Analysis of Medical Response Team Interventions and the Impact of Certified Training on the Treatment of Patients with Hypoglycaemia—A Simulation Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
2.2. Participants
2.3. Data Collection
2.4. Clinical Performance Scoring Tool
2.5. Statistical Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Teuben, M.P.J.; Löhr, N.; Shehu, A.; Berk, T.; Jensen, K.O.; Mikova, E.; Brüesch, M.; Müller, S.; Pfeifer, R.; Mica, L.; et al. The value of pre-hospital trauma life support courses for medical personnel–A questionnaire study. Front. Med. 2024, 11, 1345310. [Google Scholar] [CrossRef]
- Woodall, J.; McCarthy, M.; Johnston, T.; Tippett, V.; Bonham, R. Impact of advanced cardiac life support-skilled paramedics on survival from out-of-hospital cardiac arrest in a statewide emergency medical service. Emerg. Med. J. 2007, 24, 134–138. [Google Scholar] [CrossRef]
- Häske, D.; Beckers, S.K.; Dieroff, M.; Gliwitzky, B.; Hofmann, M.; Lefering, R.; Münzberg, M. Training Effectiveness and Impact on Safety, Treatment Quality, and Communication in Prehospital Emergency Care: The Prospective Longitudinal Mixed-Methods EPPTC Trial. J. Patient Saf. 2022, 18, 71–76. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health. Regulation of the Minister of Health of 19 April 2024 on the continuing professional development of persons practicing certain medical professions. J. Laws 2024, 674. [Google Scholar]
- Ćwiertnia, M.; Ilczak, T.; Białoń, P.; Stasicki, A.; Szlagor, M.; Dutka, M.; Kudłacik, B.; Hajduga, M.B.; Mikulska, M.; Bobiński, R.; et al. Analysis of emergency medical response team performance during the International Winter Championships in Emergency Medicine. Medicina 2022, 58, 1578. [Google Scholar] [CrossRef]
- Klein, T.A.; Tadi, P. EMS Scene Safety. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2025. Available online: https://www.ncbi.nlm.nih.gov/books/NBK557615/ (accessed on 15 October 2025).
- Gangaram, P.; Pillay, Y.; Alinier, G. Paramedics’ knowledge, attitudes, and practices regarding the use of personal protective equipment against COVID-19. Qatar Med. J. 2022, 2022, 50. [Google Scholar] [CrossRef] [PubMed]
- D’Ettorre, G.; Pellicani, V.; Vullo, A. Workplace violence against healthcare workers in Emergency Departments: A case-control study. Acta Biomed. 2019, 90, 621–624. [Google Scholar]
- Ganczak, M.; Topczewska, K.; Biesiada, D.; Korzeń, M. Frequency of occupational bloodborne infections and sharps injuries among Polish paramedics from selected ambulance stations. Int. J. Environ. Res. Public Health 2021, 18, 60. [Google Scholar] [CrossRef]
- Perkins, G.D.; Walker, G.; Christensen, K.; Hulme, J.; Monsieurs, K.G. Teaching recognition of agonal breathing improves accuracy of diagnosing cardiac arrest. Resuscitation 2006, 70, 432–437. [Google Scholar] [CrossRef]
- Albarran, J.W.; Moule, P.; Gilchrist, M.; Soar, J. Comparison of sequential and simultaneous breathing and pulse check by healthcare professionals during simulated scenarios. Resuscitation 2006, 68, 243–249. [Google Scholar] [CrossRef]
- Cretikos, M.A.; Bellomo, R.; Hillman, K.; Chen, J.; Finfer, S.; Flabouris, A. Accurate respiratory rates count: So should you! Resuscitation 2008, 77, 286–290. [Google Scholar]
- Elliott, M.; Williamson, R.; Endacott, R. Patient mortality and the neglect of vital signs’ assessment: An audit of a national coronial database. Nurs. Crit. Care 2006, 29, 1636–1642. [Google Scholar] [CrossRef]
- Perkins, G.D.; Gräsner, J.-T.; Semeraro, F.; Olasveengen, T.; Soar, J.; Lott, C.; Van de Voorde, P.; Madar, J.; Zideman, D.; Mentzelopoulos, S.; et al. European Resuscitation Council Guidelines 2021: Executive summary. Resuscitation 2021, 161, 1–60. [Google Scholar] [CrossRef]
- Cooper, R.J.; Schriger, D.L.; Flaherty, H.L.; Lin, E.J.; Hubbell, K.A. Effect of vital signs on triage decisions. Ann. Emerg. Med. 2022, 39, 223–232. [Google Scholar] [CrossRef] [PubMed]
- Taherkhani, A. Use of the ABCDE approach to assess a patient post-operatively: A case study. Nurs. Stand. 2019, 34, 77–81. [Google Scholar] [CrossRef]
- Thim, T.; Krarup, N.H.V.; Grove, E.L.; Rohde, C.V.; Løfgren, B. Initial assessment and treatment with the Airway, Breathing, Circulation, Disability, Exposure (ABCDE) approach. Scand. J. Trauma Resusc. Emerg. Med. 2012, 20, 28. [Google Scholar] [CrossRef]
- Smith, D.; Bowden, T. Using the ABCDE approach to assess the deteriorating patient. Nurs. Stand. 2017, 32, 51–63. [Google Scholar] [CrossRef] [PubMed]
- Kantonen, J.; Kaartinen, J.; Mattila, J.; Menezes, R.; Malmila, M.; Castrén, M.; Kauppila, T. Impact of the ABCDE triage on the number of patient visits to the emergency department. BMC Emerg. Med. 2010, 10, 12. [Google Scholar] [CrossRef] [PubMed]
- Gandhi, T.K.; Kachalia, A.; Thomas, E.J.; Puopolo, A.L.; Yoon, C.; Brennan, T.A.; Studdert, D.M. Missed and delayed diagnoses in the ambulatory setting: A study of closed malpractice claims. Ann. Intern. Med. 2006, 145, 488–496. [Google Scholar] [CrossRef]
- Avorn, J.; Everitt, D.E.; Baker, M.W. The neglected medical history and therapeutic choices for abdominal pain. A nationwide study of 799 physicians and nurses. Arch. Intern. Med. 1991, 151, 694–698. [Google Scholar] [CrossRef]
- Tam, V.C.; Knowles, S.R.; Cornish, P.L.; Fine, N.; Marchesano, R.; Etchells, E.E. Frequency, type and clinical importance of medication history errors at admission to hospital: A systematic review. CMAJ 2005, 173, 510–515. [Google Scholar] [CrossRef] [PubMed]
- Eze-Nliam, C.; Cain, K.; Bond, K.; Forlenza, K.; Jankowski, R.; Magyar-Russell, G.; Yenokyan, G.; Ziegelstein, R.C. Discrepancies between the medical record and the reports of patients with acute coronary syndrome regarding important aspects of the medical history. BMC Health Serv. Res. 2012, 12, 78. [Google Scholar] [CrossRef]
- LeBlanc, V.R.; Regehr, C.; Tavares, W.; Scott, A.K.; MacDonald, R.; King, K. The impact of stress on paramedic performance during simulated critical events. Prehospital Disaster Med. 2012, 27, 369–374. [Google Scholar] [CrossRef]
- Groombridge, C.J.; Kim, Y.; Maini, A.; Smit, V.; Fitzgerald, M.C. Stress and decision-making in resuscitation: A systematic review. Resuscitation 2019, 144, 115–122. [Google Scholar] [CrossRef]
- Dewitt, B.; Persson, J.; Wallin, A. Perceptions of Clinical Experience and Scientific Evidence in Medical Decision Making: A Survey of a Stratified Random Sample of Swedish Health Care Professionals. Med. Decis. Mak. 2024, 44, 335–345. [Google Scholar] [CrossRef]
- Fischer, H.; Strunk, G.; Neuhold, S.; Kiblböck, D.; Trimmel, H.; Baubin, M.; Domanovits, H.; Maurer, C.; Greif, R. The effectiveness of ERC advanced life support (ALS) provider courses for the retention of ALS knowledge. Resuscitation 2012, 83, 227–231. [Google Scholar] [CrossRef]
- Paliatsiou, S.; Xanthos, T.; Wyllie, J.; Volaki, P.; Sokou, R.; Bikouli, D.; Iliodromiti, Z.; Boutsikou, T.; Iacovidou, N. Theoretical knowledge and skill retention 3 and 6 months after a European Newborn Life Support provider course. Am. J. Emerg. Med. 2021, 49, 83–88. [Google Scholar] [CrossRef]
- Russo, S.; Berg, K.; Davis, J.; Davis, R.; Riesenberg, L.A.; Morgan, C.; Chambers, L.; Berg, D. Incoming Interns Recognize Inadequate Physical Examination as a Cause of Patient Harm. J. Med. Educ. Curric. Dev. 2020, 7, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Kachalia, A.; Gandhi, T.K.; Puopolo, A.L.; Yoon, C.; Thomas, E.J.; Griffey, R.; Brennan, T.A.; Studdert, D.M. Missed and delayed diagnoses in the emergency department: A study of closed malpractice claims from 4 liability insurers. Ann. Emerg. Med. 2007, 49, 196–205. [Google Scholar] [CrossRef] [PubMed]
- Verghese, A.; Charlton, B.; Kassirer, J.P.; Ramsey, M.; Ioannidis, J.P. Inadequacies of Physical Examination as a Cause of Medical Errors and Adverse Events: A Collection of Vignettes. Am. J. Med. 2015, 128, 1322–1324.e3. [Google Scholar] [CrossRef]
- Frier, B.M. How hypoglycaemia can affect the life of a person with diabetes. Diabetes Metab. Res. Rev. 2008, 24, 87–92. [Google Scholar] [CrossRef]
- Amiel, S.A. The consequences of hypoglycaemia. Diabetologia 2021, 64, 963–970. [Google Scholar] [CrossRef]
- Cain, E.; Ackroyd-Stolarz, S.; Alexiadis, P.; Murray, D. Prehospital hypoglycemia: The safety of not transporting treated patients. Prehosp. Emerg. Care 2003, 7, 458–465. [Google Scholar] [CrossRef]
- Urushidani, S.; Tanabe, M.; Baek, K.; Miyaguchi, K.; Ikegami, T. Seizure occurrences among hypoglycemic patients in the emergency department. Acute Med. Surg. 2024, 11, e979. [Google Scholar] [CrossRef] [PubMed]
- Chow, E.; Bernjak, A.; Williams, S.; Fawdry, R.A.; Hibbert, S.; Freeman, J.; Sheridan, P.J.; Heller, S.R. Risk of cardiac arrhythmias during hypoglycemia in patients with type 2 diabetes and cardiovascular risk. Diabetes 2014, 63, 1738–1747. [Google Scholar] [CrossRef]
- Yeh, H.F.; Chao, W.C.; Wu, C.L.; Chan, M.C. Hypoglycemia and hospital mortality in critically ill patients. Sci. Rep. 2025, 15, 2642. [Google Scholar] [CrossRef]
- Olgers, T.J.; Dijkstra, R.S.; Drost-de Klerck, A.M.; Ter Maaten, J.C. The ABCDE primary assessment in the emergency department in medically ill patients: An observational pilot study. Neth. J. Med. 2017, 75, 106–111. [Google Scholar]
- Patocka, C.; Lockey, A.; Lauridsen, K.G.; Greif, R. Impact of accredited advanced life support course participation on in-hospital cardiac arrest patient outcomes: A systematic review. Resusc. Plus 2023, 14, 100389. [Google Scholar] [CrossRef]
- Restivo, V.; Minutolo, G.; Battaglini, A.; Carli, A.; Capraro, M.; Gaeta, M.; Odone, A.; Trucchi, C.; Favaretti, C.; Vitale, F.; et al. Leadership Effectiveness in Healthcare Settings: A Systematic Review and Meta-Analysis of Cross-Sectional and Before-After Studies. Int. J. Environ. Res. Public Health 2022, 19, 10995. [Google Scholar] [CrossRef] [PubMed]
- Hunziker, S.; Johansson, A.C.; Tschan, F.; Semmer, N.K.; Rock, L.; Howell, M.D.; Marsch, S. Teamwork and leadership in cardiopulmonary resuscitation. J. Am. Coll. Cardiol. 2011, 57, 2381–2388. [Google Scholar] [CrossRef] [PubMed]
- AlQorashi, S.A.M.; Kabli, A.A.M.; Alwithenani, S.I.; Alharbi, S.S.F.; Alshehri, M.A.A. The Effectiveness of the International Trauma Life Support (ITLS) Course on Multidisciplinary Healthcare Providers. Cureus 2025, 17, e77886. [Google Scholar] [CrossRef] [PubMed]
- Benito, J.; Luaces-Cubells, C.; Mintegi, S.; Manrique Martínez, I.; De la Torre Espí, M.; Miguez Navarro, C.; Vazquez López, P.; Campos Calleja, C.; Ferres Serrat, F.; Alonso Salas, M.T.; et al. Evaluation and Impact of the “Advanced Pediatric Life Support” Course in the Care of Pediatric Emergencies in Spain. Pediatr. Emerg. Care 2018, 34, 628–632. [Google Scholar] [CrossRef] [PubMed]

| Number (N) | Percentage (%) | |
|---|---|---|
| Gender: | ||
| Female | 8 | 9.5 |
| Male | 75 | 89.3 |
| No response | 1 | 1.2 |
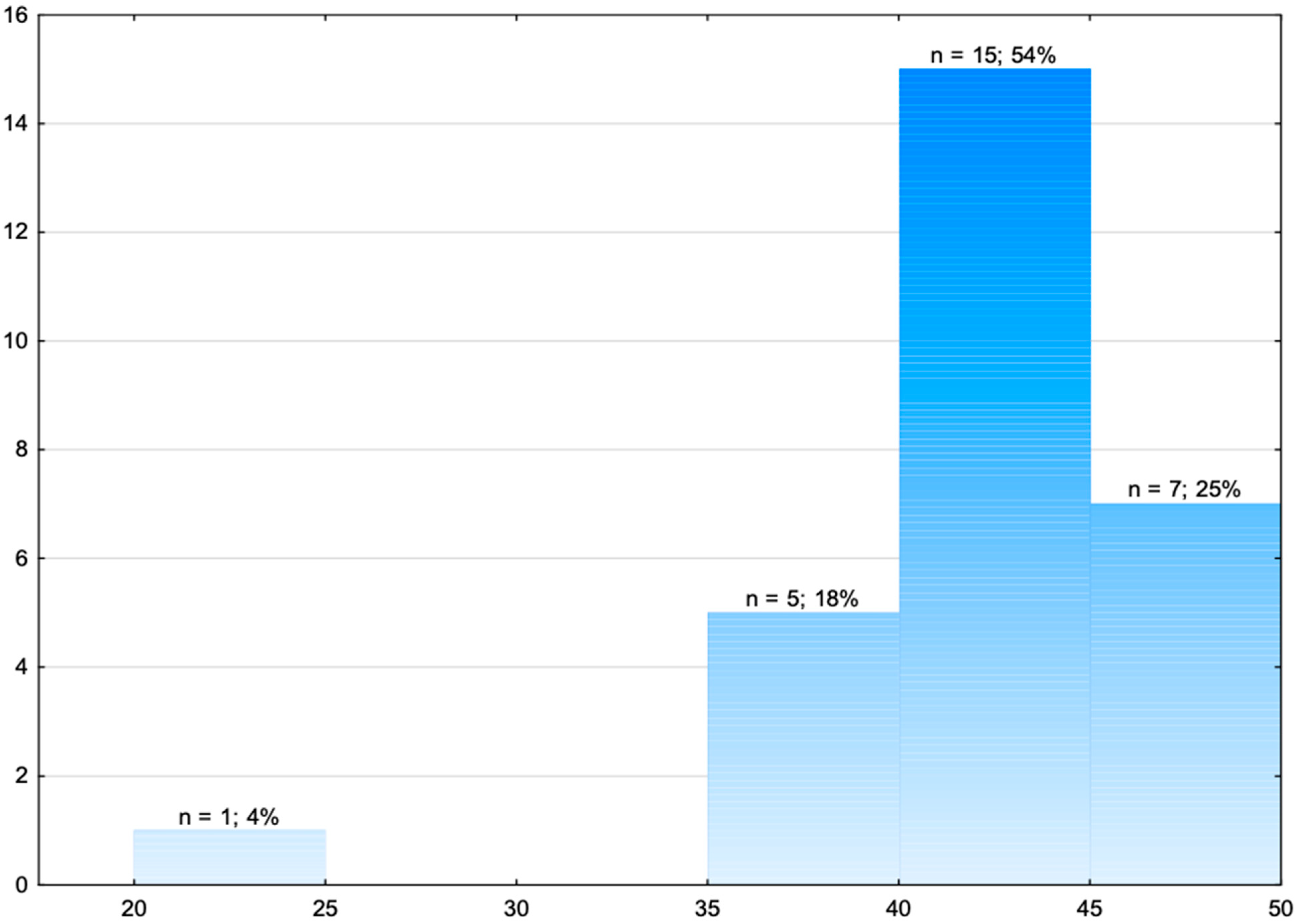
| Age: | ||
| 20–25 | 11 | 13.1 |
| 26–35 | 47 | 56 |
| 36–45 | 20 | 23.8 |
| Over 45 | 6 | 7.1 |
| Education: | ||
| Vocational school/Further education | 13 | 15.5 |
| Bachelor’s | 48 | 57.1 |
| Master’s | 23 | 27.4 |
| Profession: | ||
| Paramedic | 76 | 90.5 |
| Nurse | 2 | 2.4 |
| People with the professional title of both nurse and paramedic | 6 | 7.1 |
| Length of work experience: | ||
| 0–5 years | 24 | 28.6 |
| 6–15 years | 44 | 52.4 |
| 16–25 years | 16 | 15.5 |
| Over 25 years | 3 | 3.6 |
| Place of work: | ||
| Medical response team | 84 | 100% |
| Medical transport | 4 | 4.8% |
| Emergency department/admissions department | 18 | 21.4% |
| Hospital wards | 9 | 10.7% |
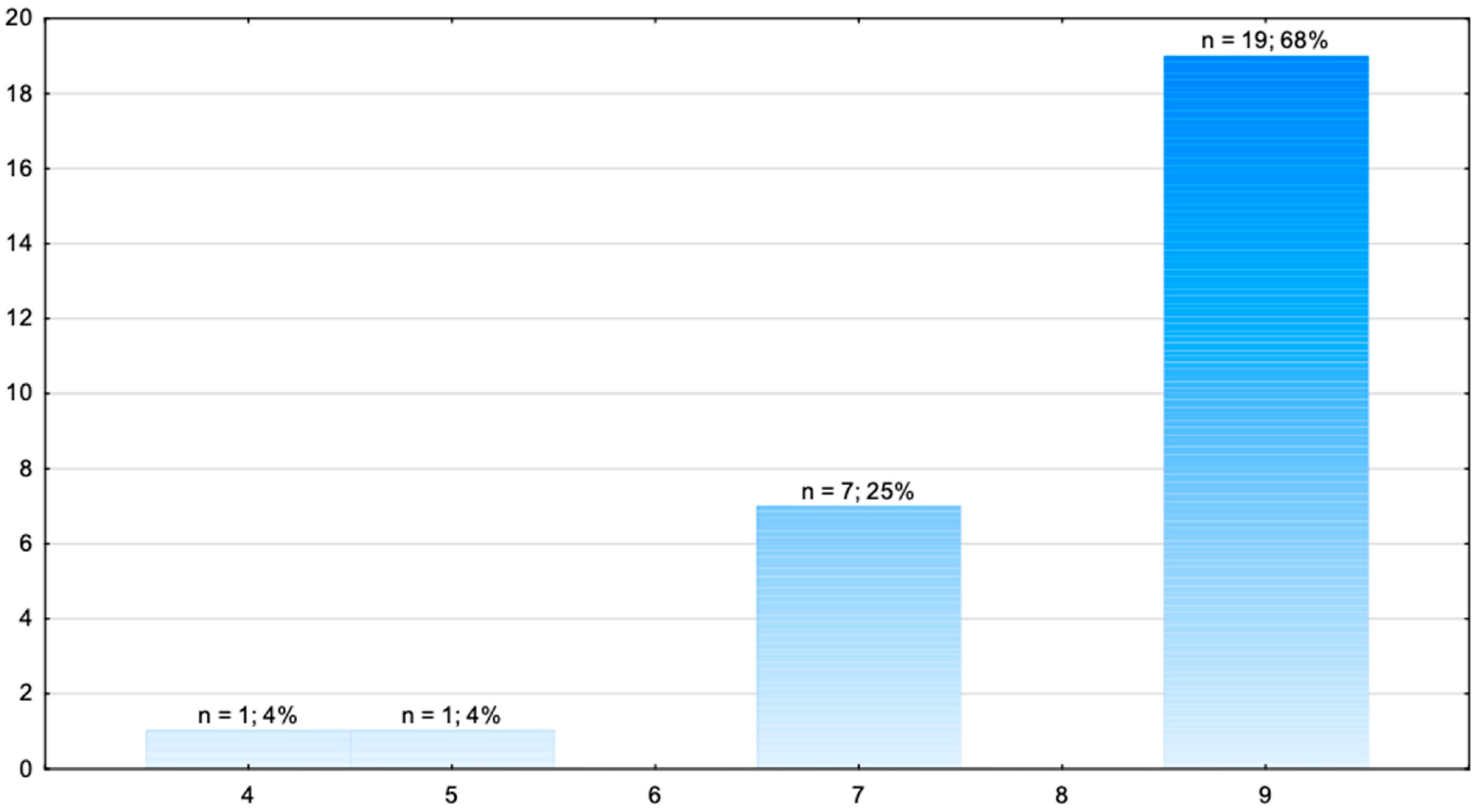
| Completed ALS course: | ||
| Yes | 19 | 68% |
| No | 9 | 32% |
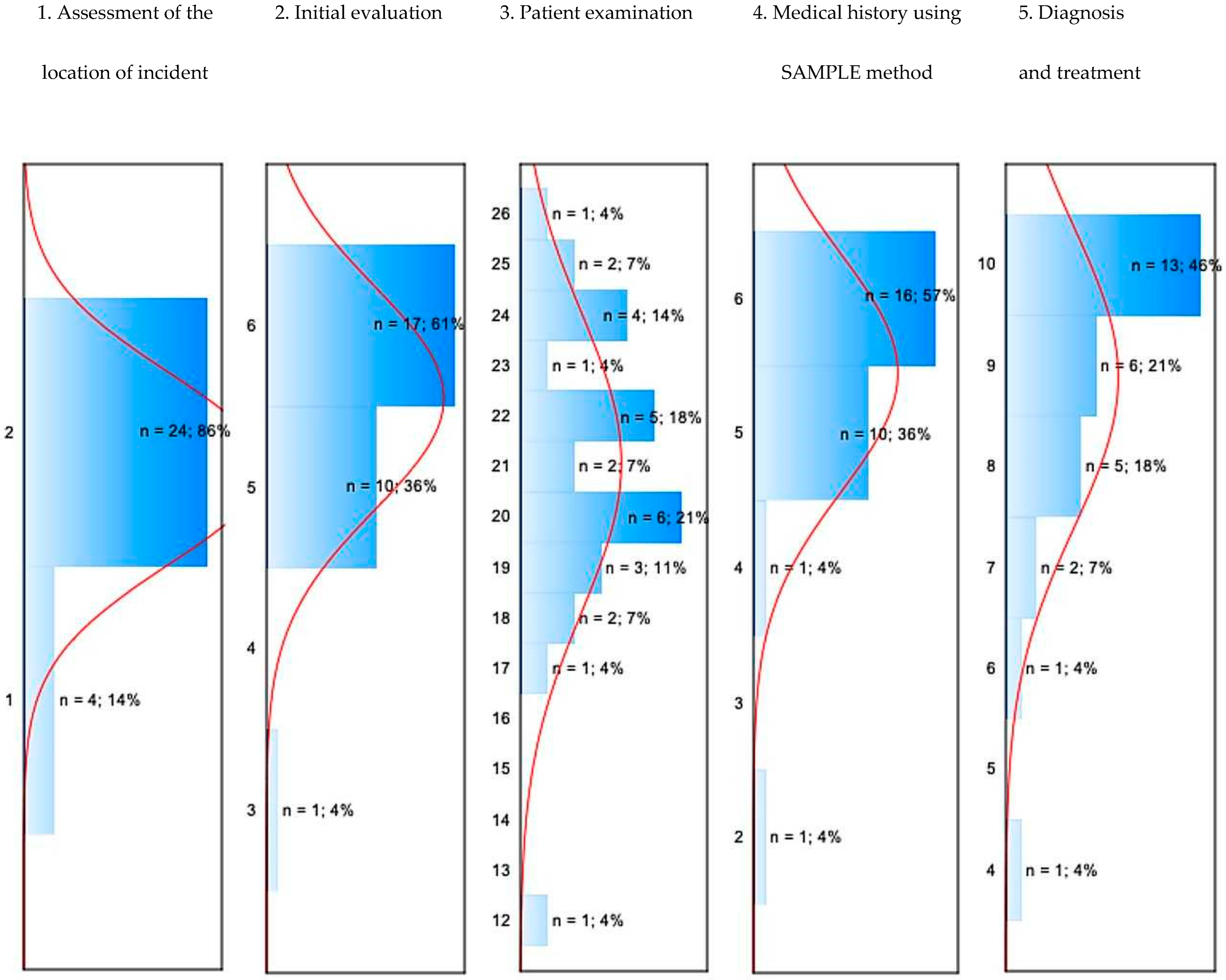
| Elements on Assessment Cards Awarded Points | Descriptive Statistics | |||||
|---|---|---|---|---|---|---|
| N | Mean | Median | Min. | Max. | Std. Dev. | |
| 1. Assessment of the location of the incident | 28 | 1.86 | 2 | 1 | 2 | 0.36 |
| 1.1. Safety assessment | 28 | 0.89 | 1 | 0 | 1 | 0.31 |
| 1.2. Personal protection equipment | 28 | 0.96 | 1 | 0 | 1 | 0.19 |
| 2. Initial evaluation | 28 | 5.54 | 6 | 3 | 6 | 0.69 |
| 2.1. Assessment of consciousness | 28 | 1.00 | 1 | 1 | 1 | 0.00 |
| 2.2. Assessment on AVPU/GCS scale | 28 | 0.64 | 1 | 0 | 1 | 0.49 |
| 2.3. Removal of contents of airways | 28 | 1.00 | 1 | 1 | 1 | 0.00 |
| 2.4. Instrumental airway management | 28 | 0.93 | 1 | 0 | 1 | 0.26 |
| 2.5. Assessment of breathing | 28 | 1.00 | 1 | 1 | 1 | 0.00 |
| 2.6. Assessment of pulse | 28 | 0.96 | 1 | 0 | 1 | 0.19 |
| 3. Patient examination | 28 | 21.04 | 21 | 12 | 26 | 2.95 |
| 3.1. Spo2 assessment | 28 | 0.96 | 1 | 0 | 1 | 0.19 |
| 3.2. Listening to the chest | 28 | 1.71 | 2 | 1 | 2 | 0.46 |
| 3.3. Assessment of the skin and capillary refill | 28 | 1.96 | 2 | 0 | 4 | 1.60 |
| 3.4. Assessment of blood pressure | 28 | 1.00 | 1 | 1 | 1 | 0.00 |
| 3.5. Performance of 12-lead ECG | 28 | 0.89 | 1 | 0 | 1 | 0.31 |
| 3.6. Assessment of the pupils | 28 | 0.96 | 1 | 0 | 1 | 0.19 |
| 3.7. Assessment of glycemia | 28 | 3.00 | 3 | 3 | 3 | 0.00 |
| 3.8. Assessment of deep temperature | 28 | 0.89 | 1 | 0 | 1 | 0.31 |
| 3.9. Patient exposure, injury diagnosis | 28 | 1.89 | 2 | 1 | 2 | 0.31 |
| 3.10. Repeated removal of the content of the airways | 28 | 1.93 | 2 | 0 | 2 | 0.38 |
| 3.11. Use of a new catheter for the second removal | 28 | 0.29 | 0 | 0 | 2 | 0.71 |
| 3.12. Selection of a second place for intraosseous access due to contraindications | 28 | 2.89 | 3 | 0 | 3 | 0.57 |
| 3.13. Obtaining i.o. access | 28 | 2.64 | 3 | 0 | 3 | 0.68 |
| 4. Medical history following the SAMPLE method | 28 | 5.43 | 6 | 2 | 6 | 0.88 |
| 4.1. SAMPLE | 28 | 5.43 | 6 | 2 | 6 | 0.88 |
| 5. Diagnosis and treatment | 28 | 8.86 | 9 | 4 | 10 | 1.48 |
| 5.1. Administration of glucose at a minimum dose of 200 mg/kg body weight | 28 | 4.68 | 5 | 0 | 5 | 1.19 |
| 5.2. Repeated glycemia measurement | 28 | 3.50 | 4 | 2 | 4 | 0.88 |
| 5.3. Securing fractured lower leg | 28 | 0.68 | 1 | 0 | 1 | 0.48 |
| Task assessment card—overall result | 28 | 42.82 | 43 | 23 | 49 | 4.96 |
| Assessment Card Elements | Descriptive Statistics | |||||
|---|---|---|---|---|---|---|
| N | Mean | Median | Minimum | Maximum | Standard Deviation | |
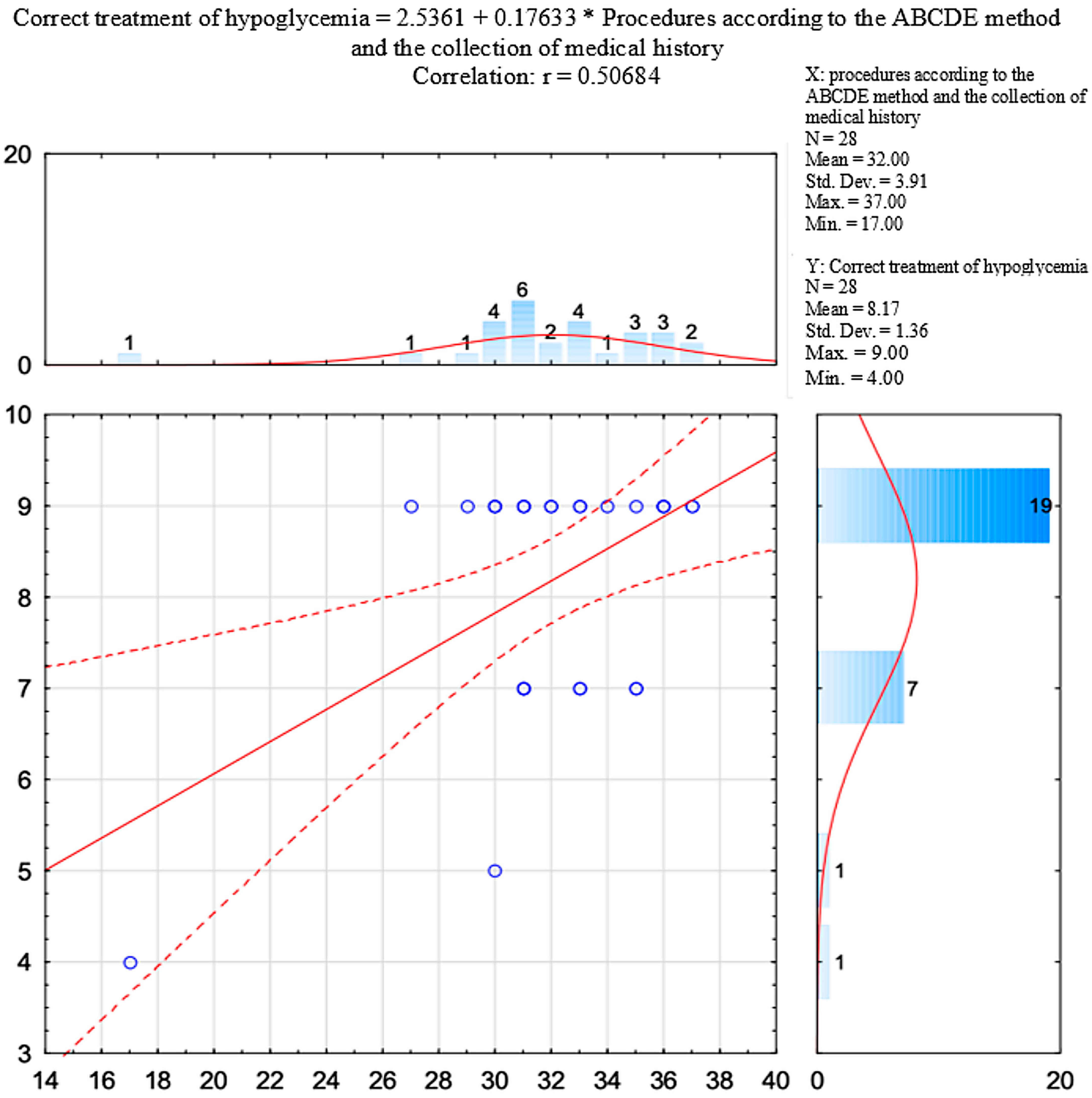
| Procedures in accordance with the ABCDE method, and collecting the medical history | 28 | 32.00 | 32 | 17 | 37 | 3.92 |
| Assessment Card Elements | Descriptive Statistics | |||||
|---|---|---|---|---|---|---|
| N | Mean | Median | Minimum | Maximum | Standard Deviation | |
| Correct treatment of hypoglycaemia. | 28 | 8.18 | 9 | 4 | 9 | 1.36 |
| Examination According to the ABCDE Method and the Collection of Medical History (Variable X) and Correct Treatment of Hypoglycaemia (Variable Y) | Procedures in Accordance with the ABCDE and SAMPLE Methods | Correct Treatment of Hypoglycaemia |
|---|---|---|
| Mean | 32.00 | 8.18 |
| Standard deviation | 3.92 | 1.36 |
| r (X,Y) | 0.507 | |
| r2 | 0.257 | |
| t | 2.998 | |
| p | 0.006 |
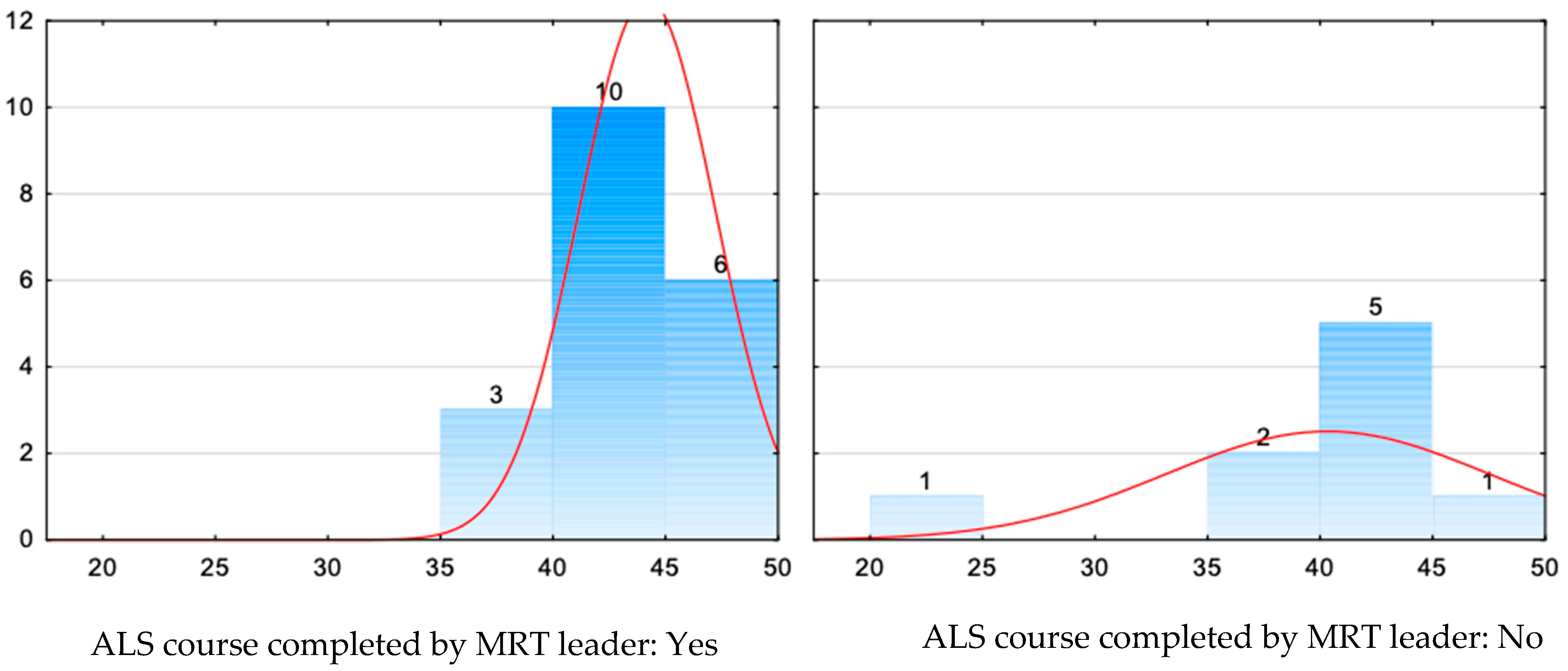
| U Mann–Whitney Test (with Continuity Correction) In Relation to the Variable: ALS Course Completed by MRT Leader | ||||||
|---|---|---|---|---|---|---|
| Rank Sum (Yes) | Rank Sum (No) | With Correction | p | N (Yes) | N (No) | |
| Total points obtained | 308.5000 | 97.50000 | 1.607560 | 0.107933 | 19 | 9 |
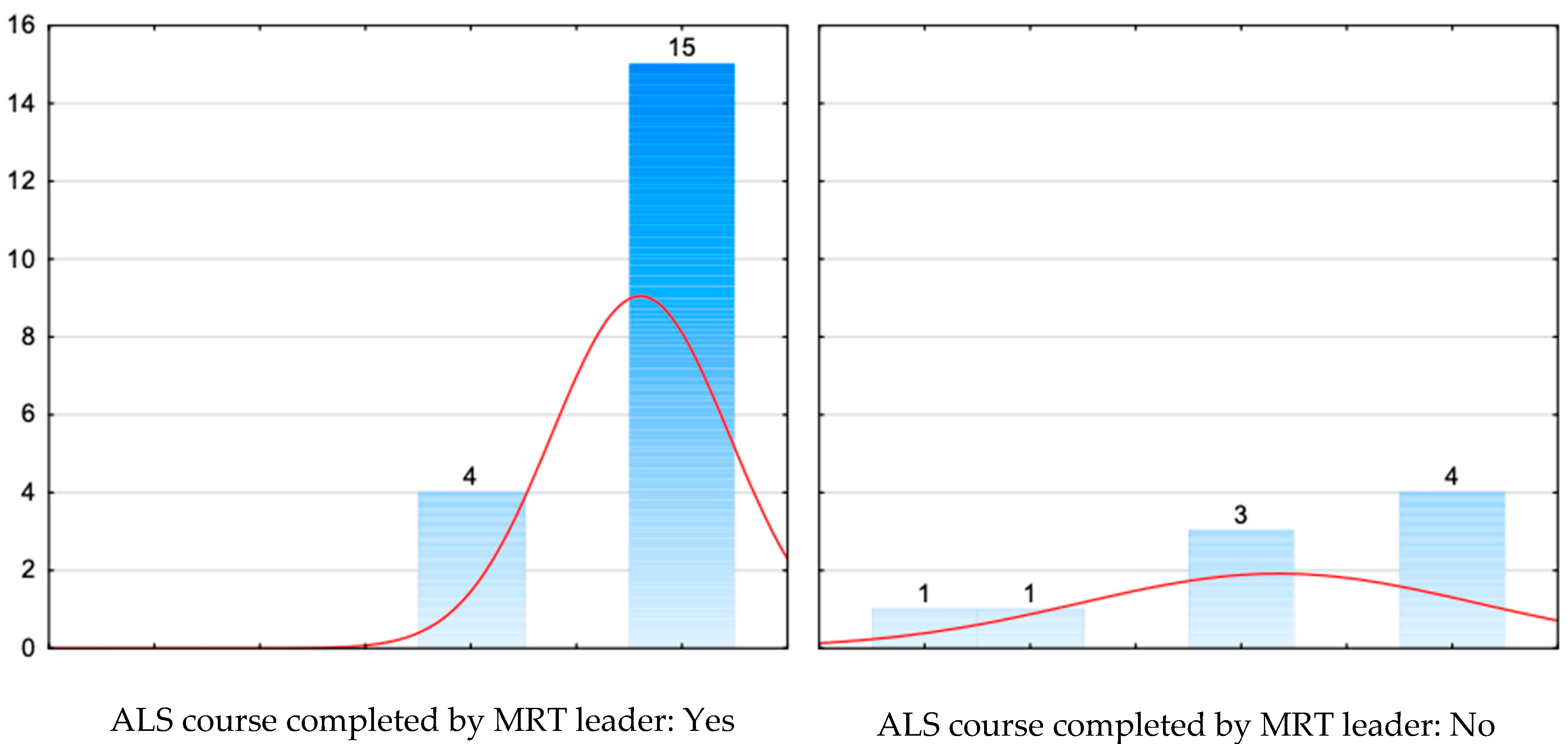
| U Mann–Whitney Test (with Continuity Correction) In Relation to the Variable: ALS Course Completed by MRT Leader | ||||||
|---|---|---|---|---|---|---|
| Rank Sum (Yes) | Rank Sum (No) | With Correction | p | N (Yes) | N (No) | |
| Correct treatment of hypoglycaemia | 309.0000 | 97.00000 | 1.979251 | 0.047789 | 19 | 9 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Krysiak, D.; Ćwiertnia, M.; Wójcik, M.; Babik, P.; Suchanek, Ł.; Jaskiewicz, F.; Trojak-Piętka, J.; Szlagor, M.; Pollok-Waksmańska, W.; Kawecki, M.; et al. Analysis of Medical Response Team Interventions and the Impact of Certified Training on the Treatment of Patients with Hypoglycaemia—A Simulation Study. J. Clin. Med. 2025, 14, 8318. https://doi.org/10.3390/jcm14238318
Krysiak D, Ćwiertnia M, Wójcik M, Babik P, Suchanek Ł, Jaskiewicz F, Trojak-Piętka J, Szlagor M, Pollok-Waksmańska W, Kawecki M, et al. Analysis of Medical Response Team Interventions and the Impact of Certified Training on the Treatment of Patients with Hypoglycaemia—A Simulation Study. Journal of Clinical Medicine. 2025; 14(23):8318. https://doi.org/10.3390/jcm14238318
Chicago/Turabian StyleKrysiak, Damian, Michał Ćwiertnia, Michał Wójcik, Piotr Babik, Łukasz Suchanek, Filip Jaskiewicz, Joanna Trojak-Piętka, Michał Szlagor, Wioletta Pollok-Waksmańska, Marek Kawecki, and et al. 2025. "Analysis of Medical Response Team Interventions and the Impact of Certified Training on the Treatment of Patients with Hypoglycaemia—A Simulation Study" Journal of Clinical Medicine 14, no. 23: 8318. https://doi.org/10.3390/jcm14238318
APA StyleKrysiak, D., Ćwiertnia, M., Wójcik, M., Babik, P., Suchanek, Ł., Jaskiewicz, F., Trojak-Piętka, J., Szlagor, M., Pollok-Waksmańska, W., Kawecki, M., & Ilczak, T. (2025). Analysis of Medical Response Team Interventions and the Impact of Certified Training on the Treatment of Patients with Hypoglycaemia—A Simulation Study. Journal of Clinical Medicine, 14(23), 8318. https://doi.org/10.3390/jcm14238318








