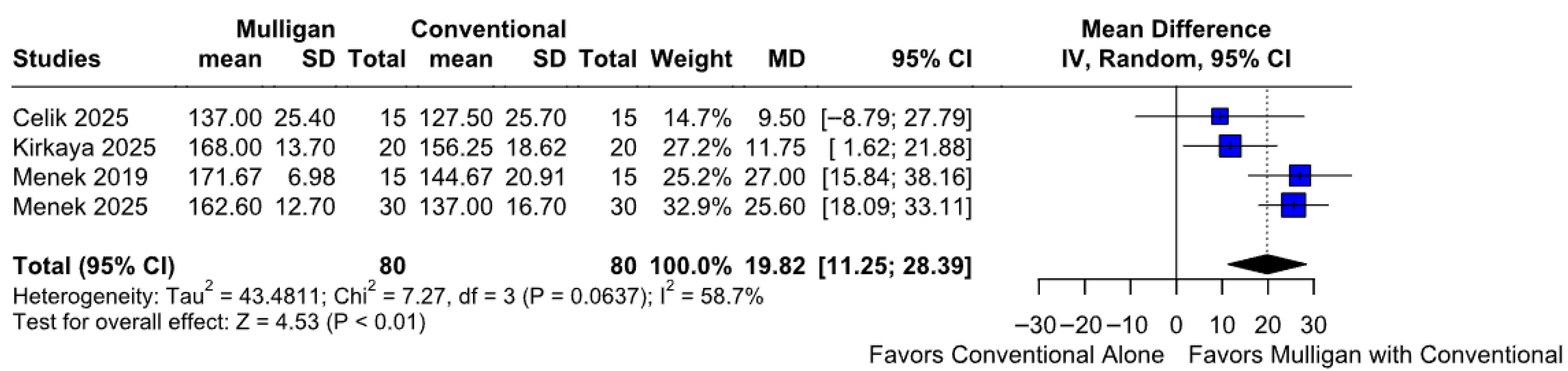
3.2.4. Range of Motion
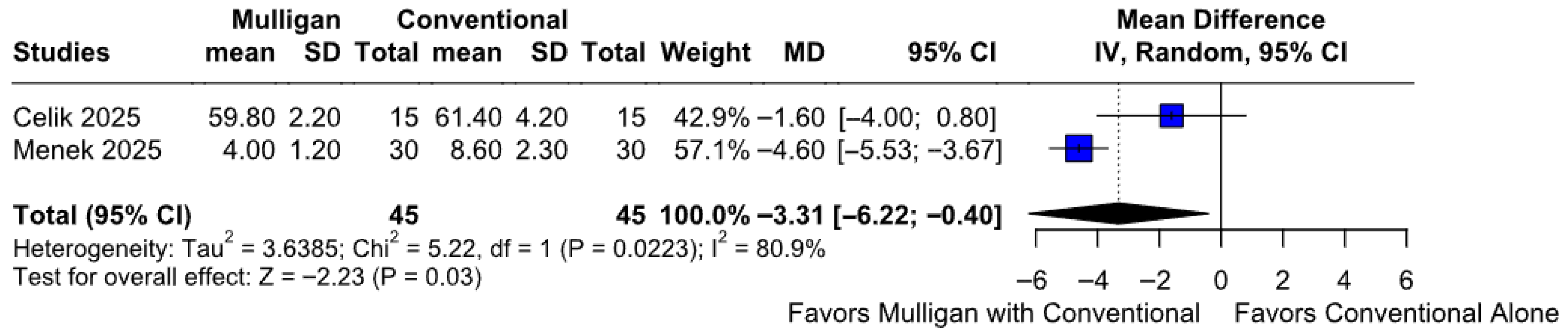
3.2.5. Join Position Sense
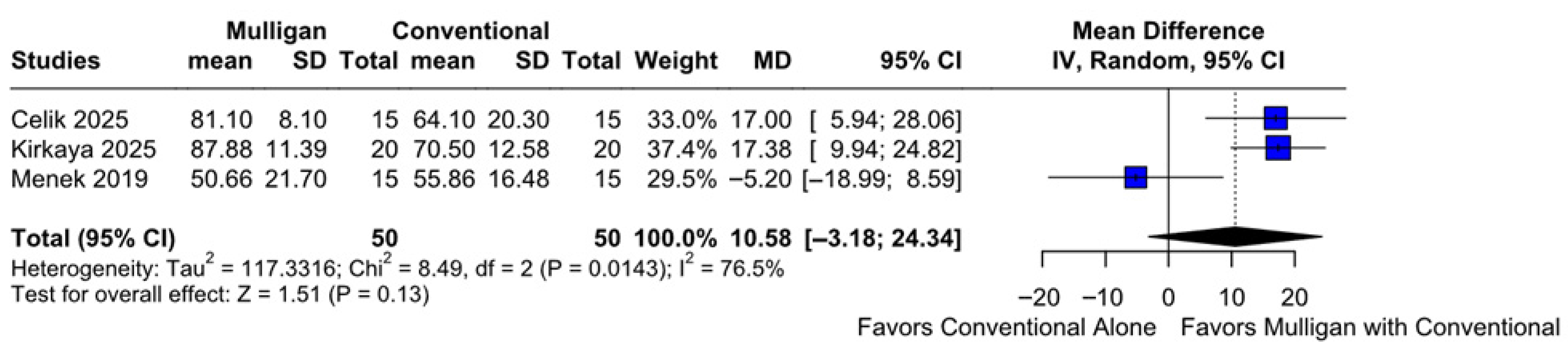
3.2.6. QoL
3.3. Subgroup Analyses
3.3.1. Pain Intensity at Rest Based on the ROB
3.3.2. Pain Intensity During Activity Based on the ROB
3.3.3. Functionality Based on the ROB
3.3.4. Range of Motion Based on the ROB
3.3.5. Joint Position Sense Based on the ROB
3.3.6. QoL
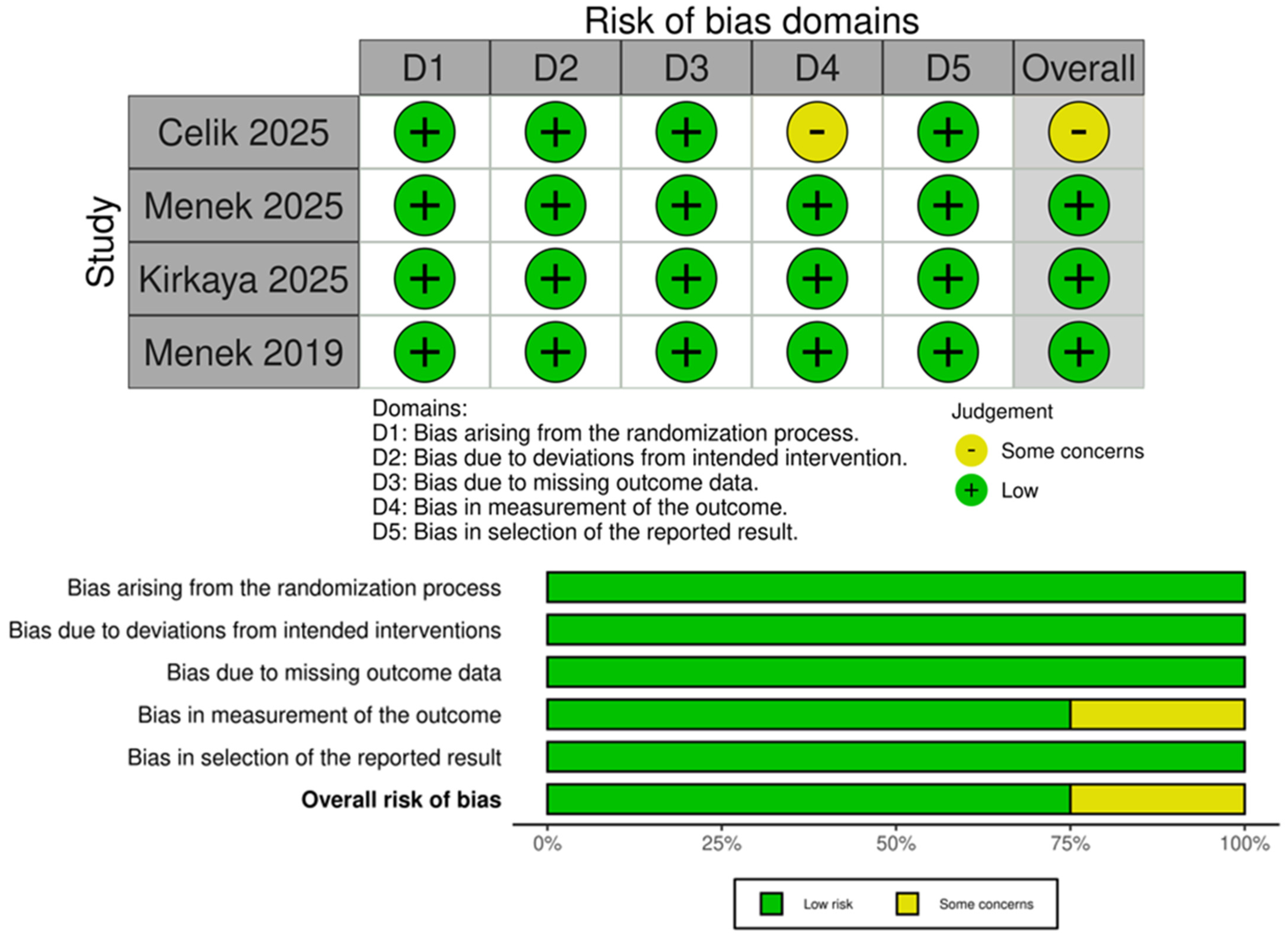
3.4. Quality Assessment
4. Discussion
4.1. Principle Findings
4.2. Mechanistic Considerations
4.3. Comparison with the Literature
4.4. Clinical Applications
4.5. Limitations
4.6. Future Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cook, J.L.; Rio, E.; Purdam, C.R.; Docking, S.I. Revisiting the continuum model of tendon pathology: What is its merit in clinical practice and research? Br. J. Sports Med. 2016, 50, 1187–1191. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Littlewood, C.; Ashton, J.; Chance-Larsen, K.; May, S.; Sturrock, B. Exercise for rotator cuff tendinopathy: A systematic review. Physiotherapy 2012, 98, 101–109. [Google Scholar] [CrossRef] [PubMed]
- Mohajjel Aghdam, A.; Kolahi, S.; Hasankhani, H.; Behshid, M.; Varmaziar, Z. The relationship between pain and physical function in adults with Knee Osteoarthritis. Int. Res. J. Appl. Basic Sci. 2013, 4, 1102–1106. [Google Scholar]
- Jepma, M.; Wager, T.D. Multiple potential mechanisms for context effects on pain. Pain 2013, 154, 629–631. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Vicenzino, B. Mobilisation with movement: The effect of two key variables. J. Man. Manip. Ther. 2007, 15, 185–190. [Google Scholar]
- Sterling, M.; Jull, G.; Wright, A. Cervical mobilisation: Concurrent effects on pain, sympathetic nervous system activity and motor activity. Man. Ther. 2001, 6, 72–81. [Google Scholar] [CrossRef] [PubMed]
- Menek, B.; Tarakci, D.; Algun, Z.C. The effect of Mulligan mobilization on pain and life quality of patients with Rotator cuff syndrome: A randomized controlled trial. J. Back. Musculoskelet. Rehabil. 2019, 32, 171–178. [Google Scholar] [CrossRef] [PubMed]
- Kirkaya, A.C.; Atici, E.; Aydin, G.; Surenkok, O. Comparing the Effectiveness of Mulligan Movement with Mobilization and Proprioceptive Neuromuscular Facilitation Techniques in Rehabilitation of Rotator Cuff Syndrome: A Randomized Controlled Trial. Indian J. Orthop. 2025, 59, 1969–1978. [Google Scholar] [CrossRef]
- Celik, T.; Menek, B. The effect of Mulligan and Maitland techniques on pain, functionality, proprioception, and quality of life in individuals with rotator cuff lesions. J. Hand Ther. 2025, 38, 574–583. [Google Scholar] [CrossRef]
- Menek, B.; Menek, M.Y. The efficacy of Mulligan mobilization and corticosteroid injection on pain, functionality, and proprioception in rotator cuff tears: A randomized controlled trial. J. Hand Ther. 2025, 38, 410–417. [Google Scholar] [CrossRef] [PubMed]
- Doiron-Cadrin, P.; Lafrance, S.; Saulnier, M.; Cournoyer, É.; Roy, J.S.; Dyer, J.O.; Frémont, P.; Dionne, C.; MacDermid, J.C.; Tousignant, M.; et al. Shoulder Rotator Cuff Disorders: A Systematic Review of Clinical Practice Guidelines and Semantic Analyses of Recommendations. Arch. Phys. Med. Rehabil. 2020, 101, 1233–1242. [Google Scholar] [CrossRef] [PubMed]
- Desjardins-Charbonneau, A.; Roy, J.S.; Dionne, C.E.; Frémont, P.; MacDermid, J.C.; Desmeules, F. The efficacy of manual therapy for rotator cuff tendinopathy: A systematic review and meta-analysis. J. Orthop. Sports Phys. Ther. 2015, 45, 330–350. [Google Scholar] [CrossRef] [PubMed]
- Satpute, K.; Reid, S.; Mitchell, T.; Mackay, G.; Hall, T. Efficacy of mobilization with movement (MWM) for shoulder conditions: A systematic review and meta-analysis. J. Man. Manip. Ther. 2022, 30, 13–32. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Higgins, J.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions; Version 6.4 (Updated August 2023); Cochrane: London, UK, 2023; Available online: https://www.training.cochrane.org/handbook (accessed on 28 February 2025).
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—A web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef]
- Nakagawa, S.; Noble, D.W.A.; Senior, A.M.; Lagisz, M. Meta-evaluation of meta-analysis: Ten appraisal questions for biologists. BMC Biol. 2017, 15, 18. [Google Scholar] [CrossRef]
- Hartung, J.; Knapp, G. On tests of the overall treatment effect in meta-analysis with normally distributed responses. Stat. Med. 2001, 20, 1771–1782. [Google Scholar] [CrossRef]
- Knapp, G.; Hartung, J. Improved tests for a random effects meta-regression with a single covariate. Stat. Med. 2003, 22, 2693–2710. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria; R Core Team: Vienna, Austria, 2024. [Google Scholar]
- Andrade, C. Mean difference, standardized mean difference (SMD), and their use in meta-analysis: As simple as it gets. J. Clin. Psychiatry 2020, 81, 11349. [Google Scholar] [CrossRef]
- Teys, P. The effects of Mulligan’s mobilization with movement on pain and range of motion in patients with shoulder impingement syndrome. Man. Ther. 2008, 13, 315–322. [Google Scholar] [CrossRef] [PubMed]
- Stroup, P. The effectiveness of mobilization with movement in the treatment of musculoskeletal conditions: A systematic review. J. Man. Manip. Ther. 2012, 20, 152–162. [Google Scholar]

| Study | Study Design | Country | No. Patients | Age * | Female, % | MG | CT | Affected Shoulder (L/R), % | Follow-up (Weeks) |
|---|---|---|---|---|---|---|---|---|---|
| Celik 2025 [9] | RCT | Turkey | 30 | MG: 43.5 CT: 51.1 | MG: 20 CT: 60 | 15 | 15 | MG: 47/53 CT: 47/53 | 3 |
| Kirkaya 2025 [8] | RCT | Turkey | 40 | MG: 46.3 CT: 56.7 | MG: 40 CT: 70 | 20 | 20 | MG: 15/85 CT: 5/95 | 4 |
| Menek 2025 [10] | RCT | Turkey | 60 | MG: 51.1 CT: 53.2 | MG: 53 CT: 60 | 30 | 30 | MG: 53/46 CT: 33/66 | 3 |
| Menek 2019 [7] | RCT | Turkey | 30 | MG: 51.7 CT: 50.2 | MG: 52 CT: 40 | 15 | 15 | MG: 53/46 CT: 46/53 | 3 |
| Study/Outcome | Pain (Rest) | Pain (Activity) | Functionality | ROM | QoL | JPS |
|---|---|---|---|---|---|---|
| Menek 2019 [7] | X | X | X | X | X | |
| Menek 2025 [10] | X | X | X | X | X | |
| Celik 2025 [9] | X | X | X | X | X | X |
| Kirkaya 2025 [8] | X | X | X |
| Certainty Assessment | № of Patients | Effect | Certainty | Importance | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| № of Studies | Study Design | Risk of Bias | Inconsistency | Indirectness | Imprecision | Other Considerations | Mulligan’s Technique with Conventional Therapy | Conventional Therapy Alone | Relative (95% CI) | Absolute (95% CI) | ||
| Rest pain intensity (follow-up: mean 3 weeks; assessed with: mean ± SD) | ||||||||||||
| 3 | randomized trials | not serious | not serious | not serious | not serious | none | 60 | 60 | - | MD 1.19 lower (1.64 lower to 0.74 lower) | ⨁⨁⨁⨁ High | |
| Active pain intensity (follow-up: mean 3 weeks; assessed with: mean ± SD) | ||||||||||||
| 3 | randomized trials | not serious | not serious | not serious | not serious | none | 60 | 60 | - | MD 2.25 lower (3.18 lower to 1.31 lower) | ⨁⨁⨁⨁ High | |
| Functionality (follow-up: mean 3 weeks; assessed with: mean ± SD) | ||||||||||||
| 4 | randomized trials | not serious | not serious | not serious | not serious | none | 80 | 80 | - | MD 14.71 lower (20.1 lower to 9.33 lower) | ⨁⨁⨁⨁ High | |
| Quality of Life (follow-up: mean 3 weeks; assessed with: mean ± SD) | ||||||||||||
| 3 | randomized trials | not serious | not serious | not serious | serious a | strong association | 50 | 50 | - | MD 10.58 higher (3.18 lower to 24.34 higher) | ⨁⨁⨁⨁ High a | |
| Range of Motion (follow-up: mean 3 weeks; assessed with: mean ± SD) | ||||||||||||
| 4 | randomized trials | not serious | not serious | not serious | not serious | none | 80 | 80 | - | MD 19.82 higher (11.25 higher to 28.39 higher) | ⨁⨁⨁⨁ High | |
| Joint position sense (follow-up: mean 3 weeks; assessed with: mean ± SD) | ||||||||||||
| 2 | randomized trials | not serious | not serious | not serious | not serious | strong association | 45 | 45 | - | MD 3.31 lower (6.22 lower to 0.4 lower) | ⨁⨁⨁⨁ High | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alqallaf, A.; Alharran, A.M.; Penchev, P.; Alkandari, Y.Y.; Almulla, B.; Almulla, A.; Alshatti, A.; AlAyyaf, A.E.; Alahmad, A.; Al-Naseem, A.O. Mulligan Mobilization Combined with Conventional Therapy vs. Conventional Care Alone in Patients with Rotator Cuff Disease: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Clin. Med. 2025, 14, 8352. https://doi.org/10.3390/jcm14238352
Alqallaf A, Alharran AM, Penchev P, Alkandari YY, Almulla B, Almulla A, Alshatti A, AlAyyaf AE, Alahmad A, Al-Naseem AO. Mulligan Mobilization Combined with Conventional Therapy vs. Conventional Care Alone in Patients with Rotator Cuff Disease: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Journal of Clinical Medicine. 2025; 14(23):8352. https://doi.org/10.3390/jcm14238352
Chicago/Turabian StyleAlqallaf, Abdulmuhsen, Abdullah M. Alharran, Plamen Penchev, Yousef Y. Alkandari, Bassam Almulla, Ahmed Almulla, Abdullah Alshatti, Abdulrahman Emad AlAyyaf, Ahmad Alahmad, and Abdulrahman O. Al-Naseem. 2025. "Mulligan Mobilization Combined with Conventional Therapy vs. Conventional Care Alone in Patients with Rotator Cuff Disease: A Systematic Review and Meta-Analysis of Randomized Controlled Trials" Journal of Clinical Medicine 14, no. 23: 8352. https://doi.org/10.3390/jcm14238352
APA StyleAlqallaf, A., Alharran, A. M., Penchev, P., Alkandari, Y. Y., Almulla, B., Almulla, A., Alshatti, A., AlAyyaf, A. E., Alahmad, A., & Al-Naseem, A. O. (2025). Mulligan Mobilization Combined with Conventional Therapy vs. Conventional Care Alone in Patients with Rotator Cuff Disease: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Journal of Clinical Medicine, 14(23), 8352. https://doi.org/10.3390/jcm14238352







