Association of Radiomics and Pericarotid Adipose Tissue Characteristics with Systemic Inflammation in Patients Undergoing Carotid Endarterectomy
Abstract
1. Introduction
2. Methods
2.1. Study Sample and Data Source
2.2. Definitions
- TIA was defined as an episode of focal brain, retinal, or spinal cord dysfunction lasting less than 24 h.
- Stroke was defined as a sudden onset focal neurological dysfunction with symptoms lasting more than 24 h [13].
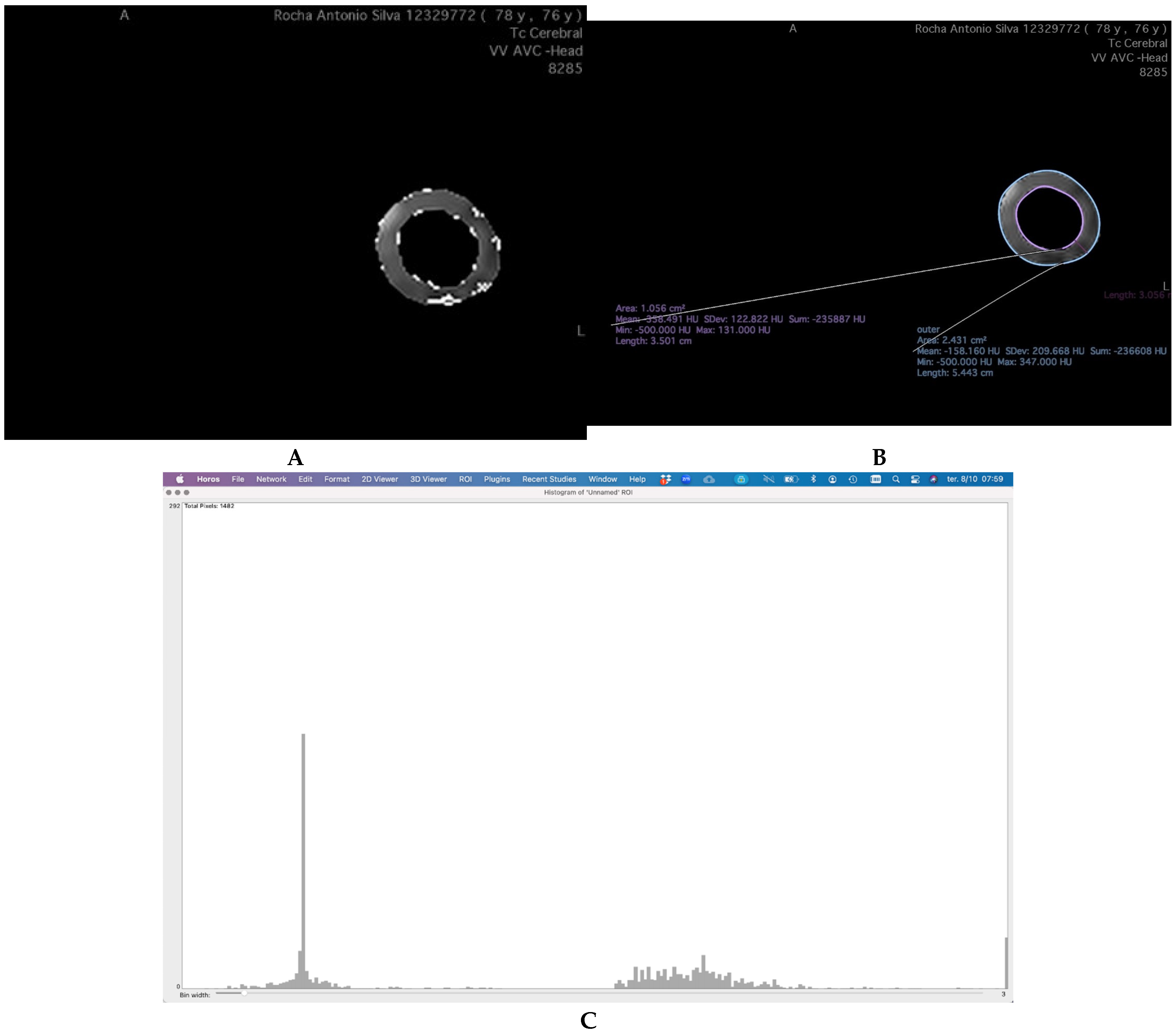
2.3. PCAT Definition
2.4. Image Analysis
2.5. Outcome Assessment
2.6. Reproducibility Study
2.7. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| Glossary | |
| CEA | carotid endarterectomy. |
| CT | computed tomography. |
| CTA | computed tomography angiography. |
| HU | Hounsfield units. |
| MRI | magnetic resonance imaging. |
| NLR | neutrophil-to-lymphocyte ratio. |
| PCAT | pericarotid adipose tissue. |
| RA | regional anesthesia. |
| RDW | red cell distribution width. |
| ROI | region of interest. |
References
- Chen, Y.; Qin, Z.; Wang, Y.; Li, X.; Zheng, Y.; Liu, Y. Role of Inflammation in Vascular Disease-Related Perivascular Adipose Tissue Dysfunction. Front. Endocrinol. 2021, 12, 710842. [Google Scholar] [CrossRef] [PubMed]
- Pereira-Neves, A.; Rocha-Neves, J.; Fragão-Marques, M.; Duarte-Gamas, L.; Jácome, F.; Coelho, A.; Cerqueira, A.; Andrade, J.P.; Mansilha, A. Red blood cell distribution width is associated with hypoperfusion in carotid endarterectomy under regional anesthesia. Surgery 2021, 169, 1536–1543. [Google Scholar] [CrossRef] [PubMed]
- Duarte-Gamas, L.; Pereira-Neves, A.; Jácome, F.; Fragão-Marques, M.; Vaz, R.P.; Andrade, J.P.; Rocha-Neves, J.P. Red Blood Cell Distribution Width as a 5-Year Prognostic Marker in Patients Submitted to Carotid Endarterectomy. Cerebrovasc. Dis. Extra 2020, 10, 181–192. [Google Scholar] [CrossRef] [PubMed]
- Yu, Y.; Cui, W.H.; Cheng, C.; Lu, Y.; Zhang, Q.; Han, R.Q. Association between neutrophil-to-lymphocyte ratio and major postoperative complications after carotid endarterectomy: A retrospective cohort study. World J. Clin. Cases 2021, 9, 10816–10827. [Google Scholar] [CrossRef]
- Liu, X.; Wu, F.; Jia, X.; Qiao, H.; Liu, Y.; Yang, X.; Li, Y.; Zhang, M.; Yang, Q. Pericarotid adipose tissue computed tomography attenuation distinguishes different stages of carotid atherosclerotic disease: A cross-sectional study. Quant. Imaging Med. Surg. 2023, 13, 8247–8258. [Google Scholar] [CrossRef]
- Cai, M.; Zhao, D.; Han, X.; Han, S.; Zhang, W.; Zang, Z.; Gai, C.; Rong, R.; Gao, T. The role of perivascular adipose tissue-secreted adipocytokines in cardiovascular disease. Front. Immunol. 2023, 14, 1271051. [Google Scholar] [CrossRef]
- Nie, J.Y.; Chen, W.X.; Zhu, Z.; Zhang, M.Y.; Zheng, Y.J.; Wu, Q.D. Initial experience with radiomics of carotid perivascular adipose tissue in identifying symptomatic plaque. Front. Neurol. 2024, 15, 1340202. [Google Scholar] [CrossRef]
- Le, E.P.V.; Rundo, L.; Tarkin, J.M.; Evans, N.R.; Chowdhury, M.M.; Coughlin, P.A.; Pavey, H.; Wall, C.; Zaccagna, F.; Gallagher, F.A.; et al. Assessing robustness of carotid artery CT angiography radiomics in the identification of culprit lesions in cerebrovascular events. Sci. Rep. 2021, 11, 3499. [Google Scholar] [CrossRef]
- AlSheikh, S.; Aljabri, B.; Alanezi, T.; Al-Salman, M.; Aldossary, M.Y.; Almashat, A.H.; Elmutawi, H.S.; Aldoghmani, R.A.; Altuwaijri, T.; Iqbal, K.; et al. Outcomes of carotid endarterectomy: Insights from a single-center retrospective cohort study. Saudi Med. J. 2024, 45, 405–413. [Google Scholar] [CrossRef]
- Mazzotta, C.; Basu, S.; Gower, A.C.; Karki, S.; Farb, M.G.; Sroczynski, E.; Zizza, E.; Sarhan, A.; Pande, A.N.; Walsh, K.; et al. Perivascular Adipose Tissue Inflammation in Ischemic Heart Disease. Arter. Thromb. Vasc. Biol. 2021, 41, 1239–1250. [Google Scholar] [CrossRef]
- Goncalves, V.A.; Geiger, M.A.; Sarti, D.A.; Guillaumon, A.T. Association between platelet lymphocyte ratio and neutrophil lymphocyte ratio and clinical outcomes following carotid endarterectomy. J. Vasc. Bras. 2023, 22, e20220122. [Google Scholar] [CrossRef] [PubMed]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P.; Strobe Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies. Int. J. Surg. 2014, 12, 1495–1499. [Google Scholar] [CrossRef] [PubMed]
- Naylor, R.; Rantner, B.; Ancetti, S.; de Borst, G.J.; De Carlo, M.; Halliday, A.; Kakkos, S.K.; Markus, H.S.; McCabe, D.J.; Sillesen, H.; et al. Editor’s Choice—European Society for Vascular Surgery (ESVS) 2023 Clinical Practice Guidelines on the Management of Atherosclerotic Carotid and Vertebral Artery Disease. Eur. J. Vasc. Endovasc. Surg. 2023, 65, 7–111. [Google Scholar] [CrossRef]
- Oates, C.P.; Naylor, A.R.; Hartshorne, T.; Charles, S.M.; Fail, T.; Humphries, K.; Aslam, M.; Khodabakhsh, P. Joint recommendations for reporting carotid ultrasound investigations in the United Kingdom. Eur. J. Vasc. Endovasc. Surg. 2009, 37, 251–261. [Google Scholar] [CrossRef]
- Yu, M.; Meng, Y.; Zhang, H.; Wang, W.; Qiu, S.; Wang, B.; Bao, Y.; Du, B.; Zhu, S.; Ge, Y.; et al. Associations between pericarotid fat density and image-based risk characteristics of carotid plaque. Eur. J. Radiol. 2022, 153, 110364. [Google Scholar] [CrossRef]
- Lan, Y.; Shang, J.; Ma, Y.; Zhen, Y.; Dang, Y.; Ren, D.; Liu, T.; Ju, R.; Guo, N.; Wang, X.; et al. A new predictor of coronary artery disease in acute ischemic stroke or transient ischemic attack patients: Pericarotid fat density. Eur. Radiol. 2024, 34, 1667–1676. [Google Scholar] [CrossRef]
- Tan, N.; Dey, D.; Marwick, T.H.; Nerlekar, N. Pericoronary Adipose Tissue as a Marker of Cardiovascular Risk: JACC Review Topic of the Week. J. Am. Coll Cardiol. 2023, 81, 913–923. [Google Scholar] [CrossRef]
- Polidori, T.; De Santis, D.; Rucci, C.; Tremamunno, G.; Piccinni, G.; Pugliese, L.; Zerunian, M.; Guido, G.; Pucciarelli, F.; Bracci, B.; et al. Radiomics applications in cardiac imaging: A comprehensive review. Radiol. Med. 2023, 128, 922–933. [Google Scholar] [CrossRef]
- van Griethuysen, J.J.M.; Fedorov, A.; Parmar, C.; Hosny, A.; Aucoin, N.; Narayan, V.; Beets-Tan, R.G.H.; Fillion-Robin, J.C.; Pieper, S.; Aerts, H.J.W.L. Computational Radiomics System to Decode the Radiographic Phenotype. Cancer Res. 2017, 77, e104–e107. [Google Scholar] [CrossRef]
- Tong, Y.; Zuo, Z.; Li, X.; Li, M.; Wang, Z.; Guo, X.; Wang, X.; Sun, Y.; Chen, D.; Zhang, Z. Protective role of perivascular adipose tissue in the cardiovascular system. Front. Endocrinol. 2023, 14, 1296778. [Google Scholar] [CrossRef]
- Ma, R.; Fari, R.; Van Der Harst, P.; N. De Cecco, C.; E. Stillman, A.; Vliegenthart, R.; Van Assen, M. Evaluation of pericoronary adipose tissue attenuation on CT. Br. J. Radiol. 2023, 96, 20220885. [Google Scholar] [CrossRef] [PubMed]
- Madaelil, T.P.; Sharma, A.; Hildebolt, C.; Parsons, M. Using Correlative Properties of Neighboring Pixels to Improve Gray-White Differentiation in Pediatric Head CT Images. AJNR Am. J. Neuroradiol. 2018, 39, 577–582. [Google Scholar] [CrossRef] [PubMed]
- Butt, K.; D’SOuza, J.; Yuan, C.; Jayakumaran, J.; Nguyen, M.; I Butt, H.; Abusaada, K. Correlation of the Neutrophil-to-Lymphocyte Ratio (NLR) and Platelet-to-Lymphocyte Ratio (PLR) with Contrast-Induced Nephropathy in Patients With Acute Coronary Syndrome Undergoing Percutaneous Coronary Interventions. Cureus 2020, 12, e11879. [Google Scholar] [CrossRef] [PubMed]
- Adachi, Y.; Ueda, K.; Takimoto, E. Perivascular adipose tissue in vascular pathologies—A novel therapeutic target for atherosclerotic disease? Front. Cardiovasc. Med. 2023, 10, 1151717. [Google Scholar] [CrossRef]
- Rami, A.Z.A.; Hamid, A.A.; Anuar, N.N.M.; Aminuddin, A.; Ugusman, A. Exploring the Relationship of Perivascular Adipose Tissue Inflammation and the Development of Vascular Pathologies. Mediat. Inflamm. 2022, 2022, 2734321. [Google Scholar] [CrossRef]
- Adachi, Y.; Ueda, K.; Nomura, S.; Ito, K.; Katoh, M.; Katagiri, M.; Yamada, S.; Hashimoto, M.; Zhai, B.; Numata, G.; et al. Beiging of perivascular adipose tissue regulates its inflammation and vascular remodeling. Nat. Commun. 2022, 13, 5117. [Google Scholar] [CrossRef]
| Total (n = 20) | |
|---|---|
| Gender, n (%) | |
| Male | 16 (75.0) |
| Female | 4 (25.0) |
| Age (years) | |
| Mean (±SD) | 71.8 (±6.9) |
| Side | |
| Right, n (%) | 10 (50.0) |
| Left, n (%) | 10 (50.0) |
| CV risk-factors | |
| Hypertension, n (%) | 18 (90.0) |
| Diabetes, n (%) | 11 (45.0) |
| Smoking history, n (%) | 12 (60.0) |
| Dyslipidemia, n (%) | 19 (95.0) |
| Obesity, n (%) | 3 (15.0) |
| CKD, n (%) | 4 (20.0) |
| PAD, n (%) | 7 (35.0) |
| CAD, n (%) | 5 (25.0) |
| COPD, n (%) | 2 (10.0) |
| CHF | 0 (0.0) |
| AF, n (%) | 2 (10.0) |
| ASA, n (%) | |
| II | 1 (5.0) |
| III | 18 (90.0) |
| IV | 1 (5.0) |
| Asymptomatic, n (%) | 16 (80.0) |
| Symptomatic, n (%) | 4 (20.0) |
| TIA | 0 (0.0) |
| Stroke | 1 (5.0) |
| Stenosis degree | 85.0 ± 10.8 |
| Mean (±SD) (%) | |
| Contralateral stenosis degree | |
| Mean (±SD) (%) | 56 ± 7.0 |
| Contralateral stenosis (>50%) | 5 (25) |
| AAS > 2 weeks, n (%) | 11 (55.0) |
| Clopidogrel, n (%) | 2 (10.0) |
| NLR | 5.79 (±4.0) |
| RDW-CV (%) | 13.75 (±1.09) |
| Total (n = 20) | |
|---|---|
| AreaRightOutter | 178.98 ± 42.4 |
| AreaRightInner | 71.38 ± 33.3 |
| AreaRightTotal | 108.27 ± 63.6 |
| FatPixelsRight | 66.77 ± 68.3 |
| pixel190to120R | 0.05 ± 0.22 |
| pixel119to70R | 18.45 ± 35.4 |
| pixel69to30R | 48.2 ± 37.3 |
| AreaLeftOutter | 185.41 ± 52.3 |
| AreaLeftInner | 65.17 ± 27.00 |
| AreLeft | 120.24 ± 26.1 |
| FatpixelsLeft | 63.94 ± 75.3 |
| pixel190to120L | 0.64 ± 2.40 |
| pixel119to70L | 18.29 ± 18.5 |
| pixel69to30L | 65.93 ± 60.8 |
| Grayweale | 1.51 ± 0.65 |
| Beta | t | p | |
|---|---|---|---|
| Area Outer | −0.677 | 5.151 | ˂0.001 |
| pixel190to120 | −3.809 | 7.281 | ˂0.001 |
| pixel119to70 | 3.814 | 7.495 | ˂0.001 |
| Contrast | −0.422 | −1.920 | 0.072 |
| Beta | t | p | |
|---|---|---|---|
| Uniformity | 0.494 | 2.411 | 0.027 |
| Contrast | −0.402 | −1.861 | 0.079 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Santos-Teixeira, D.; Myrcha, P.; Trigo, V.; Ribeiro, H.; Barbosa-Breda, J.; Dias-Neto, M.; Rocha-Neves, J.; Gloviczki, P. Association of Radiomics and Pericarotid Adipose Tissue Characteristics with Systemic Inflammation in Patients Undergoing Carotid Endarterectomy. J. Clin. Med. 2025, 14, 8342. https://doi.org/10.3390/jcm14238342
Santos-Teixeira D, Myrcha P, Trigo V, Ribeiro H, Barbosa-Breda J, Dias-Neto M, Rocha-Neves J, Gloviczki P. Association of Radiomics and Pericarotid Adipose Tissue Characteristics with Systemic Inflammation in Patients Undergoing Carotid Endarterectomy. Journal of Clinical Medicine. 2025; 14(23):8342. https://doi.org/10.3390/jcm14238342
Chicago/Turabian StyleSantos-Teixeira, Diogo, Piotr Myrcha, Vasco Trigo, Hugo Ribeiro, João Barbosa-Breda, Marina Dias-Neto, João Rocha-Neves, and Peter Gloviczki. 2025. "Association of Radiomics and Pericarotid Adipose Tissue Characteristics with Systemic Inflammation in Patients Undergoing Carotid Endarterectomy" Journal of Clinical Medicine 14, no. 23: 8342. https://doi.org/10.3390/jcm14238342
APA StyleSantos-Teixeira, D., Myrcha, P., Trigo, V., Ribeiro, H., Barbosa-Breda, J., Dias-Neto, M., Rocha-Neves, J., & Gloviczki, P. (2025). Association of Radiomics and Pericarotid Adipose Tissue Characteristics with Systemic Inflammation in Patients Undergoing Carotid Endarterectomy. Journal of Clinical Medicine, 14(23), 8342. https://doi.org/10.3390/jcm14238342








